ABSTRACT
Introduction: A strong link between voice-hearing experience and childhood trauma has been established. The aim of this study was to identify whether there were unique clusters of childhood trauma subtypes in a sample across the clinical spectrum of auditory verbal hallucinations (AVH) and to examine clinical and phenomenological features across these clusters.
Methods: Combining two independent international datasets (the Netherlands and Australia), childhood trauma subtypes were examined using hierarchical cluster analysis. Clinical and phenomenological characteristics were compared across emerging clusters using MANOVA and chi-squared analyses.
Results: The total sample (n = 413) included 166 clinical individuals with a psychotic disorder and AVH, 122 non-clinical individuals with AVH and 125 non-clinical individuals without AVH. Three clusters emerged: (1) low trauma (n = 299); (2) emotion-focused trauma (n = 71); (3) multi-trauma (n = 43). The three clusters differed significantly on their AVH ratings of amount of negative content, with trend-level effects for loudness, degree of negative content and degree of experienced distress. Furthermore, perceptions of voices being malevolent, benevolent and resistance towards voices differed significantly.
Conclusion: The data revealed different types of childhood trauma had different relationships between clinical and phenomenological features of voice-hearing experiences. Thus, implicating different mechanistic pathways and a need for tailored treatment approaches.
Introduction
The experience of hearing a voice in the absence of corresponding external stimuli (typically referred to as “voice-hearing”, “hearing voices”, or “auditory-verbal hallucinations”) is common across a number of psychiatric diagnoses (Larøi et al., Citation2012), and occurs in around 10–15% of the general population (Beavan et al., Citation2011). Traumatic or adverse childhood experiences are prevalent in populations of people who hear voices, with evidence implicating a causal relationship (Varese et al., Citation2012) involving a number of potential mechanisms.
Traumatic experiences in childhood can take different “subtypes”, ranging from emotional or physical neglect, to acts of physical, sexual or emotional maltreatment or violence (Bernstein et al., Citation1994). Sexual abuse, physical abuse, emotional trauma, and neglect have all been linked to hearing voices in both general (van Nierop et al., Citation2014) and psychiatric populations (Berg et al., Citation2015). Findings from some studies suggest that the relationship may differ depending on the type of trauma experiences, with childhood sexual abuse showing the strongest link with voices (Bentall et al., Citation2012; Daalman et al., Citation2012; Shevlin et al., Citation2007). These findings demonstrate the significance of trauma in voice hearing, and suggest that specific subtypes of trauma may have differential effects. Further studies are needed to unpack this complex relationship across the continuum of psychosis from clinical to non-clinical populations. Understanding the links between different types of traumatic events, characteristics of voices and need for care, may help to refine theoretical models and tailor therapeutic approaches.
Research has also found a specific link between some phenomenological features of voices and childhood abuse, particularly concerning the degree of negative content of voices (Rosen et al., Citation2018; Scott et al., Citation2020). This is significant because these features have also been found to separate people who do and do not find voices distressing and problematic, thereby somewhat differentiating “clinical” and “non-clinical” groups (Johns et al., Citation2014). Considerable efforts have been undertaken to dismantle the specific differences between these groups in order to inform clinical interventions, which may target mechanisms that drive voice-related distress (Brand et al., Citation2017). People who find voices distressing typically experience more frequent voices, a high degree of negative voice content (Daalman et al., Citation2011; Johns et al., Citation2014; Larøi et al., Citation2019), perceive their voices to be more powerful and malevolent (Andrew et al., Citation2008; Johns et al., Citation2014), and experience little control over their voices (Daalman et al., Citation2011; Johns et al., Citation2014).
Whereas there is a growing body of evidence supporting a link between childhood trauma and voice phenomenology, these studies have mostly focused on overall trauma severity. Of those studies that have examined subtypes of trauma, almost all have used a “top down” approach to defining trauma subtypes, thus ignoring the reality that different childhood traumatic experiences rarely occur in isolation (Jacobs et al., Citation2012). Cluster analysis is an analytical approach that is used to classify participants based on a chosen variable into groups on the basis of patterns in observations across different profiles or traits. This enables a more “bottom up”, data-driven approach to studying naturally co-occurring groups, rather than pre-defining them on the basis of existing categories. Cluster analysis has successfully been used to cluster participants according to trauma subtypes in populations with psychosis (Stevens et al., Citation2019). Stevens et al. (Citation2019) found that a cluster with moderate scores across all trauma subtypes with high scores on physical and emotional neglect, and another cluster with higher overall scores with very high emotional abuse. Those in the high abuse cluster had more severe hallucinations and delusions, implicating that emotional abuse may be particularly important in the development of these symptoms. Carbone et al. (Citation2019) also conducted a similar analysis, finding three clusters of childhood adverse events: a low overall adverse event cluster, a cluster consisting of lack of support and isolation, and a cluster consisting of abuse and neglect.
Whilst cluster analysis has been used within psychosis samples, very few studies have utilised the method for voice hearing specifically, and none yet in relation to trauma subtypes and voice phenomenology nor across the full psychosis spectrum from those without voices (no AVH), those with voices but no clinical diagnosis (non-clinical AVH), and people with voices and a clinical diagnosis (clinical AVH). Examining patterns of voice characteristics (negative content, controllability, and beliefs about voices) across trauma subtypes provides an opportunity to advance our understanding of the relationship between types of traumatic experiences and clinically important characteristics of voices. As such, the current study aimed to derive clusters of trauma subtypes within a sample of people with clinical or non-clinical voices and those without voices, and examine differences in voice phenomenology (degree of negative voice content, degree of controllability, voice-related distress, and beliefs about voices) between clusters. Further, this study aimed to evaluate the distribution of clinical and non-clinical voices across the clusters to improve understanding of how the interplay of traumatic experiences and voice characteristics may differ across these groups.
Materials and methods
Participants
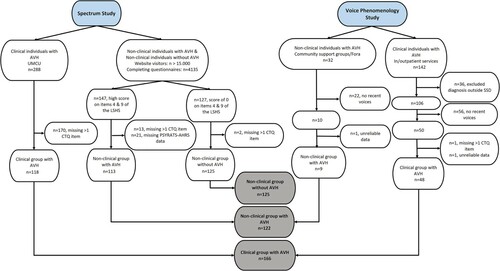
Data were obtained from two independent studies: the Spectrum study conducted at the University Medical Centre (UMC) Utrecht [the Netherlands; details described by Sommer et al. (Citation2010) and Daalman et al. (Citation2011, Citation2012)] and the Voice Phenomenology Study at Swinburne University of Technology (Melbourne, Australia; reported by Rossell et al., Citation2019). All participants were between 18 and 65 years of age and provided written informed consent for study participation.
Spectrum study
Data were collected between 2005 and 2011. In total, 118 clinical individuals with AVH, 113 non-clinical individuals with AVH and 125 non-clinical individuals without AVH were included in the current study (). Clinical individuals with AVH were recruited from the UMC Utrecht, the Netherlands. They were diagnosed with a psychotic disorder [schizophrenia, schizoaffective disorder or psychosis not otherwise specified; Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)], without current alcohol or drug abuse, confirmed by an independent psychiatrist using the Comprehensive Assessment of Symptoms and History (CASH) interview (Andreasen et al., Citation1992), in addition to the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II; First et al., Citation1997) to assess Axis II pathology. Individuals experienced AVH at least once a month for over a year.
Non-clinical individuals with and without AVH were recruited by means of a Dutch website “Explore your mind” (www.verkenuwgeest.nl). They completed an adapted version of the Launay and Slade Hallucinations Scale (LSHS; Larøi et al., Citation2004). Individuals scoring 0 (absent) for “In the past, I have had the experience of hearing a person’s voice and then found that no one was there” and “I have been troubled by voices in my head” were included as non-clinical individuals without AVH. Individuals with higher scores on these questions were contacted for a telephone screening by a trained psychologist to evaluate whether their voices were distinct from thoughts and had a perceptual quality [in line with definitions of AVH from Moritz and Larøi (Citation2008) and Slade and Bentall (Citation1988)], with a frequency of at least once per three months. Both non-clinical groups were further screened in the UMC Utrecht by trained psychologists, for absence of a psychiatric disorder (other than a depressive/anxiety disorder in remission), no alcohol or drug abuse for at least three months, no chronic somatic disorder, and Dutch-born grandparents (to restrict heterogeneity for later genetic studies) using the CASH (Andreasen et al., Citation1992) and SCID-II (First et al., Citation1997). The Spectrum study was performed in accordance with the Declaration of Helsinki of 1975 (revised in 2008) and was approved by the Human Ethics Committee of the UMC Utrecht (project numbers 05/167 and 06/191).
Voice phenomenology study
Participants were recruited between 2014 and 2017 as part of a broader study on AVH phenomenology at the Swinburne University of Technology (Melbourne, Australia), from in- and outpatient services at the Alfred Hospital, St. Vincent’s Hospital, the Melbourne Clinic and community support groups and forums in Melbourne (). To match AVH frequency with the Spectrum study, the current study included only individuals reporting AVH in the past 7 days (48 clinical individuals and 9 non-clinical individuals with AVH).
Clinical individuals with AVH had a diagnosis of schizophrenia or schizoaffective disorder and had no current substance use disorder. Non-clinical individuals with AVH did not meet the criteria of a DSM-IV diagnosis nor a current substance use disorder. Diagnosis was confirmed by the Mini International Neuropsychiatric Interview (MINI; Sheehan et al., Citation1998) for all participants, conducted by trained researchers, psychologists or higher degree Psychology students. The Voice Phenomenology study was performed in accordance with the Declaration of Helsinki and was approved by the Alfred Hospital Human Research Ethics Committee (project number 20202954).
Assessments
Basic demographic information (including age, gender, years of education) was collected for all participants.
Childhood trauma
Childhood trauma was assessed using the Childhood Trauma Questionnaire – Short form (CTQ-SF; Bernstein et al., Citation2003; Dutch version described by Thombs et al. (Citation2009)). Using a 5-point Likert-scale from “never true” to “very often true”, childhood trauma is evaluated by using multiple trauma subtypes: physical neglect (PN) and emotional neglect (EN), as well as physical abuse (PA), sexual abuse (SA) and emotional abuse (EA). Participants missing more than one item on the CTQ were excluded from analysis (n = 4); each single missing item was replaced with the individual’s mean score of the remainder of questions for that specific trauma subtype (n = 6). Cut-off scores for “moderate to severe” exposure were used to classify the presence of a specific trauma subtype (emotional abuse ≥13; physical abuse ≥10; sexual abuse ≥8; emotional neglect ≥15; physical neglect ≥10). These were used to characterise the emerging clusters: the trauma subtype was determined as relevant when over two-third of participants in a particular cluster scored above the cut-off score. The CTQ-SF shows good validity for both clinical and non-clinical populations (Bernstein et al., Citation2003; Thombs et al., Citation2009).
AVH phenomenology
Phenomenological characteristics of AVH were examined in detail using an adapted version of the Psychotic Symptoms Rating Scales (PSYRATS). This measure includes the following items: frequency, duration, perceived location (inside and/or outside the head), loudness, beliefs about the origin of the AVH, amount and degree of negative content, amount and degree of experienced distress, impact on functioning, controllability, age of onset and number of voices. Participants missing more than two items on the PSYRATS were excluded from analysis (n = 6). Missing items were replaced by the group mean score of the respective item (n = 12).
Beliefs about voices
The clinical and non-clinical participants experiencing AVH completed the revised Beliefs About Voices Questionnaire (BAVQ-R; Chadwick et al., Citation2000). This questionnaire consists of 35 questions to assess five types of beliefs about voices; omnipotence, malevolence, benevolence, resistance and engagement. Due to a difference of meaning following translation, question 8 (“My voice is helping to keep me sane”) was not assessed in the Dutch Spectrum study and was therefore left out of current study. Participants missing more than two items on the BAVQ-R were excluded from analysis (n = 8). Missing items were replaced by the individual’s mean score from the respective BAVQ-R subscale (n = 17).
Statistical analysis
Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) version 25 (IBM Corp, Citation2017).
Subgroups (clinical AVH, non-clinical AVH and no AVH) were compared for demographic variables including age, gender, years of education, age of onset and childhood trauma subtypes, using Pearson’s Chi-Square (categorical variables) and One-way Analysis of Variance (ANOVA, continuous variables). Post-hoc tests were used to evaluate significant group differences.
Agglomerative hierarchical clustering analysis (Everitt, Citation1980) was performed to define childhood trauma subgroups and increase within-group homogeneity and between-groups heterogeneity. Case similarity was computed with squared Euclidean Distance and Wards linkage (Ward, Citation1963) as agglomeration procedure specification. Collaborative examination of the dendrogram and the agglomeration schedule coefficients was used to establish the optimal number of clusters.
First, emergent trauma clusters were compared on demographic variables and CTQ subscores using Pearson’s Chi-Square (categorical variables) and One-way Analysis of Variance (ANOVA, continuous variables). Second, childhood trauma clusters were compared in AVH phenomenology (PSYRATS) and beliefs about voices (BAVQ-R) using a Multivariate analysis of variance (MANOVA) with Games Howell tests for post hoc comparison. To address demographic differences between emergent clusters, exploratory analyses were conducted for demographic variables and measures of voice phenomenology and beliefs about voices using Pearson correlation analyses and Pearson’s Chi-square tests.
Results
The total sample consisted of 413 individuals, which included a clinical group with AVH (n = 166), non-clinical individuals with AVH (n = 122), and non-clinical participants without AVH (n = 125), see . The clinical group with AVH included significantly more males than the non-clinical groups with AVH (χ2(1) = 8.71, p = 0.003) and without AVH (χ2(1) = 7.17, p = 0.007). Clinical individuals were also significantly younger (mean difference = −4.23; 95%CI = −7.98, −0.48; p = 0.022) and had attained significantly fewer years of education (mean difference = −1.07; 95%CI = −1.77, −0.36; p = 0.001) compared to the non-clinical group without AVH, but not when compared to the non-clinical group with AVH. Clinical and non-clinical individuals experiencing AVH scored significantly higher on childhood trauma overall compared to the non-clinical group without AVH (mean difference = 12.91; 95%CI = 8.49, 17.34, p<0.001; mean difference = 8.57, 95%CI = 3.82, 13.33, p<0.001, respectively). Sexual abuse scores in clinical and non-clinical individuals with AVH were also significantly higher compared to the non-clinical group without AVH (mean difference = 2.93; 95%CI = 7.77, 4.08, p<0.001; mean difference = 1.98; 95%CI = 0.73, 3.22; p = 0.001, respectively). This was also the case for emotional abuse rates (mean difference clinical AVH vs. no AVH = 3.65; 95%CI = 2.36, 4.94, p<0.001 and mean difference non-clinical AVH vs. No AVH = 3.18; 95%CI = 1.79, 4.57; p<0.001, respectively). Graded differences were found across groups for physical abuse and physical neglect, with non-clinical individuals reporting AVH as an intermediate group. Group differences for emotional neglect were not significant.
Table 1. Sample characteristics for clinical individuals with AVH, non-clinical individuals with AVH and non-clinical individuals without AVH.
Childhood trauma clusters
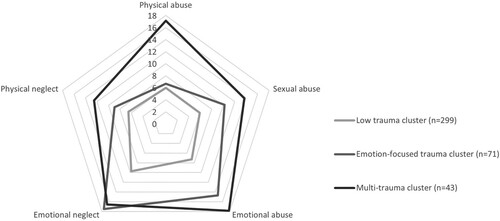
Hierarchical cluster analysis and inspection of the dendrogram (see supplementary Figure S1) resulted in a three-cluster solution. The emerging clusters were characterised as follows: a “low” trauma cluster, an “emotion-focused” trauma cluster and a “multi” trauma cluster, see and . The low trauma cluster consisted of 299 individuals and had significantly lower mean scores on all childhood trauma subtypes, as compared to the other two clusters. The emotion-focused trauma cluster consisted of 71 individuals and over two-thirds of this group met criteria for moderate to severe emotional abuse and emotional neglect (Table S1). However, this cluster also displayed relatively high scores of sexual abuse. The multitrauma cluster (n = 43) displayed significantly higher scores compared to the low trauma cluster (all trauma subtypes) and the emotion-focused trauma cluster (all subtypes apart from emotional neglect). For every trauma subtype, moderate to severe exposure was reported by over two-third of individuals in this cluster (Table S1).
Table 2. Sample characteristics for each childhood trauma cluster.
The three clusters did not differ significantly in terms of age and although years of education showed an overall significant effect (F(2) = 3.12, p = 0.045), post-hoc analyses were not significant. Compared to the emotion-focused trauma cluster, significantly more males were found in the low trauma cluster (χ2(1) = 7.12, p = 0.008) and multi-trauma cluster (χ2(1) = 9.88, p = 0.002).
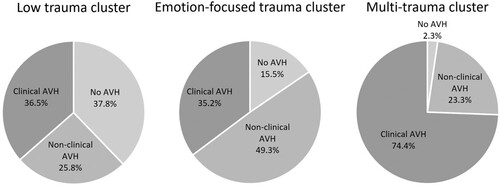
The distribution of the three subgroups across the trauma clusters is illustrated in . Within the low trauma cluster, they were quite evenly distributed: non-clinical individuals without AVH (37.79%), followed by 36.45% clinical individuals with AVH and 25.75% of non-clinical individuals with AVH. Almost half of the emotion-focused trauma cluster consisted of non-clinical individuals with AVH (49.30%), followed by 35.21% clinical individuals with AVH and 15.49% non-clinical individuals without AVH. The multi-trauma cluster mainly consisted of clinical individuals with AVH (74.42%), followed by 23.26% of non-clinical individuals with AVH and 2.33% non-clinical individuals without AVH.
AVH phenomenology (PSYRATS)
The three clusters differed significantly on their PSYRATS ratings of amount of negative content (F(2) = 4.50, p = 0.012), controllability (F(2) = 3.07, p = 0.048) and age of onset (F(2) = 6.63, p = 0.0020), see . Trend-level effects were present for loudness (F(2) = 2.79, p = 0.063), degree of negative content (F(2) = 2.50, p = 0.084) and degree of experienced distress (F(2) = 2.92, p = 0.056). Post hoc analyses showed that individuals in the multi-trauma cluster experienced their AVHs as having a greater amount of negative content compared to the low trauma cluster (mean difference = 0.72; 95%CI = 0.08, 1.36; p = 0.025) and emotion-focused trauma cluster (mean difference = 0.92; 95%CI = 0.15, 1.70; p = 0.015). The multi-trauma cluster also experienced less control over their AVHs compared to the emotion-focused trauma cluster (mean difference = 0.71; 95%CI = 0.07, 1.35; p = 0.026). Finally, individuals in the emotional-focused trauma cluster started experiencing AVHs at a younger age compared to the low trauma cluster (mean difference = −6.93; 95%CI = −11.85, −2.02; p = 0.003).
Table 3. Voice phenomenology (PSYRATS) per childhood trauma cluster.
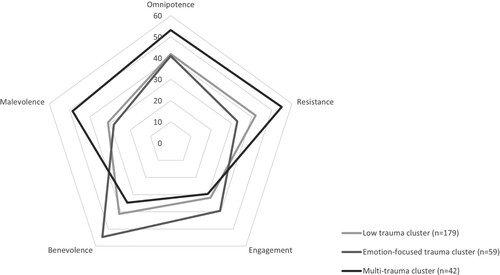
Beliefs about voices (BAVQ)
The three clusters differed significantly on the subscales malevolence (F(2) = 5.63, p = 0.004), omnipotence (F(2) = 3.48, p = 0.032), resistance (F(2) = 5.63, p = 0.004) and benevolence (F(2) = 4.58, p = 0.011), see and supplementary Table S2. Post hoc analyses revealed that the multi-trauma cluster rated their voices as more malevolent and felt more resistance against them, compared to the low trauma cluster and the emotion-focused trauma cluster. Furthermore, AVH were rated as significantly more omnipotent by the multi-trauma compared to the low trauma cluster (mean difference = 2.03; 95%CI = 0.26, 3.79; p = 0.021). Finally, the emotion-focused trauma cluster experienced their AVH as significantly more benevolent, relative to the low trauma cluster (mean difference = 2.02; 95%CI = 0.02, 4.01; p = 0.047) and the multi-trauma cluster (mean difference = 2.99; 95%CI = 0.38, 5.61; p = 0.021).
Discussion
The aim of this study was to utilise cluster analysis to derive clusters of childhood trauma subtypes within a sample of individuals experiencing auditory verbal hallucinations (AVH) with (clinical AVH) and without a diagnosed psychotic disorder (non-clinical AVH), and a non-clinical group without AVH (no AVH), and examine differences in phenomenological features and beliefs about voices across the clusters. Three clusters were produced: (1) a “low trauma cluster” (n = 299) with low scores across all trauma subtypes, consisting of a relatively even distribution of clinical AVH, non-clinical AVH and no AVH; (2) an “emotion-focused cluster” (n = 71) with moderate to severe emotional abuse and emotional neglect, consisting of predominantly non-clinical AVH with greater control over voices (compared to the multi-trauma cluster), voice onset at an earlier age (compared to the low trauma cluster), and greater perception of voices being benevolent (compared to both other clusters); and (3) a “multi-trauma cluster” (n = 43) with high scores across all trauma subtypes, consisting of predominantly clinical voice hearers with higher amount of negative voice content (compared to both other clusters), greater perceptions of voices being malevolent (compared to both other clusters) and omnipotent (compared to low trauma cluster), and more resistance towards voices (compared to both other clusters). This is the first study to use a bottom-up, data driven approach to examine how subtypes of childhood trauma relate to voice-hearing phenomenology across the psychosis spectrum.
The relatively even proportion of clinical and non-clinical voices and those without voices within the low trauma cluster suggests that low levels of childhood trauma is not likely sufficient to distinguish clinical status for people who hear voices. However, the multi-trauma cluster consisted of a high proportion of clinical voices (74.42%) and over two thirds of those in this group met CTQ cutoff, suggesting that a relationship between trauma severity and clinical status may emerge when levels of trauma are high. This emphasises the significance of severe trauma history in those with severe AVH and psychotic illness, which is in keeping with research that has indicated a general relationship between high levels of trauma and clinical voices (Berg et al., Citation2015; van Nierop et al., Citation2014). The emotion-focused cluster, despite having high scores on emotional abuse, neglect and sexual abuse trauma subtypes, with overall two-thirds scoring over CTQ severity cutoff, consisted of a relatively even distribution of clinical and non-clinical voice hearers and few without any voices. Together these findings indicate that there are likely multiple mechanistic pathways to voice hearing and trauma exposure may not always be involved (Luhrman et al., Citation2019).
The current findings somewhat contrast with two previous studies involving cluster analysis of trauma subtypes in psychosis populations. Stevens et al. (Citation2019) found two clusters distinguished predominantly by childhood emotional abuse and physical or emotional neglect, whereas the current study found that emotional abuse and emotional neglect clustered together. Similar to the current study, Carbone et al. (Citation2019) found a low trauma cluster, however differed in their second and third cluster which consisted of predominantly abuse/neglect and isolation/lack of support, respectively. These differences in the clusters may be explained by variations in samples, with Stevens et al. (Citation2019) and Carbone et al. (Citation2019) both being restricted to small, clinical samples of people with a psychotic disorder diagnosis. The current study was the first to examine clusters across a spectrum of clinical and non-clinical voices specifically, and controls without voices. Whilst the current findings require replication in other samples, this does suggest that the trauma subtypes identified in the current study may be specific to voice hearing and not psychosis in general. Further, whilst Stevens et al. (Citation2019) used the same measure of trauma subtypes as the current study (i.e., CTQ), Carbone et al. (Citation2019) utilised the Childhood Experience of Care and Abuse scale (CECA; Bifulco et al., Citation1994), which covers a broader range of adverse childhood experiences that differ to the constructs measured by the CTQ.
The current findings suggest that emotion-focused trauma may present as a distinct subtype of traumatic experience in voice-hearing populations. The composition of this cluster, with a relatively even number of clinical and non-clinical voices, suggests that this trauma profile may involve a general vulnerability to voice hearing irrespective of clinical status. Of note, there was also a moderate level of sexual abuse experienced by members of this cluster (47.89%), suggesting that sexual abuse may also play a role in this general liability. These findings challenge prior research emphasising sexual abuse as the primary trauma type related to voices (Daalman et al., Citation2012; Hardy et al., Citation2016; Sheffield et al., Citation2013), though the current analysis did not enable insights into the unique influence of specific trauma subtypes on voices. Given that sexual abuse is unlikely to occur in isolation (often co-occuring with physical and emotional abuse and neglect), it is possible, in line with past research, that the multi-trauma cluster represents the particular role of sexual abuse.
The low trauma and emotion-focused trauma clusters had significantly lower levels of negative voice content than the multi-trauma group, suggesting that high levels of childhood trauma across a range of subtypes may be particularly related to negative voice content. This is in keeping with prior research that has found links between childhood trauma and negative voice content (Rosen et al., Citation2018). In contrast to the current findings, Daalman et al. (Citation2012) found no relationship between trauma subtypes and negative voice content, however this may be explained by the conflation of voice content and voice-related distress in that study. The current findings also contrast with that of Scott et al. (Citation2020), which found an indirect relationship between negative voice content and emotional abuse and neglect, but not physical or sexual abuse or physical neglect. Scott et al. (Citation2020) interpreted their findings to reflect that interpersonal processes associated with the abuse could ultimately reflect greater negative voice content. The current study differed to Scott et al. in utilising a bottom-up approach, finding a unique emotion-focused trauma cluster with lower levels of negative voice content and a large proportion of non-clinical AVH. This group also had a strikingly younger age of voice onset around 13 years, potentially suggesting that these interpersonal processes leading to schema formation may differ for this group and that this may be related to less clinical presentations.
Those in the emotion-focused trauma cluster perceived more control over voices than the multi-trauma cluster. Very little research on the controllability of voices has been conducted, despite this being an important factor distinguishing clinical status (Johns et al., Citation2014). The greater control experienced by the emotion-focused cluster may be linked to the, perhaps more functional, relationship that people in this group have with their voices (perceiving them to be less negative, more benevolent, and resisting them less). In contrast, individuals in the multi-trauma cluster were characterised by more negative beliefs about their voices, perceiving them to be more malevolent and omnipotent and resisting them more. This corroborates previous research that has found childhood abuse to be related to increased malevolence beliefs (Offen et al., Citation2003). The multi-trauma and emotion-focused trauma subtypes are largely distinguished by the presence of physical and sexual abuse and neglect, which may reflect a particular relationship between these types of trauma and malevolence beliefs. Since physical and sexual abuse are more likely to lead to posttraumatic stress symptoms than emotional abuse or neglect, this finding might suggest that ongoing PTSD symptoms may be a predictor of negative beliefs about voices (Andrew et al., Citation2008).
Whilst the current study is unable to confirm specific mechanisms that explain these results, relevant theoretical explanations concerning mechanisms are relevant to mention as directions for future research. The patterns emerging from these data suggest three separate pathways to voice-hearing experiences. Those in the low trauma cluster are likely to be driven by different bio-psycho-social processes. The multi-trauma cluster consists of voices that are more negative in content, less controllable, more malevolent and omnipotent, and more likely to be resisted. This cluster may represent a group for whom common responses to childhood physical and sexual trauma, such as posttraumatic stress symptoms, emotional dysregulation, and dissociation, play an important role in shaping voice content, beliefs about voices, and coping styles (e.g., see Hardy, Citation2017). In contrast, the emotion-focused trauma cluster consists of voices that generally have less negative content, and are more controllable and benevolent. It could be hypothesised that this group have more general vulnerability to voices in the context of emotional maltreatment in childhood, possibly as a protective mechanism. This is consistent with the finding that onset of voices occurred at a younger age in this cluster, although it was not possible to determine the exact timing of the voice onset and trauma in this study. It is possible that, for many, cumulative exposure to multiple trauma subtypes (particularly including physical and sexual trauma) transforms these “protective” voices into more negative, malevolent voices over time. Whilst this is speculative, this hypothesis warrants further exploration, particularly in context of the significance of positive, supportive voice-hearing experiences that are commonly reported in the hearing voices community (Valavanis et al., Citation2019).
Clinical implications include the need for tailored treatment approaches based on the different trauma subtypes and the potential pathways and mechanisms these reflect. For example, if some voices arise through posttraumatic stress reactions (e.g., intrusions and dissociation) to multiple trauma exposures, then this particular group should respond to trauma-focused therapies (Brand et al., Citation2020). In comparison, those with low levels of trauma, but persisting voices may benefit more from traditional CBT for psychosis (Lincoln & Peters, Citation2019). Such a theory could be tested by observing relative responses to different treatments in these groups.
The findings of the current study should be considered in relation to several strengths and limitations. A large sample size across two countries enables confidence in the generalisability of these findings. The distribution of clinical and trauma characteristics across the trauma clusters suggests that their composition does not simply reflect clinical or trauma severity in general. The bottom-up approach to analysing the relation between trauma and voices across clinical and non-clinical groups and controls without voices, reveals insights across the continuum of psychosis, without being restricted to a specific diagnosis or trauma type. However, the data was collected from two different studies with varying procedures, and controls without voices came from only one sample, potentially limiting the comparability of the two populations. Further, the absence of a measure of other psychosis symptoms in the current sample precludes conclusions regarding the specificity of the findings to voices only. Group differences were observed, including younger age, lower level of education, and more males in the clinical group, which were not controlled for in the analysis because exploratory analyses did not indicate these factors were likely to confound the results.
This was the first study to conduct cluster analysis to provide data-driven insights into the relationship between trauma subtypes and hearing voices in a sample across the psychosis continuum. Findings revealed three distinct clusters, including a low trauma cluster, emotion-focused trauma cluster, and multi-trauma cluster. The phenomenological profile of these clusters indicated that the emotion-focused cluster may be a unique group representing general vulnerability to psychosis with less negative voices. Findings point towards the potential for three distinct pathways linking trauma to voice-hearing experiences, with clinical implications centring on a need for tailored treatment and further research required to replicate these findings and explore the underlying mechanisms.
Supplemental Material
Download MS Excel (10.7 KB)Supplemental Material
Download MS Excel (10.8 KB)Supplemental Material
Download JPEG Image (63.2 KB)Acknowledgements
The authors would like to thank the participants who shared their experiences of hearing voices for these studies, and the support of the Early Career Hallucinations Network (ECHR) through which this collaboration was formed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
Access and use of this data is protected by ethics requirements. Researchers requesting access to these data can contact the corresponding author to discuss.
Additional information
Funding
References
- Andreasen, N. C., Flaum, M., & Arndt, S. (1992). The Comprehensive Assessment of Symptoms and History (CASH): An instrument for assessing diagnosis and psychopathology. Archives of General Psychiatry, 49(8), 615–623. https://doi.org/https://doi.org/10.1001/archpsyc.1992.01820080023004
- Andrew, E. M., Gray, N. S., & Snowden, R. J. (2008). The relationship between trauma and beliefs about hearing voices: A study of psychiatric and non-psychiatric voice hearers. Psychological Medicine, 38(10), 1409–1417. https://doi.org/https://doi.org/10.1017/S003329170700253X
- Beavan, V., Read, J., & Cartwright, C. (2011). The prevalence of voice-hearers in the general population: A literature review. Journal of Mental Health, 20(3), 281–292. https://doi.org/https://doi.org/10.3109/09638237.2011.562262
- Bentall, R. P., Wickham, S., Shevlin, M., & Varese, F. (2012). Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 adult psychiatric morbidity survey. Schizophrenia Bulletin, 38(4), 734–740. https://doi.org/https://doi.org/10.1093/schbul/sbs049
- Berg, A. O., Aas, M., Larsson, S., Nerhus, M., Hauff, E., Andreassen, O. A., & Melle, I. (2015). Childhood trauma mediates the association between ethnic minority status and more severe hallucinations in psychotic disorder. Psychological Medicine, 45(1), 133–142. https://doi.org/https://doi.org/10.1017/S0033291714001135
- Bernstein, D. P., Fink, L., Handelsman, L., & Foote, J. (1994). Childhood trauma questionnaire (CTQ). The American Journal of Psychiatry, 151(8), 1132–1136. https://doi.org/https://doi.org/10.1037/t02080-000
- Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., Stokes, J., Handelsman, L., Medrano, M., Desmond, D., & Zule, W. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse and Neglect, 27(2), 169–190. https://doi.org/https://doi.org/10.1016/S0145-2134(02)00541-0
- Bifulco, A., Brown, G. W., & Harris, T. O. (1994). Childhood Experience of Care and Abuse (CECA): A retrospective interview measure. Journal of Child Psychology and Psychiatry, 35(8), 1419–1435. https://doi.org/https://doi.org/10.1111/j.1469-7610.1994.tb01284.x
- Brand, R. M., Bendall, S., Hardy, A., Rossell, S. L., & Thomas, N. (2020). Trauma-focused imaginal exposure for auditory hallucinations: A case series. Psychology and Psychotherapy: Theory, Research and Practice, 94(Suppl 2), 408–425. https://doi.org/https://doi.org/10.1111/papt.12284
- Brand, R. M., Rossell, S. L., Bendall, S., & Thomas, N. (2017). Can We Use an interventionist-causal paradigm to untangle the relationship between trauma, PTSD and psychosis? Frontiers in Psychology, 8, 306. https://doi.org/https://doi.org/10.3389/fpsyg.2017.00306
- Carbone, E. A., Pugliese, V., Bruni, A., Aloi, M., Calabrò, G., Jaén-Moreno, M. J., Segura-Garcia, C., & De Fazio, P. (2019). Adverse childhood experiences and clinical severity in bipolar disorder and schizophrenia: A transdiagnostic two-step cluster analysis. Journal of Affective Disorders, 259, 104–111. https://doi.org/https://doi.org/10.1016/j.jad.2019.08.049
- Chadwick, P., Lees, S., & Birchwood, M. (2000). The revised beliefs about voices questionnaire (BAVQ-R). British Journal of Psychiatry, 177(3), 229–232. https://doi.org/https://doi.org/10.1192/bjp.177.3.229
- Daalman, K., Boks, M. P., Diederen, K. M., de Weijer, A. D., Blom, J. D., Kahn, R. S., & Sommer, I. E. (2011). The same or different? A phenomenological comparison of auditory verbal hallucinations in healthy and psychotic individuals. The Journal of Clinical Psychiatry, 72(3), 320–325. https://doi.org/https://doi.org/10.4088/JCP.09m05797yel
- Daalman, K., Diederen, K. M. J., Derks, E. M., van Lutterveld, R., Kahn, R. S., & Sommer, I. E. C. (2012). Childhood trauma and auditory verbal hallucinations. Psychological Medicine, 42(12), 2475–2484. https://doi.org/https://doi.org/10.1017/S0033291712000761
- Everitt, B. (1980). Cluster analysis. Quality and Quantity, 14(1), 75–100. https://doi.org/https://doi.org/10.1007/BF00154794
- First, M. B., Gibbon, M., Spitzer, R., Williams, J., & Benjamin, L. (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). American Psychiatric Press, Inc.
- Hardy, A. (2017). Pathways from trauma to Psychotic Experiences: A theoretically informed model of posttraumatic stress in psychosis. Frontiers in Psychology, 8, 697. https://doi.org/https://doi.org/10.3389/fpsyg.2017.00697
- Hardy, A., Emsley, R., Freeman, D., Bebbington, P., Garety, P. A., Kuipers, E. E., Dunn, G., & Fowler, D. (2016). Psychological mechanisms mediating effects between trauma and psychotic symptoms: The role of affect regulation, intrusive trauma memory, beliefs, and depression. Schizophrenia Bulletin, 42(1), S34–S43. https://doi.org/https://doi.org/10.1093/schbul/sbv175
- IBM Corp. (2017). IBM SPSS statistics for windows, version 25.0.
- Jacobs, J., Agho, K. E., Stevens, G., & Raphael, B. (2012). Do childhood adversities cluster in predictable ways? A systematic review. Vulnerable Children And Youth Studies, 7(2), 103–115. https://doi.org/https://doi.org/10.1080/17450128.2012.658886
- Johns, L. C., Kompus, K., Connell, M., Humpston, C., Lincoln, T. M., Longden, E., Preti, A., Alderson-Day, B., Badcock, J. C., Cella, M., Fernyhough, C., McCarthy-Jones, S., Peters, E., Raballo, A., Scott, J., Siddi, S., Sommer, I. E., & Larøi, F. (2014). Auditory verbal hallucinations in persons with and without a need for care. Schizophrenia Bulletin, 40(4), S255–S264. https://doi.org/https://doi.org/10.1093/schbul/sbu005
- Larøi, F., Marczewski, P., & Van der Linden, M. (2004). Further evidence of the multi-dimensionality of hallucinatory predisposition: Factor structure of a modified version of the Launay-Slade Hallucinations Scale in a normal sample. European Psychiatry, 19(1), 15–20. https://doi.org/https://doi.org/10.1016/S0924-9338(03)00028-2
- Larøi, F., Sommer, I. E., Blom, J. D., Fernyhough, C., Ffytche, D. H., Hugdahl, K., Johns, L. C., McCarthy-Jones, S., Preti, A., Raballo, A., Slotema, C. W., Stephane, M., & Waters, F. (2012). The characteristic features of auditory verbal hallucinations in clinical and nonclinical groups: State-of-the-art overview and future directions. Schizophrenia Bulletin, 38(4), 724–733. https://doi.org/https://doi.org/10.1093/schbul/sbs061
- Larøi, F., Thomas, N., Aleman, A., Fernyhough, C., Wilkinson, S., Deamer, F., & McCarthy-Jones, S. (2019). The ice in voices: Understanding negative content in auditory-verbal hallucinations. Clinical Psychology Review, 67, 1–10. https://doi.org/https://doi.org/10.1016/j.cpr.2018.11.001
- Lincoln, T. M., & Peters, E. (2019). A systematic review and discussion of symptom specific cognitive behavioural approaches to delusions and hallucinations. Schizophrenia Research, 203, 66–79. https://doi.org/https://doi.org/10.1016/j.schres.2017.12.014
- Luhrman, T., Alderson-Day, B., Bell, V., Bless, J. J., Corlett, P., Hugdahl, K., Jones, N., Larøi, F., Moseley, P., Padmavati, R., Peters, E., Powers, A. R, & Waters, F. (2019). Beyond trauma: A multiple pathways approach to auditory hallucinations in clinical and nonclinical populations. Schizophrenia Bulletin, 45(1), S24–S31. https://doi.org/https://doi.org/10.1093/schbul/sby110
- Moritz, S., & Larøi, F. (2008). Differences and similarities in the sensory and cognitive signatures of voice-hearing, intrusions and thoughts. Schizophrenia Research, 102(1-3), 96–107. https://doi.org/https://doi.org/10.1016/j.schres.2008.04.007
- Offen, L., Waller, G., & Thomas, G. (2003). Is reported childhood sexual abuse associated with the psychopathological characteristics of patients who experience auditory hallucinations? Child Abuse & Neglect, 27(8), 919–927. https://doi.org/https://doi.org/10.1016/s0145-2134(03)00139-x
- Rosen, C., McCarthy-Jones, S., Jones, N., Chase, K. A., & Sharma, R. P. (2018). Negative voice-content as a full mediator of a relation between childhood adversity and distress ensuing from hearing voices. Schizophrenia Research, 199, 361–366. https://doi.org/https://doi.org/10.1016/j.schres.2018.03.030
- Rossell, S. L., Schutte, M. J. L., Toh, W. L., Thomas, N., Strauss, C., Linszen, M. M. J., Van Dellen, E., Heringa, S. M., Teunisse, R., Slotema, C. W., & Sommer, I. E. C. (2019). The Questionnaire for Psychotic Experiences: An examination of the validity and reliability. Schizophrenia Bulletin, 45(1), S78–S87. https://doi.org/https://doi.org/10.1093/schbul/sby148
- Scott, M., Rossell, S. L., Meyer, D., Toh, W. L., & Thomas, N. (2020). Childhood trauma, attachment and negative schemas in relation to negative auditory verbal hallucination (AVH) content. Psychiatry Research, 290, 112997. https://doi.org/https://doi.org/10.1016/j.psychres.2020.112997
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–57.
- Sheffield, J. M., Williams, L. E., Blackford, J. U., & Heckers, S. (2013). Childhood sexual abuse increases risk of auditory hallucinations in psychotic disorders. Comprehensive Psychiatry, 54(7), 1098–1104. https://doi.org/https://doi.org/10.1016/j.comppsych.2013.05.013
- Shevlin, M., Dorahy, M., & Adamson, G. (2007). Childhood traumas and hallucinations: An analysis of the national comorbidity survey. Journal of Psychiatric Research, 41(3-4), 222–228. https://doi.org/https://doi.org/10.1016/j.jpsychires.2006.03.004
- Slade, P., & Bentall, R. (1988). Sensory deception: A scientific analysis of hallucination. Johns Hopkins University Press.
- Sommer, I. E. C., Daalman, K., Rietkerk, T., Diederen, K. M., Bakker, S., Wijkstra, J., & Boks, M. P. M. (2010). Healthy individuals with auditory verbal hallucinations; Who are they? Psychiatric assessments of a selected sample of 103 subjects. Schizophrenia Bulletin, 36(3), 633–641. https://doi.org/https://doi.org/10.1093/schbul/sbn130
- Stevens, L. H., Turkington, D., Drage, L., Morrison, T., Muncer, S., Spencer, H. M., & Dudley, R. (2019). Investigation of a traumatic psychosis subgroup: A cluster analysis of an antipsychotic free cohort. Psychosis, 11(4), 298–307. https://doi.org/https://doi.org/10.1080/17522439.2019.1628290
- Thombs, B. D., Bernstein, D. P., Lobbestael, J., & Arntz, A. (2009). A validation study of the Dutch childhood trauma questionnaire-Short form: Factor structure, reliability, and known-groups validity. Child Abuse & Neglect, 33(8), 518–523. https://doi.org/https://doi.org/10.1016/j.chiabu.2009.03.001
- Valavanis, S., Thompson, C., & Murray, C. D. (2019). Positive aspects of voice-hearing: A qualitative metasynthesis. Mental Health, Religion & Culture, 22(2), 208–225. https://doi.org/https://doi.org/10.1080/13674676.2019.1601171
- van Nierop, M., Lataster, T., Smeets, F., Gunther, N., van Zelst, C., de Graaf, R., ten Have, M., van Dorsselaer, S., Bak, M., Myin-Germeys, I., Viechtbauer, W., van Os, J., & van Winkel, R. (2014). Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: Analysis of a large, representative population-based sample. Schizophrenia Bulletin, 40(2), S123–S130. https://doi.org/https://doi.org/10.1093/schbul/sbt150
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., Read, J., van Os, J., & Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661–671. https://doi.org/https://doi.org/10.1093/schbul/sbs050
- Ward, J. H. (1963). Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association, 58(301), 236–244. https://doi.org/https://doi.org/10.1080/01621459.1963.10500845