ABSTRACT
Background and Aims
Abdominal compartmental syndrome considered the most common cause of postoperative mortality in neonates scheduled for surgical repair of congenital abdominal wall defect. This study aimed primarily to observe the renal and cerebral rSO2 variation during and after surgical reduction, while secondarily to analyze correlations with other perfusion markers of intra-abdominal hypertension.
Patients and methods
A randomized, prospective, cohort study was piloted in a tertiary care pediatric surgery center from February 2017 to march 2021 where 20 neonates scheduled surgical repair of congenital abdominal wall defects. Near-infrared spectroscopy (NIRS) measurements of regional tissue oxygenation (rSO2) fluctuations performed using the two-channel mode, channel 1 for cerebral monitoring (C rSO2) and channel 2 for renal monitoring (R rSO2), and calculating differences intraoperative as well as postoperative.
Results
Intra-operative C and R ΔrSO2 had a significant positive correlation with an intraoperative post-ductal SPO2 and MABP changes, while a significant negative correlation was noted with serum lactate level and capillary refill time. Postoperative C ΔrSO2 showed a negative correlation with postoperative serum lactate level, whereas postoperative R ΔrSO2 had a positive correlation with postoperative post-ductal SPO2 changes, and negative correlations with postoperative capillary refill time changes. Pathological intraoperative ΔrSO2 had a statistically significant relation with intraoperative post-ductal SPO2, MABP, capillary refill time, serum lactate level, postoperative serum creatinine level, and postoperative vasoactive-ventilation-renal (VVR) score.
Conclusion
: NIRS is an efficient non-invasive monitor of cerebral and tissue perfusion, evaluating tissue microcirculation, and considered an early warning for detecting abdominal compartment syndrome (ACS) in neonates.
1. Introduction
Ventral abdominal wall defects involve multiple congenital malformations including gastroschisis and omphalocele, which are common anomalies relative to ectopia cordis, bladder exstrophy, and cloacal exstrophy. [Citation1] The combined prevalence of omphalocele and gastroschisis is one case per 3,500 newborns. [Citation2] Gastroschisis defined as uncovered abdominal visceral herniation through a full-thickness abdominal wall defect [Citation3]. In contrast, omphalocele is a central abdominal wall defect in which the protruded abdominal contents are covered in a thin sac [Citation4].
Abdominal compartment syndrome (ACS) considered the most common postoperative complication, especially with herniated visceral reintegration surgery, defined as intra-abdominal hypertension associated with one or more organs dysfunction. [Citation5] Intra-abdominal hypertension (IAH), defined as increased intra-abdominal pressure (IaP) >12 mmHg, lead to ventilatory and circulatory compromises in critically ill neonates [Citation6], there is no accredited standard technique for IaP measurement in neonatal surgery [Citation7].
End organ perfusion usually assessed by clinical signs as capillary refill time, urine output, heart rate, base excess, lactate concentration, and blood pressure [Citation8]. However, early perfusion disorders detection required to improve therapeutic outcome is difficult to be achieved using clinical signs alone. [Citation9]
Near infrared spectroscopy was first described in 1977 by Jobsis [Citation10] as a continuous non-invasive method of tissue oxygenation assessment. Regional oxygen saturation (rSO2) measuring the percentage of oxygenated hemoglobin in a target tissue, can detect microcirculatory dysfunctions. [Citation11]
The renal oxygen values considered a sensitive indicator for cardiac output changes, while cerebral oxygen values are relatively stable due to cerebral auto-regulation mechanisms. [Citation12] Recent studies estimated the validity of simultaneous monitoring of cerebral and renal oxygen tension in prediction of subclinical hypoperfusion. [Citation13]
The vasoactive-ventilation-renal (VVR) score introduced in 2015 as a novel predictor of postoperative prognosis in neonates [Citation14], based on the measurement of inotropic support required to provide hemodynamic stability, markers of the pulmonary, and renal systems. [Citation15]
The aim of the present study primarily was to observe the renal and cerebral rSO2 variation and pathological values during and after surgical reduction of neonatal viscera procedures, while secondarily to analyze correlations with other perfusion markers including MAP, pH, lactate concentration, and vasoactive-ventilation-renal score.
2. Patients and methods
A randomized, prospective, cohort study piloted in a tertiary care pediatric surgery center from February 2017 to march 2021 after the approval of the regional ethical committee.
A written informed approval was attained from the parents for the contribution of their infants in this study. The sample size was approved to be appropriate by the Department of Statistics, Medical Research Institute, Alexandria University, Egypt. [Citation16]
Twenty full-term neonates of both sex, weighing 3–5 kg, scheduled for congenital abdominal wall defect repair, whereas infants had hemodynamic instability, cyanic heart disease, and very low body weight (VLBW) were excluded from the study. All infants were assessed preoperatively with complete history taking, clinical examination and routine laboratory investigations.
On arrival to operating theater the neonate was attached to multichannel monitor including continuous electrocardiogram, heart rate, pulse oximeter (pre-ductal SPO2 of Rt upper limb, post-ductal SPO2 of Lt lower limb), noninvasive arterial blood pressure, and capnography (EtCO2) after endotracheal tube (ETT) insertion.
Near infrared spectroscopy measurements were performed with a continuous wave system (INVOS 5100 C, Somanetics, Troy, MI, USA), used the two-channel mode, with channel 1 for cerebral monitoring and channel 2 for renal monitoring. Cerebral (C) sensor positioned on the forehead (below the hairline) and a renal (R) sensor on the neonate’s lower back (right side) between T10 and L2, accurate localization of right kidney performed using ultrasound curvilinear transducer with a frequency ranging between 5 and 7.5 MHz. [Citation17]
All infants had general anesthesia induced by incremental concentrations of sevoflurane (2%–4%) with oxygen and 24 gauge intravenous cannula was inserted and secured.
To facilitate insertion of endotracheal tube, rocuronium 0.6 mg/kg and fentanyl 1 µg/kg was given. Maintenance of anesthesia was achieved with a pressure-controlled mechanical ventilation mode (PCV) [PIP = 18–22 mmHg, PEEP = 3 mmHg, I: E = 1:1.5, RR = 35 bpm, FiO2 = 100%] using increments of rocuronium (0.1 mg/kg), and sevoflurane (0.6%–2%).
Surgeons checked the position of the sensor and consolidated its fixation. The anesthetists made sure of uninterrupted recording of NIRS. At the end of the surgical procedure the infant was transferred intubated to NICU sedated on continuous infusion of fentanyl with rate of 1 mcg/kg/h and mechanically ventilated with pressure controlled mode (PCV) [PIP = 18–22 mmHg, PEEP = 3 mmHg, I: E = 1:1.5, RR = 35 bpm].
Demographic information (chronological age, gestational age, sex, and weight), the hemodynamic and respiratory monitoring done by HR, MABP, pre-ductal SpO2, and post-ductal SpO2 recording every 15 min intraoperative, while postoperative values were documented hourly for first 6 h, later every 3 h for 18 h.
Near infrared spectroscopy measurements were achieved by a continuous wave system. Cerebral (C rSO2), renal (R rSO2), and rSO2 variations (ΔrSO2) [ΔrSO2 = ((rSO2measured − rSO2initial)/rSO2initial) × 100 (%), initial C rSO2 and R rSO2 value on arrival to the operating theater on room air] values were simultaneously recorded and calculated along with hemodynamics and respiratory parameters. Pathological ΔrSO2 defined by a 20% or more decrease of measured rSO2, compared to initial rSO2 values.
Capillary refilling time defined as time required for return of circulation to blanched area achieved by applying sustained pressure with index finger soft bad for 5 s on forehead.
Capillary refill time and lactate concentrate were recorded every 6 h and mean value was calculated.
VVR scores = VI (Ventilation Index) + vasoactive inotrope score (VIS) + ΔCr. [Citation18]
VIS = dopamine dose + dobutamine dose + 100 × epinephrine dose + 10 × milrinone dose + 10,000 × vasopressin dose + 100 × norepinephrine dose.
VI = ((respiratory rate × Δ pressure ×PaCO2)/1,000).
ΔCr = change in creatinine from baseline × 10.
VIS and VI were calculated initially at preoperative time as zero. Baseline preoperative serum creatinine was subtracted from 24 h postoperative serum creatinine measurement.
3. Statistical analysis
Data were coded, reviewed and analyzed using the SPSS version 25.0 (Armonk, NY: IBM Corp). Quantitative data were expressed as median and range as the data was not normally distributed. Qualitative data were expressed as frequency and percentage. Friedman test was used to assess the difference between more than two related groups and Wilcoxon ranked test was used for the pairwise comparison. Mann Whitney test was used to test the significant difference between two independent variables and Pearson Correlation (r) was used to measure the strength of a linear association between two continuous variables. P value below than 0.05 was considered significant.
4. Results
A total of 32 patients were screened for eligibility; 22 patients met inclusion criteria and were approached to participate, and two infants died before surgery (Flowchart 1).
Flowchart 1. Flow diagram.
As regards demographic data, all infants incorporated in the study were full term (gestational age = 38.09 ± 0.88 weeks), weighted 2.92 ± 0.2 Kg), aged (chronological age = 4.65 ± 5.22 days), and of both sex (male/female = 60/40%).
Eight infants had primary closure of abdominal wall defects (one case of gastroschisis and seven cases of omphalocele), and six infants required a silo pouch stoma for gradual reintegration of the herniated viscera (five cases of gastroschisis and one case of omphalocele), then complete closure accomplished, respectively, on 10, 11 and 13 days post-initial surgery (), whereas the mean duration of surgeries was about 95 ± 72 minutes.
Table 1. Demographic data of the study sample
Perioperative measurements of heart rate, pre-ductal SPO2, post-ductal SPO2, and capillary refill time were stable with statistically insignificant differences (), while statistically significant decline of MABP recorded intraoperative and postoperative in comparison to preoperative measurements (P1 < 0.001*, p2 = 0.025*, p3 = 0.333), furthermore serum lactate level showed a statistically significant increase throughout intraoperative and postoperative periods (p1 < 0.001*, p2 < 0.001*, p3 = 0.537) as presented in ().
Table 2. Differences between pre, intra and postoperative as regards hemodynamic parameters
5. Cerebral and renal rSO2 variations and correlations with other perfusion markers
Cerebral rSO2 values presented a statistically significant upsurge during intra-operative and postoperative period compared to initial values (p1 = 0.004*, p2 < 0.001*, p3 = 0.742), however, R rSO2 values had a statistically insignificant decline noted throughout an intraoperative and postoperative times (F = 0.757, P value = 0.685) as reported in ().
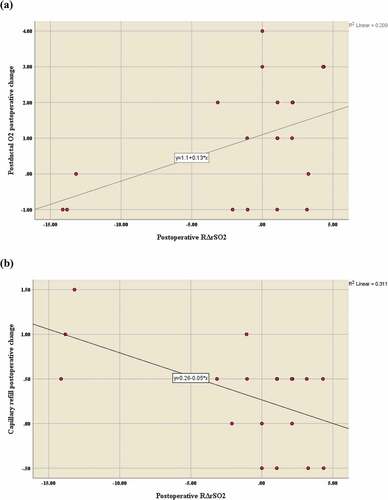
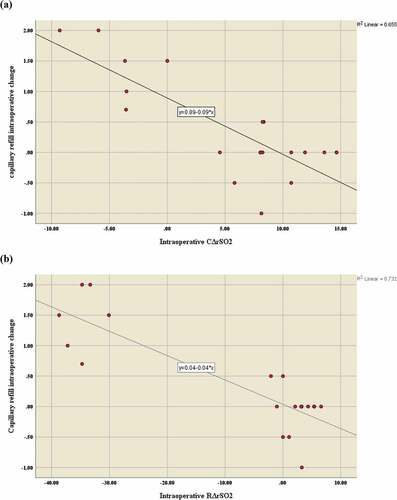
Intra-operative C and R rSO2 variations had a significant positive correlation with an intraoperative post-ductal SPO2 (respectively, r = 0.844, P < 0.001*; r = 0.930, P = <0.001*) () and MABP changes (respectively, r = 0.878, P < 0.001*; r = 0.961, P = <0.001*) (), while a significant negative correlation was noted with serum lactate level (respectively, r = −0.665, P < 0.001*; r = −0.853, P < 0.001*) () and capillary refill time (respectively, r = −0.809, P < 0.001*; r = −0.865, P < 0.001*) (), and no correlations were observed with heart rate and pre-ductal SPO2 changes ().
Table 3. Correlation between intraoperative perfusion parameters and variation of C rSO2 and R rSO2
Figure 1. Correlation of intraoperative ΔrSO2 and post-ductal O2 intraoperative change(a) intraoperative C ΔrSO2 (b)Intraoperative RΔrSO2
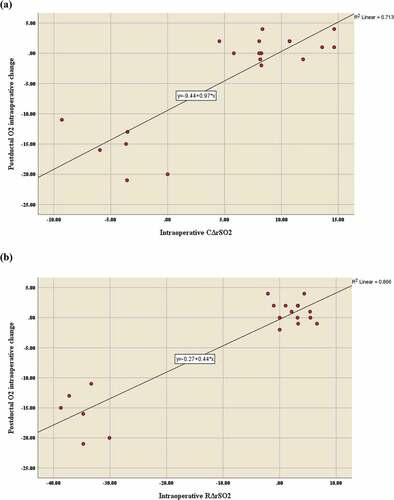
Figure 2. Correlation between intraoperative ΔrSO2 and MABP intraoperative change (a) Intraoperative C ΔrSO2 (b) Intraoperative R ΔrSO2
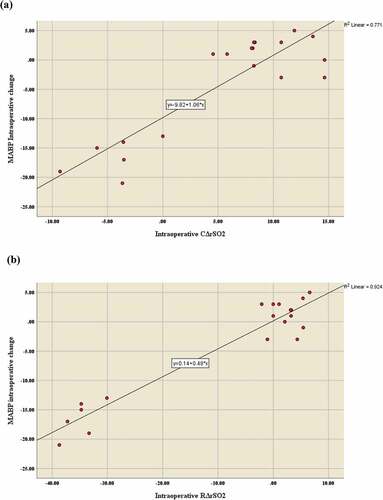
Figure 3. Correlation between intraoperative ΔrSO2 and serum lactate intraoperative change (a) Intraoperative C ΔrSO2 (b) Intraoperative R ΔrSO2
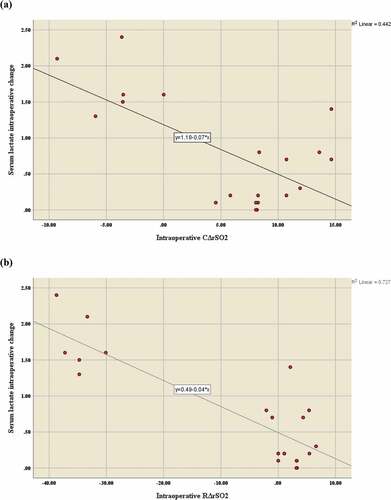
Figure 4. Correlation between intraoperativeΔrSO2 and capillary refill intraoperative change (a) Intraoperative C ΔrSO2 (b) Intraoperative R ΔrSO2
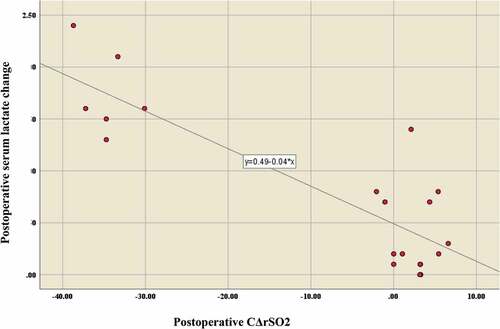
Postoperative C rSO2 variations showed a negative correlation with postoperative serum lactate level (r = −0.464, P = 0.039*) (), and no correlations were found with any of the other parameters studied (), whereas postoperative R rSO2 variations had a positive correlation with postoperative post-ductal SPO2 changes (r = 0.458, P = 0.043*), and negative correlation was recorded with postoperative capillary refill time changes (r = −0.558, P = 0.011*) (). No correlations were verified between postoperative R rSO2 variations and other perfusion parameters ().
Table 4. Correlation between postoperative perfusion parameters and variation of C rSO2 and R rSO2
6. Pathological ΔrSO2 incidence and relations with other perfusion markers
Pathological ΔrSO2 observed intra-operative in six infants, three cases had both pathological C and R ΔrSO2 occurred during progressive visceral reduction, whereas three cases showed isolated pathological R ΔrSO2 occurred with trial of abdominal wall closure, so silo pouch stoma used to permit progressive reintegration of the herniated viscera, as it was critical to achieve the reintegration in one surgical step.
The analysis of the present data documented a statistically significant relation between incidence of intraoperative pathological ΔrSO2 and intraoperative post-ductal SPO2, MABP, capillary refill time, serum lactate level, postoperative serum creatinine level, and postoperative VVR score, while no relation was found between pathological ΔrSO2 and any of the other parameters studied as presented in ().
Table 5. Correlation between pathological ΔrSO2 and perfusion markers
7. Discussion
Abdominal compartmental syndrome causes increased mortality and morbidity in neonatal intensive care, intra-abdominal hypertension associated with regional renal and mesenteric hypoperfusion. [Citation19] Early diagnosis of IAH can prevent progression to ACS and improve postoperative outcomes. [Citation20]
Previous literature data revealed that no absolute reference values for NIRS measures due to inter-individual variations; however, a 20% decrease of the initial rSO2 was established that is a sign of tissue hypoperfusion [Citation21], while an absolute value of cerebral rSO2 < 50% associated with hypoxic brain injury evident in radiological imaging and risk of disability [Citation22].
An upsurge of cerebral rSO2 noted intraoperative and postoperative resulted from high fraction of inspired oxygen (FiO2) and elevated PIP (>20 mmHg) applied to maintain effective ventilation during the increased abdominal pressure, in agreement with the present results Beck et al. [Citation23] studied changes of regional oxygen saturation during neonatal digestive surgeries and concluded that cerebral auto-regulation and high ventilation pressure were the reasons of stable CrSO2.
Intra-operative C and R rSO2 variations had a significant positive correlation with an intraoperative post-ductal SPO2 and MABP changes, while a significant negative correlation was noted with serum lactate level and capillary refill time.
Sood et al. [Citation24] reported that regional saturation variations reflect global saturation and MAP variations. Whereas Kaufman et al. [Citation25] documented negative correlation between serum lactate levels and splanchnic rSO2 levels. They reported that rSO2 considered an index for systemic oxygenation and perfusion of infants after congenital heart surgery.
Postoperative C rSO2 variations showed a negative correlation with postoperative serum lactate level whereas postoperative R rSO2 variations had a positive correlation with postoperative post-ductal SPO2 changes, and negative correlation with postoperative capillary refill time changes. Al Tayar et al. [Citation26] concluded that cerebral rSO2 considered a noninvasive predictor of shock. While Balakrishnan et al. [Citation27] assessed low somatic NIRS values in relation to other hemodynamic parameters in the critically ill children and found a positive correlation between low somatic NIRS values and early implication of life-saving interventions.
An intraoperative pathological ΔrSO2 observed in 30% of included infants occurred with trial of abdominal wall closure and had a strong relation with other perfusion markers. Conforti et al. [Citation28] studied NIRS values in neonates had congenital diaphragmatic hernia (CDH) repair and concluded that reduction of herniated viscera induced intra-abdominal hypertension, which could worsen regional abdominal tissue oxygenation.
However, Westgarth-Taylor et al. [Citation29] documented that pathological ΔrSO2 correlated to multiple factors as intra-abdominal hypertension (IAH), frailty, and fluid management issue.
The present study verified the strong relation between the incidence of pathological ΔrSO2 which necessitates circulatory as well as ventilatory support and increased postoperative morbidity measured by VVR score. Cashen et al. [Citation30] documented the value of vasoactive-inotropic score as predictor of morbidity and mortality in neonates undergoing cardiac surgery.
8. Conclusion
NIRS is an efficient non-invasive monitor of cerebral and tissue perfusion, evaluating tissue microcirculation, and considered an early warning for detecting abdominal compartment syndrome (ACS) in neonates.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethics approval and consent to participate
The present study was approved by the ethical committee of Faculty of Medicine, Alexandria University (IRB no. 00007570, FWA no. 00018702). A consent to participate was obtained as well.
Consent for publication
Written informed consent was obtained from the parents for publication of this article and any accompanying tables/images. The copies of the written consents are available for review by the Editor of this journal upon request.
Acknowledgments
Not applicable
Availability of data and material
All data supporting the study are presented in the manuscript or available upon request.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Campbell KH, Copel JA. Omphalocele. Obstetric imaging: fetal diagnosis and Care. 2ed ed. Philadelphia: Elsevier; 2018. p. 85–91.
- Gonzalez KW, Chandler NM. Ruptured omphalocele: diagnosis and management. Semin Pediatr Surg. 2019;28(2):101–105.
- Gamba P, Midrio P. Abdominal wall defects: prenatal diagnosis, newborn management, and long-term outcomes. Semin Pediatr Surg. 2014;23(5):283–290.
- Méndez-Martínez S, García-Carrasco M, Mendoza-Pinto C, García-Cano E, Montiel-Jarquín ÁJ. Surgical Complications of Simple and Complex Gastroschisis in Newborn. Eur J Gen Med. 2016;13(2):88–93. https://doi.org/10.15197/ejgm.1495
- Kirkpatrick AW, Roberts DJ, De Waele J, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–1206
- Newcombe J, Mathur M, Ejike JC. Abdominal compartment syndrome in children. Critical Care Nurse. 2012;32(6):51–61.
- Akhobadze GR, Chkhaidze MG, Kanjaradze DV, et al. Identification, management and complications of intra-abdominal hypertension and abdominal compartment syndrome in neonatal intensive care unit (a single center retrospective analysis). Georgian Med News. 2011;Mar(192):58–64.
- Stranak Z, Semberova J, Barrington K, et al. International survey on diagnosis and management of hypotension in extremely preterm babies. Eur J Pediatr. 2014;173(6):793–798.
- Weindling M, Paize F. Peripheral hemodynamics in newborns: best practice guidelines. Early Hum Dev. 2010;86(3):159–165.
- Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198(4323):1264–1267.
- Vesoulis ZA, Mintzer JP, Chock VY. Neonatal NIRS monitoring: recommendations for data capture and review of analytics. J Perinatology. 2021;41(4):675–688
- Montaldo P, De Leonibus C, Giordano L, et al. Cerebral, renal and mesenteric regional oxygen saturation of term infants during transition. J Pediatr Surg. 2015;50(8):1273–1277.
- Harer MW, Chock VY. Renal tissue oxygenation monitoring—an opportunity to improve kidney outcomes in the vulnerable neonatal population. Front Pediatr. 2020 May;14(8):241.
- Kg M, TJ S, Re D, et al. Use of a novel vasoactive-ventilation-renal score to predict outcomes after paediatric cardiac surgery. Interact Cardiovasc Thorac Surg. 2015;20(3):289–295.
- Benavidez OJ, Gauvreau K, Del Nido P, et al. Complications and risk factors for mortality during congenital heart surgery admissions. Ann Thorac Surg. 2007;84(1):147–155.
- Raghunathan V, Dhaliwal MS, Khilnani P, et al. An update on intra-abdominal hypertension and abdominal compartment syndrome in children. J Pediatr Crit Care. 2016;3(4):63–72.
- Agunloye A, Ayede A, Omokhodion S. The role of routine post-natal abdominal ultrasound for newborns in a resource-poor setting: a longitudinal study. BMC Pediatr. 2011;11(1):64.
- Zubarioglu AU, Yıldırım Ö, Zeybek C, et al. Validation of the vasoactive-ventilation-renal Score for neonatal heart surgery. Cureus. 2021;13(5):e15110.
- Kim JW, SHin WJ, Park I, et al. Splanchnic oxygen saturation immediately after weaning from cardiopulmonary bypass can predict early postoperative outcomes in children undergoing congenital heart surgery. Pediatr Cardiol. 2014;35(4):587–595.
- Thabet FC, Bougmiza IM, Chehab MS, et al. Incidence, risk factors, and prognosis of intra-abdominal hypertension in critically ill children: a prospective epidemiological study. J Intensive Care Med. 2015;31(6):403–408.
- Lejus C, Biard M, Leclair M-D. Urgences chirurgicales néonatales [Neonatal surgical emergencies]. EMC – Anesth Réanim. 2011;8(2):1–16
- Raux O, Sola C, Macq C, et al. Cerebral near-infrared spectroscopy (NIRS) in paediatric anaesthesia. Ann Fr Anesth Réanim. 2013;32(1):49–53
- Beck J, Loron G, Masson C, et al. Monitoring cerebral and renal oxygenation status during neonatal digestive surgeries using near infrared spectroscopy. Front Pediatr. 2017;5:140–150.
- Sood BG, McLaughlin K, Cortez J. Near-infrared spectroscopy: applications in neonates. Semin Fetal Neonatal Med. 2015;20(3):164–172.
- Kaufman J, Almodovar MC, Zuk J, et al. Correlation of abdominal site near-infrared spectroscopy with gastric tonometry in infants following surgery for congenital heart disease. Pediatr Crit Care Med. 2008;9(1):62–68.
- Al Tayar A, Abouelela A, Mohiuddeen K. Can the cerebral regional oxygen saturation be a perfusion parameter in shock? J Crit Care. 2017;38:164–167.
- Balakrishnan B, Dasgupta M, Gajewski K, et al. Low near infrared spectroscopic somatic oxygen saturation at admission is associated with need for lifesaving interventions among unplanned admissions to the pediatric intensive care unit. J Clin Monit Comput. 2018;32(1):89–96.
- Conforti A, Giliberti P, Landolfo F, et al. Effects of ventilation modalities on near-infrared spectroscopy in surgically corrected CDH infants. J Pediatr Surg. 2016;51(3):349–353.
- Westgarth-Taylor C, de Lijster L, Van Bogerijen G, et al. A prospective assessment of renal oxygenation in children undergoing laparoscopy using near-infrared spectroscopy. Surg Endosc. 2013;27(10):3696–3704.
- Cashen K, Costello JM, Grimaldi LM, et al. Multicenter validation of the vasoactive ventilation-renal score as a predictor of prolonged mechanical ventilation after neonatal cardiac surgery. Pediatr Crit Care Med. 2018;19(11):1015–1023.