ABSTRACT
Background
knee osteoarthritis is considered as one of the most important causes of knee pain. Conventional noninvasive lines of treatment are several, including platelet-rich plasma (PRP) that has been revealed to be helpful in the management of knee osteoarthritis. The goal of this study is to appraise the PRP ultrasound-guided injection in the management of knee osteoarthritis.
Settings and Design
This study was a prospective randomised double blind study.
Methods
Sixty adult knee osteoarthritis patients were involved in the current study. They were randomly selected from the pain clinic Faculty of Medicine, Alexandria University. There were two groups ultrasound-guided (USG) pulsed waves radiofrequency (PRF) ablation on genicular nerve (group 1) or intra-articular PRP (group 2) injection under ultrasonography (US)-guidance and articular surface RF ablation. Assessment was done applying visual analogue scale (VAS) for pain intensity. Functionally, WOMAC and IKDC scores were used at baseline and 6th month after injection.
Results
Intra-articular PRP (group 2) showed a significant improvement in pain severity and physical limitations in patients with knee pain. It also showed significant improvement compared to genicular nerve RF considering VAS score with p value (0.012*) up to 12 months follow up, WOMAC, IKDC scores with p value (<0.001*) up to 12 months and US joint assessment with p value (0.028*) up to 6 months follow up.
Conclusion
The use of US IA-PRP injection combined to pulsed radiofrequency ablation of articular surface show significant improvement in pain compared to the genicular nerve PRF.
1. Introduction
Osteoarthritis (OA) is a debilitating joint disease that causes damage to the articular cartilage and underlying bone [Citation1], it has multifactorial etiopathogenesis that is characterized by the gradual disappearance of articular cartilage, osteophyte formation, subchondral bone alteration, and aseptic synovitis. Approximately, 85% of the individuals over the age of 75 years of age in Egypt experience some symptoms of OA, 40% of the population with the disorder experience significant difficulties with daily activities to the point of interfering with work-related or social roles [Citation2]. Available therapy for OA can be labelled into three groups: pharmacologic, non-pharmacologic/nonsurgical (e.g. physiotherapy and occupational therapy, rehabilitation) and surgical therapies. The sequence of treatment application begins with drug therapies and ends with surgical therapies [Citation3].
Radiofrequency ablation (RFA) is a minimal invasive non-operative method that utilizes thermal energy ablation or wear off pain-transmitting nerve fibers. The RFA reduces or permanently decreases the transmission of painful information to the brain from the knee [Citation4].
PRP is an own patient concentrated platelets derived from his own blood aiming to stimulate tissue regeneration through the local injection of a medium of platelet-derived mitogenic growth factors and bioactive promoting molecules [Citation5]. PRP contains a complex and diverse milieu of chemical mediators that interact with endogenous cells within the joint [Citation6]. Platelets provide a growth factors (i.e., platelet-derived growth factor [PDGF]) that escalate the exhibition of stem cells. This feature gave platelets an exquisite future in OA management.
IKDC is a non-objective knee assessment model that is calculated by the summation of the score for separate items and then converting the score to a scale that vary from 0 to 100. This score is to determine recovery or worsening in manifestations, joint function, and daily activities due to knee disability. It is formed of three sections: 1) Grade symptoms, involving stiffness, pain, swelling, locking in, and giving way; 2) sports activities; and 3) The present knee function and the previous knee function. [Citation7].
WOMAC takes about twelve minutes to be finished, and can be done on paper, using phone call or computer. Both the computerized and the mobile versions of the test have been found to be comparable to the paper form, with no significant difference. The questions are plotted on a scale from 0 to 4 that correlate with: (0) No symptoms, (1) Mild, (2) Moderate, (3) Severe, and (4) Extreme. Higher scores on the WOMAC point to more pain, inflexibility, and restricted joint function [Citation8].
The primary outcome in the current study was to weigh the efficacy of USG genicular nerve RF ablation versus USG intra-articular RF ablation of knee joint combined PRP injection in knee osteoarthritis pain relief measured by visual analogue scale. While the secondary outcome was to compare between both techniques as regards safety, duration, functional capacity, complications and adverse events.
2. Patients and methods
Following the verification of the community Ethics Committee of the faculty of medicine and having an informed written consent from every patient included in the study, the present study was carried out in Alexandria University Hospitals from June 2019 to July 2020 on sixty patient, the sample size was determined using Chi-square test power analysis known to have symptomatic knee osteoarthritis resistant to conventional treatment for more than 6 months and planned for pain management. The knees were at random allocation into two equal groups using closed envelope technique. Group I (n = 30) knees, which received (USG) pulsed waves (RF) ablation on genicular nerve. Group II (n = 30) knees, which received (USG) intra-articular-pulsed waves (RF) ablation combined with (PRP) injection.
Exclusion criteria were patients who have a past history of knee operation, septic inflammatory findings, autoimmune and connective tissue diseases involving the knee joint, major psychopathological disease or neurological disorder counting sciatic, coagulopathy or patients on anticoagulant drugs, patients who received intra-articular steroid within 1 month or hyaluronic acid injection within the previous 3 months, recent intake of nonsteriodal anti-inflammatory drugs (NSAIDs) within 3 days or aspirin within 7 days.
3. Methods
3.1. Patient assessment
Patients have a visit to pain clinic 3 days before the procedure for general examinations, review their medical and surgical history, pain assessment for base line values and for assessment of the degree of osteoarthritis using Kellgren Lawrence radiographic grading system [Citation9].
3.2. Genicular nerve pulsed radiofrequency ablation
Ultrasound scanning of the knees was performed by the investigator using a 12–5 MHz linear transducer (LOGIQ E Portable; GE Healthcare, US). The examination of the genicular nerves superior and inferior on medial aspect of knee joint using ultrasound was performed in accordance with the study of Yaşar et al [Citation10]. The pathway of the (SMGN) is that it is circling the femur bone shaft and in between the adductor magnus tendon and the femoral medial epicondyle, then goes down about 1 cm in front of adductor tubercle. IMGN is located parallel and encircling the tibial medial epicondyle and below the medial collateral ligament at the center between the medial collateral ligament tibial insertion and the tibial medial epicondyle. The anatomic landmarks for ultrasound was the adductor tubercle for the SMGN and the tibial collateral ligament was used for the IMGN. The midpoint of the bony cortex between the summit of the tibial medial epicondyle and the early fibers inserting on the tibia of the tibial collateral ligament was selected for the injection of the IMGN. A 22-gauge 8.9 cm BD with Quincke Point needle was introduced along with the long axis of the transducer (in-plane approach). 2 mL lidocaine 1% were then injected into each area as a therapeutic test. A 10 cm 22-gauge RF cannula (NeuroTherm; Abbot, US) was advanced to the specific target points until the needle reached the bone. The RF probe was positioned perpendicular to the supposed length of the targeted nerve. Sensory stimulation with 50 Hz-frequency and a threshold of < 0.6 V was applied. While the sensory stimulation, the patients were questioned if they perceived prickle or tingling, discomfort inside the knee or pain. The RF probe was kept in its position till one of those senses were evoked. Furthermore, motor stimulation with 2 V was applied with a frequency of 2 Hz to exclude the presence of fasciculation. eventually, RF lesions were created using PRF treatment to the superior and inferior medial genicular nerves for about 120 seconds twofold at 42°C [Citation11].
3.3. Intra-articular PRP injection and radiofrequency ablation
All procedures was carried out under local anesthesia, in operation room. The skin was palpated to localize the anterior patellar region with the knee angled at 30–45 degrees. The patella was visualized using a 5–10 MHz linear probe in a trans-axial anatomical plane. The transducer was moved proximally until the patella was no longer visualized. After the best ultrasound image was gained in this location, the skin was marked on the probe position. Using strict aseptic procedure (skin sterilization, ultrasound transducer covering, and sterile ultrasound gel). Local anesthesia was obtained with lidocaine using a 25-gauge 10 cm needle under live ultrasound guidance from a lateral to medial transverse approach [Citation12]. Then, moved along the same needle track, 10 cm a 22-gauge Quincke needle was inserted into the knee joint under real-time ultrasound imaging. 2 mL 1% lidocaine were injected inside the joint while observing the suprapatellar pouch filling in real time. RF introducer cannula 10 cm 22-gauge with a stylet that was placed intra-articularly in two planes through a predefined area. After a successful placement, the stylet in the introducer was pulled out and RF probe was inserted via the introducer needle. Subsequently, PRF was activated for 15 minutes with 42°C degree and a pulse span of 20 milliseconds, at 2 Hz. Then 20 ml PRP were injected intra-articular using another entry site using ultrasound guide. The patients’ evaluation were done in a prospective manner from patient baseline value, at the end of the treatment, follow-ups 3, 6 and 12 months later.
Using VAS, WOMAC [Citation8], IKDC [Citation7] scores for pain assessment and to measure joint function and life style improvement also joint assessment using US knee score [Citation13] to measure joint structure after each intervention scheduled 3, 6, 12 months interval and compare with base line.
Patient were advised to have a rest for 2 days and avoid using joint excessively with puncture site care and to inform any joint abnormality especially sings of inflammation.
3.4. Statistical analysis
Sample size was statistically approved by using Chi Square-test (PASS program version 20) a minimal total hypothesized sample size of 50 patient (25 per group) is needed to detect an assumed average proportional difference in the WOMAC between group (I) and group (II) taking in consideration that the level of significance is 5% and 80% power. [Citation14]
Data were fed to the IBM SPSS software using computer and analyzed by package version 20.0. (Armonk, NY: IBM Corp) Qualitative data were expressed using number and percent. The Kolmogorov-Smirnov test was applied to confirm the normality of distribution Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level.
The used tests were Chi-square test For categorical variables, to compare between different groups, Student t-test For normally distributed quantitative variables, to compare between two studied groups, ANOVA with repeated measures For normally distributed quantitative variables, to compare between more than two periods or stages, and Post Hoc test (Bonferroni adjusted) for pairwise comparisons, Mann Whitney test For abnormally distributed quantitative variables, to compare between two studied groups, Friedman test For abnormally distributed quantitative variables, to compare between more than two periods or stages and Post Hoc Test (Dunn’s) for pairwise comparisons.
4. Results
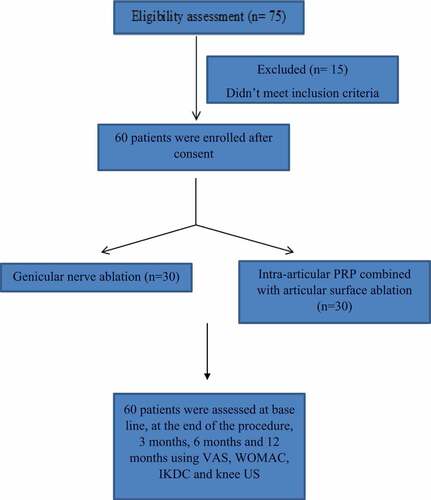
75 cases were screened for eligibility to be involved in current study and 60 patients subsequently were enrolled in the study, with no patient drop-outs (). Of the 60 patients, 30 received pulsed radiofrequency ablation on the genicular nerve (group I) and the other 30 patient received intra-articular knee joint PRP combined with radiofrequency ablation of the articular surface.
No significant difference was observed in demographic and baseline characteristics as comparing the two groups ().
Table 1. Comparison between the two studied groups according to demographic data
Table 2. Comparison between the two studied groups according to VAS
Table 3. Comparison between the two studied groups according to WOMAC, IKDC and knee joint score
No significant difference was found as regards BMI and duration of pain and grade of osteoarthritis in the studied groups.
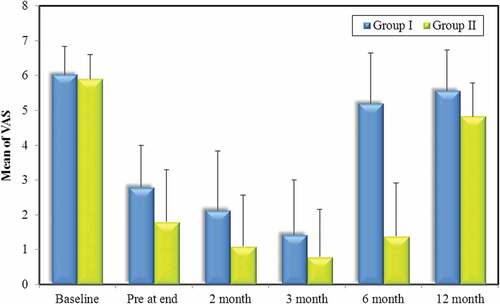
There was no statistically significance in base line VAS but at the end of the procedure group II showed a significant improvement from the base line with mean value from (5.90 ± 0.71) to (1.80 ± 1.49) at the end which was superior to group I that VAS score mean shifted from (6.03 ± 0.81) to (2.80 ± 1.19) although both group exhibit a higher statistical significant improvement than base line. Statistically significance continued up to 3-month follow up in both groups. Group II patients continued to 6 months follow up with significant improvement from base line compared to group I. Follow up at 12 months mean score tends to be statistical insignificant form base line in the studied groups but of lower VAS values in group II compared to group I with statistically significant different P value (0.012*).
A total of 9 (30%) patients had a positive response (at least 50% declination in VAS score) to the genicular nerve block procedure, group II 17 patients (56.7%) show a positive response when the procedure was completed -first evaluation – the improvement was better than base line but some complain after injection of joint pain and stiffness not exceeding 48 hours.
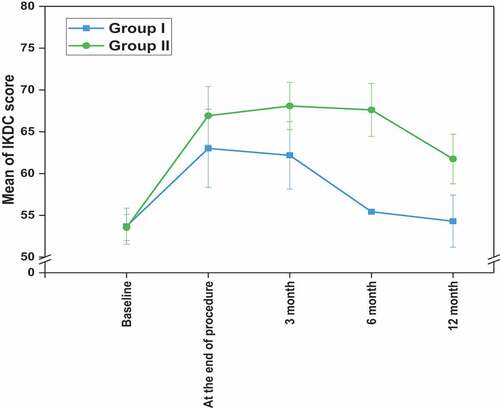
IKDC score show statistical significance in both groups starting from 3 months evaluation with higher mean in group II (68.06 ± 2.83) and p value (<0.001*), significant results in both groups continued up to 6 months follow up with superiority of group II which show statistically significance till the 12 months follow up.
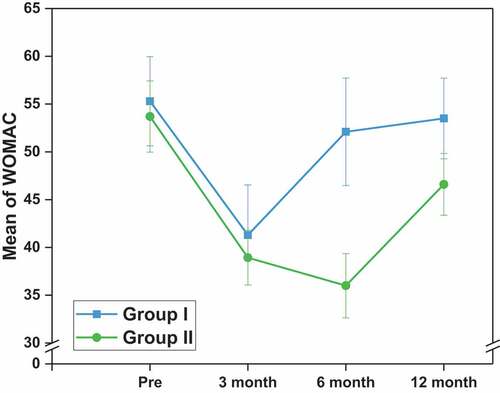
WOMAC score was significantly lower in group II with mean (38.93 ± 2.86) compared to group I (41.30 ± 5.23) that gives advantage to group II both were statistically significant from base line value up to the first 3 months, however group II exhibit significant pain relief for 12 months follow up with p value (<0.001*) and mean vale (46.60 ± 3.23) compared to group I (53.50 ± 4.22) and lower than the base line mean value (53.70 ± 3.72) of group II
As regards knee joint US score there was a significant improvement throughout the follow up intervals juxtaposed with the base line vale of the same group (group II) starting mean value (4.47 ± 1.43) to 3 months, 6 months (3.37 ± 1.47) and 12 months (3.67 ± 1.47), which was superior to group I that show no improvement in score over 6 month and might get worse in 12 months follow up compared to the base line value.
5. Discussion
The most important finding of the present study was that in Egyptian knee osteoarthritis patients, IA-PRP combined with articular surface radiofrequency ablation did not cause any grave adverse effects during the first 12 months following the treatment. Moreover, it was demonstrated that PRP therapy can significantly decrease pain, functional limitations, and stiffness up to 12 months in candidates with knee OA. All adverse events observed were mild and included stiffness, tingling sensation, and walking pain just after the injection. These symptoms resolved spontaneously within 48 hours. Although it is still unclear exactly how PRF takes effect [Citation12,Citation15,Citation16], laboratory reports suggest an actual neurobiological phenomenon modifying the pain signaling, which has been described as neuromodulator [Citation17].
PRF treatment is used in this study rather than traditional RF ablation. The temperature of the target tissue in PRF treatment is frequently set around 42°C, so that nerve destruction and the neuropathic pain or Charcot joints are not expected to be an issue. Moreover, The PRF method looks to be less risky than conventional RF ablation when it comes to motor loss, responses resembling neuritis and conserving fibers of both motor and autonomic nerves [Citation18]. The proximity of three genicular nerves (SM, IM, and SL) to the same-named genicular arteries was the reasoning for targeting them. The IL nerve, which is quite close to the fibula’s neck, was not targeted to avoid the possibility of peroneal nerve damage which is a common ailment. [Citation10]
In this study, the overall VAS score improvement was 74% in group II compared to 40% in group I. Finally, 63% of the examined patients experienced a 50% improvement during a 6 months period. In fact, the improvement process had an upward trend till twelve weeks after the intervention, and the maximum improvement was observed in that period; thereafter, there was significant decline in scores until 6 months. This might be due to an excessive use of knee joint secondary to pain relief and is considered an underestimation of the results. In this study, PRP therapy combined with PRF ablation of articular surface was more successful than PRF genicular nerve ablation in improving the quality of life of patients with knee OA proved by WOMAC, IKDC score and knee US score.
Sluijter et al suggested the hypothesis that PRF may have dual effect in intra-articular applications. PRF has two effects on the nervous system, one is that it suppresses the excitatory C-fiber response, secondly, it inhibits synaptic transmission. Chen Z et al suggested PRP has apparent benefits in the conservative treatment of osteoarthritis in the knee. Treatment with PRP long-term pain can be reduced and knee joint function can be improved with no additional dangers. [Citation19].
Sánchez et al. evaluated 176 patients (PRP group, 89 patients vs. HA group, 87 patients) with symptomatic knee osteoarthritis. In their study, IA injection-related adverse effects were generally modest and evenly distributed between the two groups, and all occurrences, such as local soreness surrounding the infiltration site, went away within 48 hours of injection. [Citation20]. In a study by Filardo et al.no major complications related to the PRP injections were observed, but the incidence of post-injection pain reaction in the PRP group was higher than in the HA group. Filardo et al. considered PRP’s negative consequences as being related to reactive oxygen species (ROS) and proteases liberated from WBCs. The absence of serious adverse events, noted in previous studies and in the present investigation, suggests that IA-PRP represents a safe treatment option for patients with osteoarthritis of the knee [Citation21].
Regarding the effectiveness of IA-PRP for knee osteoarthritis, Taniguchi Y et al [Citation22] conducted a systematic review of six randomized, controlled trials, PRP injection was found to achieve a significant clinical improvements for about 12 months after injection; moreover, the clinical outcomes and WOMAC global score was much better after treatment with leukocyte-poor PRP than after treatment with HA at 3–12 months post-injection. Despite the favorable outcomes reported with PRP treatment, the evaluated studies only included Caucasian patients. As recent studies have claimed that platelet activity varies with ethnicity [Citation23]. Our present study represents a report regarding the outcome of IA-PRP in Egyptian patients with osteoarthritis of the knee, and to demonstrate that 8 of 10 patients had a decrease in the VAS pain score of ≥50% (compared to VAS score at baseline), with the beneficial effects persisting for 12 months. In this study, the WOMAC and IKDC scores, were used for evaluation. Regarding the IKDC score, improvements in pain brought about improvements in total score, as well as in the scores for walking ability and for ascending and descending stairs. On the other hand, the WOMAC score improved significantly after 1 month, and the improvements seen after 3 months then 6 months were statistically significant.
Chang et al compared the impacts of PRP and HA injection for knee pain and concluded that PRP injection was more efficient for patients with devastated articular cartilage than was HA alone. Also, patients with mild degree OA exhibit a better response to PRP injection compared to those with severe OA [Citation24].
6. Conclusion
Our findings suggest that IA-PRP combined with articular surface pulsed radiofrequency ablation is safe for use in Egyptian patients with grade I/II knee osteoarthritis, and, while local and minor adverse events related to PRP injection occurred, all symptoms disappeared within 48 hours. This therapy has the potential to induce pain relief that is for as long as 6 months, but further study is needed to verify the efficacy.
7. Limitations
There were several limitations in the present study, being a small sized, single center study. The absence of standardization of standing knee radiographs to measure real articular cartilage changes, and the use of only PRP products not compared to any other intra-articular drugs. More researches with a randomization is needed, control group, and there is a need for bigger case population.
Furthermore, other non-intrusive condition evaluation, such as MRI, are essential to examine the cartilage thickness following therapy.
Acknowledgments
This paper and the research behind it would not have been possible without the exceptional support of my supervisors. Their enthusiasm, knowledge and exacting attention to detail have been an inspiration and kept my work on track.
References
- Sinusas K. Osteoarthritis: diagnosis and treatment. Am Fam Physician. 2012;85(1):49–56.
- Abd EL, Fatah MI, Weheida SM, et al.. Effect of contrast hydrotherapy on pain intensity and quality of life outcomes for patients with knee osteoarthritis. Assiut Sci Nurs J. 2019;7(16):35–42.
- SMA B-Z, Koes BW. Risk factors and prognostic factors of hip and knee osteoarthritis. Nat Clin Pract Rheumatol. 2007;3(2):78–85.
- Chen AF, Mullen K, Casambre F, et al.. Thermal nerve radiofrequency ablation for the nonsurgical treatment of knee osteoarthritis: a Systematic literature review. J Am Acad Orthop Surg. 2020.
- Chun N, Canapp S, Carr BJ, et al.. Validation and characterization of platelet-rich plasma in the feline: a prospective analysis. Front Vet Sci. 2020;7:512.
- Le ADK, Enweze L, DeBaun MR, et al.. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11(4):624–634.
- Collins NJ, Misra D, Felson DT, et al.. Measures of knee function: international Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63 Suppl 11(11):S208–28.
- Theiler R, Spielberger J, Bischoff HA, et al.. Clinical evaluation of the WOMAC 3.0 OA Index in numeric rating scale format using a computerized touch screen version. Osteoarthritis Cartilage. 2002;10(6):479–481.
- Georgiev T. Clinical characteristics and disability in patients with knee osteoarthritis: real world experience from bulgaria. Reumatologia. 2019;57(2):78–84.
- Yasar E, Kesikburun S, Kılıç C, et al.. Accuracy of ultrasound-guided genicular nerve block: a cadaveric study. Pain Physician. 2015;18(5):E899–904.
- Ojango C, Raguso M, Fiori R, et al.. Pulse-dose radiofrequency treatment in pain management-initial experience. Skeletal Radiol. 2018;47(5):609–618.
- Sluijter ME, Teixeira A, Serra V, et al.. Intra-articular application of pulsed radiofrequency for arthrogenic pain--report of six cases. Pain Pract. 2008;8(1):57–61.
- Riecke BF, Christensen R, Torp-Pedersen S, et al.. An ultrasound score for knee osteoarthritis: a cross-sectional validation study. Osteoarthritis Cartilage. 2014;22(10):1675–1691.
- McHugh ML. The chi-square test of independence. Biochem Med (Zagreb). 2013;23(2):143–149.
- Halim W, Chua NH, Vissers KC. Long-term pain relief in patients with cervicogenic headaches after pulsed radiofrequency application into the lateral atlantoaxial (C1–2) joint using an anterolateral approach. Pain Pract. 2010;10(4):267–271.
- Tekin I, Mirzai H, Ok G, et al.. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23(6):524–529.
- West M, Wu H. Pulsed radiofrequency ablation for residual and phantom limb pain: a case series. Pain Pract. 2010;10(5):485–491.
- Abd-Elsayed A, Anis A, Kaye AD. Radio frequency ablation and pulsed radiofrequency for treating peripheral neuralgias. Curr Pain Headache Rep. 2018;22(1):5.
- Chen Z, Wang C, You D, et al.. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. Medicine (Baltimore). 2020;99(11):e19388.
- Sánchez M, Fiz N, Azofra J, et al.. A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy. 2012;28(8):1070–1078. DOI:10.1016/j.arthro.2012.05.011.
- Filardo G, Kon E, Di Martino A, et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:229.
- Taniguchi Y, Yoshioka T, Kanamori A, et al.. Intra-articular platelet-rich plasma (PRP) injections for treating knee pain associated with osteoarthritis of the knee in the Japanese population: a phase I and IIa clinical trial. Nagoya J Med Sci. 2018;80(1):39–51.
- Morikawa Y, Kato H, Kashiwagi H, et al. Protease-activated receptor-4 (PAR4) variant influences on platelet reactivity induced by PAR4-activating peptide through altered Ca(2+) mobilization and ERK phosphorylation in healthy Japanese subjects. Thromb Res. 2018;162:44–52.
- Chang K-V, Hung C-Y, Aliwarga F, et al.. Comparative effectiveness of platelet-rich plasma injections for treating knee joint cartilage degenerative Pathology: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(3):562–575.