ABSTRACT
Objective: To evaluate the efficacy of hyaluronidase as an adjuvant with volume reduction of bupivacaine in ultrasound-guided supraclavicular brachial plexus block for chronic renal failure patients.Design: Prospective double-blinded, randomized studySetting: tertiary institutional clinical carePatients, Participants: carried out on 60 patients with American Society of Anesthesiologists Classification (ASA) of physical status grade III with chronic renal failure with end-stage renal disease (ESRD) scheduled for elective surgery for arteriovenous shunt creation.Intervention: Both groups were US guided. In group I, patients received plain bupivacaine 0.5% (30 ml) by single-injection technique while in group II, patients received plain bupivacaine 0.5% (10 ml) plus 0.9% (5 ml) normal saline containing 500 IU (100 IU/ml) hyaluronidase.Main outcome (primary and secondary): The duration of sensory block, the onset of sensory and motor block, success rate, duration of motor block, total doses of intraoperative rescue analgesia, number of patients needed for postoperative rescue analgesia, and complications were recorded.Results: Hyaluronidase group had a significantly rapid onset of sensory and motor block than that of the bupivacaine group. On the other hand, both groups were similar in the duration of sensory block and motor block.Conclusion: Single injection technique was a sufficient modality of brachial plexus block. Hyaluronidase as an adjuvant to the local anesthetics has been fastened the onset of complete sensory block of ultrasound-guided supraclavicular brachial plexus blocks with minimal effect analgesic consumption postoperatively.
1. Introduction
Ultrasound-guided supraclavicular brachial plexus block is a popular regional anesthetic technique for the upper limb and has multiple applications. [Citation1] As it has many advantages over other approaches as providing the most complete and reliable anesthesia for upper-limb surgery. [Citation2]
Local anesthetics (LAs) with additives like opioids, clonidine, dexmedetomidine, and steroids have been used to prolong this blockade, but the results are either inconclusive or associated with side effects. [Citation3]
The conventional technique required deposition of a local anesthetic close to the plexus, but was usually associated with ulnar sparing and incomplete block. While Eight ball corner pocket technique allows the deposition of local anesthetic inside the pocket formed laterally by subclavian artery and inferiorly first rib to faster the onset. [Citation4] However, this is associated with successful block only in 85% of the cases. [Citation5]
Hyaluronidase acts by catalyzing the hydrolysis of hyaluronan, decreased its viscosity, and enchasing the tissue permeability. So, this makes it a suitable additive for other drugs to speed up their distribution and delivery especially in ophthalmic surgery. [Citation6]
Several studies showed that multiple injection techniques of the brachial plexus were more successful with a faster onset of anesthesia and higher success rates, with a change in the incidence of complications. [Citation7,Citation8] On the other hand, another study found the single-injection (SI) ultrasound in the corner pocket has the highest success rate but may miss the upper part of the plexus, resulting in a patchy block. [Citation9]
This single-blinded randomized prospective study was conducted to evaluate the efficacy of hyaluronidase as an adjuvant to the two different bupivacaine volumes in ultrasound-guided supraclavicular brachial plexus block. The primary outcome of this study was the duration of sensory block, while secondary outcomes included the onset of sensory and motor block, success rate, duration of motor block, total doses of intraoperative rescue analgesia, number of patients needed for postoperative rescue analgesia, and complications.
2. Patients and methods
This prospective, randomized, double-blinded study was carried out in Tanta University Hospitals in vascular surgery department from January 2020 to June 2020 on 60 patients aged from 19–44 years, American Society of Anesthesiologists Classification (ASA) of physical status grade III with chronic renal failure with end-stage renal disease (ESRD) scheduled for elective surgery for arteriovenous shunt creation.
After the regional ethical committees’ approval, written informed consent was taken from the patients. The trial was registered in the Pan African Clinical Trial Registry with a unique identification number for the registry is PACTR202002803417431. Every patient was receiving an explanation of the purpose of the study and a secret code number and the photos applied only to the part of the body related to the research to ensure privacy to participants and confidentiality of data. Randomization was performed by an independent data manager who divided the patients into two groups based on a number in a sealed envelope generated by a computer randomization program.
Patients with neurological affection of the upper limb, bleeding diathesis, mental illness, history of drug addiction, the chronic analgesic user, or history of local anesthetic allergy were excluded from the study.
Preanesthetic routine investigations, such as complete blood count test, liver, kidney function test, coagulation profile, ABG, and electrolyte were done. The patients were fasting for 8 hr. The patients were trained to use the Visual analogue Scale (VAS) [VAS 0 = no pain, 10 = intolerable pain] used for evaluation of pain intensity, pain relief was defined as a VAS of 3 or lower. On arrival to the operating room, noninvasive monitors, such as electrocardiography, noninvasive blood pressure (NIBP), oxygen saturation (SpO2), were attached and baseline parameters as heart rate, mean arterial pressure, and peripheral oxygen saturation was recorded. Every patient received an Oxygen mask with Oxygen at the rate of 4 l/min and an intravenous line was inserted in another arm so IV fluid could be started and continued throughout the operation according to need.
In supine position and head facing the contralateral side, skin and transducer preparation, a linear 38 mm, then high-frequency 10–15 MHz transducer (SonoScape A5; Shenzhen, China) was placed at the midclavicular point over the supraclavicular fossa in the coronal oblique plane. The brachial plexus appeared as a hypoechoic round or oval cluster located lateral and superficial to the pulsatile subclavian artery and superior to the first rib. Then using an in-plane approach, a 22-G spinal needle was inserted into the lateral end of the ultrasound transducer. The needle was advanced along the long axis of the transducer in the same plane as the ultrasound beam from lateral to medial towered sheath at the corner pocket below the cluster. Then local anesthetics (LA) solution was injected to cause tissue hydro-dissection around the plexus.
Then 60 Patients were randomly allocated into two equal groups each of 30 patients: in group I, patients received 30 ml plain bupivacaine 0.5% [Citation10,Citation11] (Sunny pharmaceutical, Egypt) by single-injection technique while in group II, patients received 15 ml volume [10 ml 0.5% bupivacaine (Sunny pharmaceutical, Egypt) plus 5 ml 0.9% normal saline containing 500 IU (100 IU/ml) hyaluronidase (Hynidase, Shreya Life Sciences Pvt Ltd, India)] by single-injection technique. Hyaluronidase was prepared by diluting the vial of hyaluronidase (1500 IU) in 15 ml normal saline 0.9%.
The local anesthetic solution was prepared by an anesthesiologist who was blinded to each patient’s randomization number and not included in the study. Monitoring of all parameters was done by an independent anesthesiologist who was not involved in the study. All procedures were performed by a single anesthetist.
3. Outcome assessment
Demographic data of all included patients including age, gender, weight, and duration of the surgery were documented. The sensory loss was assessed by pinprick in the skin cross ponding to dermatomal areas supplied by the median nerve, radial nerve, ulnar nerve, and the musculocutaneous nerve at 5 minutes interval and up to 30 minutes after local anesthetic solution injection and the results were interpreted as 0 scores for no block (normal sensation); 1 for partial block (decreased sensation) and 2 for the complete block (no sensation). Motor block was assessed by the ability of patients to flex the elbow and their hand against gravity at 5 minutes interval up to 30 min and was classified as follows: 0 in patients with full muscle activity (no block); 1 for patients had decreased muscle activity (partial block); and 2 for those with no muscle activity (complete successful block). [Citation12]
Success block was defined as complete loss of sensory and motor function. In cases with unsuccessful or patchy block, supplemented intraoperative fentanyl was used as rescue analgesia at dose 1.5 µ/kg. [Citation13] If the pain disappeared, the patient continued as a part of the study. But if the pain persists or patients had failed block, general anesthesia was conducted and patients were excluded from the study.
Duration of sensory block was defined as the time interval from the achievement of complete sensory loss until the patient started to complain of pain or discomfort assessed by Visual Analogue Scale (VAS) [Citation14] (VAS>3) ranged from 0–10. Postoperative follow-up was carried out in the recovery room and postoperative ward for assessment of pain every 30 minutes for the first 10 hours then each hour for the following 12 hours. All patients in both groups received postoperatively paracetamol (E.I.P.I.CO. Egypt) 650 every 8 hours during the 1st postoperative day. [Citation15]
Duration of motor block was defined as the time interval from the total inability to move his or her fingers or to raise their hand (motor scale = 2) till the patient started to partially move them (motor scale = 1) and assessed every hour by asking the patients to move their fingers and raise their hand. Also, the number of patients needed postoperative rescue analgesia in the form of intravenous morphine at a dose of 0.05 mg/kg (15) when VAS ≥ 4 during 24 hours and incidence of complications. Horner’s syndrome, voice changes, and pneumothorax were recorded as complications.
4. Statistical analysis
The sample size calculation was performed using G. power 3.1. Thirty patients were allocated in each group. The sample size was calculated as N ≥ 27 in each group based on the following considerations: 0.05 α error and 90% power of the study. Group ratio 1:1 According to a previous study [Citation16], the mean (±SD) of a duration of sensory block was 3.6 ± 1.19 hours with bupivacaine in supraclavicular block and expected 30% increase (1.08 hour) with an addition of hyaluronidase. Three cases were added to each group to overcome dropout. Data were analyzed using SPSS Version 24 (IBM Corporation, Armonk, NY). Categorical variables were presented as absolute numbers and percentages. Continuous variables were presented as mean values with standard deviation or medians with an interquartile range. To compare data between groups, the chi-square test was used to assess categorical variables, and the Student t-test or the Mann–Whitney U test was used to analyze continuous variables as appropriate. A Paired t-test or the Wilcoxon test was used for comparison within the same group as appropriate. A 2-tailed P value of <0.05 was considered to indicate a statistically significant difference.
5. Results
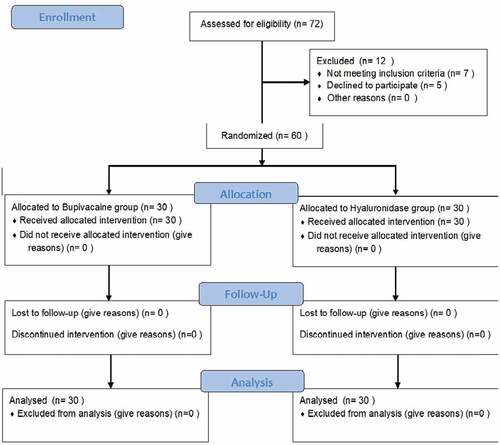
Seventy-two patients were evaluated for eligibility, 12 patients from them were excluded either 7 patients did not fulfill the inclusion criteria (2 had a neurological deficit at the upper limb, one patient was mental dysfunction, and 4 had chronic analgesic use) and 5 patients refused to participate in the study. The remaining 60 patients were randomly allocated into 2 equal groups. Data of all patients were successfully collected ().
Demographic data, including age, weight, gender, and duration of the surgery were comparable between the two groups (P = 0.693 for age; P = 0.433 for weight, P = 0.426 for gender, P = 0.967 for duration of the surgery). ()
Table 1. Demographic data
Regarding the onset of sensory block and motor block, the hyaluronidase group had statistically significantly rapid onset of both than that at bupivacaine group (p = 0.0001 for both). On the other hand, both groups were similar in the duration of sensory block and motor block (p = 0.544 and 0.558, respectively) ().
Table 2. Characters of sensory and motor block in both groups
Intraoperative, only three patients in the bupivacaine group and two patients in the hyaluronidase group had patchy block which was successfully treated by fentanyl as rescue analgesia with no statistically significant difference in the success rate between the hyaluronidase group and bupivacaine group (p = 0.64).
Regarding the numbers of patients who needed postoperative rescue analgesia, there was no statistically significant difference between the two groups (p = 0.488) as five patients in the bupivacaine group and three patients in the hyaluronidase group had VAS ≥ 4. All of them received postoperative morphine as rescue analgesia.
As regards the incidence of complications including Horner’s syndrome, voice changes, and pneumothorax, there were statistically insignificant differences between the two groups. (p = 0.41)
6. Discussion
The anesthesia for arteriovenous shunt creation varied between general anesthesia, regional anesthesia, and local infiltration. One of the most important advantages of regional anesthesia was sympathetic nerve which enhanced venous dilatation and increased blood flow, prevent thrombosis and fistula failure either intraoperatively or postoperatively. [Citation17]
The minimum local anesthetic volume for the successful supraclavicular block was 23 ml to minimize the frequency and dose-dependent manner of systemic toxicity. Therefore, one of the anesthetist goals was the reduction of used LA volume to maintain the safety of regional anesthesia without affecting the success rate. [Citation18] Hyaluronidase is known to enhance the onset of the block and improve the quality of anesthesia especially, in regional anesthesia for ophthalmology surgery and subcutaneous infiltration blocks to maximize the distribution of local anesthetics. [Citation6]
De Jong [Citation19] stressed the importance of adequate volume for the first time then Winnie [Citation20] suggested that 0.5 ml per 2.54 cm of height was adequate volume to fill the axillary sheath. So, the present study evaluated the efficacy of hyaluronidase as an adjuvant to small volumes of bupivacaine in chronic renal failure patients scheduled for arteriovenous shunt creation surgery under ultrasound-guided supraclavicular brachial plexus block.
The present study was postulated that hyaluronidase may improve the spread of the local anesthetic solution, but may increase absorption of bupivacaine, both onset of sensory block and motor block significantly rapid in hyaluronidase group than bupivacaine group. On the other hand, both groups were similar in the duration of sensory block (p = 0.544) and motor block (p = 0.558), success rate (p = 0.64), and the number of patients who needed postoperative rescue analgesia (p = 0.488). This reduction of the time to reach complete sensory block allows rapid turnover between operations, associated with efficient utilization of operation rooms, especially if preoperative specialized room to perform nerve block was not available [Citation21].
As the present study used hyaluronidase with lower volume, the current study depends on its mechanism of action by catalyzing the hydrolysis of hyaluronan of the extracellular matrix, decreased its viscosity, and increasing tissue permeability, so although single-injection (SI) ultrasound-guided technique may miss the upper part of the plexus, resulting in a patchy block. The present study theory of hyaluronidase addition speeds up their distribution and ensures the complete successful block. [Citation6]
The results of this present study in harmony with Koh et al. study on axillary brachial plexus block used 3000 IU hyaluronidase added to ropivacaine and showed that significantly reduced sensory and motor onsets of the block than the control group. [Citation22]
Elsayed S, et al. study [Citation23], which compared the effect of hyaluronidase or adrenaline as an adjuvant to bupivacaine in supraclavicular brachial plexus block for upper limb surgeries, concluded that Hyaluronidase decreases the block onset time with minimal effect on block duration or postoperative analgesia; moreover, adrenaline has prolonged block duration and postoperative analgesia with minimal influence on block onset time. The results of Elsayed S, et al. study regarding adding hyaluronidase to supraclavicular were the same of the results as the present study.
Moreover, according to Adams, hyaluronidase has commonly used as an adjuvant in ophthalmic surgery to fasten the onset time of the ocular block and increase the success rate. [Citation24] de Moura BD, et al. Meta-Analysis of Randomized Clinical Trials [Citation25], which evaluated the efficacy of hyaluronidase in preventing total/partial failure of the regional block in ophthalmic surgery, was concluded that the efficacy of hyaluronidase associated with local anesthetics in preventing regional block failure in ophthalmic surgery. de Moura BD, et al. was similar to the results of this study by increasing the success rate of the regional block.
Besides, Kim et al., 2011a used the hyaluronidase in the epidural block as an adjuvant for LA and steroid for chronic back pain control. [Citation26]
Mohamed AA, et al. study [Citation27], which discussed the safety and efficacy of addition of hyaluronidase to a mixture of lidocaine and bupivacaine in scalp nerves block in craniotomy operations, supported the idea that addition of hyaluronidase to the local anesthetic mixture improves the success rates of the scalp nerves block and its efficacy especially during stressful intraoperative periods and in the early postoperative period with no evident undesirable effects concerning the addition of hyaluronidase. Mohamed AA, et al. study and this study supported that the use of hyaluronidase is an effective adjuvant to different regional blocks increasing the success rate and safety, improving efficacy, with no adverse effects related to hyaluronidase use.
However, despite ultrasound guidance, the rate of success of blocks in the present study is not 100%. Other than expertise operator, certain anatomical factors could be the cause of an unsuccessful or failed block. Similarly, in a study by Subramanyam et al., slower onset of the ulnar blockade and ulnar sparing remain the main drawbacks of the supraclavicular block. This may result from incorrect placement of needle tip and they recommended double-point injection technique of supraclavicular block to prevent ulnar sparing and increases the success rate. [Citation28] The most common side effect of hyaluronidase is allergy according to many studies [Citation25,Citation29–31]. It did not happen in the present study.
In disagreement with the current study, Keeler et al. reported significantly reduced the duration of the sensory and motor block by use of 3000 IU hyaluronidase additives to bupivacaine 0.5% for axillary brachial plexus blocks with no effect on the number of patients experiencing has a sensory block at 30 min after block and no increase in postoperative analgesic consumption. [Citation32]
While in kamal Hakim and Ahmed’s study, 1500 IU hyaluronidase was mixed with LA. Similar results of reduced duration of sensory and motor block were reported. When compared with the control group by Keeler et al. study, their difference was non-significant. [Citation33]
Although the results of the present study appeared promising, this study had few limitations as small sample size, plasma bupivacaine concentrations in hyaluronidase group were not assessed, absence of group in which traditional triple supraclavicular brachial plexuses block. Also, the present study could not report clear conclusions about the tolerance and safety of hyaluronidase in axillary brachial plexus block, although no adverse events were reported due to drawbacks mentioned previously.
7. Conclusion
The use of hyaluronidase with LA reduces the time to achieved complete sensory block without significant effect on the total analgesic duration and consumption.
Previous presentation in conferences
The contents have not been published elsewhere and the paper is not being submitted elsewhere. The manuscript has been read and approved by all co-author.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Williams SR, Chouinard P, Arcand G, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97(5):1518–1523.
- Neal JM, Hebl JR, Gerancher J, et al. Brachial plexus anesthesia: essentials of our current understanding. Reg Anesth Pain Med. 2002;27(4):402–428.
- Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014 Mar;112(3):427–439.
- Soares LG, Brull R, Lai J, et al. Eight ball, corner pocket: the optimal needle position for ultrasound-guided supraclavicular block. Reg Anesth Pain Med. 2007;32(1):94–95.
- Brull R, Chan VW. The corner pocket revisited. Reg Anesth Pain Med. 2011;36(3):308.
- Dunn AL, Heavner JE, Racz G, et al. Hyaluronidase: a review of approved formulations, indications and off-label use in chronic pain management. Expert Opin Biol Ther. 2010;10(1):127–131.
- Vester‐Andersen T, Broby‐Johansen U, Bro‐Rasmussen F. Perivascular axillary block VI: the distribution of gelatine solution injected into the axillary neurovascular sheath of cadavers. Acta Anaesthesiol Scand. 1986;30(1):18–22.
- Partridge B, Katz J, Benirschke K. Functional anatomy of the brachial plexus sheath: implications for anesthesia. Anesthesiology. 1987;66(6):743–747.
- Fredrickson M, Patel A, Young S, et al. Speed of onset of ‘corner pocket supraclavicular’ and infraclavicular ultrasound guided brachial plexus block: a randomised observer‐blinded comparison. Anaesthesia. 2009;64(7):738–744.
- Agarwal S, Aggarwal R, Gupta P. Dexmedetomidine prolongs the effect of bupivacaine in supraclavicular brachial plexus block. J Anaesthesiol Clin Pharmacol. 2014 Jan;30(1):36–40.
- Kapral S, Krafft P, Eibenberger K, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994 Mar;78(3):507–513.
- Kathuria S, Gupta S, Dhawan I. Dexmedetomidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block. Saudi J Anaesth. 2015;9(2):148–154.
- Launay-Vacher V, Karie S, Fau J-B, et al. Treatment of pain in patients with renal insufficiency: the World Health Organization three-step ladder adapted. J Pain. 2005;6(3):137–148.
- Lee JS, Hobden E, Stiell IG, et al. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med. 2003 Oct;10(10):1128–1130.
- Mazer M, Perrone J. Acetaminophen-induced nephrotoxicity: pathophysiology, clinical manifestations, and management. J Med Toxicol. 2008;4(1):2–6.
- Chan VW, Perlas A, Rawson R, et al. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97(5):1514–1517.
- Shemesh D, Olsha O, Orkin D, et al. Sympathectomy-like effects of brachial plexus block in arteriovenous access surgery. Ultrasound Med Biol. 2006;32(6):817–822.
- Jorgensen MS, Farres H, James BL, et al. The role of regional versus general anesthesia on arteriovenous fistula and graft outcomes: a single-institution experience and literature review. Ann Vasc Surg. 2020;62:287–294.
- DE Jong CRH. Axillary block of the brachial plexus. Anesthesiol J Am Soc Anesthesiologists. 1961;22(2):215–225.
- Winnie AP. Interscalene brachial plexus block. Anesth Analg. 1970;49(3):455–466.
- Minville V, Amathieu R, Gris C, et al. Infraclavicular brachial plexus block versus humeral approach: comparison of anesthetic time and efficacy. Anesth Analg. 2005;101(4):1198–1201.
- Koh W, Min H, Park H, et al. Use of hyaluronidase as an adjuvant to ropivacaine to reduce axillary brachial plexus block onset time: a prospective, randomised controlled study. Anaesthesia. 2015;70(3):282–289.
- Elsayed S, Ahmed FM, Khalifa OY. Hyaluronidase versus adrenaline as an adjuvant to bupivacaine in ultrasound-guided supraclavicular brachial plexus block for upper limb surgeries. Res Opin Anesthesia Intensive Care. 2019;6(2):206–213.
- Adams L. Adjuvants to local anaesthesia in ophthalmic surgery. Br J Ophthalmol. 2011;95(10):1345–1349.
- de Moura BD, de Miranda DB, Govêia CS. Addition of hyaluronidase reduces failure of regional block in ophthalmic surgery-meta-analysis of randomized clinical trials. Biomed J Sci Tech Res. 2020;29(4):22672–22678.
- Kim SB, Lee KW, Lee JH, et al. The additional effect of hyaluronidase in lumbar interlaminar epidural injection. Ann Rehabil Med. 2011;35(3):405–411.
- Mohamed AA, Radwan TA, Mohamed MM, et al. Safety and efficacy of addition of hyaluronidase to a mixture of lidocaine and bupivacaine in scalp nerves block in elective craniotomy operations; comparative study. BMC Anesthesiol. 2018;18(1):129–137.
- Subramanyam R, Vaishnav V, Chan VW, et al. Lateral versus medial needle approach for ultrasound-guided supraclavicular block: a randomized controlled trial. Reg Anesth Pain Med. 2011;36(4):387–392.
- Kim TW, Lee JH, Yoon KB, et al. Allergic reactions to hyaluronidase in pain management-A report of three cases. Korean J Anesthesiol. 2011;60(1):57–59.
- Kallio H, Paloheimo M, Maunuksela E-L. Hyaluronidase as an adjuvant in bupivacaine-lidocaine mixture for retrobulbar/peribulbar block. Anesth Analg. 2000;91(4):934–937.
- Yousef AAAM, EL‐deen AS, Al‐deeb AE. The role of adding hyaluronidase to fluoroscopically guided caudal steroid and hypertonic saline injection in patients with failed back surgery syndrome: a prospective, double‐blinded, randomized study. Pain Pract. 2010;10(6):548–553.
- Keeler J, Simpson K, Ellis F, et al. Effect of addition of hyaluronidase to bupivacaine during axillary brachial plexus block. Br J Anaesth. 1992;68(1):68–71.
- Kamal Hakim KY, Ahmed MA. Effect of addition of hyaluronidase as an adjuvant to local anesthetics in ultrasound-guided supraclavicular brachial plexus block. Ain-Shams J Anaesthesiol. 2017 Jan 1;10(1):213–218.