ABSTRACT
The aim of the present study was to assess the presence and course of the anterior loop in the mental foramen region according to age and gender, using cone beam computed tomography (CBCT). Both the right and left sides were retrospectively studied in 141 patients (n = 282). Axial, sagittal, cross-sectional and panoramic images were evaluated and three-dimensional images were reconstructed and evaluated as necessary. The morphology, course and length of the anterior loop were measured. The reliability and reproducibility were assessed based on the intraclass correlation coefficient (ICC) and the coefficient of variation. An anterior loop was found in about 86% of the scans. The mean anterior loop proximal edge was 3.15 mm and the mean distance between the buccal border of the anterior loop and buccal alveolar wall was 2.24 mm. The mean volume of the mandibular canal was 1140 mm3 and the mean volume of the anterior loop was 90 mm3. Statistically significant difference was found in male patients in terms of the canal and anterior loop volume (p < 0.05). A high prevalence of anterior loop was detected by CBCT imaging, with predominance in female patients. Clinicians should be careful during implant or bone surgery procedures to avoid possible complications, with special emphasis on patient age, using this imaging modality that involves use of less radiation.
Introduction
The inferior alveolar neurovascular bundle containing the inferior alveolar nerve is located in the mandibular canal of the lower jaw and leaves the canal from the mental foramen in the anterior wall of the premolar region of the alveolar bone. The inferior alveolar nerve forms the anterior loop (AL) of the mandibular canal in the anterior of the mental foramen when leaving and splits into two nerve branches: mental and incisive nerves.[Citation1] The mental branch innervates the skin and the mucous membrane of the lower lip and chin together with the adjacent buccal nerve and the vestibular gingiva of the mandibular anterior teeth, whereas the incisive branch innervates the anterior teeth, including the first premolar.[Citation2–4]
The end branches of the inferior alveolar nerve are critical for implant surgery of the anterior mandible, since injury to violation of mental or incisive branches may lead to neurosensory disturbance in the area of the lower lip.[Citation5] For that reason the position of the anterior loop limits the placement of dental implants in between the mental foramens, i.e. the interforaminal region. This anatomical structure is important not only for implant surgery, but also for open reduction of a mandibular fracture, or orthognathic surgery.[Citation6–9] The interforaminal region is usually known as the safest area for dental implant surgery. Therefore, panoramic radiographs are used as the single preoperative diagnostic or radiographic tool for implant planning. However, panoramic radiographs have some disadvantages: the magnification in the anterior region is small on panoramic radiographs, there are often distortions and magnifications of the anatomical structures, which result in either over- or underestimation of the real size of the anatomical structures.[Citation10,Citation11]
In the past, computer tomography (CT) with special dental software programs was used to determine the anatomical structures for dental implant planning, and it has been recognized as a useful imaging device.[Citation12] Today, cone beam CT (CBCT), as a three-dimensional dental diagnostic tool, provides reliable data for correct distance measurements and can be used to obtain detailed information for three-dimensional analysis of the region of interest.[Citation13] Currently, the use of CBCT imaging is increasing, especially in dental implant planning as a result of low cost, fast image acquisition and lower exposure dose compared to CT.[Citation14]
Different studies have focused on detection of the incisive canal (IC), anterior loop of the mandibular canal, mental foramen and lingual foramen, using CBCT imaging,[Citation15–19] but, to our knowledge, no attempt has been made to study the visualization of the anterior loop according to both age and gender together, using this imaging modality. Thus, the aim of the present study was to assess the presence and course of the anterior loop in the mental foramen region according to the dental status, age and gender, using CBCT in a group of Turkish patients.
Subjects and methods
Subjects
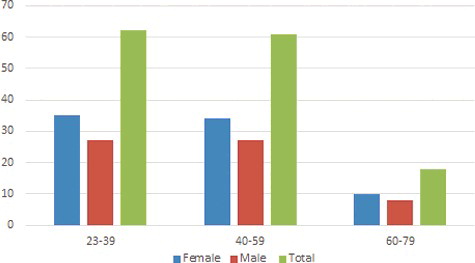
The study cohort comprised 141 subjects [79 (56%) female, 62 (44%) male] who had undergone CBCT imaging. CBCT images were retrospectively evaluated.
The average age of the 141 patients was 41.2 years with a standard deviation (SD) of 17.74 (range, 23–79 years). The mean age of the male patients was 40.9 (SD, 15.4; n = 79) years (range, 23–79 years), while the mean age of the female patients was 41.5 (SD, 17.36; n = 62) years (range, 27–71 years).
The study group was divided into two subgroups according to age and gender, as presented in . Age groups were classified as follows: 23 to 37, 38 to 51, 52 to 64 and 65 to 79 years. Patients with evidence of bone disease (especially osteoporosis), relevant drug consumption, skeletal asymmetries or trauma, congenital disorders, anamnesis of surgical procedures in the mental region and pathological disorders of the mandible as well as syndromic patients were excluded from the study.
The study protocol was carried out in accordance with the principles described in the Declaration of Helsinki, including all amendments and revisions. Only the investigators had access to the collected data. The institutional ethical review board of the faculty reviewed and approved the informed consent forms and the study. There was no preference for gender regarding the sample choice; however, only Turkish patients were included in the study. Only high-quality scans were used. Low-quality images, e.g. ones that contain scattering or insufficient accuracy of bony borders, were excluded.
CBCT imaging
CBCT scans were obtained using a Planmeca Promax 3D max (Helsinki, Finland) unit. Despite the fact that recent studies have indicated that small variations in head position do not influence measurement accuracy using three-dimensional CBCT [Citation20], each CBCT scan obtained in our clinics undergoes a strict, standardized scanning protocol. Patients were asked to stand in a vertical position, stabilized with a head band and chin support, and monitored to ensure that they remained motionless throughout the duration of the scan.
Scans of the patients were made at 96 kVp and 12 mA at different resolutions: 0.150 to 0.400 voxel sizes. The field of view was 10 cm in diameter and 5.5 cm in height. Slices were 1024 × 1024 pixels. All constructions and measurements were performed on a 21.3 in flat-panel colour-active matrix TFT (thin film transistor) medical display (NEC MultiSync MD215MG, Munchen, Germany) with a resolution of 2048 × 2560 at 75 Hz and 0.17 mm dot pitch operated at 11.9 bits.
Image evaluation
All CBCT images were retrospectively evaluated by a dentomaxillofacial radiologist and a periodontology consultant with five years of experience (H.E, N.B) using CBCT device software (Romexis 3.2, Helsinki, Finland). An interexaminer calibration based on the anatomic diagnosis of CBCT images had been previously performed to assess data reliability.
Axial, sagittal, cross-sectional and panoramic images were reconstructed for all mandibles and three-dimensional reconstructions were used as necessary ().
Figure 2. Three-dimensional CBCT (a), cross-sectional (b), panoramic reconstructed images (c) showing the mandibular canal and anterior loop.
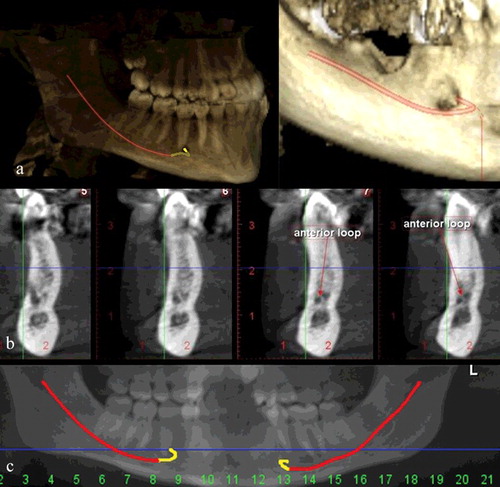
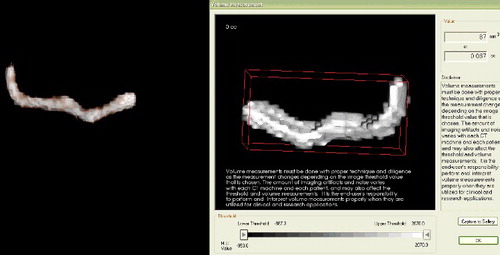
The presence, morphology, course and length of the anterior loop were determined. Where an anterior loop was present, four distances were also measured: the length from the medial margin of the mental foramen to the anterior loop proximal edge, the distance between the buccal border of the anterior loop and the buccal alveolar wall, the distance between the lingual border of the anterior loop and the lingual alveolar wall and the distance between the inferior border of the anterior loop and the inferior border of the mandible (). Additionally, the course of the mandibular canal together with AL was traced. The volumes of the mandibular canal and the anterior loop were measured using 3D Invivo software version 5.1.2 (Anatomage, San Jose, CA). After obtaining axial images from the CBCT data, they were exported in a DICOM (digital imaging and communications in medicine) file format with a 1024 × 1024 matrix and imported into the Invivo software. Three-dimensional surface representations were prepared from the DICOM images. Using this software, the volumes of the canal and the anterior loop were calculated by a dentomaxillofacial radiologist (M.M). The software allows the user to ‘sculpt out’ the desired volume from the three-dimensional structure, and, by adjusting the brightness and opacity values, to remove ‘unwanted’ voxels before calculating the final volume as described by the manufacturer ().
Figure 3. Cross-sectional (a) and sagittal (b) CBCT images showing the measurements for anterior loop morphology.
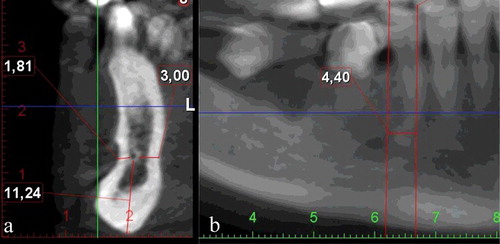
Figure 4. Volume of mandibular canal and anterior loop measured three-dimensionally (using 3D Invivo software).
All measurements were taken twice by the same observers and the mean values of all measurements were included in the statistical analysis. The observers also performed the study twice with an interval of two weeks to detect intra-observer variability. Moreover, before starting the radiographic examination in the study, the examiners were calibrated to recognize and identify the IC anatomy. For this purpose, a set of 50 CBCT images which were not included in the present study were used by observers for training. The examiners only examined the CBCTs and were blinded to any other patient data in the radiographic examination procedure.
Examiner reliability and statistical analysis
Statistical analyses were carried out using Statistical Package for the Social Sciences 12.0.1 (SPSS, Chicago, IL, USA). Intra- and inter-examiner validation measures were conducted. To assess intra-observer reliability, the Wilcoxon matched-pairs signed rank test was used for repeat -measurements. The inter-observer reliability was determined by the intraclass correlation coefficient (ICC) and the coefficient of variation (CV) [CV = (standard deviation/mean) × 100%]. ICC values range from 0 to 1. ICC values greater than 0.75 show good reliability, and the low CV demonstrates the precision error as an indicator for reproducibility.[Citation21] Pearson's chi-square test and Student's t-test were performed for statistical analysis of differences in age, gender, localization and measurements (p < 0.05).
Results and discussion
Intra-observer consistency
Repeated CBCT evaluation and measurements indicated no significant intra-observer difference for both observers (p > 0.05). The overall intra-observer consistency for observer 1 was rated at 87.6% and 93.2%, while the consistency for observer 2 was found to be 88.2% and 91.4% between the two evaluations and measurements, respectively. All measurements were found to be highly reproducible for both observers and there was no significant difference between the two measurements of the observers (p > 0.05).
Inter-observer consistency
shows the ICCs between Observer 1 and Observer 2, which ranged from 0.940 to 0.992. There was high inter-observer agreement, while a high ICC and a low CV demonstrated that the procedure was standardized between the evaluations and measurements of the observers. No statistical differences were found among the observers’ evaluations and measurements (p < 0.05). Observer 1 had higher intra-observer consistency, thus the mean values of this observer's evaluations and measurements were chosen for further analysis of the anterior loop.
Table 1. Inter-observer consistency of measurements.
Identification of anterior loop of mandibular nerve by CBCT examinations
Radiographic evaluation is a must in implant planning to avoid neurological damage during implant surgery in the anterior mandibular region. The most commonly seen complication related to implant surgery of this region is dysesthesia of the lower lip due to mental nerve injury.[Citation22] The risk of nerve injury after dental implant placement in the anterior mandibular region is 7%, if the dental implant is inserted within the 3 mm mesial to the anterior border of the mental foramen.[Citation23] However, the risk is reduced to 1%, if this distance is greater.[Citation24]
In the present study, an anterior loop in the mental region was detected in 86% (282 sides) of the scans. These results are in line with previous studies reporting that an anterior loop is identified by three-dimensional imaging in 71% to 88% of Japanese and Iranian patients and that this rate is higher when compared to panoramic radiographs.[Citation8,Citation18] In another study by Li et al. [Citation25], the prevalence of anterior loop was reported to be 83.1% in a group of patients from the Chinese population.
In our study, there was a statistically significant difference in the prevalence of an anterior loop depending on gender (p < 0.05), whereas no difference was found among the studied age groups (p > 0.05). The prevalence of an anterior loop in females (83.7%) was found to be higher than that in males (72.2%).
shows the correlations among age, gender and mean anterior loop measurement values. The mean length from the medial margin of the mental foramen to the anterior loop proximal edge ranged from 2.9 to 3.3 mm (mean, 3.15 mm), which is similar to the values ranging from 0.89 to 5.3 mm reported in the previous studies.[Citation25] In addition, there was good agreement between the length of the longest anterior loop measured in our study (12.4 mm) and values reported in other studies, 11 and 9 mm.[Citation21,Citation26] However, although the mean length of the anterior loop in our study was found to be similar to that reported by others, it would not be correct to identify an average safe area in the mesial mental foramen region due to the wide range of variation in the anterior loop length. Thus, CBCT of the mental foramen region must be performed to identify and correctly measure the anterior loop during the implant-planning process to avoid damage of the mental nerve.
Table 2. Mean values of anterior loop measurements (mm) according to age groups and gender.
In this study, the distances from the buccal border of the anterior loop to the buccal alveolar wall, from the lingual border of the anterior loop to the lingual alveolar wall and from the inferior border of the anterior loop to the inferior border of the mandible were also measured. The distance between the buccal border of the anterior loop and the buccal alveolar wall ranged from 1.9 to 2.54 mm (mean, 2.24 mm). The measurements did not differ significantly according to side or gender (p > 0.05).
The mean distance between the lingual border of the anterior loop and the lingual alveolar wall ranged from 3.8 to 4.9 mm (mean, 4.24 mm), and that of the distance between the inferior border of the anterior loop and the inferior border of the mandible ranged from 8.2 to 9.0 mm (mean, 8.63 mm). These measurements were statistically significant according to gender and age (p < 0.05). The male patients had higher measurements (p < 0.05) than the female patients in each age group (). This could be explained by the fact that the mandible is generally larger in volume in males, and that the vertical height and buccolingual width of the mandible is also greater in males than in females.[Citation26–29]
The volume of the mandibular canal and the anterior loop was also measured. shows the mean measurements of the variables according to age and sex. The difference between the measurements according to age group was not statistically significant (p > 0.05). The mean volume of the mandibular canal wall ranged from 1270 to 986 mm3 (mean, 1140 mm3) and that of the volume of the anterior loop ranged from 98 to 81 mm3 (mean, 90 mm3). These measurements were statistically significant according to gender (p < 0.05). The male patients had larger volumes (p < 0.05) than female patients in each age group ().
Table 3. Mean values (mm3) of anterior loop measurements according to age groups and gender.
Final remarks
Panoramic radiography is still the most commonly used imaging method in implant planning due to the fact that it is cheap and easily accessible. However, this rotational imaging method has some disadvantages, such as distortions, superimpositions and magnifications of the anatomical structures that prevent accurate measurements, especially in the anterior region. In some cases, it may not even be possible to accurately identify the mental foramen or the extension of the anterior loop.[Citation5] The vertical distance measurements in a panoramic radiograph are less reproducible than the horizontal ones,[Citation30] and there are differences between the images obtained with different panoramic units.[Citation11,Citation31] As a result, panoramic radiographs are considered unreliable in identifying the anterior loop of the mental nerve when compared with three-dimensional imaging.[Citation10] Previous studies have shown variable results to identify the anterior loop ranging from 11% to 40.2% with panoramic radiographs.[Citation32,Citation33]
Three-dimensional imaging modalities have been developed to resolve the limitations of two-dimensional imaging. Additionally, as a result of technological advances in the field of dental imaging, three-dimensional imaging techniques such as CBCT have become routinely used. Alternatively, multi-slice CT can also be used in the field of three-dimensional imaging of the dentomaxillofacial region. But, in general, CBCT is a technique which uses lower doses in scanning the maxillofacial region when compared with multi-slice CT.[Citation21,Citation34,Citation35] There are a lot of studies on evaluation of radiation dose of CBCT which support that the CBCT method uses lower doses than multi-slice CT.[Citation35–41] The effective dose of CBCT examination ranges from 13 to 479 μSv, depending on the device used.[Citation39,Citation41,Citation42] Therefore, CBCT can be considered a diagnostic tool as effective as multi-slice CT according to radiation dose levels. Therefore, CBCT can be preferred instead of multi-slice CT if three-dimensional imaging is necessary for dental implant planning.[Citation40] This condition allows CBCT to be used in the analysis of the dentomaxillofacial region and, especially, of variations in the anatomy.
To the best of our knowledge, no attempt has been made to measure the mandibular canal and anterior loop volume in the Turkish population, using this imaging modality. The results from our study revealed a higher volume of the mandibular canal and the anterior loop in males, with significant differences between genders in all age groups. The similar trend that was observed with regard to the distances from the lingual and inferior borders to the lingual alveolar wall and the inferior border of the mandible, could suggest that the shape and volume of the mandible might also affect the actual volume of the mandibular canal and anterior loop. However, further studies are needed in order to obtain more reliable results and verification.
Conclusions
In the studied cohort of Turkish patients, there was a high prevalence of anterior loop as detected by CBCT imaging, with predominance in female patients. Therefore, clinicians should be careful during implant or bone surgery procedures in the mandibular premolar region to avoid possible complications resulting from damage of the mandibular nerve. For this purpose, it is suitable to use the CBCT imaging method for implant planning to correctly identify the course of the mandibular nerve. Three-dimensional methods are a must to accurately view the anatomical structures. Considering the radiation dose levels, the CBCT imaging method should be preferred instead of multi-slice CT to determine the anatomical structures for implant planning.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bavitz JB, Harn SD, Hansen CA, et al. An anatomical study of mental neurovascular bundle-implant relationships. Int J Oral Maxillofac Implants. 1993;8:563–567.
- Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part II: Mandibular incisive canal, mental foramen and associated neurovascular bundles in relation with dental implantology. J Oral Maxillofac Res [Internet]. 2010 [cited 2015 Jun 27];1(1):e3. Available from: http://www.ejomr.org/JOMR/archives/2010/1/e3/e3ht.htm.
- Drake RL, Vogl AW, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia (PA): Churchill Livingstone; 2010. p. 1056–1060.
- Won SY, Kim DH, Yang HM, et al. Clinical and anatomical approach using Sihler's staining technique (whole mount nerve stain). Anat Cell Biol. 2011;44:1–7.
- Vujanovic-Eskenazi A, Valero-James JM, Sánchez-Garcés MA, et al. A retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and cone beam computerized tomography. Med Oral Patol Oral Cir Bucal. 2015;20:239–245.
- Hwang K, Lee WJ, Song YB, et al. Vulnerability of the inferior alveolar nerve and mental nerve during genioplasty: an anatomic study. J Craniofac Surg. 2005;16:10–14.
- Kim IS, Kim SG, Kim YK, et al. Position of the mental foramen in a Korean population: a clinical and radiographic study. Implant Dent. 2006;15:404–411.
- Uchida Y, Noguchi N, Goto M, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–750.
- Uchida Y, Yamashita Y, Goto M, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve when installing endosseous implants in the interforaminal region. J Oral Maxillofac Surg. 2007;65:1772–1779.
- Kuzmanovic DV, Payne AG, Kieser JA, et al. Anterior loop of the mental nerve: a morphological and radiographic study. Clin Oral Implants Res. 2003;14:464–471.
- Yim JH, Ryu DM, Lee BS, et al. Analysis of digitalized panorama and cone beam computed tomographic image distortion for the diagnosis of dental implant surgery. J Craniofac Surg. 2011;22:669–673.
- White SC, Heslop EW, Hollender LG, et al. American academy of oral and maxillofacial radiology, ad hoc committee on parameters of care. Parameters of radiologic care: an official report of the American academy of oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:498–511.
- Park HS, Lee YJ, Jeong SH, et al. Density of the alveolar and basal bones of the maxilla and the mandible. Am J Orthod Dentofacial Orthop. 2008;133:30–37.
- Nakagawa Y, Kobayashi K, Ishii H, et al. Preoperative application of limited cone bean computerized tomography as an assessment tool before minor oral surgery. In J Oral Maxillofac Surg. 2002;31:322–336.
- Makris N, Stamatakis H, Syriopoulos K, et al. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res. 2010;21:766–771.
- Pires CA, Bissada NF, Becker JJ, et al. Mandibular incisive canal: cone beam computed tomography. Clin Implant Dent Relat Res. 2012;14:67–73.
- Al-Ani O, Nambiar P, Ha KO, et al. Safe zone for bone harvesting from the interforaminal region of the mandible. Clin Oral Implants Res. 2013;24(Suppl A100):115–121.
- Parnia F, Moslehifard E, Hafezeqoran A, et al. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:420–425.
- Liang X, Jacobs R, Corpas LS, et al. Chronologic and geographic variability of neurovascular structures in the human mandible. Forensic Sci Int. 2009;190:24–32.
- Hassan B, van der Stelt P, Sanderink G. Accuracy of three dimensional measurements obtained from cone beam computed tomography surface-rendered images for cephalometric analysis: influence of patient scanning position. Eur J Orthod. 2009;31:129–134.
- SEDENTEXCT Project. Radiation protection: Cone beam CT for dental and maxillofacial radiology. Evidence-based guidelines [Internet]. Manchester: SEDENTEXCT project; c2007-2015. revised 2010 Oct 31 [cited 2015 Jun 27]. Available from: http://www.sedentexct.eu/files/radiation_protection_172.pdf.
- Vazquez L, Saulacic N, Belser U, et al. Efficacy of panoramic radiographs in the consecutively treated patients. Clin Oral Implants Res. 2008;19:81–85.
- Wismeijer D, van Waas MA, Vermeeren JI, et al. Patients' perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg. 1997;35:254–259.
- Walton JN. Altered sensation associated with implants in the anterior mandible: a prospective study. J Prosthet Dent. 2000;83:443–449.
- Li X, Jin ZK, Zhao H, et al. The prevalence, length and position of the anterior loop of the inferior alveolar nerve in Chinese, assessed by spiral computed tomography. Surg Radiol Anat. 2013;35:823–830.
- Kalender A, Orhan K, Aksoy U. Evaluation of the mental foramen and accessory mental foramen in Turkish patients using cone-beam computed tomography images reconstructed from a volumetric rendering program. Clin Anat. 2012;25:584–592.
- Chrcanovic BR, Abreu MH, Custódio AL. Morphological variation in dentate and edentulous human mandibles. Surg Radiol Anat. 2011;33:203–213.
- Apinhasmit W, Methathrathip D, Chompoopong S, et al. Mental foramen in Thais: an anatomical variation related to gender and side. Surg Radiol Anat. 2006;28:529–533.
- Merrot O, Vacher C, Merrot S, et al. Changes in the edentate mandible in the elderly. Surg Radiol Anat. 2005;27:265–270.
- Schulze R, Krummenauer F, Schalldach F, et al. Precision and accuracy of measurements in digital panoramic radiography. Dentomaxillofac Radiol. 2000;29:52–56.
- Kaya Y, Sencimen M, Sahin S, et al. Retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–925.
- Jacobs R, Mraiwa N, Van Steenberghe D, et al. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26:329–333.
- Ngeow WC, Dionysius DD, Ishak H, et al. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–237.
- De Vos W, Casselman J, Swennen GRJ. Cone-beam computerized tomography (CBCT) ımaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg. 2009;38:609–625.
- Eren H, Gorgun S. Evaluation of effective dose with two-dimensional and three-dimensional dental imaging devices. J Contemp Dent. 2015;5(2):80–85.
- Loubele M, Bogaerts R, Van Dijck E, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71:461–468.
- Jeong D, Lee S, Huh K, et al. Comparison of effective dose for ımaging of mandible between multi-detector CT and cone-beam CT. Imaging Sci Dent. 2012;42:65–70.
- Anson CM Chau, Fung K. Comparison of radiation dose for ımplant ımaging using conventional spiral tomography, computed tomography, and cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:559–565.
- Frederiksen NL, Benson BW, Sokolowski TW. Effective dose and risk assessment from film tomography used for dental ımplant diagnostics. Dentomaxillofac Radiol. 1994;23:123–127.
- Ludlow JB, Davies-Ludlow LE, Brooks SL, et al. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226.
- Brenner DJ, Hall EJ. Computed tomography — an ıncreasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284.
- Assaf M, Gharbyah AZ. Accuracy of computerized vertical measurements on digital orthopantomographs: posterior mandibular region. J Clin Imaging Sci [Internet]. 2014 [ cited 2015 Jun 27];4:7. Available from: http://www.clinicalimagingscience.org/text.asp?2014/4/2/7/148274