Abstract
The aim of this in-silico study was to compare stress distributions in implants and zirconia frameworks of mandibular and maxillary implant-supported crowns. For comparison, vertical and oblique loading forces were used. Three-dimensional finite-element implant models of a mandibular section of bone (D2) and a maxillary section of bone (D4) with missing second molars and their zirconium-based superstructures were used. Zimmer dental implants of 13 mm in length and 4.7 mm in diameter were modelled. A load of 200 N was applied toward vertical and oblique (30° to the vertical) directions. Maximum and minimum von Mises stress values of the implants and the zirconia framework were calculated. The highest stress value was concentrated in the zirconia framework of the maxillary implant-supported model with the oblique loading force (301.17 MPa). The lowest stress value was concentrated in the mandibular implant-supported model. And the stress values in the maxilla were higher than in the mandible. The maxilla (D4) showed higher stress values than in the mandible (D2), because the trabecular bone is weaker and less resistant to deformation than the cortical bone. Stress values with oblique loading forces were higher than with vertical loading forces. Because of the high Young's modulus of zirconia (low elastic properties), zirconia frameworks showed higher stress values than the implants.
| Abbreviations | ||
| 3D | = | three dimensional |
| D2 | = | mandibular section of bone |
| D4 | = | maxillary section of bone |
| FE | = | finite element |
| FPDs | = | fixed partial dentures |
| Y-TZP | = | yttrium oxide partially stabilized |
Introduction
Use of dental implants for replacing missing teeth is now a widely recognized and practised treatment method.[Citation1] Implants have various designs, which affect their potential long-term success.[Citation2,Citation3] Implants should have anatomically correct contours and replicate the optical properties of a natural tooth, including the cervical area corresponding to the crown–root junction.[Citation2,Citation4]
When inserting an implant into the maxilla and mandible, a clinician should know that the maxilla and mandible show different physical characteristics in terms of structure and density. The maxilla is more spongy than the mandible or the mandible is more rigid than the maxilla. The mandible is said to have D2 bone quality and the maxilla has D4 bone quality.[Citation5]
The choice of framework is important in use in clinical dental implant-supported prosthesis. Frequently, in practice metal–ceramic combinations are used. All-ceramic restorations cannot be used for implant-supported prosthesis, because ceramics are brittle and susceptible to failure beyond a critical stress, which is dependent on the internal and surface flaw distributions, and their fracture problems have not been solved completely.[Citation6] In recent years, Y-TZP (yttrium oxide partially stabilized) frameworks are frequently used in dental implant-supported prosthesis due to their superior durability and aesthetics. In our study, we used a Y-TZP framework for this reason.[Citation7,Citation8]
Y-TZP zirconia is a recent core material for all-ceramic fixed partial dentures. This oxide ceramic was first used biomedically in orthopaedics for total hip replacements.[Citation9] Its use was successful because of its high-grade mechanical properties.[Citation10,Citation11] Specifically, Y-TZP shows superior strength, better mechanical performance, high fracture resistance, more abrasion resistance, colour stability and aesthetics than other all-ceramic cores. Additionally, oxide ceramics generally exhibit high biocompatibility with low bacterial surface adhesion and reduced thermal conductivity.[Citation10,Citation12]
The flexural strength of Y-TZP is over 1000 MPa, its fracture toughness is up to 10 MPa/m0.5 (fracture toughness unit) and its Young's modulus value is ∼210 GPa, making Y-TZP suitable for all all-ceramic bridges, even those in the posterior region requiring a high degree of strength.[Citation10,Citation13] Because their successful use depends on the stress applied and the physical properties of the materials used, dental materials must be evaluated under compressive loading to determine their fatigue strength. Three-dimensional (3D) finite-element (FE) analysis has been used extensively in dental biomechanical studies to produce detailed and animate or inanimate structures.[Citation14–20] The von Mises stress is a combination of normal and shear stresses occurring in all directions. This stress is important in examining restorative materials and tooth tissue damage that may occur.[Citation21]
The aim of this study was to compare the stress values in implants and zirconia frameworks of mandibular and maxillary implant-supported crowns.
Materials and methods
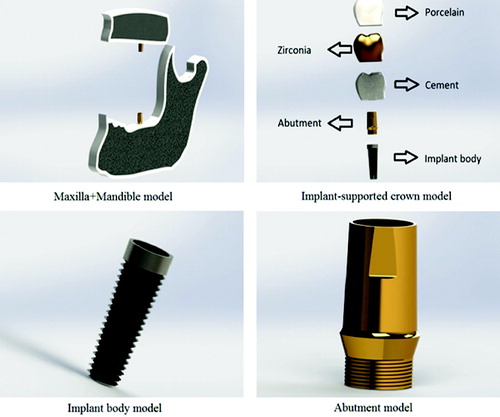
In this in-silico study, 3D FE models of maxillary and mandibular sections of bone with a missing second molar tooth were created. 3D tetrahedral structural solid models were used to create the bone, implant (implant body + abutment), framework and occlusal surface materials (). The maxillary bone was modelled as a cancellous core D4 bone surrounded by a 1-mm-thick cortical layer in the upper part. The mandibular bone was modelled as a cancellous core D2 bone surrounded by a 2-mm-thick cortical layer in the upper part. The crowns consisted of framework material and porcelain. The length and diameter of the crowns were 8 and 6 mm, respectively. Two solid 4.7 × 13 mm screw-type dental implant systems (Zimmer Dental, Carlsbad, CA) were selected for this study. The frameworks were developed according to the manufacturer's instructions on Y-TZP coping (NobelProcera, NobelBiocare AB, Goteborg, Sweden). The design of the frameworks respects the anatomical form of the final restoration, with an occlusal veneering thickness of 1–2 mm. The frameworks were customized with a minimum thickness of 0.8 mm. Feldspathic porcelain (Ceramco II, Dentsply, Burlington, NJ) was used for the occlusal surfaces.
lists the Young's modules and Poisson ratios of cortical bone (D2),[Citation22] spongious bone (D4),[Citation22] titanium (implant body + abutment),[Citation22] zirconia,[Citation10] porcelain [Citation23] and cement.[Citation24] The vertical and oblique (30° to the vertical) load applied in the model was 200 N, based on the literature.[Citation25,Citation26]
Table 1. Poisson ratio and Young's modulus values of materials used in the study.
The geometry of the tooth models was compared with data from ‘Wheeler's dental anatomy, physiology and occlusion.’ [Citation27] The forces applied were static. Stress levels were calculated using von Mises stress values, which are appropriate for hard materials, such as implants, abutments, frameworks and porcelain.
To perform this study, we used an Intel Pentium D CPU 3.00-GHz processor, with a 250-GB hard disk and 3 GB of RAM. The computer was equipped with the Windows XP Professional operating system (ver. 2002 + Service Pack 3). FE stress analysis and 3D model creation were performed using a laser scanner (NextEngine, Inc., Santa Monica, CA, USA), 3D modelling software (Rhinoceros 4.0, McNeel North America, Seattle, WA, USA) and the stress analysis software (ANSYS Rel.6.0, ANSYS Inc., Houston, TX, USA).
In total, eight models were created. For each, the maximum and minimum von Mises stress values were calculated.
Results and discussion
FE analysis is a computer-based technique that calculates the behaviour of engineering structures and their strength numerically. With this technique, a structure is separated into many small simple blocks or elements. Then, the structure is fully [re]built by joining together these sets of elements; thus, the behaviour of the whole structure is described by an enormously large set of equations that actually describe the behaviour of individual elements joined together. The behaviour of the individual elements is evaluated using computer software. Thus, the stresses of all parts of the structure are calculated.[Citation1,Citation28] 3D FE analyses are preferred to 2D techniques because they present an actual representation of stress behaviours on the supporting bone.[Citation2,Citation29]
In our study, maximum and minimum von Mises stress values of the implants and zirconia frameworks of mandibular and maxillary implant-supported crowns were compared under the vertical and oblique occlusal loading forces. When making comparisons, maximum stress values were checked. In this way, eight models were created and each was compared with the others according to the maximum and minimum stresses.
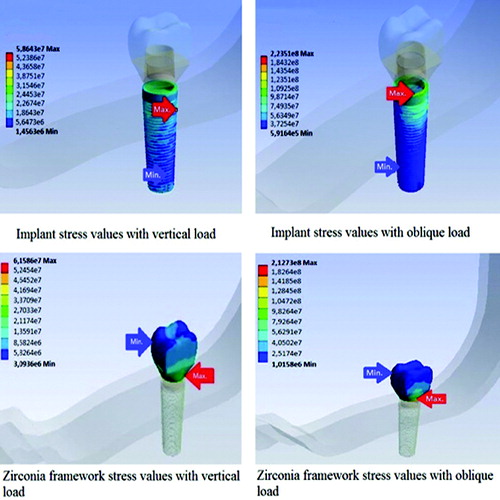
Stress analysis of the mandibular (D2 bone quality) implant-supported crown
The stress distribution within the implant and zirconia framework for the mandible is presented in . For both loading forces, maximum stresses were concentrated at the neck of the implant; however, minimum stresses were concentrated at the root apex of the implant. Moreover, while the maximum stress values for the zirconia frameworks were concentrated around the gingival area for both loading forces, minimum stresses were concentrated at the occlusal area of the zirconia frameworks. Maximum stresses were: 58.64 MPa for the implant with vertical loading, 223.51 MPa for the implant with oblique loading, 61.58 MPa for the zirconia framework with vertical loading and 212.73 MPa for the zirconia framework with oblique loading.
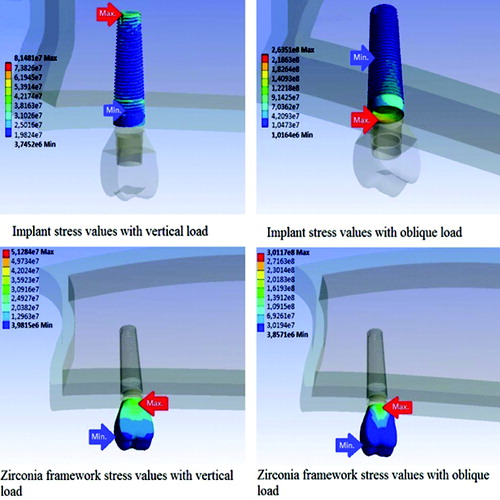
Stress analysis of the maxillary (D4 bone quality) implant-supported crown
presents the stress distribution within the implant and zirconia framework for the maxilla. For the vertical loading force, while maximum stresses were concentrated at the root apex of the implant, minimum stresses were concentrated at the neck; however, for oblique loading, while maximum stresses were concentrated at the neck of the implant, minimum stresses were concentrated at the root apex. Moreover, while the maximum stress values for the zirconia frameworks were concentrated around the gingival area for both loading forces, minimum stresses were concentrated at the occlusal area of the zirconia frameworks. Maximum stresses were: 81.48 MPa for the implant with vertical loading, 263.51 MPa for the implant with oblique loading, 51.28 MPa for the zirconia framework with vertical loading, and 301.17 MPa for the zirconia framework with oblique loading.
When the two groups were examined, the highest stress values were concentrated in the maxillary implant-supported model with the oblique loading force. The highest stress value was concentrated in the zirconia framework of the maxillary implant-supported model with the oblique loading force (301.17 MPa) (). The lowest stress values were concentrated in the mandibular implant-supported model.
These results suggest that the stress values with the oblique loading forces were higher than those with the vertical loading forces for both the implants and zirconia frameworks of the two groups. Also, the stress values in the maxilla were higher than those in the mandible. Moreover, the zirconia frameworks showed higher stress values than the implants ().
Table 2. Maximum and minimum stress values after force application (MPa).
Final remarks
Since the values obtained by FE stress analysis are variances that occur as a result of non-mathematical calculations, no statistical analysis was performed. The aim of this study was rather to review and analyse the values and stress distributions.
When FE analysis is applied to dental implants, it is important to consider oblique occlusal forces because the stress results will be more realistic in the structures, compared with only a vertical occlusal force.[Citation1,Citation30] Papavasiliou et al. [Citation31] showed that oblique loads could increase stresses 10-fold. Similarly, the results of the present study indicated that oblique loading forces caused the highest maximum stress values for both implants and zirconia frameworks.
Zarb and Schmitt [Citation32] stated that bone structure was the most important factor in selecting the most favourable treatment outcome in implant dentistry. Using a 3D FE analysis technique, Sevimay et al. [Citation23] investigated the effects of bone quality on the stress distribution in an implant and implant-supported crown. They showed the presence of lower stresses with D1 and D2 bone qualities and increased stresses for D3 and D4 bone qualities because trabecular bone was weaker and less resistant to deformation.[Citation1,Citation23] Thicker cortical bone (D2) reduces stress concentration around the implants.[Citation33,Citation34] The results of the present study are consistent with the studies above in terms of stress values being greater with trabecular bone (D4) than with cortical bone (D2).
Y-TZP has a high tensile strength (900–1200 MPa) and high Young's modulus (210,000 MPa). The Young's modulus of Y-TZP is higher than that of all dental alloys. Indeed, zirconia has a higher Young's modulus than titanium. In our study, the zirconia framework showed higher maximum stress values than the implant. The zirconia framework used in the present study was also used by Sannino et al. [Citation10], who found that maximum von Mises stress values were concentrated around the gingival area of the Y-TZP frameworks. Similarly, in our study, the maximum stress values were concentrated around the gingival area of the zirconia frameworks. Sannino et al. [Citation10] stated that the Y-TZP framework reduced the maximal and effective stresses. The much higher Young's modulus of Y-TZP allowed a more uniform distribution of stress within the framework, providing more efficient and durable load transfer.
When loading vertical and oblique forces to the maxillary implant-supported crown, respectively, von Mises stresses were concentrated at the different points of the implant (). For vertical loading, stresses were concentrated at the root apex of the implant; however, for oblique loading, stresses were concentrated at the neck of the implant of the implant. Therefore, we conclude that vertical forces are transmitted through the implant in the maxilla more effectively than are oblique forces. Thus, oblique forces may be more harmful to implants.[Citation31]
Further in vitro studies, such as stress distribution analysis, laboratory experiments and clinical studies, need to be conducted to determine stress distributions in different bone qualities of single and multi-unit fixed implant-supported prosthesis with different implant angles.
Conclusions
Within the limitations of this study and based on the results obtained, stress values in the maxilla (D4) were higher than in the mandible (D2), because, trabecular bone is weaker and less resistant to deformation than cortical bone. Stress values with oblique loading forces were higher than with vertical loading forces for both the implants and the zirconia frameworks. Zirconia frameworks showed higher stress values than the implants because of the high Young's modulus of zirconia. Vertical forces are transmitted through the implant in the maxilla more effectively than are oblique forces.
Acknowledgements
The authors thank Dr Emre Ari (Dicle University, Department of Mechanical Engineering) and Veysel Eratilla (Diyarbakir Oral and Dental Health Center) for their helpful advices on the FE analysis.
Disclosure statement
The authors have declared no conflict of interest.
References
- Desai SR, Singh R, Karthikeyan I, Reetika G. Three-dimensional finite element analysis of effect of prosthetic materials and short implant biomechanics on D4 bone under immediate loading. J Dent Implant. 2012;2:2–8.
- Ciftçi Y, Canay S. Stress distribution on the metal framework of the implant supported fixed prosthesis using different veneering materials. Int J Prosthodont. 2001;14:406–411.
- Kinni ME, Hokama SN, Caputo AA. Force transfer by osseointegrated implant devices. Int J Oral Maxillofac Implants. 1987;2:11–14.
- Tripodakis APD, Strub JR, Kappert HF, Witkowski S. Strength and mode of failure of single implant all-ceramic abutment restorations under static load. Int J Prosthodont. 1995;8:265–272.
- Morris HF, Ochi S, Crum P, Orenstein I, Pleiza R. Bone density: its influence on implant stability after uncovering. J Oral Implantol. 2003;29:263–269.
- Rekow ED, Silva NR, Coelho PG, Zhang Y, Guess P, Thompson VP. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011;90(8):937–952.
- Eraslan O, Inan O, Secilmis A. The effect of framework design on stress distribution in ımplant-supported FPDs: a 3-D FEM study. Eur J Dent. 2010;4:374–82.
- Tsumita M, Kokubo Y, Ohtsuka T, Nakayama Y, Fukushima S, Steyern PVV. [Influences of core frame design on the mechanical strength of posterior all-ceramic fixed partial dentures. Part 1. Two dimensional finite element analysis]. Tsurumi Shigaku. 2005;31:203–210. Japanese.
- Piconi C, Maccauro G, Muratori F, Brach Del Prever E. Alumina and zirconia ceramics in joint replacements. J Appl Biomater Biomech. 2003;1(1):19–32.
- Sannino G, Pozzi A, Schiavetti R, Barlattani A. Stress distribution on a three-unit implant-supported zirconia framework. A 3D finite element analysis and fatigue test. Oral Implantol. 2012;5:11–20.
- Raigrodski AJ, Chiche GJ. The safety and efficacy of anterior ceramic fixed partial dentures: a review of the literature. J Prosthet Dent. 2001;86:520–525.
- Mclean JW, Kedge M. The science and art of dental ceramics. In: Preston J, editor. Perspectives in dental ceramics. Chicago, IL: Quintessence; 1988. p. 13–40.
- Christel P, Meunier A, Heller M, Torre JP, Peille CN. Mechanical properties and short-term in vivo evaluation of yttrium-oxide-partially-stabilized zirconia. J Biomed Mater Res. 1989;23:45–61.
- Guven S, Akdogan M, Oz C, Dogan MS, Unal M, Unal S, Sahbaz C. Three-dimensional finite-element analysis of two ceramic inlay restorations with different cavity designs. Biotechnol Biotechnol Equip. 2015; 29(3):579–585.
- Guven S, Atalay Y, Asutay F, Ucan MC, Dundar S, Karaman T, Gunes N. Comparison of the effects of different loading locations on stresses transferred to straight and angled implant-supported zirconia frameworks: a finite element method study. Biotechnol Biotechnol Equip. 2015;29(4):684–690.
- Eyupoglu TA, Onal B, Erdilek N, Goren B, Ergucu Z. Molar dişlerde inley restorasyonların mekanik performansının incelenmesi: 3-boyutlu sonlu elemanlar analizi [Evaluation of the mechanical performance of inlay restorations on molar teeth: a 3-D finite element analysis]. GÜ Diş Hek Fak Derg. 2008;25:27–33. Turkish.
- Ausiello P, Rengo S, Davidson CL, Watts DC. Stress distributions in adhesively cemented ceramic and resin-composite Class II inlay restorations: a 3D-FEA study. Dent Mater. 2004;20:862–872.
- Bott B, Hannig M. Effect of different luting materials on the marginal adaptation of class I ceramic inlay restorations in vitro. Dent Mater. 2003;19:264–269.
- Dietschi D, Moor L. Evaluation of the marginal and internal adaptation of different ceramic and composite inlay systems after an in vitro fatigue test. J Adhes Dent. 1999;1:41–56.
- Shor A, Nicholls JI, Phillips KM, Libman WJ. Fatigue load of teeth restored with bonded direct composite and indirect ceramic inlays in MOD class II cavity preparations. Int J Prosthodont. 2003;16:64–69.
- Beer FP, Johnston ER. Mechanics of materials. New York: McGraw-Hill; 1981.
- Baggi L, Cappeloni I, Girolima MD, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry. J Prosthet Dent. 2008;100:422–431.
- Sevimay M, Turhan F, Kılıçarslan MA, Eskitaşçıoğlu G. Three dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J Prosthet Dent. 2005;93:227–234.
- O'Brien WJ, editor. Dental materials and their selection. 3rd ed. Hanover Park, IL: Quintessence Pub. Co. Inc.; 2002.
- Pellizzer EP, Verri FR, de Moraes SL, Falcón-Antenucci RM, de Carvalho PS, Noritomi PY. Influence of the implant diameter with different sizes of hexagon: analysis by 3-dimensional finite element method. J Oral Implantol. 2013;39(4):425–431.
- Morneburg TR, Pröschel PA. Predicted incidence of occlusal errors in centric closing around arbitrary axes. Int J Prosthodont. 2002;15(4):358–364.
- Ash MM, Nelson N. Wheeler's dental anatomy, physiology, and occlusion. 8th ed. Philadelphia (PA): Saunders; 2002.
- Pierrisnard L, Hure G, Barquins M, Chappard D. Two dental implants designed for immediate loading: a finite element analysis. Int J Oral Maxillofac. 2002;17:353–362.
- Darbar UR, Huggett R, Harrison A. Stress analysis techniques in complete dentures. J Dent. 1994;22:259–264.
- Holmgren EP, Seckinger RJ, Kilgren LM, Mante F. Evaluating parameters of osseointegrated dental implants using finite element analysis-a two-dimensional comparative study examining the effects of implant diameter, implant shape, and load direction. J Oral Implantol. 1998;24:80–88.
- Papavasiliou G, Kamposiora P, Bayne SC, Felton DA. Three-dimensional finite element analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading during function. J Prosthet Dent. 1996;76:633–640.
- Zarb GA, Schmitt A. Implant prosthodontic treatment options for the edentulous patient. J Oral Rehabil. 1995;22:61–71.
- Holmes DC, Loftus JT. Influence of bone quality on stress distribution for endosseous implants. J Oral Implantol. 1997;23:104–111.
- Kitagawa T, Tanimoto Y, Nemoto K, Aida M. Influence of cortical bone quality on stress distribution in bone around dental implant. Dent Mater J. 2005;24:219–224.