ABSTRACT
The aim of this study was to assess the prevalence of sinus-lifting procedures and survival rates of implants placed in the posterior maxilla. This retrospective chart review examined consecutive patients with tooth/teeth loss in the posterior maxilla between 2008 and 2012 treated with sinus lift, when needed, and implant insertion. Demographic variables, health status, residual alveolar bone height, augmentation types, the implant position, diameter and height, and implant failure, prosthesis types, and the marginal bone loss were recorded. The study included 302 patients at a mean age of 5.2 years, who received a total of 609 dental implants. A total of 380 (62.3%) implants were inserted in native areas, 203 (33.3%) ones in external sinus-lifted areas and 26 (4.4%) ones in internal lifted areas. The survival rate in native or internal lifted areas were 100% and 95.6% in external sinus lifted ones (10 implant failures/203 implants). Almost half of the implants were examined radiologically with a mean duration of 30 months and the mean marginal bone loss was 0.64 ± 1.2 mm. The results showed that the survival rates of native bone and the internal sinus lifting were slightly higher than that of external sinus lifting. Implants placed with sinus augmentation exhibited more marginal bone loss than implants in native bone.
Introduction
Implant placement is often challenging in the posterior maxilla due to pneumatization of maxillary sinuses, post-extraction bone resorption, and poor quality and quantity of alveolar bone. Bone resorption frequently causes severe loss of bone both vertically and horizontally which may limit the use of dental implants. When the distance between the sinus floor and the alveolar crest is less than 8–10 mm, sinus floor elevation may be indicated. Different augmentation procedures have been suggested for the placement of dental implants in resorbed posterior maxilla. There are two surgical treatment alternatives: sinus floor elevation with a lateral wall approach (external sinus floor elevation [ESFE]) and sinus floor elevation with a crestal approach (internal sinus floor elevation [ISFE]).[Citation1–6]
ESFE is the most common technique for elevating the sinus floor.[Citation3,Citation4] Although ESFE has some disadvantages such as higher cost, enhanced morbidity, increased risk of infection and prolonged treatment period, the long-term success of this technique has been reported even with the use of different types of graft materials and implants.[Citation6–9]
ISFE, which was described by Summers [Citation5] in 1994, is a relatively more convenient alternative; it can provide localized lifting of the sinus floor, which minimizes postsurgical complications. Reports on sinus augmentation techniques indicate that ISFE is also a predictable and efficacious technique for simultaneous implant placement.[Citation5] Both techniques can be applied in one-stage (simultaneous) or two-stage (delayed) protocols. However, the height of the residual bone is a key factor, which determines the protocol that should be applied.[Citation10] The one-stage protocol is selected in cases when the residual bone height is more than 5 mm and primary stability of the implant is achievable; then, sinus lifting and implant placement are implemented simultaneously. Otherwise, it is compulsory to use the delayed approach and place the implants after the healing period.[Citation7,Citation11] There are few studies that compare the ISFE and ESFE procedures. Therefore, the aim of this study was to estimate the prevalence of sinus lifting (external or internal) for the treatment of resorbed posterior maxilla and compare the implant survival rates of the ISFE and ESFE methods.
Subjects and methods
The patients included in the study consisted of those who presented at the clinics of Yeditepe University, Faculty of Dentistry, Department of Oral Surgery, between January 2008 and December 2012, for rehabilitation of the posterior maxilla. The patients were treated either with dental implants alone or in combination with a sinus-lifting procedure (internal or external), when needed. Retrospective evaluation was conducted in the oral surgery clinic by examining the digital record system in combination with the manual chart record system of the faculty. The study variables were divided into demographic, health status, anatomical and implant variables. The patient's age and gender were recorded as the demographic variables. Health status variables were classified according to the American Society of Anesthesiology (ASA) system (ASA I, ASA II or ASA III).[Citation12] Smokers (>10 cigarettes/day), uncontrolled diabetes patients and patients with bruxism habits were excluded from the study. Residual crestal bone height was recorded as an anatomical variable. Residual crestal bone height was grouped according to the typical technique used to augment the sinus relative to the height of the residual bone. Heights > 10 mm are most likely not involved in sinus augmentation, and those with 7–10 mm may have an ISFE technique, and those with <6 mm are most likely to have an ESFE procedure. Other anatomical variables included the implant position (second premolar, first molar and second molar), prosthesis types (single crown, fixed partial denture, complete denture and hybrid prosthesis) and the marginal bone level at the final radiological examination.
Data about the implant types (five different manufacturers), implant diameter and height, and implant failure were obtained from the patient record as the implant variables. The implant surfaces were OsseoSpeed (50.1%), hydroxyapatite (HA) coatings (44.3%) and sand-blasted large-grit, acid-etching (SLA) (5.6%). The length of the implants was defined as short (8–10 mm), medium (10–12 mm) or long (13–15 mm), and the diameter of the implants was defined as narrow (<3.7 mm), regular (3.7–4.8 mm) or wide (<4.8 mm).
Depending on the radiographically determined vertical dimension of the residual bone between the maxillary sinus floor and the alveolar crest, the implants had been inserted following one of the three specified surgical protocols.
External sinus floor elevation (ESFE)
This technique was applied in the cases when the vertical dimension of the residual bone was 6 mm or less. Following local anesthesia (Ultracain DS-Forte, 1/100,000 epinephrine, Sanofi-Aventis Deutschland GmbH, Germany), a midcrestal incision and vertical releasing incisions were performed. After a mucoperiosteal flap elevation, the lateral wall of the sinus was reflected. After the window preparation, the trap door and Schneiderian membrane were carefully elevated without perforation. Sinus cavity was filled with alloplastic material (deproteinized bovine bone) to provide the desired bone height. Implants were inserted simultaneously when performing the one-stage technique (simultaneous ESFE), whereas implants were inserted after a healing period of 7.5–10 months following sinus floor elevation when the two-stage technique (delayed ESFE) was used.
Internal sinus floor elevation (ISFE)
Under local anesthesia, midcrestal incision was performed and flaps were reflected. For the preparation of the recipient sites, either proper implant drills or osteotomes of increasing diameter were used. Finally, a sinus osteotome was used to fracture the sinus floor. Using a depth gauge which has a rounded, smooth tip, the Schneiderian membrane was elevated apically. To prevent membrane perforation, this procedure was carried out with special care. After the sinus was lifted, implants were inserted without using alloplastic material.
Prescribed medicines were antibiotics (amoxicillin and clavulanic acid [Augmentin BID 1 gr, Glaxo SmithKline, West Sussex, UK]), analgesics (naproxen sodium [Apranax 275 mg, Abdi Ibrahim, Istanbul, Turkey]) and mouth rinses (chlorhexidine [Klorhex Mouth Rinse, Drogsan, Ankara, Turkey]). For the whole ESFE group, nasal spray decongestant (xylometazoline hydrochloride [Otrivine nasal spray, Novartis, Luleburgaz, Turkey]) was also added for 5 days postoperatively. The sutures were removed 7–10 days postoperatively.
Radiological examination
The measurements were performed by a single observer who was blind to the samples evaluated. Intraobserver calibration was done by measurements performed prior to the study to obtain an intraclass correlation coefficient (ICC) of p < 0.01, indicating that the measurements can be repeated safely with a negligible error range. Orthopantomograph (OPTG) of the initial situation and at 6 months follow-up control were taken. Final radiological examination could not be performed in all the patients. The OPTGs attained were reviewed and analysed for marginal bone loss. The marginal bone level around implants was evaluated mesially and distally. The distance between a reference point on the implant and the bone level was measured using a magnifying lens (×7) with a measuring scale of 0.1 mm graduations.
Results and discussion
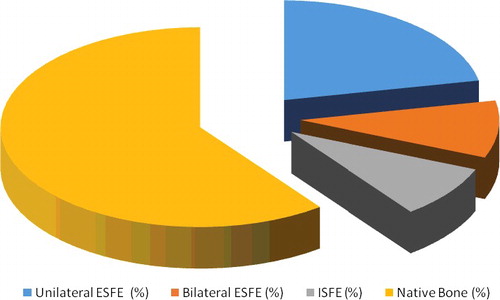
The study cohort consisted of 302 patients whose edentulous posterior maxillary sites were treated via insertion of 609 dental implants. shows the patients' demographic variables and health status. A total of 66 (21.8%) patients were scheduled to have a unilateral procedure, 28 (9.2%) patients, a bilateral procedure and 26 (8.6%) ones, with internal lifting (). summarizes the distribution of implants according to the anatomical and implant variables. The majority of the implants inserted in the augmented sinuses were in the position of the first molar (53.7%) followed by the second premolar (36.3%) and second molar (12.1%) (). The residual crest height in the ESFE group (33.3%) was between 3 and 6 mm above maxillary sinus and that in the ISFE group 26 (4.4%) was between 7 mm and 10 mm. While the narrow diameter implants (13.1%) were placed less often, the long- and medium-length ones were inserted at a high frequency (74.8%). The implant cumulative survival rate was 100% in native areas, 95.6% in the external sinus-lifted area (10 failures/203 implants) and 100% in the internal lifted area. A total of 4 (1.7%) failed implants were placed with one-stage ESFE and 6 (2.6%) were placed with two-stage ESFE ().
Table 1. Patients’ demographıc variables and health status.
Table 2. Distribution of implants according to study variables.
Final radiological examination could not be performed in all the patients due to drop-out. The mean duration for the 285 (46.7%) implants was 30 months. The mean marginal bone loss mesial to the implant and distal to the implant in the augmented region was 0.63 ± 1.2 mm and 0.65 ± 1.2 mm, respectively ().
Table 3. Marginal bone loss around the implants.
Various techniques have been proposed in order to provide the necessary bone dimension for the placement of implants. In cases of severely atrophic maxilla, ESFE is mostly suggested. However, some edentulous sites in the posterior maxilla show only limited resorption and in such cases, ISFE is suggested.[Citation13] Studies have shown that ISFE has some advantages including a shorter surgical duration and minimum postsurgical complications.[Citation13–16] Furthermore, the ISFE procedures can also improve the bone density and quality.[Citation17] However, fracturing the sinus floor during ISFE is intolerable for the patient due to mallet pressure. The overall prevalence of sinus augmentation within this study was 37.7%. This ratio should be well reviewed, because some patients may have chosen not to have implant treatment because of the need for a sinus augmentation procedure.
Existing the bone height is the determinative factor when evaluating patients as candidates for implant therapy.[Citation18–20] The selection of the sinus augmentation technique was dependent on the vertical dimension of the residual bone, from a two-step ESFE in cases with a severely resorbed maxilla to a less invasive osteotome technique when there was only limited resorption.[Citation3–5,Citation21–23] Block and Kent [Citation19] reported that when the height of bone between the alveolar crest and the floor of the sinus is ˂10 mm, sinus augmentation is necessary to support long implants and the subsequent prosthesis. Misch [Citation18] proposed four subantral treatment options for the posterior maxilla that vary depending on the available bone height. The results of this study are consistent with those studies. When the bone height was ˂10 mm (62.3%), implants were inserted without any additional procedures. Most of the implants were inserted in native bone, and the one-stage ESFE was the most frequently used technique among all the implants (19.4%), followed by the two-stage ESFE (13.9%) and ISFE (4.4%).
Maxillary sinus pneumatization can occur after the age of 20 or the eruption of the third molars and posterior tooth extraction. The inferior wall of the maxillary sinus is closest to the teeth in the molar region, which frequently causes loss of the thin bone between the alveolar socket and the sinus during extraction, resulting in an expansion of the sinus.[Citation24] The results from this study that sinus augmentation was more prevalent in molar sites (66.8%) than in premolar sites (33.2%) relate to this statement.
Recently, for the rehabilitation of the resorbed alveolar bone, narrow or short implants are frequently used.[Citation25–27] However, there is still a debate on the definition of a short implant in the literature. Some authors suggest 10 mm as the minimal length for predictable success; thus, they assume any implant less than 10 mm in length as short.[Citation25] Others define an implant of 10 mm in length also as a short implant.[Citation26] The same problem appears also with regard to the implant diameter.[Citation27] In our study, implants that are less than 10 mm in length were defined as short and implants less than 3.75 mm in diameter as narrow. Li et al. [Citation28] proposed that implant diameter greater than 4.0 mm and length greater than 9.0 mm are the ideal implant dimensions in the posterior maxilla. In this study, while the use of long and medium implants was highly prevalent, 37.9% and 36.9%, respectively, mostly medium implants were preferred in augmented area. It was regular implant diameters that were mostly used in the posterior maxilla (83.5%) and augmented region (83%). Due to the wide buccolingual nature of the posterior maxillary alveolar crest, surgeons place wider dental implants to enhance the biomechanics of the implants placed in augmented bone.
Poor bone quality or inadequate bone quantity due to the resorption of the alveolar bone after tooth extraction and subsequent pneumatization of the maxillary sinus affects both implant stability and, as a result, the implant success.[Citation18,Citation29] It has been suggested that implants placed in grafted areas show a higher risk of failure than implants placed in native maxillary bone. Recently, it was observed that implants inserted in grafted sinuses had a lower survival rate (86.1%) compared to implants placed in native bone (96.4%) after a 6-year follow-up period.[Citation17] On the contrary, according to other studies and various systematic reviews, survival rates for implants partially inserted in grafted maxillary sinuses are similar or even superior to those associated with implants placed in native maxillary areas.[Citation8,Citation9,Citation20,Citation21] A total survival rate of 99% for implants inserted with the ISFE approach after 6 months and 94% after 42–56 months was reported in another study.[Citation30] A review study of the ISFE approach reported survival rates of 95.7–96% after 2 years and 3 years, respectively.[Citation14] Uckan et al. [Citation31] obtained a survival rate of 100% with the ISFE technique. In the present study, the overall survival rate of the implant was 98.3%, and the survival rate of implants in the augmented region was 95.6% with a mean follow-up period of 30 months. The reason for the high success rate was associated with including implants placed in native bone. Implant survival may be more related to the amount of residual bone supporting the implant than to the grafted bone.[Citation32,Citation33] It has been suggested that a greater residual bone height is significantly associated with higher survival rates.[Citation34–37] In the present study, the success rate in the two-stage ESFE (92.9%) was lower than that in the one-stage ESFE (96.6%). This may be associated with the smaller surface area in contact with the bone. On the other hand, in a randomized controlled clinical trial that compared one- and two-stage ESFE, survival rates of 85.5% and 90.5% were reported, respectively.[Citation38] The survival rate of the implants inserted in sinuses augmented with the ISFE technique was between 88.6% and 100%.[Citation2,Citation14,Citation21]
Assessment by radiography is accepted as a reliable method to measure crestal bone loss to facilitate successful implant treatment. Intraoral radiography with a parallel technique is the recommended technique for assessing bony changes, despite the developments of extraoral radiographic systems.[Citation39] A number of clinical studies reported that a vertical marginal bone loss in the first year is 1–1.5 mm, followed by 0.1–0.2 mm yearly.[Citation40–42] The criteria proposed by Bryant and Zarb [Citation42] are widely used for the assessment of the success of dental implants, including the one that vertical bone loss should be less than 0.2 mm annually following the first year of function of an implant. A mean of 0.6 mm of radiographic bone loss within the first year of placement was reported without any significant bone loss in follow-up visits up to 5 years.[Citation43] Also similar results were reported after 8 years.[Citation44] In the present study, 46.7% of the patients were examined radiographically with up to 46 months follow-up and marginal bone loss was measured on OPTG. The results were in agreement with these previous studies and the mean mesial and distal bone changes at the 30 months interval were 0.48 ± 0.9 mm and 0.47 ± 0.8 mm, respectively. The implants placed in sites with ESFE or ISFE procedures manifested more marginal bone loss than implants placed in native bone. The mean mesial and distal marginal bone losses were recorded to be 0.63 ± 1.2 mm and 0.65 ± 1.2 mm, respectively. While the marginal bone loss for 40 implants was between 2 mm and 4 mm, extreme bone loss with a mean of 6.5 mm was only observed in three implants. Although the distortion was calculated for each implant, OPTG is a less reliable technique than the parallel technique.
It should be noted that this retrospective study had some limitations. They were the irregular follow-up periods and the small sample size. Further studies with larger sample groups are needed to obtain stronger evidence.
Conclusions
Within the limitations of this study, the results showed that almost half of the maxillary posterior implants were involved with a sinus augmentation procedure. As the residual alveolar bone height decreases, the prevalence of sinus augmentation was shown to increase. The survival rate of the native bone area was slightly higher than that in the external sinus-lifting group. Implants placed in augmented sites showed more marginal bone loss than implants placed in native bone. In the posterior maxilla, both the ESFE and ISFE techniques were reliable methods for implant treatment, and the survival rates of the implants in the ESFE group were similar to those in the ISFE group.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Woo I, Le BT. Maxillary sinus floor elevation: review of anatomy and two techniques. Implant Dent. 2004;13:28–32.
- Uckan S, Deniz K, Dayangac E, et al. Early implant survival in posterior maxilla with or without beta-tricalcium phosphate sinus floor graft. J Oral Maxillofac Surg. 2010;68:1642–1645.
- Tatum H Jr. Maxillary and sinus implant reconstruction. Dent Clin North Am. 1986;30:207–229.
- Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616.
- Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:152, 154–156, 158.
- Summers RB. The osteotome technique: part 3—less invasive methods of elevating the sinus floor. Compendium. 1994;15:698, 700, 702–704.
- Galindo-Moreno P, Avila G, Fernandez-Barbero JE, et al. Evaluation of sinus floor elevation using a composite bone graft mixture. Clinical Oral Implants Res. 2007;18:376–382.
- Pjetursson BE, Tan WC, Zwahlen M, et al. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35:216–240.
- Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8:328–343.
- Esfahanizadeh N, Rokn AR, Paknejad M, et al. Comparison of lateral window and osteotome techniques in sinus augmentation: histological and histomorphometric evaluation. J Dent (Tehran). 2012;9(3):237–246.
- Krennmair G, Krainhofner M, Schmid-Schwap M, et al. Maxillary sinus lift for single implant-supported restorations. Int J Oral Maxillofac Implants. 2007;22:351–358.
- ASA physical status classification system [Internet]. Schaumburg, IL: American Society of Anesthesiologists; c1995–2015 [cited: 2015 Aug 24]. Available: http://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system.
- Jensen OT, Shulman LB, Block MS, et al. Report of the sinus consensus conference of 1996. Int J Oral Maxillofac Implants. 1998;13:11–32.
- Emmerich D, Att W, Stappert C. Sinus floor elevation using osteotome: a systematic review and meta-analysis. J Periodontol. 2005;76:1237–1251.
- Toffler M. Site development in the posterior maxilla using osteocompression and apical alveolar displacement. Compend Contin Educ Dent. 2001;22:775–787.
- Toffler M. Minimally invasive sinus floor elevation procedures. N Y State Dent J. 2004;70:38–44.
- Barone A, Orlando B, Tonelli P, et al. Survival rate for implants placed in the posterior maxilla with and without sinus augmentation: a comparative cohort study. J Periodontol. 2011;82:219–226.
- Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol. 1987;4:49–58.
- Block MS, Kent JN. Sinus augmentation for dental implants: the use of autogenous bone. J Oral Maxillofac Surg. 1997;55:1281–1286.
- Olson JW, Dent CD, Morris HF, et al. Long-term assessment (5 to 71 months) of endosseous dental implants placed in the augmented maxillary sinus. Ann Periodontol. 2000;5:152–156.
- Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004;24:565–577.
- Kent JN, Block MS. Simultaneous maxillary sinus floor bone grafting and placement of hydroxylapatite-coated implants. J Oral Maxillofac Surg. 1989;47:238–242.
- Ferrigno N, Laureti M, Fanali S. Dental implants placement in conjunction with osteotome sinus floor elevation: a 12-year lifetable analysis from a prospective study on 588 ITI implants. Clin Oral Implants Res. 2006;17:194–205.
- Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants. 2008;23:48–56.
- Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: providing a rationale for the use of short implants. J Oral Implantol. 2007;33:257–266.
- Das Neves FD, Fones D, Bernardes SR, et al. Short implants an analysis of longitudinal studies. Int J Oral Maxillofac Implants. 2006;21:86–93.
- Mijiritsky E, Mazor Z, Lorean A, et al. Implant diameter and length influence on survival: interim results during the first 2 years of function of implants by a single manufacturer. Implant Dent. 2013;22:394–398.
- Li T, Kong L, Wang Y, et al. Selection of optimal dental implant diameter and length in type IV bone: a three-dimensional finite element analysis. Int J Oral Maxillofac Surg. 2009;38:1077–1083.
- Kan JY, Rungcharassaeng K, Kim J, et al. Factors affecting the survival of implants placed in grafted maxillary sinuses: a clinical report. J Prosthet Dent. 2002;87:485–489.
- Shalabi MM, Manders P, Mulder J, et al. A meta-analysis of clinical studies to estimate the 4.5 year survival rate of implants placed with the osteotome technique. Int J Oral Maxillofac Implants. 2007;22:110–116.
- Uckan S, Tamer Y, Deniz K. Survival rates of implants inserted in the maxillary sinus area by internal or external approach. Implant Dent. 2011;20:476–479.
- Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22:49–70.
- Lambert FE, Weber HP, Susarla SM, et al. Descriptive analysis of implant and prosthodontic survival rates with fixed implant-supported rehabilitations in the edentulous maxilla. J Periodontol. 2009;80:1220–1230.
- Rosen PS, Summers R, Mellado JR, et al. The bone added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants. 1999;14:853–858.
- Toffler M. Osteotome-mediated sinus floor elevation: a clinical report. Int J Oral Maxillofac Implants. 2004;19:266–273.
- Pjetursson BE, Rast C, Bragger U, et al. Maxillary sinus floor elevation using the (transalveolar) osteotome technique with or without grafting material. Part I: implant survival and patients' perception. Clin Oral Implants Res. 2009;20:667–676.
- Pjetursson BE, Ignjatovic D, Matuliene G, et al. Transalveolar maxillary sinus floor elevation using osteotomes with or without grafting material. Part II. Radiographic tissue remodeling. Clin Oral Implants Res. 2009;20:677–683.
- Wannfors K, Johansson B, Hallman M, et al. A prospective randomized study of 1- and 2-stage sinus inlay bone grafts: 1-year follow-up. Int J Oral Maxillofac Implants. 2000;15:625–632.
- De Smet E, Jacobs R, Gijbels F, et al. The accuracy and reliability of radiographic methods for the assessment of marginal bone level around oral implants. Dentomaxillofac Radiol. 2002;31:176–181.
- Albrektsson T, Zarb G, Worthington P, et al. The long term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25.
- Hartman GA, Cochran DL. Initial implant position determines the magnitude of crestal bone remodeling. J Periodontol. 2004;75:572–577.
- Bryant SR, Zarb GA. Crestal bone loss proximal to oral implants in older and younger adults. J Prosthet Dent. 2003;89:589–597.
- Weber HP, Crohin CC, Fiorellini JP. A 5 year prospective clinical and radiographic study of non-submerged dental implants. Clin Oral Implants Res. 2000;11:144–153.
- Buser D, Mericske-Stern R, Dula K, et al. Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 1999;13:153–161.