ABSTRACT
Introduction: Postoperative delirium is a common complication of cardiac surgery. This study aimed to assess the effect of supplementing dexmedetomidine infusion with oral melatonin in prevention of postoperative delirium after coronary artery bypass graft surgery.
Methods: 110 patients of both sexes above 60 years of age were included. Anesthetic management was standardized. Patients were randomly allocated into one of the two study groups, dexmedetomidine/melatonin (DM) group or dexmedetomidine (D) group. Patients in the DM group received oral Melatonin tablet 5 mg the night before surgery and same dose was repeated every 24 hours for 3 postoperative days. After completion of surgery and upon ICU arrival, patients in both groups received a bolus of 0.4 µg/kg dexmedetomidine followed by 0.2–0.7 µg/kg/h infusion, for 24 maximum hours. Delirium was assessed for 5 days postoperatively at 12 hr intervals using confusion assessment method (CAM) for ICU and after discharge from ICU to surgical ward using CAM. Delirious patients were treated with IV haloperidol.
Results: No significant differences between studied groups regarding baseline, preoperative, intraoperative and postoperative characteristics. Incidence of delirium was significantly lower, onset significantly more delayed, and duration was significantly shorter in group-DM as compared to group-D. No significant differences between all cases, cases who had delirium, and cases who did not have delirium in the two groups as regards extubation time, ICU stay, and hospital stay.
Conclusion: supplementing dexmedetomidine with melatonin decreases incidence, delays onset, and shortens duration of postoperative delirium in patients above 60 years of age undergoing CABG surgery.
1. Introduction
Delirium is a serious brain illness, which commonly presents with a sudden onset (e.g., hours to days) of altered level of consciousness and clouded sensorium of relatively short duration. It is marked by disorganized thinking, with irrelevant or incoherent speech. There may also be sensory misperceptions; disturbance of sleep-wake cycle and level of psychomotor activity; disorientation to time, place, and person; and memory impairment [Citation1].
Postoperative delirium is a common complication of cardiac surgery and is associated with increased mortality, morbidity, and long-term cognitive dysfunction [Citation2].
A meta-analysis of 14 trials which randomized 3,029 patients showed that use of dexmedetomidine was associated with significant reductions in incidence of delirium, agitation and confusion [Citation3].
Melatonin is a neurohormone secreted into the bloodstream in a circadian pattern by the pineal gland. It accelerates initiation of sleep and improves maintenance and efficiency of sleep. Most of critically ill patients have an altered sleep pattern, abnormal levels of melatonin, and loss of circadian rhythms. Melatonin has a major role in control of circadian rhythm and sleep regulation [Citation4].
The aim of this study was to assess effect of supplementing dexmedetomidine infusion with oral melatonin in prevention of postoperative delirium after coronary artery bypass graft surgery.
2. Methods
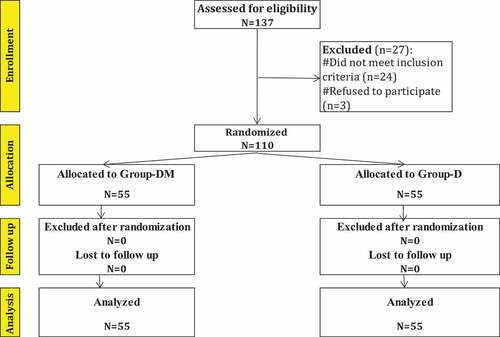
After approval of the Research Ethics Committee, this prospective, randomized controlled clinical trial was conducted on 110 patients undergoing elective coronary artery bypass graft (CABG) surgery. Those patients were selected out of 137 patients studied for eligibility criteria and for consenting to participate in the study (). The study included patients of both sexes above 60 years of age. An informed written consent was taken from all patients during the preadmission anesthesia clinic visit. Exclusion criteria included patients undergoing emergency procedures, any preoperative mental illness, preoperative renal failure, patients diagnosed with chronic liver disease (Child classification class B and C), patients diagnosed by carotid duplex to have carotid disease, patients with prolonged postoperative intubation and re-exploration (those patients were replaced by other patients to maintain the number of patients in each group).
3. Anesthesia and cardiopulmonary bypass
To minimize impact on outcome, the anesthetic management was standardized.
Midazolam was used before surgery with a maximum of 0.03 mg/kg. Induction of anesthesia was with incremental doses of fentanyl up to 10–12 ug/kg and incremental doses of propofol 0.5–2 mg/kg. Muscle relaxation was achieved by 0.6 mg/kg rocuronium followed by top-up doses during the surgery guided by the nerve stimulator. Maintenance of anesthesia was done using isoflurane 0.5–2%. Blood pressure and heart rate were maintained at around 20% of baseline values. Heparin was used for anticoagulation and maintenance of activated clotting time more than 480 s. The cardiopulmonary bypass circuit was primed with 1 L of Ringer’s Lactate and 250 ml of 20% mannitol. Membrane oxygenator (Medtronic Affinity NT) was used. During CPB temperature was lowered to 30–32°C and maintained at the same level, the pump flow rate 2.4–2.8 l/min/m2, and mean perfusion pressure was targeted between 60 and 80 mmHg. Increments of morphine and propofol were used to maintain anesthesia during CPB. Hematocrit was maintained within 25–35%, fractional concentration of inspired oxygen adjusted to keep oxygen partial pressure within 150–250 mmHg, and gas flow was adjusted to maintain arterial carbon dioxide tension within 35–40 mmHg. Intermittent antegrade and occasionally retrograde blood cardioplegia was given for myocardial protection. Rewarming to 36º-37°C was done before separation from CPB. Protamine sulfate 1 mg/100 U heparin was given after separation from CPB to reach activated clotting time within 10% of baseline. After surgery all patients were transferred to ICU.
3.1. Study drugs administration
Patients were randomly allocated into one of the two study groups, dexmedetomidine/melatonin (DM) group or dexmedetomidine (D) group. Patients in DM group received oral Melatonin tablet 5 mg at 10 PM the night before surgery and the same dose was repeated every 24 hours for 3 postoperative days. After completion of the surgery and upon ICU arrival, patients in both groups received a bolus of 0.4 µg/kg dexmedetomidine over 20 minutes followed by 0.2–0.7 µg/kg/h infusion, for 24 maximum hours. Bolus was omitted if the patient was hemodynamically unstable. The infusion was tapered to reach a minimum by the end of the 24 hours. Level of sedation was assessed using Riker Sedation Agitation Scale (SAS) [Citation5]. Dexmedetomidine infusion was titrated aiming for light sedation to have a calm and cooperative patient (SAS score 4). Assessment was done every 2 h (more often if patient’s condition changed).
3.1.1. Study endpoints
Delirium was assessed preoperatively (baseline) and for 5 days postoperatively at 12 hr intervals or as needed by using confusion assessment method (CAM) for ICU and after discharge from ICU to surgical ward using CAM [Citation6]. Patients are either CAM Positive or CAM negative. Patients were considered delirious until CAM is negative. The CAM-ICU includes a four-step algorithm identifying:
(1) Acute onset of changes or fluctuations in the course of mental status. To aid in the assessment of this point, patients were followed up daily with the Glasgow Coma Scale [Citation7] and Richmond Agitation Sedation Scale (RASS) [Citation8]. Any fluctuation during the prior 24-hour period in the patient’s Glasgow Coma Scale or RASS scores is used to indicate a positive mental status.
(2) Inattention. To aid the assessment of inattention, an Attention Screening Examination (ASE) [Citation9], which included a visual recognition component and an auditory recognition component was used. The cut point for presence of inattention was rated as present if the patient scored less than 8 correct answers on either the visual or auditory components of the ASE.
(3) Disorganized thinking. Assessment of disorganized thinking was done by adding four questions and three commands. Disorganized thought was said to be present if the patient was unable to answer at least three of the four questions correctly and could not complete commands.
(4) An altered level of consciousness. An altered level of consciousness is considered if the patient had anything other than alert, as being vigilant or lethargic or in a stupor or coma using the standardized definitions mentioned in the score.
Patients were considered delirious in the presence of features: (1) and (2) plus either (3) or (4).
If the delirious patient was agitated, the infusion rate of dexmedetomidine was increased. Patients with severe agitation were treated with IV haloperidol in 1–5 mg increments every 30–60 min as needed.
The following measurements were made:
Patients’ demographics
Surgery related characteristics
Frequency of delirium
The onset of delirium
Duration of delirium
Haloperidol use
Extubation time
Length of ICU stay
Length of hospital stay
3.2. Statistical analysis
Setting the power = 0.80 and ∝ = 0.05 with using PASS 11th release, a minimal sample size of 55 cases in each melatonin-containing and non-melatonin-containing group was required difference to get statistically significant between delirium frequencies of 8.0% and 28.0% respectively [Citation10].
4. Statistical methods
The collected data were coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013. Descriptive statistics were done for quantitative data as mean±SD (standard deviation) for quantitative normally distributed data and Median (1st−3rd interquartiles) for quantitative non-normally distributed data, while it will be done for qualitative data as number and percentage. Inferential analyses will be done for quantitative variables using Shapiro-Wilk test for normality testing, independent t-test in cases of two independent groups with normally distributed data, Mann Whitney test in cases of two independent groups with non-normally distributed data and paired t-test in cases of two dependent groups with normally distributed data. In qualitative data, inferential analyses for independent variables were done using Chi square test for differences between proportions and Fisher’s Exact test for variables with small expected numbers. Long Rank test was used to compare rate of delirium. The level of significance was taken at P value < 0.050 was significant, otherwise is non-significant.
5. Results
Figure 2. Kaplan Meier curve for delirium onset
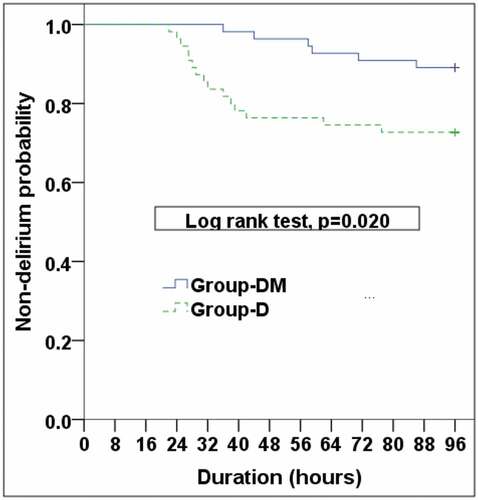
Figure 3. Kaplan Meier cure for delirium end
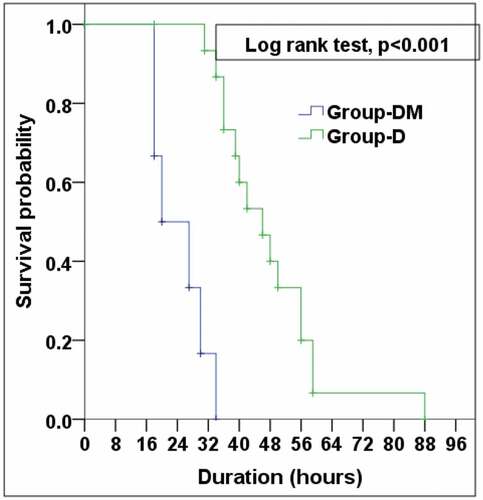
Table 1. Comparison according to baseline, preoperative, intraoperative and postoperative characteristics
Table 2. Comparison according to delirium characteristics and important times in the two groups
6. Discussion
There is a wide variation in the reported incidence of postoperative delirium depending on the methodological differences between the studies, mainly the used delirium diagnostic tools and the characteristics of the study populations. The incidence may reach up to 50–67% among patients undergoing cardiac surgery [Citation11].
A study on 142 elderly patients, 70 years old or more, who had routine cardiac surgery reported postoperative delirium in 54.9% of patients [Citation12].
In the current study, delirium was assessed using confusion assessment method (CAM) for ICU and after discharge from ICU to surgical ward using CAM.
The validation study of CAM-ICU demonstrated a sensitivity between 95% and 100% and a specificity between 89% and 93% [Citation13].
The results of the current study showed that the incidence of delirium was significantly lower, and the onset of delirium was significantly more delayed in patients who received melatonin and dexmedetomidine as compared to patients who received dexmedetomidine only. Delirium stayed for a highly significant duration in patients who received dexmedetomidine only as compared to patients who received melatonin and dexmedetomidine. In DM group, two out of six patients needed haloperidol and in group D, nine out of fifteen patients needed haloperidol. In both groups the other patients who developed delirium and didn’t need haloperidol (4/6 in DM group and 6/15 in D group) responded to increasing the dexmedetomidine infusion. There were no significant differences between all cases, cases who had delirium, and cases who did not have delirium in the two groups as regards extubation time, intensive care unit stay, and hospital stay.
The use of dexmedetomidine for the prevention of postoperative delirium was reported in several studies.
A study was conducted on 118 patients who had cardiac surgery and were randomly assigned to one of three postoperative sedation protocols: dexmedetomidine, propofol, or midazolam. The incidence of delirium was significantly lower in patients who received dexmedetomidine as compared to patients in the other two groups which were comparable. Patients who developed postoperative delirium experienced significantly longer ICU stays and longer total hospitalization [Citation14].
Another prospective, randomized controlled trial was conducted on 183 patients 60 years or older undergoing cardiac surgery. Upon admission to ICU, patients received either dexmedetomidine or propofol. Assessment of delirium was performed at 12-h intervals during the five postoperative days. POD was present in 17.5% and 31.5% patients in dexmedetomidine and propofol groups, respectively. Median onset of POD was on postoperative day 2 versus 1, and duration of POD was 2 days versus 3 days, in dexmedetomidine and propofol groups, respectively [Citation15]. The incidence of delirium in this study was lower than our results (17.5% versus 27.3% respectively), however the onset and duration of delirium in patients who received dexmedetomidine were comparable to our results.
A third study randomized 164 patients 1:1 ratio to receive intravenous infusion of propofol with or without dexmedetomidine for general anesthesia maintenance during cardiac surgery. Upon admission to ICU, patients received propofol for postoperative sedation. Postoperative delirium (POD) was assessed every day during the first five postoperative days. There was no significance in incidence of POD between the dexmedetomidine group and the propofol group, 39.3% versus 26.3% respectively. In patients treated with dexmedetomidine, the median onset time of delirium was delayed (second day vs first day) and the duration of delirium reduced (2 days vs 3 days) when compared with propofol-treated patients [Citation16]. The incidence of delirium in this study was higher than our results (39.3% versus 27.3% respectively), however the onset and duration of delirium in patients who received dexmedetomidine were comparable to our results. The higher incidence of delirium in this study as compared to ours might be explained by the fact that in both groups propofol was used for postoperative sedation and it was shown in a previous study [Citation15] that postoperative sedation with propofol was associated with higher incidence of delirium than dexmedetomidine.
The lower incidence of postoperative delirium with the use of dexmedetomidine was also reported in adults more than 60 years old who had non-cardiac surgery. An example is a study that included 453 patients admitted to ICU after joint replacement surgery [Citation17]. Another example is a study that included 619 patients who had thoracoabdominal laparoscopic and open surgeries as well as spine surgeries [Citation18].
The results of the current study showed lower incidence, delayed onset, and shorter duration of delirium when dexmedetomidine infusion was supplemented with oral melatonin.
A study included two groups, 250 patients each, operated upon in a various elective or urgent cardiac surgery. Group A was control and group B patients received prophylactic perioperative melatonin 5 mg the evening before the operation, and the treatment was continued until postoperative day 3. Delirium developed in 20.8% patients from group A and 8.4% patients from group B, with the difference in incidence of delirium between the two groups being statistically significant (p = 0.001). Patients with postoperative delirium in both groups had a significantly longer stay in the ICU and a significantly longer total duration of hospitalization [Citation19]. The authors did not mention an explanation for this prolonged ICU and hospital stay in delirious patients. The incidence of delirium in this study was lower than our results (8.4% versus 27.3% respectively). In our study delirium did not prolong ICU or hospital stay. The differences between this study and our results may be explained by the fact this study included urgent cases and they used only melatonin without dexmedetomidine.
Another study was conducted to investigate the preventive and the curative effect of melatonin supplementation on postoperative delirium in elderly patients undergoing coronary artery bypass surgery. Fifty patients were allocated into two groups. Patients in melatonin group received 3 mg melatonin orally at 9 p.m. the night before surgery and another 3 mg melatonin with 15 ml of plain water 30 min before operation and 3 mg melatonin at 9 p.m. in the day of operation after weaning from mechanical ventilation and 9 p.m. the first three postoperative days. The use of prophylactic melatonin had succeeded to decrease the incidence of POD from 28% to 8%. The number of patients who were cured after melatonin therapy were 100% in melatonin group compared to 42.9% in control group [Citation10]. The incidence of delirium in patients who received melatonin in this study (8%) was comparable to our study (10.9%).
A more recent study on 140 patients undergoing CABG to assess the effect of melatonin on incidence of delirium in elderly patients included two groups of 70 patients each. In group 1, 3 mg/day oral melatonin was administered from three days before beginning of the intervention until three days after its completion. Group 2 received placebo for seven days. There was a significant difference in the frequency of the CAM-ICU result on the day of surgery and three days after surgery between the two groups, so that the delirium was lower in melatonin group [Citation20]. This is consistent with our results.
The lower incidence of delirium in older adults with the perioperative use of melatonin was reported in a meta-analysis that included six studies (number of patients = 1155). The mean age of patients in included studies ranged from 59 to 84 years. Patients in intervention groups typically received melatonin at daily doses of two to eight milligrams around cardiothoracic, orthopedic, or hepatic surgeries for one to nine days, starting on the evening before or the day of surgery. The incidence of delirium was significantly less in the groups that received melatonin [Citation21].
In conclusion, supplementing dexmedetomidine with melatonin decreases the incidence, delays the onset, and shortens the duration on postoperative delirium in patients above 60 years of age undergoing coronary artery bypass graft surgery.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Kroustos KR, Sweeney MA. Palliative care. In: Chisholm-Burns MA, Schwinghammer TL, Malone PM, et al., editors. Pharmacotherapy: principles & practice. 5th ed. New York (NY):McGraw Hill Education; 2019. p.31–42.
- Kots K, Szylinska A, Listewnik M, et al. Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;13:1061–1070.
- Pasin L, Landoni G, Nardelli P, et al. Dexmedetomidine reduces the risk of delirium, agitation and confusion in critically ill patients: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. 2014;28:1459–1466.
- Bellapart J, Boots R. Potential use of melatonin in sleep and delirium in the critically ill. Br J Anaesth. 2012;108(4):572–580.
- Riker RR, Picard JT, Fraser GL. Prospective evaluation of the sedation-agitation scale for adult critically ill patients. Crit Care Med. 1999 July;27(7):1325–1329.
- Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286:2703–2710.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;1:81–84.
- Sessler C, Gosnell M, Grap MJ, et al. A new agitation-sedation scale (RASS) for critically ill patients: development and testing of validity and inter-rater reliability. Am J Respir Crit Care Med. 2000;161:A506.
- Hart RP, Levenson JL, Sessler CN, et al. Validation of a cognitive test for delirium in medical ICU patients. Psychosomatics. 1996;37:533–546.
- Sharaf SI, Nasr El-Din DA, Mahran MG, et al. A study of the prophylactic and curative effect of melatonin on postoperative delirium after coronary artery bypass grafting surgery in elderly patients. Egypt J Hosp Med. 2018;72(7):4919–4926.
- Norkienė I, Ringaitienė D, Kuzminskaitė V, et al. Incidence and risk factors of early delirium after cardiac surgery. Biomed Res Int. 2013;2013:323491.
- Smulter N, Lingehall HC, Gustafson Y, et al. Delirium after cardiac surgery: incidence and risk factors. Interact Cardiovasc Thorac Surg. 2013;17:790–798.
- Tomasi CD, Grandi C, Salluh J, et al. Comparison of CAM-ICU and ICDSC for the detection of delirium in critically ill patients focusing on relevant clinical outcomes. J Crit Care. 2012;27(2):212–217.
- Maldonado JR, Wysong A, van der Starre PJA, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50:206–217.
- Djaiani G, Silverton N, Fedorko L, et al. Dexmedetomidine versus propofol sedation reduces delirium after cardiac surgery, a randomized controlled trial. Anesthesiology. 2016;124:362–368.
- Shi C, Jin J, Qiao L, et al. Effect of perioperative administration of dexmedetomidine on delirium after cardiac surgery in elderly patients: a double-blinded, multi-center, randomized study. Clin Interv Aging. 2019;14:571–575.
- Xuan Y, Fan R, Chen J, et al. Effects of dexmedetomidine for postoperative delirium after joint replacement in elderly patients: a randomized, double-blind, and placebo-controlled trial. Int J Clin Exp Med. 2018;11(12):13147–13157.
- Li CJ, Wang BJ, Mu DL, et al. Randomized clinical trial of intraoperative dexmedetomidine to prevent delirium in the elderly undergoing major non-cardiac surgery. BJS. 2020;107:e123–e13.
- Artemiou P, Bily B, Bilecova-Rabajdova M, et al. Melatonin treatment in the prevention of postoperative delirium in cardiac surgery patients. Pol J Cardiothorac Surg. 2015;12(2):126–133.
- Kasnavieh FH, Rezaeipandari H, Hadadzadeh M, et al. Effect of melatonin on incidence rate of delirium in elderly patients undergoing open-heart surgery without a pump: a clinical trial. Elderly Health J. 2019;5(1):32–39.
- Campbell AM, Axon DR, Martin JR, et al. Melatonin for the prevention of postoperative delirium in older adults: a systematic review and meta-analysis. BMC Geriatr. 2019;19:272.