ABSTRACT
Background
Hemodynamic derangement due to pneumoperitoneum and postoperative pain after laparoscopic cholecystectomy can be detrimental; this study investigated whether preoperative intravenous (I.V.) infusion of clonidine or Magnesium Sulfate (MgSO4) could attenuate hemodynamic responses, reduce serum cortisol level and improve post-operative analgesia.
Materials and Methods
In total, 105 patients scheduled for laparoscopic cholecystectomy were randomized to either group C (I.V. infusion of clonidine 1.5 µg/kg), group M (I.V.infusion of MgSO2 30 mg/kg) or group S (I.V. infusion of isotonic saline) 15 min before induction of general anesthesia. Outcome variables were heart rate (H.R.), mean arterial pressure (MAP), serum cortisol leveln, total analgesic requirements and recovery time.
Results
HR was significantly lower in group C than that in groups M and S. MAP and serum cortisol were significantly lower in groups C and M than that in control group. Pain score was better in groups C and M than group S at the first 2 hours post-operative with (P values 0.024 and 0.19), respectively. Reduced post-operative analgesic requirement with delayed onset to first analgesic request were observed in groups C and M compared with the control group . Recovery time was significantly rapid in group C than that of groups M and S.
Conclusion
Pre-operative I.V. infusion of clonidine and MgSO4 significantly attenuated the hemodynamic response to pneumoperitoneum, reduced serum cortisol level, reduced postoperative pain and analgesic requirement as compared to controls in patients undergoing laparoscopic cholecystectomy. Clonidine was superior compared to MgSO4 regarding H.R. control and rapid recovery.
1. Introduction
Laparoscopic cholecystectomy has become the milestone accomplishment in the modern arena of surgical practice as a great advance in the management of patients with symptomatic gallbladder diseases. It has also become an integral component of ambulatory and one-day procedures; hence, it requires a balanced anesthesia technique to obtain a smooth post-operative recovery. It has the advantages of lesser tissue trauma, reduced post-operative pain, shorter hospital stay, more rapid return of normal activities with significant cost savings [Citation1].
However, the pneumo-peritoneum created during laparoscopy can induce stimulation of the neuro -endocrinal pathway which in turn increase the levels of several mediators such as catecholamines, renin, vasopressin, prostaglandins and cortisol with subsequent various hemodynamic and respiratory effects that may be harmful to the patients [Citation2,Citation3].
Methods to reduce these effects include administration of some pharmacological preparations to the patients, which will modify the response of anesthetic drugs [Citation4,Citation5].
Clonidine is a commonly used α2-agonist premedication that showed subsequent significant reduction in anesthetic requirements, less airway hyper-reactivity, less heart rate and less blood pressure increase [Citation6].
Magnesium sulfate is an antagonist of N-methyl-D-Aspartate (NMDA) receptors that has been recently shown to have a potential to reduce intra-operative anesthetic requirements and to reduce post-operative pain [Citation7].
This study is designed to compare the effects of pre-operative infusion of clonidine and magnesium sulfate on hemodynamic stability, peri-operative cortisol levels and post-operative analgesia in elective laparoscopic cholecystectomy procedures.
2. Materials and methods
This prospective, randomized, double-blind, placebo-controlled, comparative clinical study was carried out in Qena university hospitals in the time period from January 2016 to July 2017. Written informed consent was taken from every patient participating in the study after getting approval from Ethical Committee of Qena University Hospitals, Qena, Egypt (Chairperson Prof. Ahmad Abolyosr).
This study was registered in the Australian New Zealand Clinical Trials Registry (ANZCTR) and the allocated number is: ACTRN12616001233415. The web address of the trial is http://www.ANZCTR.org.au//ACTRN .aspx.
One hundred five (105) patients, of either sex, aged 18–60 years, American Society of Anesthesiologists (ASA) grade I and II scheduled for elective laparoscopic cholecystectomy were included. Patients with cardiovascular, respiratory, renal, hepatic, neurological diseases, morbidly obese patients, diabetes mellitus, pregnant or breast-feeding females, prolonged procedure (more than 60 minutes), anticipated difficult intubation, patients on anti-hypertensives, anti-psychotics, analgesics, corticosteroids or sedative medications were excluded from the study.
During pre-anesthetic checkup, a thorough clinical examination was done along with routine laboratory investigations for each patient. All patients were kept in an NPO status for 8 hours before surgery.
All patients who fulfilled inclusion criteria were included and an intravenous (I.V.) line was started and preloading with done with 10 mL/kg ringer,s lactate solution. Randomization method was done according to a computer-generated random table. Allocation concealment was done using closed envelops to randomize the patients into three groups.
Group C (n = 35): Received 1.5 µg/kg of clonidine hydrochloride (Catapressin ampoule 0.150 mg/mL – Boehringer Ingelheim) diluted with normal saline (total volume 50 mL), given slow intravenous infusion via syringe pump over 15 min before induction of general anesthesia.
Group M (n = 35): Received 30 mg/kg of magnesium sulfate diluted in normal saline (total volume 50 mL), given slow intravenous infusion via syringe pump over 15 min before induction of general anesthesia.
Group S (n = 35): Received 50 mL normal saline, given slow intravenous infusion via syringe pump over 15 min before induction of general anesthesia.
In order to facilitate blinding, the test solution was prepared by the first anesthesiologist who is not involved in the study in identical syringes and infused with syringe pumps (perfuser compact, B Braun). Neither the recording (second) anesthesiologist, nor the patient were aware of the kind of the drug.
In all cases, surgery was performed as the first operation of the day to eliminate diurnal variation in circulating steroid hormones.
In the operation theatre, standard monitoring including pulse oximetry, non-invasive blood pressure, five-lead electrocardiography (E.C.G.), end-tidal carbon dioxide (EtCO2) and temperature were connected to the patient and baseline cardio-respiratory parameters were noted and recorded at an interval of 10 min.
The level of anesthesia was continuously monitored intraoperative with bispectral index (BIS) (E-Enotropy – 01,GE monitor, Enotropy easy fit sensor-GE healthcare-Finland). The target BIS range was 40–60 for surgical anesthesia to prevent any hemodynamic changes arising due to awareness. Intermittent boluses of propofol were titrated and administered when indicated to achieve this target and the total intraoperative dose of propofol was recorded.
After 3 min pre-oxygenation with O2 100%, anesthesia was induced with a standard anesthetic protocol using intravenous (I.V.) fentanyl citrate 1 µg/kg, propofol 2 mg/kg over 30 s until BIS was below 60 and then endotracheal intubation was facilitated by atracurium 0.5 mg/kg body weight. Lungs were mechanically ventilated with O2 100% and anesthesia was maintained with isoflurane 1.1% and atracurium 0.1 mg/kg every 20 min. Ventilation was adjusted to maintain ETCO2 in the range of 32–36 mm Hg. Patients were placed in supine position with 15° left lateral tilt and 30° head elevation. During surgery, CO2 pneumo-peritonium was established and maintained at a pressure of around 12–14 mm Hg by an automatic insufflation unit till the completion of surgery. Normothermia was maintained during the operation and Ringer lactate solution was administered in a maintenance dose according to volume requirements and blood loss.
Any hypotension (MAP <20% preoperative) was treated with a fluid bolus of normal saline 250–300 mL if hypotension did not respond to fluid administration, ephedrine 5 mg I.V. was the second line of management. Any incidence of bradycardia (H.R. < 50/min.) was managed with atropine 0.5 mg I.V. Hypertension (MAP>20%preoperative) was managed with nitroglycerine infusion.
At the end of surgery, inhalational anesthesia disconnected and BIS was allowed to rise to 80 and residual neuromuscular block was reversed by neostigmine in a dose of 0.04 mg/kg and atropine in a dose of 0.02 mg/kg intravenously. Trachea was extubated after complete reversal of neuromuscular blockade and restoration of spontaneous respiration and patients were transferred to recovery room.
The following intra-operative and recovery parameters were recorded;
- Mean intra-operative abdominal pressure (mm Hg).
- Mean duration of pneumoperitoneum (min).
- Intraoperative consumption of propofol (mg/kg/hour).
- Tracheal extubation time (BIS >80).
-Time to response to verbal commands (spontaneous eye opening).
The incidence of post-operative adverse events including postoperative nausea and vomiting (PONV), shivering, post-operative agitation and patient sedation score ≥2 (was noted according to Ramsay sedation score) as follows: 0:Alert; 1: Quickly awake; 2: Asleep but easily aroused; 3: Asleep with sluggish response to verbal commands or touch; 4: No response to verbal command or touch were recorded.
Pain was assessed using 10 point visual analogue score (VAS) at 2, 4, 6, 8, 10 and 12 h postoperatively. Patients were observed in the postoperative period till VAS of 5 . Rescue analgesia in the form of injection ketolorac 30 mg I.M. first. Tramadol 2 mg/kg I.V. was given as a second line of analgesic. Time to first postoperative rescue analgesic request as well as total analgesic consumption in the first 24 hours postoperatively were recorded.
Mean blood pressure and Heart rate were recorded at the following times:
1- Baseline (upon arrival in the operative room).
2- Pre-induction (before induction of general anesthesia).
3- Three minutes after endotracheal intubation.
4- Before pneumoperitoneum (P0).
5- Fifteen minutes after pneumoperitoneum (P15).
6- Thirty minutes after pneumoperitoneum (P30).
7- Five minutes after exsufflation.
8- Five minutes after extubation.
2.1. Hormonal stress response evaluation
Neuroendocrine stress responses were assessed by quantitative measurement of resting plasma concentrations of cortisol using in vitro diagnostic method with the IMMULITE ® and IMMULITE 1000 analyzers (Siemens healthcare diagnostics ,USA) in blood sample collected peripherally from an antecubital vein of the arm contralateral to the intravenous infusion . The volume required is 10 UL serum (sample cup must contain at least 100 UL more than the total volume required). Storage of samples 7 days at 2–8°C or 3 months at −20°C.
Blood samples were obtained at:
Thirty minutes before transferring the patient to operative room (Baseline) [I0].
Three minutes after endotracheal intubation [I1].
Fifteen minutes after pneumoperitoneum [I2].
Five minutes after exsufflation [I3].
Six hours after extubation [I4].
First postoperative day [I5].
The samples were transferred to precooled tubes and soon centrifuged at −4°C, and the plasma was stored at −80°C until analysis. Concentrations of cortisol were measured by commercially available radioimmunoassay kit (Roche Diagnostics,USA).
The primary outcome variable of this study was Hemodynamic variables: (heart rate and mean blood pressure) and plasma cortisol levels. The secondary outcomes were: analgesic requirements, postoperative sedation and any possible adverse events.
2.2. Sample size
The primary outcomes were heart rate, mean arterial blood pressure (MAP) and plasma cortisol level (type I error [α] 5% and power of study 90%). Based on a pilot study on 10 patients subjected for laparoscopic cholecystectomy, it was calculated that 27 and 5 patients per group were required to detect a significant 20% intergroup difference in heart rate, mean arterial blood pressure and plasma cortisol level respectively. To compensate for possible dropouts, 35 patients per group were included.
2.3. Statistical analysis
Data analysis was performed using SPSS version 21 (SPSS Inc.Chicago,USA). Data were presented as mean ± SD or number (percentage). To compare mean values between the three groups, one-way analysis of varianc e(ANOVA) and post-hoc Tukey’s were used. Variations within the same group were analyzed using the paired-samples t-test. The χ2-test was used for comparison of proportions and frequencies among groups. P value <0.05 was considered statistically significant .
3. Results
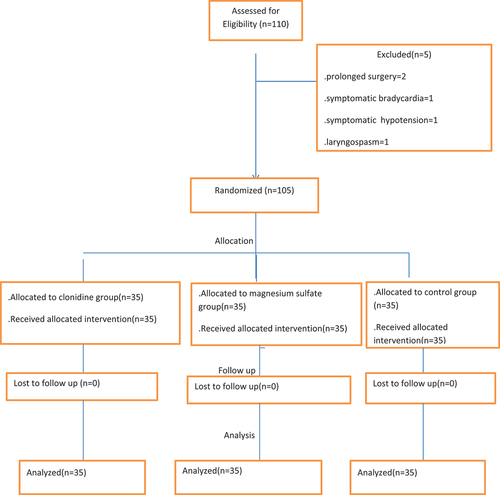
One hundred ten patients assessed for eligibility and only one hundred-five patients were included in the present study during a 18-month period with 33 patients in each group of the studied three groups: two patients experienced prolonged surgery, one patient developed symptomatic bradycardia requiring atropine, one patient developed hypotension requiring vasopressor support and one patient developed laryngospasm () .
All the three groups were comparable with respect to age, sex, body weight, ASA grade and the duration of surgery (P > 0.05) ().
Table 1. Demographic characteristics of the three studied groups(Mean ± SD)
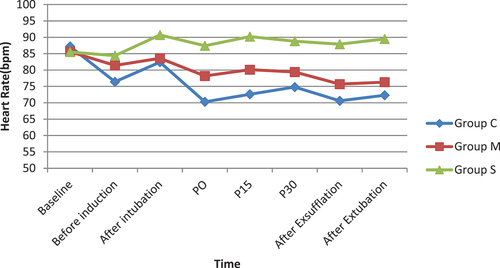
Regarding hemodynamic variables such as HR and MAP, the baseline vitals were comparable among the three groups. H.R. had statistically significant lower values in group C compared to groups M and S at P0, P15, P30, after exsufflation and after extubation (P < 0.001). No significant episodes of bradycardia were noted in any group ().
Figure 2. Heart rate changes in the studied three groups.
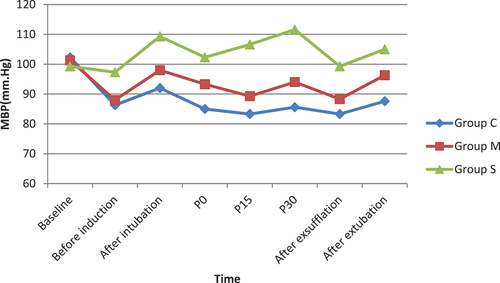
MAP was statistically significantly lower in groups C and M compared with group S at P0, P15, P30, after exsufflation and after extubation (P < 0.05). No significant episodes of hypotension were noted in any group ().
Figure 3. Mean arterial blood pressure (MBP) changes in the studied three groups.
Plasma concentration of cortisol hormone was a primary outcome in our study. Repeated measures ANOVA revealed a highly statistically significant higher hormone levels in the control group (group S) compared to the studied two groups (groups C and M) . The post hoc analyses showed similar hormonal levels at baseline and highly statistically significant higher levels of cortisol in the control group compared to the two studied groups groups after endotracheal intubation (I1), 15 minutes after pneumoperitoneum (I2) and 5 minutes after exsufflation (I3) {P < 0.001}. Then, slightly statistically significant higher cortisol level in the control group compared to the two studied groups at 6 hours after extubation (I4) (P < 0.05), but there was no statistically significant differences between the three studied groups at first postoperative day (I5) (P > 0.05) ().
Table 2. Plasma cortisol (ug /dl) level during different time intervals in the studied three groups
Regarding the intra-operative events, there were no statistically significant differences among the three groups regarding the mean intra- abdominal pressure and the mean duration of pneumoperitoneum (P > 0.05) (). Intra-operative requirement of propofol was highly statistically significant in group S compared to both groups C and M (P < 0.001) ().
Table 3. Intra- operative conditions and recovery characteristics in the studied three groups
When the three groups were compared for the parameters of recovery; extubation time and time to response to verbal commands had statistically significant longer times in group M compared to both groups C and S (P < 0.001) (). There was no statistically significant difference in extubation time and time to response to verbal commands between group C and group S (P > 0.05) ().
Regarding postoperative a dverse events, group S showed higher incidence of shivering, PONV and post-operative agitation compared to groups C and M but with no statistically significant differences (p > 0.05) (). Also, group M showed higher incidence of patient sedation score (5.7%) compared to groups C and S but not statistically significant (P > 0.05) ().
Table 4. Postoperative adverse events in the studied three groups
Referring to post-operative pain, pain scores were statistically significant higher in group S (Control group) compared to both groups C and M at the first 2 hours post-operative where as P value = 0.024, 0.019, respectively. Post-operative pain scores did not differ significantly among the three groups at 4, 6, 8, 10 and 12 post-operative hours (). However, analgesic consumptions during the first 24 hours post-operative was statistically significant higher in group S compared to both groups C and M (P < 0.05) (). The total post-operative analgesic consumption showed no statistically significant differences between the two studied groups. Also, time to first analgesic requirement was statistically significant longer in the two studied groups compared to the control group ().
Table 5. Post-operative analgesic consumption in the three studied groups
4. Discussion
The present study confirmed that preoperative I.V. administration of either clonidine or magnesium sulfate had attenuated the hemodynamic stress response to pneumo-peritoneum, suppressed the elevation of the stress hormone plasma cortisol level, reduced postoperative pain with less consumption of post-operative analgesics and without increased incidence of post-operative side effects following laparoscopic cholecystectomy. Clonidine was superior than MgSo4 regarding better intra-operative control of heart rate and earlier recovery criteria.
Importantly, the present study used an objective qualitative measure of anesthetic state (BIS) to guide anesthetic requirements and to determine end-points [Citation8], and measured the stress hormone serum cortisol level to evaluate the possible mechanism of action of both clonidine and magnesium sulfate in obtunding stress responses of laparoscopic cholecystectomy.
Altan and Colleagues used clonidine 3 µg/kg intravenously over a period of 15 minutes before induction and 2 µg/kg /hour by continuous infusion intra-operatively. They observed frequent episodes of bradycardia and hypotension in their study [Citation9].
Kulka and colleagues observed similar incidences of bradycardia and hypotension in their study [Citation10]. Based on their observations, we administered clonidine 3 µg/kg I.V. 15 minutes before induction only.
Also, Elsharnouby and Elsharnouby used magnesium sulfate 40 mg/kg I.V. over a period of 15 minutes before induction and 15 mg/kg/hour by continuous infusion intra-operatively. They noticed more episodes of severe hypotension [Citation11]. In the present study, we reduced the dose to 30 mg/kg before induction only. The dose selection in the present study for both drugs resulted in a steady and smooth reduction of heart rate and MAP with no episodes of bradycardia and hypotension.
Clonidine, a selective α2- adrenergic agonist, has desirable actions like anxiolysis, sedation, analgesia, anti-emesis, and anti-shivering . It inhibits catecholamine and vasopressin-mediated increase in systemic vascular resistance (SVR) caused by pneumoperitoneum [Citation6]. Numerous studies using clonidine found effective prevention of hemodynamic derangement because of intubation and during laparoscopic cholecystectomy [Citation12,Citation13]. However, higher doses of clonidine resulted in significant bradycardia and hypotension [Citation14].
Magnesium sulfate has shown to reduce the plasma catecholamines and vasopressin levels, thus contributing to its obtunding effect on sympatho-adrenal hemodynamic stress response and has also been shown to have a vasodilatory action, thus contributing to the reduction of blood pressure [Citation7].
The present study showed that clonidine has a better control of H.R. as compared to magnesium sulfate. However, the H.R. in magnesium sulfate group never increased more than the control group. Contradiction to our study, Mahajan and colleagues observed that the laryngoscopy-induced haemodynamic variation was better controlled with magnesium sulfate while maintaining a BIS of 40–50 [Citation15] .
Clonidine acts on central α-adrenoceptors and reduce plasma concentrations of cortisol and adrenocorticotrophic hormone in healthy adults [Citation6]. Masala et al. reported that I.V. infusion of clonidine suppressed the response of sympathetic system and the elevation of plasma cortisol concentration in surgery for chronic sinusitis [Citation2]. However, other studies showed that administration of clonidine depressed the responses of sympathetic systems but could not blunt the elevation of plasma cortisol concentration in pelvic and breast surgeries [Citation8,Citation9].
Yotsui stated that administration of clonidine can not suppress the responses of the hypothalamic-pituitary-adrenal axis to surgical stress, except in minor surgeries [Citation16]. Also, Joris etal., used 8 ug/kg of clonidine which significantly reduced the concentration of catecholamines but not vasopressin or plasma cortisol concentration [Citation17]. Differences in species, route of administration, time intervals and doses may explain these contradictions.
The present study showed that both clonidine and magnesium sulfate has attenuated the plasma cortisol level while in the control group, the plasma cortisol level increased after pneumoperitoneum and at the end of surgery compared with the two studied groups. The main and most reliable peripheral hormones that correlate well with the extent of the surgical trauma are cortisol and caticholamines . In this light, this study investigated the suitability of the studied two drugs (clonidine and magnesium sulfate) for ameliorating the body response to the wounds of laparoscopic cholecystectomy.
Our results showed that both clonidine and magnesium sulfate have better postoperative pain relief with lower consumption of rescue analgesics than in the control group. Safe management of post-operative pain represents a unique challenge and multimodal analgesia is usually implemented to reduce both inhalational anesthetics and opioid requirements with their predicted side effects. The perioperative use of clonidine and magnesium sulfate have shown to reduce postoperative pain as well as postoperative analgesic consumption [Citation18–20]. Clonidine, being a centrally acting α2 agonist, blocks the central sympathetic system [Citation9] and this explains its better control of hemodynamics and its analgesic sparing effects. The analgesic properties of magnesium sulfate are are mainly attributed to its N-Methyl-D-aspartate (NMDA) receptor antagonist effect, besides it regulates calcium influx into the cell. The peripheral abundancy of glutamate receptors allowed the use of peripheral NMDA receptor antagonists such as MgSO4 to alleviate pain [Citation21].
The present study showed that recovery time was significantly prolonged in patients receiving magnesium sulphate compared to the other two groups, which may be due to CNS depressant effect of magnesium sulphate. Peck and Meltzer [Citation22] in their study observed a similar state in patients subjected to herniorhaphy after magnesium sulphate infusion. However, Aldrete and Vazeery [Citation23] suggested that this was actually sleep-like state caused by cerebral hypoxia from progressive respiratory and cardiac depression.
5. Limitations
The present study has some limitations: First, we used fixed doses of the study drugs. Second, we only observed cortisol level changes till 24 hours after surgery in a limited time points. Third, to evaluate the stress response, we had to measure growth hormone, glucagone, catecholamines and other markers, which represent the stress response to anesthesia and surgery like blood glucose level. Finally, we did not measure serum magnesium level to accurately detect its optimum dose.
6. Conclusions
To conclude, both clonidine and magnesium sulfate are useful anesthetic adjuvants which can set the hemodynamics to a lower level and prevent swinging changes, reduce serum cortisol level with subsequent abundance of stress response and reduce anesthetic and analgesic requirements in laparoscopic cholecystectomy operations but clonidine has a superior intra-operative H.R. control and better recovery profile.
Financial support and sponsorship
Nil.
Disclosure statement
The Author declares that there is no conflict of interest.
References
- Jean LJ. Anaesthesia for laparoscopic surgery. In: Miller RD, editor. Anesthesia. 7th ed. Philadelphia: Churchill Livingstone, NewYork; 2010. p. 2185–2202.
- Sharma KC, Brandstetter RD, Brensilver JM, et al. Cardiopulmonary physiology and patho -physiology as a consequence of laparoscopic surgery. Chest. 1996;110(3):810–815.
- Larsen JF, Svendsen FM, Pedersen V. Randomized clinical trial of the effect of pneumoperitoneum on cardiac function and haemodynamics during laparoscopic cholecystectomy. Br.J.Surg. 2004;91(7):848–854.
- Koivusalo AM, Scheinin M, Tikkanen I, et al. Effects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand. 1998;42(5):510–517.
- Aho M, Scheinin M, Lehtinen AM, et al. Intramuscularly administered dexmedetomidine attenuates hemodynamic and stress hormone responses to gynecologic laparoscopy. Anesth Analg. 1992;75(6):932–939.
- Hazra R, Manjunatha S, Manuar M, et al. Comparison of the effects of intravenously administered dexmedetomidine with clonidineon hemodynamic responses during laparoscopic cholecystectomy. Anaesth Pain Intensive Care. 2014;18:25–30.
- Jee D, Lee D, Yun S, et al. Magnesium sulfate attenuates arterial pressure increase during laparoscopic cholecystectomy. Br.J.Anaesth. 2009;103(4):484–489.
- Khafagy HF, Ebied RS, Osman ES, et al. Perioperative effects of various anesthetic adjuvants with TIVA guided by bispectral index. Korean J Anesthesiol. 2012;63(2):113–119.
- Altan A, Turgut N, Yildiz F, et al. Effects of magnesium sulphate and clonidine on propofol consumption,haemodynamics and post-operative recovery. Br.J.Anaesth. 2005;94(4):438–441.
- Kulka PJ, Tryba M, Sczepanski U, et al. Does clonidine modify the hypnotic effect of propofol. Anaesthetist. 1993;42:630–637.
- Elsharnouby NM, Elsharnouby MM. Magnesium sulphate as a technique of hypotensive anaesthesia. Br.J.Anaesth. 2006;96(6):727–731.
- Singh SW, Arora K. Effect of oral clonidine premedication on perioperative haemodynamic response and post-operative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2011;55(1):26–30.
- Tripathi DC, Shah KS, Dubey SR, et al. Hemodynamic stress response during laparoscopic cholecystectomy: effect of two different doses of intravenous clonidine premedication. J Anaesthesiol Clin Pharmacol. 2011;27(4):475–480.
- Ray M, Bhattacharjee DP, Hazra B, et al. Effect of clonidine and magnesium sulphate on anesthetic consumption, hemodynamics,and post operative recovery:A comparative study. INDIAN J ANESTH. 2010;54(2):137–141.
- Mahajan L, Kaur M, Gupta R, et al. Attenuation of the pressor responses to laryngoscopy and endotracheal intubation with intravenous dexmedetomidine versus magnesium sulphate under bispectral index-controlled anaesthesia:A placebo-controlled prospective randomized trial. Indian J Anaesth. 2018;62(5):337–343.
- Yotsui T. Clonidine premedication prevents sympathetic hyper activity but does not prevent hypothalamo-pituitary-adrenocortical responses in patients undergoing laparoscopic cholecystectomy. J.Anesth. 2001;15(2):78–82.
- Joris JL, Chiche JD, Canivet JL, et al. Hemodynamic changes induced by laparoscopy and their endocrine correlates:Effects of clonidine. J Am Coll Cardiol. 1998;32(5):1389–1396.
- Fairbanks CA, Stone LS, Kitto KF, et al. α2C-adrenergic receptors mediate spinal analgesia and adrenergic-opioid synergy. J.Pharmacol.Exp.Ther. 2002;300(1):282–290.
- Anjum N, Tabish H, Debdas S, et al. Effects of dexmedetomidine and clonidine as propofol adjuvants on intra-operative hemodynamics and recovery profiles in patients undergoing laparoscopic cholecystectomy:A prospective randomized comparative study. Avicenna J Med. 2015;5(3):67–73.
- Telci L, Esen F, Akcora D, et al. Evaluation of effects of magnesium sulphate in reducing intraoperative anesthetic requirements. Br.J.Anesth. 2002;89(4):594–598.
- Revez JA, Glass PSA, and Lubarsky DA. Nonbarbiturates intravenous anesthetics .ANESTHESIA. In: Miller RD, Cucchiara RF, and Miller RD Jr, et al., editors. Savarese JJ.Philadelphia. 5th edition ed. Philadelphia: Churchill Livingstone; 2000. p. 228–272.
- Peck CH, Meltzer SJ. Anesthesia in human beings by intravenous administration of magnesium sulphate. Jama. 1916;67(16):1131–1133.
- Aldrete JA, Vazeery A. Is magnesium sulphate an anesthetic. Anesth Analg. 1989;68(2):186–187.