ABSTRACT
Objective
The purpose of this study was to examine cultural beliefs, attitudes, and practices of Black sub-Saharan Africans (BsSAs) in the UK regarding their type 2 diabetes (T2D) self-management using the concepts of the PEN-3 cultural model.
Method
A qualitative study involved 36 semi-structured interviews with BsSAs living with T2D in the UK to examine relevant cultural practices and beliefs that have contributed to the uneven burden of self-management behaviours. A narrative thematic analysis of the data was then conducted for the study using NVivo software and guided by the PEN-3 cultural model, which moves beyond individualistic health behaviour models of diabetes but centralises culture in understanding health behaviours.
Results
Cultural perceptions and self-management behaviours of T2D varied among the BsSAs. Systems of self-management and treatment practices that were congruent with their cultural beliefs and personal priorities were seen as essential in the positive response to self-managing T2D. Knowledge and perceptions of non-conventional and alternative remedies linked to cultural beliefs reflected the existential health-seeking behaviours, and the significance attached to BsSAs negotiated cultural identities and collective practices within the communities. Social network supports were seen as enablers while advice and regimens from healthcare professionals (HCPs) were presented as medicalised and devoid of cultural sensitivities to respondents.
Conclusion
The study findings highlight the need to be not only aware of the negative impact of diabetes perceptions and health behaviours among the BsSA communities, but also be aware of the enabling factors and collective practices within the communities that are equally critical in influencing the self-management and health-seeking decisions of BsSAs living with T2D. PEN-3 model was significant with exploring not only how cultural context shapes health beliefs and practices, but also how social networks and systems play a critical role in enabling or nurturing positive health behaviours and health outcomes.
Introduction
Type 2 diabetes (T2D) is classified as the fastest-growing public health challenges to the UK health system (Diabetes UK Citation2019). It has a significant impact on increased mortality and morbidity, health inequalities and reduced life expectancy, especially among Black and Minority Ethnic (BME) groups (McCormack and Grant Citation2013; Diabetes UK Citation2019). Black sub-Saharan African (BsSA) communities are one of the most affected BME groups as they are up to three times more likely than people of White European origin to be diagnosed with T2D (Tillin et al. Citation2012; Diabetes UK Citation2019). The BsSA population is one of the ethnic minority groups with known health disparities, especially in health issues related to unhealthy behaviours and lifestyle such as obesity, diabetes, cardiovascular disease and other health complications resulting from an individual’s ways of living and self-management (Carr Citation2012; Harrison Citation2014).
Self-management
Self-management as an essential aspect of self-care for a long-term health condition, such as diabetes, requires individual responsibility and actions directed towards the individual, community or environment in order to enable people to live healthy and functional lives, and support their well-being (Funnell et al. Citation2011; Grady and Gough Citation2014). Several self-management models have been developed to maximise treatment efficacy and clinical outcomes and to reduce unnecessary health risks and unhealthy behaviours (Modi et al. Citation2012). However, there has been a shift from individualistic health behaviour models to collective social network and social capital frameworks that recognise other external factors that influence health decisions and outcomes within communities (Grace et al., Citation2008; Coulter, Roberts, and Dixon Citation2013; Vassilev et al. Citation2014). Several studies have shown that diabetes self-management is culturally embedded. These studies acknowledged the importance of knowledge and understanding of other external social-cultural factors and practices that influences individuals’ self-management behaviours (Greenhalgh, Helman, and Chowdhury Citation1998; Murphy et al., Citation2011; Nam et al. Citation2011; Patel et al. Citation2015). Similarly, Abubakari et al. (Citation2013) emphasised that people’s understanding and interpretation of health management and other actions and beliefs that pertain to health could be shaped by people’s broader social and behavioural factors such as cultural context and collective health beliefs. Individual culturally driven health behaviours are often an important component of more holistic self-management models.
Several socio-cultural factors have been identified as barriers to the embracing of healthy lifestyles and behaviours, engagement with the National Health Service (NHS) interventions programme in the UK and the emergence of health inequalities among individuals with T2D (Brown, Avis, and Hubbard Citation2007; Abubakari et al. Citation2013; Patel et al. Citation2015). The diverse dynamics of cultural beliefs and practices influence people’s actions in rejecting standard biomedical treatments in favour of self-care, home remedies and consultation with non-medical practitioners (Harrison Citation2014). Previous studies provide insight into some of the contributing factors to poor health behaviours and outcomes among the BME groups (Brown, Avis, and Hubbard Citation2007; Johnson et al. Citation2011; Carr Citation2012; Abubakari et al. Citation2013). However, there is a significant gap in the research literature related to the influence of socio-cultural factors on T2D self-management behaviour among BsSA communities in the UK. This study used an emic research perspective to understand how cultural beliefs and health-seeking practices shape health behaviours and experiences to understand T2D self-management among BsSA communities as distinct from other BME groups. The illness experience from inside this cultural group also contributes to broader conceptions of health behaviours and the understanding of the complexity of culture, which does not easily fit into a medicalised care model of T2D in the UK. This paper argues there is a need to identify the social and cultural factors that perpetuate not only the construction of T2D but also how to manage the use of non-conventional health practices for T2D within BsSA communities.
Conceptual framework: the PEN-3 cultural model
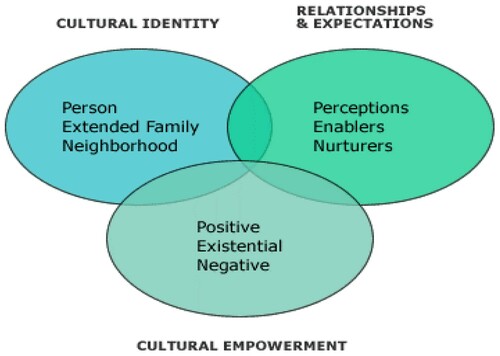
Understanding the broader cultural contexts in which a person or a particular group lives provides a deeper level of interpretation of health behaviours that could be a better guide for delivering culturally congruent health care interventions. Historically, interventions used to address health issues in various cultural groups have often suffered from focusing on health behaviours through a bio-medical or biopsychosocial lens (Eckersley Citation2006). Health issues embedded in cultural practices within a community are often invisible and thus overlooked, and the strategies that are designed and implemented fail to achieve any impact on collective health behaviours. To address this gap, concepts from the PEN-3 cultural model (see ) were adopted for this study as a comprehensive approach to address the complexity of cultural beliefs and practices associated with self-management behaviours among the BsSA communities. The PEN-3 cultural model explicitly contextualises the role of culture in shaping the understanding of, and actions towards, diabetes self-management. The model consists of three dimensions that are dynamically interrelated and interdependent: Cultural Empowerment, Relationship and Expectations, and Cultural identity (Airhihenbuwa and Webster Citation2004). The study utilised the three domains to address not only the positive, existential and negative aspect (Cultural empowerment) of self-management behaviours but also to explore the role of collective social networks and practices (Cultural identity) as enablers and nurturers (Relationship and Expectations) of health-seeking behaviours and health-related decisions among the BsSA communities. Utilising the PEN-3 cultural model and focusing on how cultural contexts shape T2D self-management behaviours, may provide health care providers (HCPs) and policymakers with valuable guidelines for ensuring that recommended programmes are culturally specific and have the collective cultural components that would fit the health needs of the BsSA communities.
Figure 1. The PEN-3 Cultural Model (Airhihenbuwa and Webster Citation2004).
The central argument in this study is that knowledge of cultural belief, and of how members of that cultural environment use this knowledge, offers an in-depth understanding of the lived experience of people living with T2D that can potentially promote more holistic and integrative diabetes self-care. The aim of this study, therefore, was to explore and provide analysis of the interrelationship and significance of illness perceptions, cultural beliefs and practices in T2D self-management among BsSA communities.
Methods
Research design
The study adopted a qualitative emic research strategy to explore, describe and interpret the lived experiences and self-management behaviours of BsSAs living with T2D in the UK (Creswell Citation2014). This approach was chosen to obtain insiders’ perspectives on self-management and health-seeking practices in a set of cultural and subcultural contexts (Fetterman Citation2010). This strategy allows for deeper understanding and study of core cultural knowledge(s), beliefs and behavioural patterns, and practices associated with T2D self-management outside the standard biomedical knowledge framework. This method was able to gather rich knowledge and understanding of BsSAs’ lived experiences with T2D. It highlights how knowledge is woven through different levels of complexity and contestation in the respondents and their cultural environments (Hammersley and Atkinson Citation2007).
Description of sample
This study was undertaken with 36 people living with T2D (Age range 35–65years) from BsSA communities in the UK (see ). It took place in specific geographical areas heavily populated by the BsSA communities. A purposive sampling approach was used to recruit participants through community channels such as self-help and support groups, churches, mosques, families and friends. These channels were seen as natural settings where participants would be willing to participate in the research voluntarily.
Table 1. Demographics of participants (BsSAs with T2D).
Data collection
Primary data were collected between 2016 and 2,017 using semi-structured interviews and field notes. The principal researcher conducted the interviews for the study. The semi-structured interview was based on a topic guide, and the process sought to understand and interpret patterns of health-seeking behaviours related to T2D management among the BsSA communities. The principal researcher’s BsSA identity and familiarity with the cultural beliefs of the BsSA communities facilitated the recruitment of the participants, access, communication and building of trust during the data collection process. It allowed an open discussion with participants to yield rich information and descriptions of their experiences and views on living with T2D as a BsSA living in diaspora communities in the UK (Silverman Citation2013). Interviews lasted between 45 and 60 min, each with open-ended questions to facilitate discussion with participants. All conversations were recorded with consent from all participants.
Data analysis
Using a narrative thematic analysis approach, the principal researcher organised and categorised the data through a coding process to generate emerging themes from the research findings (Creswell Citation2014). The PEN-3 cultural model was then used as a guide to identifying the interrelationship between and within each of the categories and emerging themes. It identifies explicitly responses that represent cultural empowerment, relationship and expectations within the cultural context of the study. All interviews were transcribed verbatim by the principal researcher to ensure the accurate representation of collected data. Each audio-recorded interview was compared with the discussion notes and reflective diary notes kept by the researcher to enable reflection on the responses. The audio recordings used in the semi-structured interviews allowed the researcher to become familiar with the data, and coded responses were categorised using NVivo software. All transcripts were given unique codes and numbers for identification, and non-narrative lines and any other information that could identify participants were removed. Combining and comparing narratives from several people from different BsSA communities using a triangulation approach helped to examine the evidence from the various sources within the communities and build coherence of the themes identified from the findings (Creswell Citation2014). Attention was given to data whose accounts differed notably from other participants during the interview. Triangulating the data by comparing with each other helped to reduce bias (Silverman Citation2013). A follow-up phone call to some participants and further discussion with the self-help groups was carried out to clarify responses and to explore emerging themes of the research to validate the findings (Creswell and Miller Citation2000).
Results
The findings show several differences in the perceptions, experiences and knowledge of BsSAs diabetes self-management behaviours. The demographics of the participants in the study are presented in . The study findings are presented under three key themes generated from the qualitative data and categorised using the PEN-3 model as a guide: Beliefs and knowledge about T2D (relationships and expectations), social stigma and self-denial of T2D (cultural empowerment) and the use of alternative remedies for diabetes self-management (cultural identity).
Beliefs and knowledge about T2D management
Perceptions
One of the themes that emerged to explain T2D self-management behaviours was the knowledge and perceptions about T2D. Beliefs and knowledge in the context of this study refer to the lived experiences of BsSAs with T2D. Participants associated their beliefs and knowledge about T2D more on personal and family experiences, and defined diabetes only in terms of sugar, which often does not coincide with the medical perspective of diabetes:
You only get it from sugar, don’t you? When you eat a lot of sugar, and you have them stored in your body. (BALWD#14)
I have heard that if you urinate and you taste it if it is sweet [sic], you have diabetes, and if it is not sweet, you do not have it. We call diabetes ‘sugar’ in my cultural language. I understood this well when I was diagnosed with diabetes. My urine became sweet (BSSALWD#17)
I was told diabetes are only caused by starchy foods, such as rice, pasta, bread and sugar … so I think I must have gotten my diabetes from the starchy food I eat … my sugar level even gets too high each time I eat too much bread or fried plantain (BALWD#3)
Many of us go for canned foods like canned fish, beans, sausage and tuna … we can now see that most of these foods are chemically processed, and they expose us more to diseases like diabetes. You don’t even know what they use to preserve them. Back in Africa, there is no need to preserve with chemicals because we eat mostly natural food and cook them fresh (BSSALWD#1)
Family influence on perception and beliefs
According to the participants, friends and families were primary sources of their knowledge about T2D signs and symptoms even before diagnosis. Family history and experience of T2D, particularly the perceived risk, has a strong influence on participants’ attitude and beliefs. Perceptions of becoming diabetic and understanding the risk of the disease come mainly from recognising family members’ experiences with diabetes and the related complications (including excessive sweating, loss of weight, poor eye sights, limb amputation etc.), much more than individual behaviour and other risk factors that could impact on self-management behaviour.
My family on both sides have it; I was told my grandfather had it, so I was able to relate to it when I was diagnosed. I have always known that I would have it. Therefore, it was left to me to prepare myself and understand how I can manage it (BALWD#8)
I do not know what the cause of it is, we have it in my family, my grandfather died of it, my mother had it, my aunties have it, and most of their children have it. We all have it in the family, some are on insulin, and some are not. It is a disease within my family. (BALWD#31)
I am 58 years now, and I have had my diabetes for a long time. Not so much has changed from what your doctor tells us. It’s still the same thing over and over again. Maybe a change of medication, but every other thing else is always the same. (BALWD#11)
Modification of the African diet
Within the context of nutrition, the modification of traditional African diets was another sub-theme that emerged from the study. In response to perceptions about self-managing T2D, participants felt it was important to them to adhere to their cultural values and, therefore, they preferred to modify their traditional African diet rather than ruling out their foods completely. Participants noted that specific food choices and cultural ways of preparation that affirms cultural beliefs and family values should be seen as positive practices.
… though you often feel you will get more energy eating our diet (shoulder shrug), then it is all filled with lots of starch, and if you do not balance your diet with other nutrients, it becomes harmful to your body. (BSSALWD#3)
I have not changed my [African] diet since I have been diagnosed. I eat what every other person eats [in the family], but I eat in moderation. Eating and cooking together in the family is a tradition and culture we respect very much in our community. I must still admit that eating in moderation really helps in regulating my sugar level. (BSSALWD#15)
It is very difficult staying on a diet when I have to cook for others. Most of the times, I have to take out my portion before [sic] seasoning the rest. It is a struggle doing this every day whilst trying to follow recommended doctor’s regimens. (BSSALWD#2)
You understand modifying your diet can sometimes be very upsetting for women. She wants to see me eat, but she ends up getting upset when she cooks, and I tell her that I cannot eat it. Women take this as being inconsiderate; you know [sic] (BSSALWD#17)
Would you believe that whenever I go home for a holiday in Zimbabwe, my diabetes disappears? I never take my medication because I eat good [unprocessed] and natural food. (BSSALWD#15)
GPs tell you some of your traditional food is not the healthiest food, especially when you have been diagnosed with diabetes, but still, you choose to eat them because of cultural values and beliefs. We often have strong family bond and beliefs around some these foods, we see them as natural medications, but could be difficult to change them completely whilst trying to follow the GP’s diet regimens (BSSALWD#27)
Social stigma and self-denial
Social stigma
This study showed limited awareness and many misconceptions about T2D among the BsSA communities as key factors driving the social stigma of diabetes and the consequent feelings of discrimination that engendered amongst the communities.
Once people see you are taking insulin, especially in my culture and community [sigh] they put on this sympathy look; people think you have a killable disease. People need to be more aware of the risk associated with this disease. It doesn’t mean you will die because you have it. (BALWD#5)
Sometimes, I feel ashamed to go out, especially when you have to go out to visit friends or go to another family’s house for lunch or dinner. (BALWD#12)
No, diabetes is not something that you would like to discuss with friends or families. You just don’t talk about health issues like type 2 diabetes. (BSSALWD#7)
It sounds improper discussing your health in a social setting. You are meant to be having fun, not making others feel responsible for your health or safety [in terms of having the right food]. (BSSALWD#22)
I felt awful, really bad about it. Sometimes I even lock myself in the room. I remember when I was first diagnosed; I will lock myself in the room and cry my heart out. I felt bad and sad when I got to know I have it (BALWD#2)
I still struggle with accepting it. I ask myself why me? Even though we have some people in my family, that has it, but I still feel bad that unfortunately, I am one of those that unfortunately will have to live with it. (BALWD#8)
It is important you let your family be aware of your diabetes. If they don't know you have it, how would they offer you help when you urgently need it? (BSSALWD#13)
Diabetes is a big stigma-related problem in our community, especially among the Black African community because of lack of awareness and ignorance of people. Going for treatment or diagnosis at the hospital is not always the first call for people because of the stigma. People self-diagnose, self-medicate, and some just ignore it because of beliefs or other family commitment. (BALWD#1)
Self-denial
Participants described how they lived with their diabetes; some were reluctant to accept their diagnosis and others seem to prioritise other aspects of life. Many feel frustrated and angry about their diagnosis or at the risk of the disease. For many, managing diabetes can be overwhelming, particularly for those that had no prior family history of diabetes and those assumed to be living a healthy lifestyle.
I felt awful, really bad about it. Sometimes I even lock myself in the room. I remember when I was first diagnosed; I will lock myself in the room and cry my heart out … I felt bad and sad when I got to know I have it (BALWD#2)
I still struggle with accepting it. I felt angry; I wanted to blame somebody responsible for it. I ask myself why me? Even though we have some people in my family, that has it, but I still feel bad that unfortunately, I am one of those that unfortunately will have to live with it. (BALWD#27)
You only live this life once and will die of something someday. Some people still live with their diabetes and live a normal life; eat what they want, so why should I worry so much because of what one doctor says to me (BALWD#23)
Use of alternative remedies for diabetes self-management
Another key finding in the study was the belief in, and use of, traditional and alternative remedies and also the importance of spiritual and religious beliefs that directly relates to their African heritage. The use of these remedies to manage their T2D is closely associated with their traditional and family cultural beliefs. The tensions between study participants’ cultural beliefs about T2D and translating their cultural ideas into health-seeking practices were apparent when they self-managed the disease daily.
Efficacy of alternative remedies
Cultural factors relating to BsSAs’ belief systems that influence health behaviours include the integration of traditional and alternative remedies into their every day health behaviour practices. These alternative remedies were perceived to be effective, but also participants demonstrated they use them because of their fear and mistrust of medical treatments for T2D. Many expressed trust in specific herbal remedies, which were used both independently or in combination with prescribed medication. Some of the participants expressed fear and mistrust of their medical treatment. Natural remedies were seen as more affordable and have cultural value, and the belief that traditional treatments were tried and trusted:
I use Aloe Vera to lower my blood sugar. You need something very bitter to help you reduce your sugar consumption in the body. I grow this in my garden, and I used them regularly (BSSALWD#2)
My major concern was that I got scared and afraid of the way my GP keeps changing my medication without proper examination, and these changes have made my diabetes feel worse than before. So, I’ve decided to be using more of natural herbs, they are accessible for me, and that has now improved my health. (BALWD#9)
I believe in traditional remedies, and I know some of them works for diabetes. My mother has diabetes as well, and she usually uses herbs and bitter kola, it is called Orogbo in the Yoruba language. She usually gets from Nigeria to manage her sugar level, so I use it as well. They are quite very bitter, but I use it most of the time. I have sincerely seen changes in my diabetes in the past months and has reduced the way I depend on medication (BSSALWD#21)
If I keep using the herbs, I’m using now, which I know it’s working for me, I know I will soon stop taking my medication completely. (BSSALWD#7)
I use my own traditional remedy as well as my medical medication. It is a mixture of herbs and green vegetables, which my wife usually does for me to help my diabetes. It helps to reduce my blood sugar level. It is a mixture of ginger, rosemary and pumpkin leaves (BSSALWD#11)
I was initially placed on just two metformin a day, and then it was increased to four by my doctor, in addition to other medications I take for my high blood pressure. All these medications will have a side effect on me in the long run because this will eventually get to a point where it becomes poisonous and toxic to my body. (BALWD#1)
Oral medications or insulin injections put chemicals into the body while natural remedies remove chemicals from the body. I feel like I’m close to death if I keep putting those chemicals into my body. (BALWD#10)
Religious beliefs and spirituality
Another significant finding was that prayer and spirituality were considered as an alternative and essential way of effectively controlling and managing their T2D. The majority of BsSAs in the study have a belief in God and practice either the Christian or Muslim faith. Most study participants prayed for their overall emotional, psychological and physical well-being, as well as some praying specifically for the cure of their T2D and other illnesses:
Prayer is my main key to my strength and managing my diabetes [sic]. You do not have power over a thing, we have to rely on and trust in God to take us through the situation (BSSALWD#3)
You put everything in prayers. Even though I don’t use medication to control my glucose level, I still put other remedies I use in prayer. (BSSALWD#10)
Most times when I fast and pray, I always feel better with my diabetes (BSSALWD#19)
I pray more now and spiritually committed to the things of God. I have gone through difficult phases of life since I have been diagnosed with diabetes. And this has only taught me to be closer to God and be more prayerful (BSSALWD#26)
It is part of our tradition in South Africa; we use oils, plants and herbs for treatment alongside prayers. They do not work in place of each other. The herbs and plants have their roles, and prayer has its purpose. We also need to pray for those herbs to work. We could pray on herb mixtures for days before being finally used on anyone that is sick. (BSSALWD#28)
Discussion
The study findings are translated into the PEN 3 framework (cultural empowerment, relationship and expectations, and cultural identity) to structure the discussion section. This qualitative study reveals many important cultural factors that influence self-management behaviours among BsSAs living with T2D. These results are based on the narratives from BsSAs living with T2D and demonstrated the differences in perceptions, knowledge and beliefs about T2D within the BsSA communities, and the underlying contestedness of cultural perspectives of health behaviours. Utilising the concepts of PEN-3 cultural model (see ) helps to identify and contextualise the role of cultural belief systems in shaping the understanding of and actions towards health and illness (Cowdery, Parker, and Thompson Citation2010; Iwelunmor, Newsome, and Airhihenbuwa Citation2014). It addresses the collective health behaviours of the BsSA communities beyond the biomedical and individualistic approach of diabetes intervention, and how this dynamic interrelationship of the identified factors creates a belief system outside of an individual’s control, which further determines their health decisions and the choice of treatments. The study findings show that cultural beliefs can shape self-management behaviours in multiple ways including, limiting knowledge and health literacy, misconceptions about diabetes, lack of adherence to or disengagement from prescribed medications, a strong belief in the efficacy of herbal and other alternative remedies, and the importance of religion and spirituality, and family kinship within BsSA communities. These study findings clearly show the dynamics of cultural beliefs and how these greatly influence how individuals understand, treat and self-manage their diabetes. The narratives from the BsSAs living with T2D reflects the collective sense of being of an individual, emphasising the cultural identity-sustaining ties of an individual through relationships with other people within the community and the impact on self-management behaviours (Modi et al. Citation2012; ).
People’s subjective practice of healing and health-seeking decisions are based on their cultural experiences, and the use of alternative remedies remains strong in the BsSA communities despite the contestedness of their use by biomedicine. Although biomedical knowledge and health professionals continue to exert firm paradigmatic control of illness narratives within mainstream healthcare, based exclusively on ‘scientific’ evidence and individualistic health behaviour models (Schoenberg et al. Citation2009), understanding the dynamics of cultural knowledge and practices, such as within the BsSA communities, remain an invisible yet powerful force for individuals to exert in the self-management of T2D. Utilising PEN-3 for the study enables a consideration of the cultural perceptions people living with T2D may have about their self-management behaviours, the actions that facilitate their health decisions and the influence of family and community practices in nurturing the behaviour. In this way, the narratives and interpretation of self-management behaviours are examined as functions of broader cultural contexts, rather than a medicalised approach, and particularly demonstrate how cultural belief systems define the roles of individuals and their relationship and expectations in family and community (Modi et al. Citation2012).
Another significant finding from the study relates to the modification of diet among the BsSA communities in the prevention and management of T2D. When discussing T2D in the Black African context, it is important to recognise the role of traditional food and diet patterns (Nettleton Citation2013). Although some study participants admitted that solely African diets were not a particularly good way to manage T2D due to the high composition of sugar, fat and starch and large portion sizes, many participants also argued that African food has curative and medicinal properties that could support their health. Study participants reported that traditional African food has a significant role in their way of life, especially at social and family events, such as ceremonies, weddings and festive activities, where families and friends share cultural food from the same plate. This is a key tradition that shows family cohesion and provides opportunities for building relationships (). Many study participants sought to alter their diets by reducing portion sizes of African foods, eating in moderation and making traditional dishes with less fat and oil. They believed that this process would allow them to manage their diabetes effectively. Nonetheless, participants acknowledged that modifying their traditional diets could be challenging when following through HCPs diet regimes because traditional African foods are generally seen as unhealthy. This finding of study participants struggling to modify their traditional diets have also been reported in other qualitative studies conducted among Afro-Caribbeans and South Asians within and outside the UK (Brown, Avis, and Hubbard Citation2007; Lawton et al. Citation2008; Bramble, Cornelius, and Simpson Citation2009; Johnson et al. Citation2011). Study participants with T2D believed that the struggle was as a result of the lack of cultural information about African diets included in diet regimens from HCPs. These findings support the arguments of Wood et al. (Citation2010) and Everson-Hock et al. (Citation2013) on limited dietary advice from HCPs and focus on western diet regimes for diabetes management. Also, the findings clearly illustrate the need for developing inclusive nutritional guidelines that include both the dietary values of African foods and suggestions of substitutes that could still offer culturally appropriate diets for managing T2D, as well as recognising traditional diets that have no harmful consequences. Thus, rather than disregarding culturally-tailored nutritional information that could enhance self-management among the BsSA communities, the PEN-3 cultural model affirms the potentials of improved health outcomes by encouraging health decisions that are positive while discouraging dietary decisions known to be harmful to health. The study findings are also likely to be relevant to lifestyle intervention programmes for other health disorders.
Social stigma and self-denial were identified as a major factor in health behaviours and a lack of self-confidence in disclosing illness or use of diabetes treatments among the BsSAs community. This supports the argument of Potter et al. (Citation2015) and Winkley et al. (Citation2015) about the importance of identifying diabetes as a stigma-related illness. It is often not recognised as such by HCPs. Some studies have linked misconceptions, lack of awareness and local health beliefs about diabetes to social stigma and discrimination (Brown, Avis, and Hubbard Citation2007; Mosnier-Pudar et al. Citation2010; Noakes Citation2010; Browne et al. Citation2013; Harrison Citation2014). Increased cases of stigma may reflect a lack of health education and awareness of T2D at the community level, reflecting stereotypical perceptions of cultural identity and the fact that health information is mainly disseminated through clinics and HCPs (Winkley et al. Citation2015). Good awareness of T2D and its related complications at community level and through community channels could contribute to better management, reduce the fear of stigma, and improve health behaviours among the studied communities.
The study findings also established that cultural practice of the use of alternative therapies play a significant role in diabetes self-management choices among BsSA communities and often create disengagement with mainstream healthcare services. Alternative treatments are used within a cultural landscape of treatment for people living with T2D. However, these practices are obscured behind the professionalised and medicalised processes designed for diabetes care (Uskul Citation2010). Concerns about the toxicity of prescribed medication (often for multiple illnesses) and the biomedical representation of diabetes were identified as contributing factors towards treatment choices and decisions. Consequently, the participants’ beliefs and practices around the use of traditional medicine as a form of ‘alternative’ to conventional medicines, reflect concerns about the medicalised approach to the treatment and management of T2D. Beliefs about T2D and the efficacy of alternative and traditional medicine are similar to those identified in studies among British South Asian and African Caribbean with T2D in the UK (Brown, Avis, and Hubbard Citation2007; Patel et al. Citation2015 and Lucas, Murray, and Kinra Citation2013) and outside the UK (Awah, Unwin, and Phillimore Citation2008; Ogbera et al. Citation2010; Keter and Mutiso Citation2012; Semenya, Potgieter, and Erasmus Citation2012; Chinenye and Ogbera Citation2013). Individual’s interpretation of the use of alternative remedies as a recognition of cultural values, and family and community practices potentially allows a more open discussion on the non-medical options of diabetes treatment, as opposed to the professional emphasis on medical treatment of diabetes. The findings from this study and other studies on the prevalent use of alternative and traditional medicines among the BsSA communities have shown that HCPs and other researchers need to be more aware of the significance of non-biomedical interventions in diabetes care and management (Keter and Mutiso Citation2012; Chinenye and Ogbera Citation2013). Herbal treatments and traditional foods are concurrently and interchangeably used with prescribed medication as an effective complementary treatment for T2D and overall well-being. The use of traditional remedies ties into their cultural beliefs, traditional practices and family experiences. It is, therefore, crucial that HCPs acknowledge and discuss the role and use of non-biomedical treatments and modalities in culturally-informed diabetes care at both individual and community level among the BsSA communities.
T2D is constructed as a multi-faceted public health issue that requires a rigorous approach from the aetiology of the disease to curative measures. Still, limited knowledge of cultural determinants amongst HCPs makes the health issue even more challenging (Diabetes UK Citation2019). The study findings demonstrate how the context of lay narratives and lived experiences of BsSAs with T2D can shape our understanding of how cultural beliefs influence their self-management behaviours. When people feel embedded in socio-cultural expectations and community relations, for example, values of cultural knowledge and family connectedness, their decisions of self-management may take a lower priority over efforts to solve other more immediate problems in their lives. Nettleton (Citation2013) and Vassilev et al. (Citation2014) argue that shared perceptions and shared lived experiences within communities are of key-value and importance to inform and negotiate relationships and collective interventions that can promote healthy outcomes and behavioural changes within a community. It is, therefore, necessary to recognise from the study findings that medical representations of illness and individualistic health behaviour models appeared to ignore the collective perspectives of diabetes care among the BsSA communities.
Implications of study
The findings from this study point out the need for specific understandings of the different groups and beliefs that makes up the BsSA communities and for the designing and implementation of specific diabetes programmes to be sensitive to those differences that exist within the communities. The study provides substantial evidence in support of the need for co-designing and co-participation treatment pathway, enabling both individual and community empowerment for innovative and integrative diabetic care that addresses both positive and negative impact of social-cultural practices among high-risk populations. The study proposes the PEN-3 cultural model (see ) as a tool, which promotes the importance of ethnographic approaches for engaging and empowering individual and community networks for inclusive diabetes care practices. Understanding the social construction of diabetes and health-seeking practices could enable HCPs to consider the wider underlying determinants normally unaccounted for in conventional health needs assessments. The PEN-3 cultural model offers guidelines for not only addressing the negative impact of culture on people’s beliefs and perceptions of health but also identifies the positive aspects of culture that recognises the role of collective perspectives when defining individual and community experiences. Such information would add value to the work of professional practices when dealing with BsSA communities concerning diabetes care and self-management behaviours.
Study limitations
The research approach adopted for the study was appropriate as it allows an in-depth understanding of the cultural contexts of health behaviours studied using concepts from the PEN-3 cultural model, but utilising mixed methods and other quantitative approaches could generate a more generalisable data for a wider population of BsSAs with T2D. Semi-structured interviews were conducted among BsSAs recruited only through community channels and the information obtained from narratives may be prone to bias; therefore, specific findings may need to be validated in other clinical and social settings. Despite these limitations, the findings provide a deep and rich understanding of the influence of cultural values and practices on diabetes self-management, in that it illuminates the experience of diabetes care beyond individualistic health behaviour models. Triangulation of the narratives from the participants, coupled with the consistency of findings with published studies on the role of cultural belief systems and practices on diabetes self-management and health-seeking behaviours, increases confidence in the analysis and validity of the data (Silverman Citation2013).
Conclusion
This study identifies a range of T2D-related beliefs, perceptions about cultural values and the use of traditional remedies as a form of alternative medicine, which plays a crucial role in shaping diabetes self-management behaviours among the BsSA communities. The narratives of T2D experiences among the BsSA communities explains the complex nature of culture and how it does not fit into the ‘medicalised’ care model of diabetes management in the UK. Nonetheless, participant narratives and utilising PEN-3 cultural model for the study helped in identifying the positive cultural values and harmony within family relationships and communities and how this can further strengthen the cultural relevance of diabetes programmes. The study findings underline the need for a behavioural change approach that moves beyond the biomedical and focuses on individuals, and takes account of the need for assessing and discussing cultural practices that could better enable more positive self-management behaviours. The identified cultural factors in this study offer routes that could facilitate the development of more appropriate interventions tailored to modifying beliefs and support culturally tailored diabetes intervention for improved health outcomes, leading to community participation. It is argued that T2D healthcare interventions should be enhanced through integrative approaches to treatment and the use of culturally sensitive strategies, and community-level interventions which consider not only the socio-cultural constraints to health behaviours but also acknowledge the cultural frames within which behavioural ‘choices’ and health-seeking practices are utilised amongst BsSA communities. Establishing lay views and experiences from this study has been valuable for understanding self-management behaviours amongst the studied population and the need for an integrated approach to diabetes care.
Acknowledgement
The authors would like to thank Professor Robert Dingwall, for his valuable comments and discussions in relation to this research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Abubakari, A. R., M. C. Jones, W. Lauder, A. Kirk, J. Anderson, D. Devendra, and E. K. Naderali. 2013. “Ethnic Differences and Socio-Demographic Predictors of Illness Perceptions, Self-Management, and Metabolic Control of Type 2 Diabetes.” International Journal of General Medicine 6: 617–628. doi:https://doi.org/10.2147/IJGM.S46649
- Airhihenbuwa, C. O., and J. D. Webster. 2004. “Culture and African Contexts of HIV/AIDS Prevention, Care and Support.” SAHARA: Journal of Social Aspects of HIV/AIDS Research Alliance 1 (1): 4–13. doi:https://doi.org/10.1080/17290376.2004.9724822
- Awah, P. K., N. Unwin, and P. Phillimore. 2008. “Cure or Control: Complying with Biomedical Regime of Diabetes in Cameroon.” BMC Health Services Research 8 (1): 43. doi:https://doi.org/10.1186/1472-6963-8-43
- Bramble, J., L. J. Cornelius, and G. M. Simpson. 2009. “Eating as a Cultural Expression of Caring among Afro-Caribbean and African American Women: Understanding the Cultural Dimensions of Obesity.” Journal of Health Care for the Poor and Underserved 20 (20): 53–68. doi:https://doi.org/10.1353/hpu.0.0158
- Brown, K., M. Avis, and M. Hubbard. 2007. “Health Beliefs of African–Caribbean People with Type 2 Diabetes: a Qualitative Study.” The British Journal of General Practice 57 (539): 461–469.
- Browne, J. L., A. Ventura, K. Mosely, and J. Speight. 2013. “‘I Call it the Blame and Shame Disease’: A Qualitative Study About Perceptions of Social Stigma Surrounding Type 2 Diabetes.” BMJ Open 3 (11): e003384. doi:https://doi.org/10.1136/bmjopen-2013-003384
- Carr, C. V. 2012. “Minority Ethnic Groups with Type 2 Diabetes: The Importance of Effective Dietary Advice.” Journal of Diabetes Nursing 16 (3): 88–96.
- Chinenye, S., and A. O. Ogbera. 2013. “Socio-cultural Aspects of Diabetes Mellitus in Nigeria.” Journal of Social Health and Diabetes 1 (01): 15–021. doi:https://doi.org/10.4103/2321-0656.109833
- Coulter, A., S. Roberts, and A. Dixon. 2013. Delivering Better Services for People with Long-Term Conditions: Building the House of Care, 1–28. King's Fund.
- Cowdery, J. E., S. Parker, and A. Thompson. 2010. “Application of the PEN-3 Model in a Diabetes Prevention Intervention.” Journal of Health Disparities Research and Practice 4 (1): 3.
- Creswell, J. W. 2014. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. London: SAGE.
- Creswell, J. W., and D. L. Miller. 2000. “Determining Validity in Qualitative Inquiry.” Theory Into Practice 39 (3): 124–130. doi:https://doi.org/10.1207/s15430421tip3903_2
- Diabetes UK. 2019. Diabetes: Facts and Statistics. https://www.diabetes.org.uk/resources-s3/2019-04/Diabetes%20UK%20Tackling%20the%20Crisis.pdf?.
- Eckersley, R. 2006. “Is Modern Western Culture a Health Hazard?” International Journal of Epidemiology 35 (2): 252–258. doi:https://doi.org/10.1093/ije/dyi235
- Everson-Hock, E. S., M. Johnson, R. Jones, H. B. Woods, E. Goyder, N. Payne, and J. Chilcott. 2013. “Community-based Dietary and Physical Activity Interventions in low Socioeconomic Groups in the UK: A Mixed Methods Systematic Review.” Preventive Medicine 56 (5): 265–272. doi:https://doi.org/10.1016/j.ypmed.2013.02.023
- Fetterman, D. M. 2010. Ethnography: Step-by-Step. Los Angeles: Sage.
- Funnell, M. M., T. L. Brown, B. P. Childs, L. B. Haas, G. M. Hosey, B. Jensen, M. Maryniuk, et al. 2011. “National Standards for Diabetes Self-Management Education.” Diabetes Care 34: S89–S96. doi:https://doi.org/10.2337/dc11-S089
- Grace, C., R. Begum, S. Subhani, P. Kopelman, and T. Greenhalgh. 2008. “Prevention of Type 2 Diabetes in British Bangladeshis: Qualitative Study of Community, Religious, and Professional Perspectives.” BMJ 337: a1931.
- Grady, P. A., and L. L. Gough. 2014. “Self-management: A Comprehensive Approach to Management of Chronic Conditions.” American Journal of Public Health 104 (8): e25–e31. doi:https://doi.org/10.2105/AJPH.2014.302041
- Greenhalgh, T., C. Helman, and A. M. M. Chowdhury. 1998. “Health Beliefs and Folk Models of Diabetes in British Bangladeshis: A Qualitative Study.” BMJ 316 (7136): 978–983.
- Hammersley, M., and P. Atkinson. 2007. Ethnography Principles in Practice. 3rd ed. London: Routledge.
- Harrison, G. 2014. “Health Beliefs of Black and Minority Ethnic Groups and the Implications for Diabetes Care.” Journal of Diabetes Nursing 18: 362–368.
- Iwelunmor, J., V. Newsome, and C. O. Airhihenbuwa. 2014. “Framing the Impact of Culture on Health: A Systematic Review of the PEN-3 Cultural Model and its Application in Public Health Research and Interventions.” Ethnicity & Health 19 (1): 20–46. doi:https://doi.org/10.1080/13557858.2013.857768
- Johnson, M., E. Everson-Hock, R. Jones, H. B. Woods, N. Payne, and E. Goyder. 2011. “What are the Barriers to Primary Prevention of Type 2 Diabetes in Black and Minority Ethnic Groups in the UK? A Qualitative Evidence Synthesis.” Diabetes Research and Clinical Practice 93 (2): 150–158. doi:https://doi.org/10.1016/j.diabres.2011.06.004
- Keter, L. K., and P. C. Mutiso. 2012. “Ethnobotanical Studies of Medicinal Plants Used by Traditional Health Practitioners in the Management of Diabetes in Lower Eastern Province, Kenya.” Journal of Ethnopharmacology 139 (1): 74–80. doi:https://doi.org/10.1016/j.jep.2011.10.014
- Lawton, J., N. Ahmad, L. Hanna, M. Douglas, H. Bains, and N. Hallowell. 2008. “‘We Should Change Ourselves, but we Can’t’: Accounts of Food and Eating Practices Amongst British Pakistanis and Indians with Type 2 Diabetes.” Ethnicity & Health 13 (4): 305–319. doi:https://doi.org/10.1080/13557850701882910
- Lucas, A., E. Murray, and S. Kinra. 2013. “Heath Beliefs of UK South Asians Related to Lifestyle Diseases: A Review of Qualitative Literature.” Journal of Obesity 2013. doi:https://doi.org/10.1155/2013/827674
- McCormack, S., and S. F. Grant. 2013. “Genetics of Obesity and Type 2 Diabetes in African Americans.” Journal of Obesity 2013: 1–12. doi:https://doi.org/10.1155/2013/396416
- Modi, A. C., A. L. Pai, K. A. Hommel, K. K. Hood, S. Cortina, M. E. Hilliard, S. M. Guilfoyle, W. N. Gray, and D. Drotar. 2012. “Pediatric Self-Management: A Framework for Research, Practice, and Policy.” Pediatrics 129 (2): e473–e485. doi:https://doi.org/10.1542/peds.2011-1635
- Mosnier-Pudar, H., G. Hochberg, E. Eschwege, S. Halimi, M. L. Virally, P. J. Guillausseau, C. Touboul, and S. Dejager. 2010. “How Patients’ Attitudes and Opinions Influence Self-Care Behaviours in Type 2 Diabetes. Insights from the French DIABASIS Survey.” Diabetes & Metabolism 36 (6): 476–483. doi:https://doi.org/10.1016/j.diabet.2010.08.004
- Murphy, K., D. Casey, S. Dinneen, J. Lawton, and F. Brown. 2011. “Participants’ Perceptions of the Factors that Influence Diabetes Self-Management Following a Structured Education (DAFNE) Programme.” Journal of Clinical Nursing 20: 1282–1292.
- Nam, S., C. Chesla, N. A. Stotts, L. Kroon, and S. L. Janson. 2011. “Barriers to Diabetes Management: Patient and Provider Factors.” Diabetes Research and Clinical Practice 93 (1): 1–9. doi:https://doi.org/10.1016/j.diabres.2011.02.002
- Nettleton, S. 2013. The Sociology of Health & Illness. 3rd ed. Cambridge: Polity Press.
- Noakes, H. 2010. “Perceptions of Black African and African-Caribbean People Regarding Insulin.” Journal of Diabetes Nursing 14 (4): 148–156.
- Ogbera, A. O., O. Dada, F. Adeleye, and P. I. Jewo. 2010. “Complementary and Alternative Medicine use in Diabetes Mellitus.” West African Journal of Medicine 29 (3). doi:https://doi.org/10.4314/wajm.v29i3.68213
- Patel, N. R., C. Chew-Graham, C. Bundy, A. Kennedy, C. Blickem, and D. Reeves. 2015. “Illness Beliefs and the Socio-Cultural Context of Diabetes Self-Management in British South Asians: A Mixed Methods Study.” BMC Family Practice 16 (1): 58. doi:https://doi.org/10.1186/s12875-015-0269-y
- Potter, L., K. Wallston, P. Trief, J. Ulbrecht, V. Juth, and J. Smyth. 2015. “Attributing Discrimination to Weight: Associations with Well-Being, Self-Care, and Disease Status in Patients with Type 2 Diabetes Mellitus.” Journal of Behavioral Medicine 38 (6): 863–875. doi:https://doi.org/10.1007/s10865-015-9655-0
- Schoenberg, N. E., E. M. Drew, E. P. Stoller, and C. S. Kart. 2009. “Situating Stress: Lessons from lay Discourses on Diabetes.” In Anthropology and Public Health: Bridging Differences in Culture and Society, 2nd ed., edited by R. A. Hahn, and M. C. Inhorn, 94–113. New York: Oxford University Press, Inc.
- Semenya, S., M. Potgieter, and L. Erasmus. 2012. “Ethnobotanical Survey of Medicinal Plants Used by Bapedi Healers to Treat Diabetes Mellitus in the Limpopo Province, South Africa.” Journal of Ethnopharmacology 141 (1): 440–445. doi:https://doi.org/10.1016/j.jep.2012.03.008
- Silverman, D. 2013. Doing Qualitative Research. 4th ed. London: SAGE.
- Tillin, T., N. G. Forouhi, P. M. McKeigue, and N. Chaturvedi. 2012. “Southall And Brent REvisited: Cohort Profile of SABRE, a UK Population-Based Comparison of Cardiovascular Disease and Diabetes in People of European, Indian Asian and African Caribbean Origins.” International Journal of Epidemiology 41 (1): 33–42. doi:https://doi.org/10.1093/ije/dyq175
- Uskul, A. K. 2010. “Socio-Cultural Aspects of Health and Illness.” Health Psychology 347–359.
- Vassilev, I., A. Rogers, A. Kennedy, and J. Koetsenruijter. 2014. “The Influence of Social Networks on Self-Management Support: A Metasynthesis.” BMC Public Health 14 (1): 719. doi:https://doi.org/10.1186/1471-2458-14-719
- Winkley, K., C. Evwierhoma, S. A. Amiel, H. K. Lempp, K. Ismail, and A. Forbes. 2015. “Patient Explanations for Non-Attendance at Structured Diabetes Education Sessions for Newly Diagnosed Type 2 Diabetes: A Qualitative Study.” Diabetic Medicine 32 (1): 120–128. doi:https://doi.org/10.1111/dme.12556
- Wood, F., M. Robling, H. Prout, P. Kimmersley, H. Houston, and C. Butler. 2010. “A Question of Balance: A Qualitative Study of Mothers' Interpretations of Dietary Recommendations.” The Annals of Family Medicine 8: 51–57. doi:https://doi.org/10.1370/afm.1072
