ABSTRACT
Background: Oxygenation failure one of the main covid-19 presentation in pandemic. Prone position (PP) and non-invasive ventilation (NIV) have been traditionally used in acute respiratory distress syndrome (ARDS) to improve oxygenation and avoiding invasive ventilation complications. Awake proning and noninvasive ventilation are being used as a therapy in COVID-19 hypoxic failure to improve outcomes.
Methods: A prospective study of 30 COVID patients admitted in our Hospital critical care isolation. Co-operative hemodynamically stable patients, SaO2 ˂90%, PaO2/FiO2 ˂200, respiratory rate ˃ 24, bilateral lung infiltration on CT chest into two groups (15 pts in each) Oxygen was administered through non-rebreathing mask(NRB) mask O210-15 L/min with awake PP or NIV for 1-2 h each session, 3 h apart during waking hours for the first 3 days. Primary target improve oxygenation (SaO2 > 95% and P/f > 200 mm Hg), avoid intubation. ICU days and hospital stay are the secondary end points. Other COVID therapies were used according to our hospital protocol.
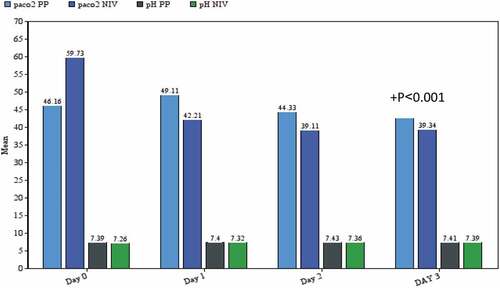
Results: The mean SaO2 at admission 79 ± 8.47% in PP, 82 ± 7.05% in NIV, after PP or NIV applying the mean saO2 and paO2 was significantly increased (mean SaO2 93 ± 5.9%, mean PaO2 107 ± 12 mmHg)PP, (mean sop2 95 ± 4.2%, mean PaO2 129 ± 11 mmHg) NIV, the mean pacO2 was decreased significantly in NIV (39.34 ± 5.12 mmHg) compare to PP (43.41 ± 3.2 mmHg) p value ˂0.001 with no significant results regarding the PH (7.40 ± 0.02&7PP group .33 ± 0.06 NIV group), ICU mortality 20% in each group in whom need intubation, with no significant value in ICU or hospital stay .
Conclusion: Awake prone positioning and non-invasive ventilation showed marked improvement in SaO2 and PaO2 in COVID-19 patients with improvement in clinical symptoms with reduced rate of intubation with superiority of NIV in hypercapnic patients.
1. Introduction
SARS-COV-2 disease 2019 (COVID-19) has rapidly spread round the world and has now become a worldwide public health crisis. COVID-19 mortality of in some European cities ˃11% and therefore the death rate is up to 61.5% in mechanically ventilated patients [Citation1]. The disease is spread through respiratory droplets and get in touch with fomites [Citation2]. Transmission mechanism has occasionally been implicated in patients with COVID-19 during procedures that are capable of generating aerosols [Citation3,Citation4]. Prone positioning(PP) may be a salvage therapy for refractory hypoxemia and has proven to be effective in increasing tidal volume and improving oxygenation and diaphragmatic function in patients with acute respiratory distress syndrome (ARDS) [Citation5].Non-invasive ventilation (NIV) is a method of respiratory support in which a mask easily applied and also easily disconnected from the patient. The harmful effects of the treatment of acute respiratory distress syndrome (ARDS) with invasive ventilation such as barotrauma and nosocomial pneumonia have led to deeper studies of NIV methods [Citation6,Citation7].We conduct this study to determine the advantages with PP or NIV in improving the oxygenation, decreasing the intubation rate, ward discharge and hospital stays in COVID19 patients.
2. Patients and methods
The present study was prospective randomized comparative conducted during the period from June 2020 to September 2020 at Qena University Hospital, COVID- 19critical care isolation, after approval from faculty of medicine and ethical committee. Written informed consent was obtained from the patient or his legal guardian of the patient. Using website software thirty eligible covid 19 patients were enrolled in the study if:hospitalized patient with a positive nasopharyngeal/oropharyngeal covid-19 swab is confirmed, ˃18 years old SaO2 ˂90% (5–10O2l/min simple face mask), PaO2/FiO2 ˂200, respiratory rate ˃ 24 b/m, bilateral lung infiltration in CT chest, not explained by cardiac failure and ready to co-operate pp or NIV. We excluded the patients with the subsequent criteria; need invasive and immediate ventilation, RR˃40b/m, use accessory muscle, systolic pressure ˂100 mmHg, unable or unwilling trail of PP and NIV. We illustrated the possible prone variations (arms could either be positioned at the side or abducted to less than 90 degrees at the shoulder and flexed), and NIV to the patients under study.
All the patients received high flow oxygen through nonrebreathing facemask (NRB) mask O2 10–15 l/min after randomization the patients divided into two groups awake PP group (15 patients) or NIV group (15 patients), each session last for 1 to 2 h according to patient to tolerability (either pp or NIV) with 3hs apart during waking hours, in the pp group the attendant physician leads the team to coordinate rolling the patient if needed with judicious use of pillows under the pelvis, caution should be maintained to ensure that lines and catheters do not get dislodged. Patients who could not tolerate prone positioning were allowed to interrupt and back to the supine position. NIV was performed using Bennett 840 ventilators initiated with CPAP of 10 cm H2O and PSV of 15 cm H2O and titrate to RR < 24/min, FIO2 at 0.6 and titrate to maintain SaO2 > 92% through a facemask with Full personal protective equipment PPE and N-95 masks for health-care providers, determination of effective mask ventilation is improvement in the O2 saturation and arterial blood gases follow up.).No sedation was used in this study for safety concerns.
If the patient deteriorated, i.e., P/F˂100 mmHg or SaO2˂90% at a Fio2 100% for at least 5 min but with respiratory distress worsen, altered sensorium, hypotension or shock endotracheal intubation and invasive ventilation were commenced.
Specific COVID-19 treatment was given to all or any patients consistent with our hospital protocol. Intra-arterial line was inserted for frequent blood gas monitoring. Vital signs [electrocardiogram (ECG), SaO2, noninvasive blood pressure (NIBP), rate of respiration, and temperature]were continuously monitored. Target for discharging from ICU was SaO2of >95% and PaO2/fiO2 > 200 on intermittent low flow O2 (nasal cannula3-5O2l/min)with improvement in clinical status (respiratory distress) at least 24 h.
Our primary end points were improved in oxygenation and avoiding intubation within the first 3 days of critical care admission (arterial blood gas at admission then daily after the procedure within the two groups for frequent 3 days).
Our secondary end points were reducing in ICU stay and hospital stay.
3. Statistical analysis
We calculated the sample size consistent with our hospital data for non intubated oxygen-dependent COVID 19 pneumonia as 8of 20 patients (40%) need critical care admission. Our recording data suggest that just one out of ten patients required intubation, calculations a total sample size 30;15 in each group indicated a confidence level 90% (α- error = 0.05,B-error = 0.2). Descriptive variables are expressed as percentage, mean and stander deviation (SD), or median and interquartile range (IQR), as appropriate for every variable. We used the student t test or Mann–Whitney test for numerical variables and chi-squared test or Fisher exact test for categorical variables, to match variables across the two group. Missing data weren’t imputed. Analyses were performed on an entire case analysis basis. All tests were two-sided, and a P -value < 0.05 was considered statistically significant. All analyses were performed with SPSS version 23.
4. Results
There is no significant difference in demographic characteristics and laboratory findings between the two group, 8 patients out of PP group,9 patients out of NIV group had no coexisting diseases, the mean SaO2 (on simple face mask 5–10 l/min) at admission 79 ± 8.47%in PP group, 82 ± 7.05% in NIV group (), O2 therapy started immediately after admission through NRB face mask 10–15 L/min to both group. After prone position or non-invasive ventilation applying the mean arterial blood oxygen saturation and tension was significantly increased mean SaO2 93 ± 5.9%, mean PaO2 107 ± 12 mmHg PP group (), mean SaO2 95 ± 4.2%, mean PaO2 129 ± 11 mmHg NIVgroup (), the mean arterial partial pressure of carbon dioxide was decreased significantly in NIV group paco239.34 ± 5.12 mmHg compare to PP group paco2 43.41 ± 3.2 mmHg (day3) p-value ˂0.001 () with no significant results regarding the PH7.40 ± 0.02 PP group,33 ± 0.06 NIV group ().
Table 1. Patient characteristics and outcomes of all patients who received awake prone position (PP) and invasive ventilation(NIV)
Figure 1. Mean oxygenation changes (SaO2%, PaO2mmHg, PacO2mmHg) through the first 3 days of ICU in prone position (pp)group
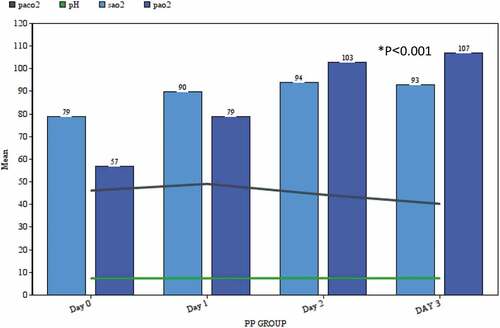
Figure 2. Mean oxygenation changes (SaO2%, PaO2mmHg,PacO2mmHg) through the first three days of ICU in noninvasive ventilation(NIV) group
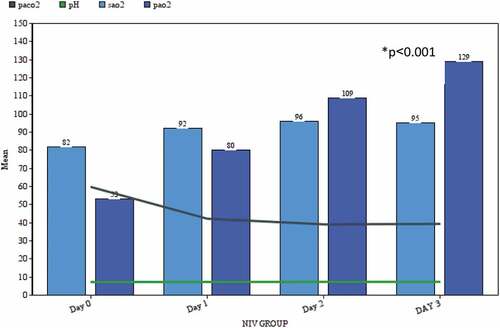
Figure 3. paco2mmHg &pH changes through the first three days in the two groups
80% from PP group had more than 50% bilateral pulmonary infiltration 73% NIV group. Three patients from each group requiring invasive mechanical ventilation with median time to invasive ventilation (20 ± 5hs PP group, 25 ± 8hs NIV group) due to haemodynamic instability with multiple organ dysfunction all had multiple coexisting diseases as (chronic obstructive pulmonary disease COPD, diabetes mellitus DM, obesity) and all eventually died (ICU mortality 20% in each study group), with no significant value regarding ICU or hospital duration of stay ().
5. Discussion
In this study, we were trying to determine the effect and advantages of two different and worldwide methods of treatment in covid19 pandemic in acute hypoxemic respiratory failure patients oxygen-dependent, we randomized 30 patients with different and multiple coexisting chronic diseases as (hypertension, DM, COPD,obesity) but with no other organ dysfunction or haemodynamic instability depended on only in PaO2/fiO2 PFR˂200 to awake PP or NIV as a strategy to avoid intubation and early ward discharge due to limited resources .
Other study considering awake PP in patients with SaO2 > 94% requiring either 0.3–0.6 FiO2 (with HFNC or NIV) or an oxygen flow rate of 2–10 L/min (with a face-mask or nasal cannulae). These oxygen requirements correspond to an SaO2/FiO2 range of 140–315 which approximates a PFR 100–300 mmHg, indicating mild to moderate ARDS(Citation8–11) [Citation9–11].
In our study, we found significantly improving in oxygenation through the days of study in both groups specifically in the survivor patients with no comorbidities (8 in PP group,9 in NIV group), the PP well establishes in classic ARDS as reduced ventilation perfusion mismatch (V/Q) due to its homogenous gas distribution [Citation12], but we found the superiority of NIV in the patient with comorbidities as (COPD&obesty) hypercapnic and inability to carry out work of breathing (paco2 39.34 ± 5.12 mmHg)p˂0.001 and normalizing metabolic status (pH33 ± 0.06) which decrease the need of invasive ventilation and ICU stay, this gives us abroad sight about covid 19 patient selection to a certain protocol in type II respiratory failure management or covid upgrading strains and mutation.
Practically speaking, many covid 19 cases with respiratory failure/hypoxaemia do not present symptoms of dyspnea (silent hypoxaemia), especially elderly patients [Citation13,Citation14] and their SaO2 is greatly affected by FiO2.patients with sever disease requiring high oxygen therapy and noninvasive positive pressure ventilation, so any method that improves oxygenation, survival rate and prevents lung injury should be considered.
The duration of a wake PP or NIV 1–2hs is tolerable to most of conscious and cooperative patients, the most reason for the patients’ intolerance of PP is discomfort, anxiety [Citation15], and therefore the inability to vary position. Our strategy was psychological care and a small change of position every 2 h in pp group and. Spontaneous modes are generally used with NIV to reinforce synchrony .Only Six patients with acute hypoxic failure transferred to invasive mechanical ventilation (20%in each group). Recent studies on the management of acute hypoxemic respiratory failure ARF in covid-19 pandemic have shown that the overwhelming majority need invasive MV with prolonged times on the ventilator [Citation16,Citation17]. Other studies used Alternatives simple technique with few side effects to invasive respiratory support like HFNO and awake-PP widely used during the pandemic to correct hypoxemia and avoid the necessity for invasive ventilation [Citation11,Citation18–21].
Thompson et al [Citation19]. during a similar population of 25 patients managed with conventional oxygen therapy found a heterogeneous response to awake-PP with improvements in SaO2 starting from 1 to37%, but 12 patients (48%) patients required intubation. Better results were found by Ng et al. [Citation20] who applied daily awake-PP sessions of 5 h in 10 non-ICU patients with just one needing intubation. Similar results were reported by Sartini et al. [Citation11] in 15 non-ICU patients supported with NIV in whom awake-PP was used as a rescue therapy, leading to an improvement of oxygenation and rate of respiration, and just one patient required intubation.
In our study, we use the target markers of the awake prone position or NIV effectiveness as changes in blood gas parameters: a rise in pH and a decrease in PacO2.We carefully observed the patients under the study for 1 to 2 h after instituting NIV, an increasing rate of respiration and recruitment of accessory muscles use would indicate high work of breathing, suggesting the necessity for intubation as the disadvantage of NIV is that the need for patient motivation [Citation22].
In a meta-analysis conducted by Muir, the NIV procedure was discontinued thanks to intolerance to patients with the presence of a mask in 37 of 747 cases (5%) [Citation23]. Fortunately, in our clinical practice, NIV is widely used which permit higher level of quality and patient comfortability. Analyzing current trends in NIV and HFNC usage altogether published series in major journals shows the subsequent mean NIV usage in hospitalized patients in China was 20.1% [Citation3,Citation24,Citation25]; in Italy 11 to %15; and in USA from 0 to 19% [Citation26,Citation27].
In the current study, all the patients who needed invasive ventilation died with rapid deterioration in their clinical and haemodynamic status duo to shock mainly sepsis with multiple organ failure with no difference between the two groups in time needed to intubation or mortality. Coppo et al. [Citation21] didn’t find any differences in time to intubation between responders and non-responders to awake-PP in their cohort of COVID-19 patients. In previous studies of corona virus disease in 2019 patients, severe acute hypoxaemic respiratory failure (AHRF) necessitates admission to an ICU for invasive mechanical ventilation with an associated mortality of >50% [Citation28–30].
6. Limitation
High-flow nasal cannula wasn’t available in our hospital which is very recommended.
Small sample size.
7. Conclusion
Prone positioning and NIV showed marked improvement in PaO2 and SpO2 in COVID-19 patients with superiority of NIV in those who were hypercapnic or inability to carry out work of breathing with improvement in clinical symptoms. In comparing both groups were decreased the rate of conversation of sever COVID 19 to critically ill and avoid invasive ventilation with no significant difference between the two groups.
Disclosure statement
No potential conflict of interest was reported by the author.
References
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481.
- Hui DS, Chow BK, Chu L, et al. Exhaled air dispersion during coughing with and without wearing a surgical or N95 mask. PLoS One. 2012;7(12):e50845.
- Tang JW, Li Y. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7(12):758.
- Yang W, Elankumaran S, Marr LC. Concentrations and size distributions of airborne influenza A viruses measured indoors at ahealth centre, a day-care centre and on aeroplanes. J R Soc Interface. 2011;8(61):1176–1184.
- Guérin C, Beuret P, Constantin JM, et al. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS prone position network) study. Intensive Care Med. 2018;44:22–37.
- Alraddadi BM, Qushmaq I, Al-Hameed FM, et al. Noninvasive ventilation in critically ill patients with the middle east respiratory syndrome. Influenza Other Respir Viruses. Saudi Critical Care Trials Group. 2019;13(4):382–390.
- Arabi YM, Fowler R, Hayden FG. Critical care management of adults with community-acquired severe respiratory viral infection. Intensive Care Med. 2020;46(2):315–328.
- Xu Q, Wang T, Qin X, et al. Early awake prone position combined with high-flow nasal oxygen therapy in severe COVID-19: a case series. Crit Care. 2020;24(1):250.
- Ding L, Wang L, Ma W, et al. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020;24(1):28.
- Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad Emerg Med. 2020;27(5):375–378.
- Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323(22):2338–2340.
- Telias I, Katira B, Brochard L. Is the prone position helpful during spontaneous breathing in patients with COVID-19? JAMA. 2020;323:2265–2267.
- Tobin MJ, Laghi F, Jubran A. Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med. 2020;202(3):356–360.
- Wilkerson RG, Adler JD, Shah NG, et al. Silent hypoxia: a harbingerof clinical deterioration in patients with COVID-19. Am J Emerg Med. 2020;S0735–6757(20):30390–30399.
- DiSilvio B, Young M, Gordon A, et al. Complications and outcomes of acute respiratory distress syndrome. Crit Care Nurs Q. 2019;42(4):349–361.
- Grasselli G, Zangrillo A, Zanella A. The COVID-19 Lombardy ICU network «baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581.
- Ferrando C, Suárez-Sipmann F, Mellado-Artigas R, et al. Main features, ventilatory management and outcomes of patients with COVID-19 inducedARDS. Intensive Care Med. 2020. DOI:10.1007/s00134-020-06192-2
- Elharrar X, Trigui Y, Dols A-M, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323:2336–2338.
- Thompson AE, Ranard BL, Wei Y, et al. Prone positioning in awak, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med. 2020;e203030. Online ahead of print. DOI:10.1001/jamainternmed.2020.3030
- Ng Z, Chiao W, Ho CHB. Awake prone position for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur Respir J. 2020;56(1):2001198.
- Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8:765–774.
- Hui DS, Hall SD, Chan MT, et al. Noninvasive positive-pressure ventilation: an experimental model to assess air and particle dispersion. Chest. 2006;130:730–740.
- Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426.
- Cheung JC, Ho LT, Cheng JV, et al. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8(4):e19.
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612–1614.
- Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Crit Care. 2020;24(1):154.
- Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099–1102.
- These data arise from the ICNARC Case Mix Programme Database. The Case Mix Programme is the national clinical audit of patient outcomes from adult critical care coordinated by the Intensive Care National Audit & Research Centre (ICNARC). For more information for the representativeness and quality of these data, please contactICNARC; [ cited 2020 May 15]. Available from: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061e9.
- Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region e case series. N Engl J Med. 2020;382:2012e22.
