ABSTRACT
The standardized hemoglobin A1c (HbA1c) test is an essential tool to evaluate the glycaemic control and the diabetes care. The aim of our study was to evaluate and compare the actual HbA1c level in a cohort of Bulgarian patients with type 1 diabetes aged 0–19 years in two consecutive national studies, in 2012 and 2014. We used a standardized method for HbA1c high performance liquid chromatography (HPLC). Тhe survey was conducted in 11 paediatric endocrinology practices in Bulgaria. Overall 829 patients with type 1 diabetes participated in the first study, 422 boys and 407 girls, aged 11.9 ± 4.2 years. The second study included 498 patients: 261 boys and 237 girls, aged 11.6 ± 4.1 years. The mean HbA1c level for the patients studied in 2014 (8.42 ± 1.69%) was significantly lower compared to that in the patients studied in 2012 (8.93 ± 1.98%, p < 0.001). Significantly more patients in the second study (36%) showed optimal control with HbA1c < 7.5% (p < 0.05) compared to those from the first one (24.9%). Teenagers in both studies had higher HbA1c levels compared to the other age groups: 9.19 ± 2.11% in 2012 and 8.8 ± 1.87% in 2014. We found significant differences in the HbA1c levels between the different centres in Bulgaria (from 7.92% to 9.95% in 2012 and from 7.42% to 9.13% in 2014). All age groups, except the teenagers showed improvement in the glycemic control in the second study as a result of continuous and structured education of the patients and their families.
Introduction
The number of children and adolescents with type 1 diabetes is rapidly increasing in the last decades. At the same time, there is a trend towards diabetes being diagnosed at a younger age [Citation1–4]. Frequent and accurate monitoring of blood glucose levels is essential for the optimal adjustment of the insulin dose to the carbohydrate intake and/or physical activity [Citation5–7].
The standardized hemoglobin A1c (HbA1c) test is an essential tool to evaluate the glycaemic control and the diabetes care. The target of HbA1c for children and adolescents with type 1 diabetes recommended by ISPAD Clinical Practice Consensus Guidelines 2014 Compendium is below 7.5% (58 mmol/mol) [Citation6].
The data from the Diabetes Control and Complications Trial (DCCT) and Epidemiology of Diabetes Interventions and Complications (EDIC) showed that constantly elevated HbA1c (>8.9%) for 5–7 years during adolescence and young adulthood, results in an increased risk for microvascular and macrovascular complications in the subsequent 6–10 years [Citation7–11]. These data support the necessity to achieve HbA1c levels close to the normal range without severe or frequent hypoglycemia for every individual with diabetes.
The DCCT and the National Glycohemoglobin Standardization Program (NGSP) have recommended High performance liquid chromatography (HPLC) as a standard method for examination of HbA1c. The International Federation of Clinical Chemistry (IFCC) developed a new reference method for precise measurement of the concentration of glycated HbA1c only [Citation12,Citation13]. The reference procedure measures the fraction of βN1-deoxyfructosylhemoglobin, and the recommended SI measurement units are mmol/mol [Citation14,Citation15].
In Bulgaria as well as in other countries, there are significant differences in the level of glycated hemoglobin measured by various methods. This makes it difficult to evaluate the actual glycemic control in the diabetic patients both individually and for a cohort of patients.
With the development of new technologies, the attempts to equalize the opportunities for glycemic control are worthwhile. Our goal was to investigate the glycemic control of Bulgarian children and adolescents (aged 0–19 years) with type 1 diabetes mellitus by examining HbA1c with the same standardized HPLC method and the same device in a Central laboratory. Using the standardized method, we organized two national surveys of glycated hemoglobin in Bulgarian children and adolescents with type 1 diabetes mellitus: in 2012 and 2014. The results were given in the two units of measurement: percent (%) and mmol/mol. Additional continuous training for the patients and their parents was conducted between the two studies. Further, the mean levels of HbA1c in the cohort of patients studied in 2012 and 2014 were compared and the impact of age and gender on the glycaemic control was analysed.
Subjects and methods
Cohort and study design
Two national multicentre cross-sectional studies of the HbA1c levels of patients with diabetes mellitus aged 0–19 years were conducted in 11 pediatric endocrine practices in Bulgaria in 2012 (from 1 February 2012 to 30 August 2012) and in 2014 (from 15 January 2014 to 15 September 2014). The studies included all patients who visited the offices of their paediatric endocrinologist during the above-mentioned defined periods. The exclusion criterion for both studies was duration of the disease of less than three months.
In the first study (2012), 829 patients with type 1 diabetes participated, 422 boys and 407 girls, aged 11.9 ± 4.2 years (). In the second study (2014), 498 patients with type 1 diabetes were examined, 261 boys and 237 girls, aged 11.6 ± 4.1 years. The number of patients who participated in both studies was 281. Some of the outpatient offices in the rural areas included a smaller number of patients in the second survey due to organizational issues (difficulties in the distribution of the kits and timely delivery of samples).
Table 1. Age and sex distribution of the cohort.
We divided the patients in different age groups in order to determine if the age influences the level of glycated hemoglobin.
HbA1c determination
A standardized HPLC (Bio-Rad) method for measurement of HbA1c in a Central lab (Sofia, Bulgaria) was used in both studies. New HPLC systems utilizing more modern chromatographic materials in order to reduce the effects of abnormal and minor fractions of hemoglobin were used. The Bio-Rad D-10™ HbA1c Program has been certified by the NGSP as being traceable to the DCCT reference method using the precision criteria of 4% coefficient of variation (CV). The D-10™ Hemoglobin A1c Program, based on the chromatographic separation of HbA1c in a cation exchange cassette, was used. Separation was optimized to eliminate interference from hemoglobin, labile A1c and carbamylated hemoglobin. A single capillary blood sample was taken in the offices of endocrinologists, coded and stored according to the requirements and shipped weekly to the Central lab.
Data collection
A special web page was developed for the project. The data for the patients (age, sex, date of the onset of diabetes etc.) were coded and entered by the physicians. The results for HbA1c were entered by the lab technician. Every participating physician had access to the results of his/her patients only.
The study was approved by the Ethics Committee at the Medical University of Sofia, Bulgaria, in 2011. Informed consent was obtained from the children's parents or guardians, according to the local regulations.
Statistical analysis
The results were entered and processed with statistical package SPSS for Windows, Version 16.0. Differences were considered to be statistically significant at p < 0.05. Descriptive statistics was used for presentation of data by summarizing statistical characteristics (average values, standard deviations (±SD), minimum and maximum values etc.). Chi-squared test or Fisher's exact test were applied for verification of the hypothesis of a link between two categorical variables. The non-parametric test of Kolmogorov–Smirnov was applied for checking the distribution of the statistical sample for normality. Differences in the mean values between groups were analysed with Student's t-test and Mann–Whitney U-test.
Results and discussion
Descriptive statistics
The total number of patients included in the two studies was 1327 and represents about 60% of the children and adolescents with type 1 diabetes mellitus in Bulgaria. The ratio between girls and boys in both studies was similar: 49.1% girls and 50.9% boys in the first study, and 47.6% girls and 52.4% boys in the second one. The distribution of the participants in both studies () did not differ by gender (p = 0.595) and age (p = 0.258). No significant differences in the duration of diabetes were found either: 4.32 ± 3.54 years, and 4.52 ± 3.38 years, for the first and the second study, respectfully (p = 0.089). There was no significant difference in the duration of diabetes, according to the gender of the participants in the two studies (p = 0.505).
HbA1c levels
The mean level of HbA1c for diabetic patients studied in 2014 was 8.42 ± 1.69% (68.57 ± 18.50 mmol/mol). It was significantly lower compared with the HbA1c level of 8.93 ± 1.98% (74.35 ± 21.47 mmol/mol) for the patients studied in 2012 (p < 0.001).
This level of glycated hemoglobin does not meet the targets for good glycemic control with HbA1c < 7.5%. Nevertheless, we find it important that over the two years following the first study, there was significant improvement. Continuous well-structured education of patients, their families and medical staff in different areas of the country may have led to improvements in the diabetes care for patients, and respectively, to improvement of the glycemic control as shown in the second study.
Latest data on the level of glycemic control are represented by the international project SWEET, collecting data for children with diabetes from 48 centres around the world. The mean glycated hemoglobin in 2015 for all participants in this consortium is 7.8% (61.7 mmol/mol) [Citation16]. This is a good result; however, it must be taken into consideration that this project involved large diabetic centres (>150 patients) where the monitoring of patients is well organized at a highly professional level. The data from this project show that 39.1% of patients have a median HbA1c level under the ISPAD target of 7.5% (58 mmol/mol), 41.4% are between 7.5%–9% (58–75 mmol/mol) and 19.5% show HbA1c above 9% (75 mmol/mol). Wide variation between different centres still remains. Fourteen centres achieved a median HbA1c < 7.5% (58 mmol/mol) [Citation16].
We did not find gender differences in the level of glycated hemoglobin () in both studies (p = 0.854), which is in agreement with the results reported by other authors [Citation17–19]. Another study, however, demonstrates higher levels of glycated hemoglobin in girls as opposed to boys at diagnosis of diabetes and during follow-up in children above 10 years of age [Citation20].
Table 2. Average levels of glycated hemoglobin in girls and boys from both studies.
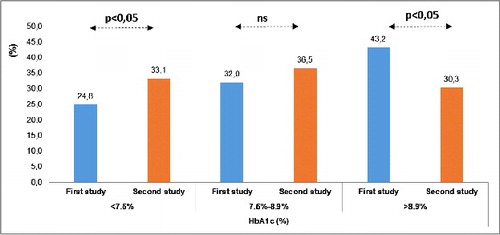
Significantly more patients in the second study (33.1%) showed optimal control with HbA1c < 7.5% (p < 0.05) as compared to the first one (24.8%). A significantly lower proportion of patients () with poor glycemic control (HbA1c > 9%) was found in the second study (30.3%) compared to the first one (43.2%), (p < 0.05).
The data obtained in our studies is similar to data reported for many countries in Europe, Asia and North America based on population or clinical data [Citation19,Citation21]. For example, in Denmark and the Netherlands, about 30% of children <15 years have optimal glycemic control [Citation19]. The situation in other countries such as England, Wales and France is slightly worse than that in Bulgaria: about 20% of children and adolescents reach a level of HbA1c < 7.5% [Citation19]. In the United States, 27% of the children below the age of 13 years and 23% of those between 13 and 19 age achieve this goal [Citation22]. Good results are achieved by the children with diabetes in Germany, Austria and Italy, where more than 40% of diabetic patients < 15 years reach the desired goal [Citation19]. In Sweden, 60% of children with diabetes under 13 years of age and 36% of those between 13 and 18 years had an average HbA1c < 7.5%, in 2013 [Citation23].
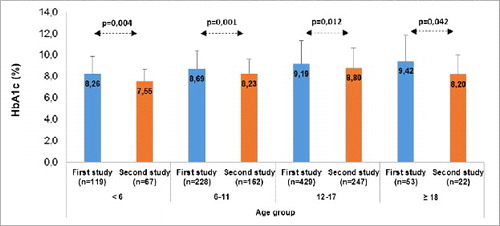
We found some improvement in the glycaemic control in the second study in all age groups (). The teenagers in both studies had higher HbA1c compared to the subjects in the other age groups: the mean HbA1c was 9.19% ± 2.11% (77.32 ± 22.69 mmol/mol) for the first study in 2012 and 8.8% ± 1.87% (72.82 ± 20.43 mmol/mol) for the second study in 2014.
Many adolescents experience deterioration in metabolic control due to erratic meal and exercise patterns, poor adherence to treatment regimens, psychological problems and insufficient motivation to maintain optimal control of diabetes [Citation24]. In the second study, children with type 1 diabetes up to the age of 6 years achieved the target goal of a good glycemic control with a mean level of glycated hemoglobin of 7.55% ± 1.12% (58.9 ± 12.25 mmol/mol). This improvement in the glycemic control, in our opinion, could be associated with the additional training of the patient, the families and the medical staff that was organized in different regions of the country.
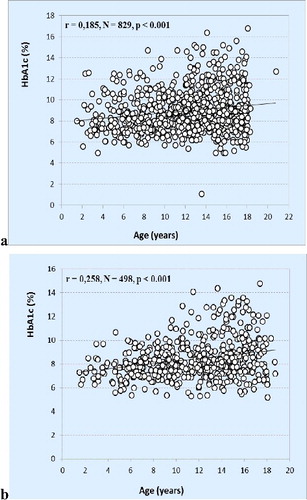
There was a positive correlation (p < 0.001) between the age of patients and glycated hemoglobin (HbA1c) in both studies (). Our results are similar to data from a Scottish study group that found an increase in glycated hemoglobin with the age of the patients [Citation17].
Figure 3. Relationship between the level of glycated hemoglobin and the age of patients with diabetes in the first study in 2012 (a) and in the second study in 2014 (b).
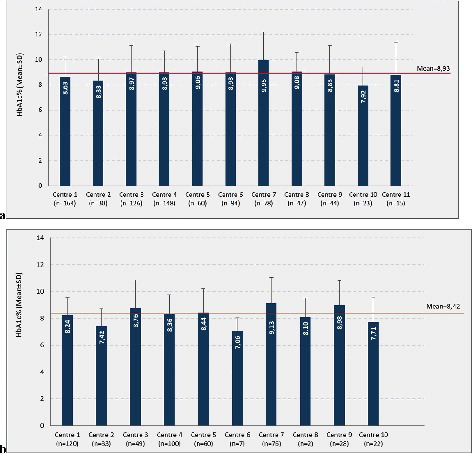
Our results revealed significant differences in the average level of glycated hemoglobin () between different centres in Bulgaria with variations from 7.92% (63.0 mmol/mol) to 9.95% (85.32 mmol/mol) in the first study and from 7.42% (57.43 mmol/mol) to 9.13% (76.17 mmol/mol) in the second study (2014). These results are in accordance with previous reports [Citation16,Citation17,Citation21]. We hypothesize that the factors responsible for this variation could be the social status of families and difficulties in their training and/or more limited access to specialists in some areas of the country. Last but not least, some centres included much less patients in the second survey. These centres are based in rural areas and observed a smaller number of patients in the second survey due to difficult distribution of kits and timely delivery of samples. Notwithstanding this limitation, we monitored the actual glycemic control in the majority of children and adolescents with type 1 diabetes from 11 different regions and paediatric practices in Bulgaria. Further research is needed with a larger number of patients and better organization in more distant centres.
Figure 4. Distribution of median HbA1c in paediatric centers in Bulgaria in the first study in 2012 (a) and in the second study in 2014 (b).
Our research of glycemic control indicated that most patients do not reach the desired target for HbA1c < 7.5%, which is recommended by the ISPAD guidelines. However, in the second study, there was some improvement in the glycemic control. Another reason for the unfavorable results may be the limited number of patients treated with the new technologies, such as insulin pumps and glucose sensors in Bulgaria, compared to other European countries and the United States. Recent data mostly suggest that treatment with insulin pumps, especially sensor-augmented pumps, significantly improves glycemic control [Citation25–31]. Most patients treated with insulin pumps, particularly in early childhood and preschool age, reach desired levels of glycated hemoglobin below 7.5% [Citation27,Citation30]. It is good that after the start of reimbursement of insulin pumps in June 2016 in Bulgaria, the number of children treated with insulin pumps is rapidly increasing. In the coming years, this is a good chance for further improvement of the glycemic control of children with diabetes in our country.
Conclusions
This is the first study to report national data on glycemic control in Bulgarian children and adolescents with type 1 diabetes. It demonstrated that there is substantial variation of the achieved HbA1c levels between diabetes centres within our country. Maintaining optimal glycaemic control was shown to be most difficult in teenagers, which is most likely connected with the specifics of this age, low motivation, psychological lability and issues with parents and school. Small children under 6 years achieved good glycemic control easier due to families’ devotion to diabetes control, which gives hopes for maintaining this good glycemic control in the following years. Continuous education and tracking of its effectiveness will increase the motivation of patients and their families to achieve better glycaemic control in all age groups.
Acknowledgements
We thank the families for their participation.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Soltesz G, Patterson CC, Dahlquist G, et al. Worldwide childhood type 1 diabetes incidence – what can we learn from epidemiology ? Pediatr Diabetes. 2007;8(Suppl. 6):6–14.
- Maahs DM, West NA, Lawrence JM, et al. Chapter 1: epidemiology of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39(3):481–497.
- Patterson CC, Dahlquist GG, Gyürüs E, et al. Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: A multicenter prospective registration study. Lancet. 2009;373:2027–2033.
- Tuomilehto J, Karvonen M, Pitkäniemi E, et al. Record-high incidence of type 1 (insulin-dependent) diabetes mellitus in Finnish children. Diabetologia. 1999;42:655–660.
- Enander R, Gundevall C, Stromgren A, et al. Carbohydrate counting with a bolus calculator improves post-prandial blood glucose levels in children and adolescents with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2012;13:545–551.
- Rewers MJ, Pillay K, de Beaufort C, et al. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes. 2014;15(Suppl. 20):102–114.
- Cameron FJ, de Beaufort C, Anstoot H-J, et al. Lessons from the Hvidoere International study group on childhood diabetes: be dogmatic about outcome and flexible in approach. Pediatr Diabetes. 2013;14:473–480.
- Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA. 2003;290:2159–2167.
- Donaghue K, Fung A, Hing S, et al. The effect of prepubertal diabetes duration on diabetes. Microvascular complications in early and late adolescence. Diabetes Care. 1997;20:77–80.
- Dovc K, Telic S, Lusa L, et al. Improved metabolic control in pediatric patients with type 1 diabetes: a nationwide prospective 12-year time trends analysis. Diabetes Technol Ther. 2014;16(1):33–40.
- Fullerton B, Jeitler K, Seitz M, et al. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2014 [cited 2017 Mar 12];2:CD009122. DOI:10.1002/14651858.CD009122.pub2
- Report of the ADA/EAS/IDF working group of the HbA1c assay, London, UK. Diabetologia. 2014;47:R53–R54.
- Rhea JM, Molinaro R. Pathology consultation on hba1c methods and interferences. Am J Clin Pathol. 2014;141:5–16.
- Rhea JM, Koch D, Ritchie J, et al. Unintended reporting of misleading HbA1c values when using assays incapable of detecting hemoglobin variants. Arch Pathol Lab Med. 2013;137:1788–1791.
- Weykamp C. HbA1c: a review of analytical and clinical aspects. Ann Lab Med. 2013;33:393–400.
- Witsch M, Kosteria I, Kordonouri O, et al. Possibilities and challenges of a large international benchmarking in pediatric diabetology. The SWEET experience. J Pediatr Diabetes. 2016;17(Suppl. 23):7–15.
- Alexander V, Blair A, Blair M, et al. Factors influencing glycemic control in young people with type 1 diabetes in Scotland. A population-based study (DIABAUD2). Diabetes Care. 2001;24:239–244.
- Ngwiri T, Fred Were F, Predieri B, et al. Glycemic control in Kenyan children and adolescents with type 1 diabetes mellitus. Int J Endocrinol. 2015 [cited 2017 Mar 12];2015:761759. DOI:10.1155/2015/761759
- McKnight JA, Wild SH, Lamb MJE, et al. Glycaemic control of type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabetic Med. 2015;32:1036–1050.
- Hanberger L, Akesson K, Samuelsson U. Glycated haemoglobin variations in paediatric type 1 diabetes: the impact of season, gender and age. Acta Paediatrica. 2014;103(4):398–403.
- O'hagan M, Harvey JN, Brecon Group. Glycemic control in children with type 1 diabetes in Wales. Influence of the pediatric diabetes specialist nurse. Diabetes Care. 2010;33:1724–1726.
- Wood JR, Miller KM, Maahs DM, et al. Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013;36:2035–2037.
- Samualsson U, Hanberger L, Pundzuite-Lycka A, et al. Yearly report. SWEDAIDKIDS. National quality register for children and adolescents with diabetes. Register Center Vastra Gotaland; 2013. Available from:https://swediabkids.ndr.nu/
- Cameron FJ, Amin R, de Beaufort C, et al. ISPAD clinical practice consensus guidelines – 2014: diabetes in adolescence. Pediatr Diabetes. 2014;15(Suppl. 20):245–256.
- Battelino T, Longet I, Olsen B, et al. The use and efficacy of continuous glucose monitoring in type 1 diabetes treated with insulin pump therapy: a randomized controlled trial. Diabetologia. 2012;55(12):3155–3162.
- Berghaeuser MA, Kapellen T, Heidtmann B, et al. Continuous subcutaneous insulin infusion in toddlers starting at diagnosis of type 1 diabetes mellitus. A multicenter analysis of 104 patients from 63 centres in Germany and Austria. Pediatr Diabetes. 2008;9:590–595.
- Szypowska A, Schwandt A, Svensson J, et al. Insulin pump therapy in children with type 1 diabetes: analysis of data from the SWEET registry. J Pediatr Diabetes. 2016;17(Suppl. 23):38–45.
- Sherr JL, Herrmann JM, Campbell F, et al. Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: comparison of results from three large, transatlantic paediatric registries. Diabetologia. 2016;59(1):87–91.
- Phillip M, Danne T, Battelino T, et al. Use of insulin pump therapy in the pediatric age-group. Consensus statement from the ESPE, the LWPES and ISPAD, endorsed by ADA and EASD. Diabetes Care. 2007;30:1653–1662.
- Litton J, Rice A, Friedman N, et al. Insulin pump therapy in toddlers and preschool children with type 1 diabetes mellitus. J Pediatrics. 2002;141:490–495.
- Thabit H, Tauschmann M, Allen JM. Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015;373:2129–2140.