ABSTRACT
Background: Sevoflurane unfortunately increases the cranial blood flow, blood volume, and pressure changes cope with cerebral aneurysmal neuroanesthesia goals. Propofol decreases the brain metabolism, blood flow, preserve cerebral reactivity to carbon dioxide, creates neuroprotective effect during cerebral ischemia. Hypothesis: Propofol-based total intravenous anesthesia would be more appropriate than sevoflurane-based inhalational technique during surgical clipping of cerebral aneurysm. Methods: A prospective, randomized, comparative study on 50 patients subjected for elective clipping of cerebral aneurysm, randomly allocated into two equal groups of 25 patients each: propofol-dormicum total intravenous only group and sevoflurane based inhalational group. Results: Jugular oxygen saturation (primary outcome), cerebral blood flow equivalent, heart rate, mean arterial blood pressure, and end tidal carbon dioxide tension were statistically significantly decreased in propofol group compared to sevoflurane group at basal, just after dura opening, at 1,2,3 hours later, and after scalp closure. Arterio-Jugular oxygen content difference, cerebral extraction ratio of O2, estimated cerebral metabolic rate for O2, serum lactate (mg/dl) showed significant increase in propofol group compared to sevoflurane group at basal, 1, 2, 3 h, and after scalp closure. Duration of surgery, time of recovery, blood loss, blood transfusion, intraoperative complications, urine output, total midazolam consumption, surgeon satisfaction, intensive care unit stay time, and Ramsay sedation scale difference was not significant in between both studied groups during the early postoperative period. Conclusion: Propofol based total intravenous anesthesia has better cerebral oxygenation and neuro anesthesia profile compared to sevoflurane-based inhalational anesthesia during cerebral aneurysm clipping surgery with systemic hemodynamic stability.
Introduction: Subarachnoid hemorrhage (SAH) leads to cerebrovascular vasospasm, cerebral irritation, high intracranial pressure (ICP) and re-bleed [Citation1] Complications result in disability and even death. Anesthesia Goals are stable systemic pressure and ICP, thereby adequate cerebral perfusion pressure (CPP), optimal oxygenation, normocarpia, and normothermia. Recovery and postoperative complication; hypertension, coughing, and ventilator asynchrony increase the chances of postoperative cerebral hematoma and edema. Fully awake recovery allows accurate neurological examination [Citation2].
Cerebral metabolism goes in parallel to cerebral blood flow (CBF) “flow metabolism coupling” [Citation3]. Increasing cerebral PaCO2 level causes vasodilatation and increases CBF. Decrease in CBF occurs during hypocapnia [Citation4]. Decreased arterial Oxygen tension (PaO2) below 50 mmHg cerebral vasodilatation occur and CBF increases. When arterial Oxygen tension (PaO2) decreases below 50 mmHg, cerebral vasodilatation occurs and CBF increases. The combination of arterial hypoxemia and hypercarbia exerts a synergistic effect, with an increase in CBF that exceeds the increase that would be produced by either factor alone [Citation5]. Oxygen delivery (DO2) = CBF x arterial Oxygen content (CaO2). If DO2 decreases the O2 extraction ratio increases consequently the jugular venous oxygen saturation (SjO2) will decrease results in reflex cerebral VD thus, CBF increases to improve the oxygen delivery [Citation6].
Jugular venous oxygen saturation (SjO2) values range from 55% to 70% [Citation6]. As long as CMRO2 and hemoglobin concentration remains relatively constant. The difference between arterial oxygen saturation (SaO2) and SjO2 will reflect CBF changes [Citation7]. If CMRO2 increases not associated with CBF elevation, the arterio-jugular oxygen content difference (CaO2- jO2) will increases concomitantly with cerebral oxygen extraction (CEO2). Oxygen content and saturation of the cerebral venous blood decreases, hence the SjO2 is an indicator of cerebral oxygen demand [Citation6].
Sevoflurane volatile anesthetic increases CBF, CBV, and ICP an effects which don’t cope with cerebral aneurysmal neuroanesthesia goals. Propofol IV anesthetic decreases cerebral metabolism, CBF and preserves the CO2 cerebral reactivity [Citation8,Citation9]. Propofol neuroprotective effect decreases the conductance of the voltage-activated sodium channel at the clinical range concentrations [Citation10]. Propofol combination with midazolam 15 min prior to ischemia decreases the neuronal damage induced by forebrain ischemia via GABAA-receptor-Clª channel complex in the brain [Citation11].
Hypothesis: High quality evidence regarding propofol or sevoflurane anesthesia in cerebral oxygenation during cerebral aneurysmal clipping is still lacking [Citation12]. In this present study; we hypothesized that propofol-midazolam based total intravenous anesthetics (TIVA) has more appropriate effect on cerebral oxygenation and metabolism than Sevoflurane based inhalational anesthesia and guarantee stable intraoperative hemodynamics and early smooth recovery in patients undergoing clipping of cerebral aneurysm.
Aim of the work: To evaluate the global cerebral oxygenation, cerebral hemodynamics as well as the systemic hemodynamic changes using propofol-midazolam-based total intravenous anesthetics (TIVA) in comparison with sevoflurane based inhalational anesthesia in clipping of cerebral aneurysm.
1. Material and methods
This prospective, randomized, comparative study carried out in the department of anesthesia Mansoura university hospital after Institutional research board (IRB) registration with a reference number (MD ⁄17.08.07 on 14/8/2017) and clinical trials.gov/registration code of NCT 03778723 on 16/12/2018.
This present study included fifty patients ASA I–II, of both gender and the aged 20 to 60 years old in the neurosurgery department subjected for elective clipping of cerebral aneurysm with fisher grading scale (1–3) [Citation13]. Patients with Glasgow coma scale score above 12 [Citation14].
Exclusion criteria: ASA physical status ≥ II or GCS ≤12, morbid obese patients, if sitting or prone position is a prerequisite for the surgery. Severe or uncompensated cardiovascular, renal, hepatic or endocrinal diseases, pregnancy, postpartum or lactating females, allergy to one of the drugs used, and lastly patient or his family refusal to sign the consent all were excluded from this present study.
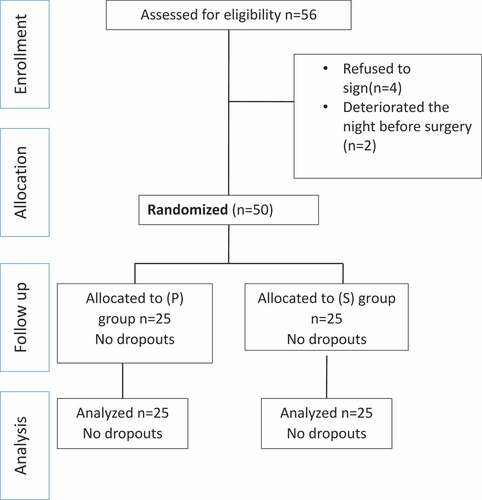
Fifty-six patients were enrolled and assessed for eligibility, of which four patient’s family didn’t accept to be a part of the study, and two other patients showed rapid deterioration the night before surgery (increased intracranial pressure) which necessitated emergency external ventricular drainage (EVD). Remaining 50 patients were randomly allocated by a computer-generated randomization table, and group assignments were concealed in sealed opaque envelopes into 2 equal groups; 25 patients each according to the maintenance technique of anesthesia: TIVA group (group P) and inhalational group (group S) [consort flow diagram ()].
Figure 1. Consort flow diagram
A day before surgery a signed informed written consent was obtained from the patient himself -if he can sign the consent- or from his 1st degree relatives (father, mother son, husband or wife), full medical history, clinical examination for manifestation of increased intracranial tension (ICP), GCS, Fisher grading, electrocardiogram (ECG) and full laboratory investigations including; complete blood picture (CBC), hepatic function tests, plasma creatinine, random blood glucose, prothrombin time and activity and INR. Patient fasting started 8 h prior surgery for solids and semisolids and 2 h for water.
The day of surgery; on arrival to the pre-anesthesia room, all patients were placed in supine position then a wide bore (18 G) intravenous cannula was inserted and 5 ml/kg of normal saline was infused. Prior induction of anesthesia by 10 min, all patients were received IV midazolam 0.05 mg/kg (Midathetic 5 mg/ml) and 1.5–2 µg/kg fentanyl while monitoring all vital parameters; noninvasive blood pressure (NIBP), pulse oximeter, and ECG.
Anesthesia induction& endotracheal intubation: According to the patient randomization, after mask preoxygenation with 100% O2, in TIVA group for 3–5 min, then IV bolus dose of 2 mg/kg Propofol (Propofol 1% Fresenius), and IV bolus dose of 0.5 mg/kg Atracurium muscle relaxant, then tracheal intubation was done with the appropriate sized cuffed endotracheal tube(female 7–7.5 mm & male 7.5–8 mm), in inhalational group; just before anesthesia induction, the face mask was removed and the circuit placed firmly against the bed linen with an open “pop-off” valve. The free gas flow of anesthesia machine was adjusted at 6 L/min oxygen, maximum sevoflurane (SEVOrane Abbott) delivery by adjusting the vaporizer at 8%. After reservoir bag evacuation and refilling 30-sec period of circuit priming, the patient was informed that sevoflurane has a definite pleasant odor that would not be irritant or annoying to his breathe. After ordering the patient to do forced exhalation, a tight face rubber mask over the mouth and nose (to residual volume) was placed then the patient was asked to take three maximum (vital capacity) breaths as previously learned that can be repeated as needed till loss of consciousness (tested by loss of lash& corneal reflex using a piece of cotton), then IV bolus dose of 2mic fentanyl plus IV bolus dose of 0.5 mg/kg atracurium (Atrabesylate 50 mg/5 ml) muscle relaxant, then tracheal intubation was done with the appropriate sized cuffed endotracheal tube(female 7–7.5 mm & male 7.5–8 mm).
Anesthesia Maintenance: Immediately after induction; TIVA group; using two syringe pump (B Braun syringe pump) one for propofol IV infusion (1.5–2 mg/kg/h using 50 ml syringe containing 50 ml Propofol 1% Fresenius) and the other pump for 0.12 mg/kg/h infusion midazolam (Midathetic 5 mg/ml). Inhalational group; sevoflurane 2–2.5%.
Both of the study groups were given repeated Fentanyl boluses of 50µ when needed (heart rate or mean arterial blood pressure increase more than 20% of the basal value). Atracurium was administered in both groups in incremental doses of 0.1 mg/kg, every 20 minutes to facilitate muscle relaxation and mechanical ventilation using volume-controlled mode utilizing Oxygen 30% in air mixture. Minute volume was modified to keep PETCO2 around 35 mmHg. Warm saline 0.9% and lactated ringer’s in equal volumes were infused to keep CVP around 5 mmHg. Blood was transfused aiming to keep Hb≥10 gm/dl and/or Hct around 30%. Mannitol (20%) 0.5–1 gm/kg during craniotomy, via central line, the whole mannitol volume was infused over 20 minutes.
Cannulation and Catheterization: Immediately after intubation, and under complete aseptic conditions; A)-The non-dominant hand radial artery (after modified Allen`s test) was cannulated using 20 G arterial catheter. B)-The right subclavian vein was cannulated with the suitable catheter then position confirmatory chest X-Ray was done. C)-The right internal jugular vein was cannulated using retrograde technique the Jugular bulb catheterization with confirmation of the catheter tip position using X-Ray (C-arm), at cricoid cartilage level while the patient head is neutral in the supine position, using Seldinger technique the right internal jugular vein was cannulated in the cephalic direction, the catheter through introducer to the jugular bulb, approximately at the mastoid process level [Citation15]. Extra cerebral blood mixing was prevented by strict catheter positioning as close to the jugular bulb roof as possible, catheter tip correct placement was confirmed by neck X ray. Lateral x ray film, the catheter tip should be above the disc of C1/C2 and tightly at skull base. Antoposterior view, catheter tip should lie between; atlanto-occipital joint space (Bi-mastoid level) cranially and the lower orbital margin level caudally. Reversal of the muscle relaxant effect: IV mixture of Neostigmine 0.05 mg/kg with Atropine 0.02 mg/kg was given to the patient at end of operation, then the endotracheal tube was removed and patient was transferred to neurosurgical intensive care.
2. Monitoring and sampling
2.1. Primary outcome: Jugular venous oxygen saturation (SjO2)
2.1.1. Secondary outcomes
Hemodynamics and O2 parameters: HR, NIBP, SpO2 (pulse oximetry), PETCO2 and CVP were monitored continuously and recorded just after intubation, then each 30 min. intraoperatively till 240-min surgical time.
Brain oedema score (subjective surgeon score): Brain relaxation noticed by surgeon was recorded at time of dural opening a grade of 1–3 [Grade 1: denoting brain bulging above the level of craniotomy, Grade 2: brain is at the level of craniotomy, Grade 3: brain is below the level of craniotomy].
Blood sampling for laboratory assessment: simultaneous radial artery and jugular bulb samples. For: arterial (blood gases analysis) (AVL, Compact3, rouch), Hb level and Hct (SysmexKX-21, rouch), serum lactate and Na+ & K+ Time: immediately after cannulation (basal), after opening dura, then after 1 h, After scalp closure.
3. Calculated parameter
1-Estimated cerebral metabolic rate for O2 (eCMRO2): [(Ca.O2-JO2) × Pa.CO2)/100, CaO2 = (Sa.O2 x Hb. x 1.34) + (0.003 x Pa. O2), Cjv.O2 = (Sjv.O2 x Hb x 1.34) + (0.003 x Pjv.O2), Pa.CO2 (arterial CO2 tension). [Citation16]
2-Cerebral, extraction ratio of O2 (CE. O2): SaO2 – SjvO2.
3-Cerebral Blood Flow equivalent (CBFe): 1/[CaO2 – CjvO], flow/metabolism index reciprocal of Arterio-jugular O2 content difference. [Citation17]
Other recorded parameters: Duration of surgery, urine output, blood loss volume, blood transfusion, total consumption of opioids intra operative, recovery time: (time from cessation of anesthetic infusion and the ability of self-oxygenation and ventilation) and surgeon satisfaction (poor, fair, good). Fisher grading scale; Grade 1: No bleeding, Grade 2: Thin or diffuse blood layer below 1 mm thickness, Grade 3: blood layer over 1 mm thickness in the vertical plane, Grade 4: Intra-cerebral or intra-ventricular clots diffuse or without basal cisterns bleeding].
Postoperative Parameters: Ramsay sedation score every 5 minutes after extubation till shifting to ICU unit [Citation18]. All patients were admitted to neurosurgical ICU minimum for 24 h of monitoring and follow up and postoperative complications recording.
Sample size calculation: Based on a pilot study done on 6 patients, calculation of this study power was done using G. Power program (3.0.10). A priory analysis with one-tailed t test for difference between two independent means as a statistical test with the difference between the SjvO2 as the primary outcome. The effect size was calculated as 1.02 (large effect size), α error was 0.05 and power (1-ß error) of 0.95 was used. The resulted a total sample size was 44 patients (22 per group). To compensate for dropouts and deviation from normality, 50 patients were enrolled and 25 patients for each group.
Statistical Analysis: Using SPSS windows program (statistical package for social scientists) version 21. The continuous data normality was judged with Kolmogorov-smirnov test. Chi-square or fisher exact test was used to test qualitative data represented in number and percent. Continuous variables were expressed in mean and SD (standard deviation) while the categorical one were presented as median and range. Unpaired student t test (for parametric) and mann whitney test (for non-parametric) were applied for intergroup comparison. For intragroup comparisons the paired student-t-test was used for comparison of the first result (basal) in each group with the other 3 results, pairwise, in jugular oxygen saturation, and the other calculated cerebral parameters. Statistical differences showing P (probability) value, ≤0.05, was recorded as significant.
4. Results
Patients demographic data showed no significant differences in between both groups ().
Table 1. Patients characteristics
As regard systemic hemodynamics as regard heart rate (), mean arterial blood pressure and PETCO2 () showed statistically significant decrease in (P) group compared to (S) group, however, SpO2 () and CVP () showed no significant difference in between both groups.
Table 2. Peripheral oxygen saturation (SpO2), mean arterial blood pressure, end tidal carbon dioxide
Figure 2. Heart rate
Figure 3. Central venous pressure (CVP)
Jugular oxygen saturation (SjO2) [primary outcome] showed significant decrease in propofol group compared to sevoflurane group at basal (after cannulation), just after dura opening, at 1,2,3 h later, and after scalp closure. p value 0.041, 0.049, 0.038, 0.005, 0.004, respectively. ()
Table 3. Jugular Oxygen saturation and the arterio-jugular oxygen content difference
Arterio-Jugular oxygen content difference (CaO2-jO2) showed significant increase in propofol group compared to sevoflurane group at basal (after cannulation), 1, 2, 3 h and after scalp closure with ().
Cerebral blood flow equivalent (CBFe) was significantly decreased propofol group compared to sevoflurane group at basal (after cannulation), after 1, 2, 3 h and after scalp closure P: <0.05 ().
Table 4. Cerebral blood flow equivalent (CBFe) & Serum Lactate (mg/DL)
Serum lactate (mg/dl) showed statistically significant increased values in group. (P) compared to group. (S) at 1, 2, 3 h and after scalp closure and significant increase compared to basal values at 1&2 h after cannulation in group (P) and at 1, 2 h and after scalp closure group (S). P: <0.05 ().
Estimated cerebral metabolic rate for O2 (eCMRO2) showed significant increase in group propofol compared to group sevoflurane during the whole study period. Group (P) was highly significantly increased compared to basal value later at scalp closure. Group (S) showed highly significantly increased compared to basal value after 1 h, and after scalp closure, P: <0.05, ().
Cerebral extraction ratio of O2 (CEO2%) showed significant increase in group. (P) compared to group. (S) at basal (after cannulation), after dura opening, 1,2,3 h later, and after scalp closure. P: <0.05, ().
Table 5. Cerebral extraction ratio of oxygen (CEO2) & Estimated cerebral metabolic rate for oxygen (eCMRO2) [ml/100 g/min]
As regard; duration of surgery (min), time of recovery (min), blood loss (ml), blood transfusion (ml), intraoperative complications (hypertension& arrhythmia), urine output (UOP) (ml), total intraoperative fentanyl dose (µg), surgeon satisfaction, ICU stay time (hours), and Ramsay sedation scale difference was not significant in between both studied groups during the early postoperative period as shown in ().
Table 6. Surgical information and ICU stay time
5. Discussion
Anesthesia goals in intracranial surgery include keeping adequate CPP to avoid cerebral ischemia, maintenance of; hemodynamic stability, cerebral metabolism, and cerebral oxygenation cerebral blood flow, in association with reduction of intracranial tension targeting optimal surgical circumstances (slack brain), as well as early emergence. [Citation19] No adequate research work validates a strong evidence of recommendation of a particular anesthetic approach as regard anesthesia for clipping of cerebral aneurysm.
As regard results of this present study; cerebral blood flow equivalent, jugular oxygen saturation, serum lactate, systemic hemodynamics (MAP, HR and PETCO2); showed significant decrease in propofol-based IV anesthesia technique compared to sevoflurane based inhalational anesthesia. On the other hand; estimated cerebral metabolic rate for O2, cerebral extraction ratio of O2, were significantly decreased with sevoflurane more than propofol-based anesthesia. Duration of surgery (min), time of recovery (min), blood loss (ml), blood transfusion (ml), intraoperative complications (hypertension& arrhythmia), urine output (UOP) (ml), total midazolam consumption (mg), surgeon satisfaction, ICU stay time (hours), and Ramsay sedation scale; all these variables were not significant in between both studied groups during the early postoperative period.
The choice of the anesthetic agents whether intravenous (TIVA) or inhalational in craniotomies has been always a matter of significant debates [Citation17,Citation20].
This present study TIVA group (P) compared to Inhalational group(S) showed; significantly decreased systemic hemodynamics (HR, MAP, and PETCO2) which can be attributed to one of two or both explanation; The 1st is the negative inotropic& chronotropic effects of Propofol itself. In line with our result explanation, Hino etal.,2019 [Citation21] who advised superiority of Thiopental over Propofol for avoiding hypotension during GA induction. Contrary to our hemodynamic results, Lauta E etal 2010 [Citation22] reported no significant hemodynamic differences with either propofol or sevoflurane. Far in opposition to our hemodynamic results, Bastola et al. 2015 [Citation23] also Citerio et al. 2012 [Citation24] reported lower arterial blood pressure with sevoflurane-based anesthesia compared with propofol-based anesthesia.
The 2nd explanation of the persistent significantly decreased hemodynamics during the whole study period in propofol group compared to Sevoflurane inhalational group; addition of midazolam infusion to propofol regimen in TIVA group which would potentiate and maintain the direct cardiac depressant effect of Propofol. Yang Gao et al., 2017 [Citation25] supported this explanation that midazolam can reduce the adrenergic but not affect renin or cortisol response to surgical stress, leading to systemic vascular resistance drop specially where it is already high as in hypertensive patients and those emotionally stressed prior to surgery.
Anesthetic regimen used for neuroanesthesia in addition to hemodynamic stability, should maintain CBF and reduce CMR without affecting autoregulation and cerebral blood flow/metabolism coupling [Citation26].
The primary outcome of this present study; Jugular venous bulb oxygen saturation (SjO2), clearly reflects [CBF/CMR.O2] ratio is an accurate method to detect CBF adequacy for cerebral metabolism [Citation27]. In this present study, SjO2 and consequently CBFe (1/CaO2- SjO2) were significantly decreased in the group (P) compared to (S) group. These finding indicate that both regimens of anesthesia; (TIVA and inhalational techniques) kept the balance between cerebral blood flow and cerebral metabolism, while the higher values in group (S) indicates limited increased flow or reduced cerebral metabolism compared to group (P).
Propofol-induced reduction of SjO2 was reported by Liao et al., 2010 [Citation28] who compared the effect of propofol/remifentanil versus sevoflurane anesthesia. Absence of SjO2 intragroup differences compared to basal values confirm stability of the flow/metabolism balance during both propofol and sevoflurane-based anesthesia, while the higher values in propofol group compared with sevoflurane group indicates limited decrease in flow or increase in metabolism.
Cerebral oxygen extraction (CEO2= SaO2 – SjvO2) judges the adequacy of cerebral blood flow to supply the brain metabolic needs. Flow reduction or metabolism augmentation would reduce SjVO2 and consequently increase CEO2 value. In this present study, CEO2 was significantly increased during propofol-based IV anesthesia compared to sevoflurane-based inhalational anesthesia, a result goes parallel to Liao et al., 2010 [Citation28]. As regard the Estimated cerebral metabolic rate O2 (eCMRO2) = [(Ca.O2-Jo2) × Pa.CO2)/100, Holmström and colleague 2005 [Citation29] reported that cerebral vasodilation effect of Sevoflurane is the least among other inhalation anesthetics. Conti et al, 2006 [Citation30] documented that Sevoflurane has a dose-dependent cerebral vasodilation and leads to dose-related increase in cerebral blood flow combined with its depressive effect on CMRO2, a fact goes in line with our results that revealed reduced CEO2 and CMRO2 in Sevoflurane inhalational anesthesia compared to propofol- based TIVA regimen, this could be explained by the higher depressive sevoflurane effect exerted on cerebral O2 tissue extraction leading to increases jugular venous O2 content and in turn reduces the eCMRO2, finding coincides with Molnár et al., 2007 [Citation31] results included decline in cerebral metabolism with sevoflurane based inhalational anesthesia.
As regard CBF and CMRO2 relationship; In the present study, propofol showed inverse proportion significantly decreased CBF while CMRO2 was significantly increased (both within the normal levels values) when compared to the sevoflurane inhalational group. Intragroup analysis of the propofol group showed CBF stability all through the study period, this can be explained by the fact that propofol reduces CBF 17% by both cerebral vasoconstriction and suppresses CMRO2. Propofol cerebro-vascular vasoconstriction and cerebral metabolic suppression effects relationship is still unclear; some studies have reported equivalency [Citation32] and others long time back have reported the dominance of vasoconstriction [Citation33]. On the other hand, as regard sevoflurane anesthesia-at a level of one MAC sevoflurane dose- Grathwohl K.W et al., 2008 [Citation34] reported a balance between the reduction in CMR and the increase in CBF while at MAC concentration over 1, and in parallel to our results, CBF increases and CMR value doesn’t change, in normal intracranial compliance the effect of sevoflurane on brain hemodynamics is trivial, so TIVA is more preferred in patients with unstable ICP or large lesions where disturbed flow/metabolism ratio occurs. One year later Matchett G.A et al., 2009 [Citation35] documented that Sevoflurane have GABA receptors agonistic effect, NMDA receptors antagonism, and glutamate reduction, results explained the sevoflurane CMR depressive effect while its regulation of nitric oxide synthetase production, and dose-dependent cerebral autoregulation effect can explain the augmented CBF in our study in sevoflurane group compared to propofol.
Rapid emergence from anesthesia is an essential goal in neuroanesthesia to allow early discovery of any neurological insults such as hematoma, cerebral herniation or cerebrovascular ischemia. In this present study, recovery times from anesthesia showed no significant difference in the two studied groups, in this study. These findings were confirmed by previous studies [Citation22,Citation26] comparing propofol TIVA and inhalation anesthesia. On contrary to these results, Castagnini et al., 2004 [Citation36] compared sevoflurane 1 to 3% with 60% nitrous oxide (N2O) in oxygen (O2), to propofol infusion dosing range of 4–10 mg·kg−[Citation1]·hr−[Citation1], he concluded that propofol has a relatively longer recovery period compared to sevoflurane based anesthesia and explained this with higher dose of propofol used which is still very high dose compared to the dose used in this present study.
Other tabulated variables, which may affect or indicate changes of neuroanesthesia profile, showed no significant differences between both of the present study groups. Duration of surgery (min), time of recovery (min), blood loss (ml), blood transfusion (ml), intraoperative complications (hypertension& arrhythmia), urine output (UOP) (ml), total intraoperative fentanyl dose (µg), surgeon satisfaction, ICU stay time (hours), and Ramsay sedation scale difference was not significant in between both studied groups during the early postoperative period as shown in ().
Conclusion: Propofol based TIVA has better neuroanesthesia profile, better cerebral oxygenation profile (lower Jugular oxygen saturation not only due to improved cerebral metabolic rate for oxygen but also improved cerebral extraction ratio of oxygen and wider arterio-jugular oxygen content difference), compared to Sevoflurane-based Inhalational anesthesia which improved Cerebral blood flow statistically during cerebral aneurysm clipping surgery both techniques guarantee systemic hemodynamic stability.
6. Limitations of the study
-Sitting and prone positions were excluded from this study. These positions are the most commonly accompanied with hemodynamic and ventilatory changes. These positions are really in need for careful choice and tailoring of the anesthetic regimen.
-Regaining cognitive functions and late post-operative complications were not examined in depth in this present study.
- Unavailability of bispectral index tool.
- Future studies should be designed to exclude the previous limitations.
Contribution Details (ticked marked as applicable):
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Kassell J. Aneurysmal subarachnoid hemorrhage: an update on the medical complications and treatments strategies seen in these patients. Curr Opin Anaesthesiol. 2011;24(5):500–507.
- Matta F, Heath J, Tipping K, et al. Direct cerebral vasodilatory effects of sevoflurane and isoflurane. Anesthesiology. 1999;91(3):677. . The Journal of the American Society of Anesthesiologists
- Frasco E, Croughwell D, Reves J. Cerebral blood flow and metabolism during cardiopulmonary bypass. Anesth Analg. 1993 Apr;76(4):849–865. .
- Albrecht F, Miletich J, Madala R. Normalization of cerebral blood flow during prolonged halothane anesthesia. Anesthesiology. 1983 Jan;58(1):26–31. .
- Goadsby J, Kaube H, Hoskin L. Nitric oxide synthesis couples cerebral blood flow and metabolism. Brain Res. 1992;595(1):167–170.
- White H, Baker A. Continuous jugular venous oximetry in the neurointensive care unit—a brief review. Can J Anaesth. 2002;49(6):623–629.
- Feldman Z, Robertson S. Monitoring of cerebral hemodynamics with jugular bulb catheters. Crit Care Clin. 1997;13(1):51–77.
- Shafer A, Doze A, Shafer L, et al. Pharmacokinetics and pharmacodynamics of propofol infusions during general anesthesia. Anesthesiology. 1988;69(3):348–356.
- Vandesteene A, Trempont V, Engelman E, et al. Effect of propofol on cerebral blood flow and metabolism in man. Anaesthesia. 1988;43(s1):42–43. .
- Deiner S. Highlights of Anesthetic Considerations for Intraoperative Neuromonitoring. SCVA Journal. 2010;14(1):51–53.
- Zhou 1, Li C, Yu M, et al. Neuroprotection of gamma-aminobutyric acid receptor agonists via enhancing neuronal nitric oxide synthase (Ser847) phosphorylation through increased neuronal nitric oxide synthase and PSD95 interaction and inhibited protein phosphatase activity in cerebral ischemia. J Neurosci Res. 2008;86(13):2973–2983.
- Kamath K, Venkataramaiah S. Concerns and challenges during anesthetic management of aneurysmal subarachnoid hemorrhage. Saudi J Anaesth. 2015 Jul-Sep;9(3):306–313. . 2015
- Jiménez L, Alén F, Gómez A, et al. Volumetric analysis of subarachnoid hemorrhage: assessment of the reliability of two computerized methods and their comparison with other radiographic scales. J Neurosurg. 2013;118(1):84–93. .
- Ahmed N, Kuo H. Evaluating the outcomes of blunt thoracic trauma in elderly patients following a fall from a ground level: higher level care institution vs. lower level care institution. Eur J Trauma Emerg Surg. 2019. DOI:10.1007/s00068-019-01230-1.. Received 2019 Jun 18. /Accepted: 3 September 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019
- Willeford L, Reitan A. Neutral head position for placement of internal jugular vein catheters. Anaesthesia. 1994 Mar;49(3):202–204.
- Jaggi L, Cruz J, Gennarelli A. Estimated cerebral metabolic rate of oxygen in severely brain-injured patients: a valuable tool for clinical monitoring. Crit Care Med. 1955;23(1):66–70.
- Ghoneimy E, Regal M, El-Tahan M, et al. Changes in cerebral oxygenation in patients with pulmonary dysfunction after lung resection. Semin Cardiothorac Vasc Anesth. 2013;17(1):72–81.
- Ramsay M, Savege T, Simpson B, et al. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2(5920):656–659.
- Elsayed A AA, Anthony S, Wehby N, et al. Anesthetic Management of Patients with Intracranial Aneurysms. Ochsner J. 2014;14(3):418–425.
- Guo Y, Fang Y, Xu R, et al. Effects of propofol versus sevoflurane on cerebral oxygenation and cognitive outcome in patients with impaired cerebral oxygenation. 2016;12:81. Journal of therapeutics and clinical risk management.
- Hino H, Matsuura T, Kihara Y, et al. Comparison between hemodynamic effects of propofol and thiopental during general anesthesia induction with remifentanil infusion: a double-blind, age-stratified, randomized study. J Anesth. 2019;33(4):509–515.
- Lauta E, Abbinante C, Del-Gaudio A, et al. Emergence times are similar with sevoflurane and total intravenous anesthesia: results of a multicenter RCT of patients scheduled for elective supratentorial craniotomy. J Neurosurg Anesthesiol. 2010;22(2):110–118. .
- Bastola P, Bhagat H, Wig J. Comparative evaluation of propofol, sevoflurane and desflurane for neuroanaesthesia: a prospective randomised study in patients undergoing elective supratentorial craniotomy. Indian J Anaesth. 2015;59(5):287–294.
- Citerio G, Pesenti A, Latini R, et al. A multicentre, randomised, open-label, controlled trial evaluating equivalence of inhalational and intravenous anaesthesia during elective craniotomy. Eur J Anaesthesiol. 2012;29(8):371–379. .
- Gao Y, Kang K, Liu H, et al. Effect of dexmedetomidine and midazolam for flexible fiberoptic bronchoscopy in intensive care unit patients. A retrospective study. Medicine (Baltimore). 2017;96(25):e7090.
- Magni G, Baisi F, La-Rosa I, et al. No difference in emergence time and early cognitive function between sevoflurane-fentanyl and propofol-remifentanil in patients undergoing craniotomy for supratentorial intracranial surgery. J Neurosurg Anesthesiol. 2005;17(3):134–138. .
- Steiner LA, Andrews PJ. Monitoring the injured brain: ICP and CBFL. Br J Anaesth. 2006;97(1):26–38.
- Liao R, Li J, Liu J. Volatile induction/maintenance of anaesthesia with sevoflurane increases jugular venous oxygen saturation and lumbar cerebrospinal fluid pressure in patients undergoing craniotomy. Eur J Anaesthesiol. 2010;27(4):369–376.
- Holmström A, Åkeson J. Sevoflurane induces less cerebral vasodilation than isoflurane at the same A‐line® autoregressive index level. Acta Anaesthesiol Scand. 2005;49(1):16–22.
- Conti 1, Iacopino G, Fodale V, et al. Cerebral haemodynamic changes during propofol-remifentanil or sevoflurane anaesthesia: transcranial Doppler study under bispectral index monitoring. Br J Anaesth. 2006;97(3):333–339.
- Molnár C, Settakis G, Sárkány P, et al. Effect of sevoflurane on cerebral blood flow and cerebrovascular resistance at surgical level of anaesthesia: a transcranial Doppler study. Eur J Anaesthesiol. 2007;24(2):179–184. .
- Oshima T, Karasawa F, Satoh T. Effects of propofol on cerebral blood flow and the metabolic rate of oxygen in humans. Acta Anaesthesiol Scand. 2002;46(7):831–835.
- De-Hert S, Sevoflurane MA [v1; ref status: indexed] http://f1000r.es/57cF1000 Research 4 (F1000 Faculty Rev) (2015):626. doi: 10.12688/f1000research.6288.1.
- Grathwohl W, Black H, Spinella C, et al. Total intravenous anesthesia including ketamine versus volatile gas anesthesia for combat-related operative traumatic brain injury. Anesthesiology. 2008;109(1):44–53. . The Journal of the American Society of Anesthesiologists
- Matchett A, Allard W, Martin D, et al. Neuroprotective effect of volatile anesthetic agents: molecular mechanisms. Neurol Res. 2009;31(2):128–134.
- Castagnini E, Van F, Salevsky C, et al. Sevoflurane for interventional neuroradiology procedures is associated with more rapid early recovery than propofol. Can J Anaesth. 2004;51(5):486.
