ABSTRACT
This study aims to determine whether breastfeeding duration affects the prevalence of nonrighthandedness in later life. A systematic search for studies on this topic was completed in 2018, and risk of bias was assessed by means of the Newcastle-Ottawa scale. Seven national surveys in five countries with Individual Participant Data (IPD) were identified (n = 62,129 mother-child dyads). These surveys had low risk of bias. An IPD meta-analysis showed that breastfeeding for < 1 month, 1 to 6 months, and > 6 months, when compared to bottle feeding, was associated with a 9%, 15% and 22% decreased prevalence of nonrighthandedness, respectively (Prevalence Ratio (PR) = 0.91, 95% confidence interval (ci): 0.83, 1.00; p-value = 0.05, PR = 0.85, 95% CI: 0.79, 0.92; p-value < 0.0001 and PR = 0.78; 95% CI: 0.71, 0.85; p-value < 0.0001). This dose-response relationship was significant (p < 0.001). No significant heterogeneity across surveys was detected (p-value > 0.54). Breastfeeding for longer than 9 months was not associated with further reductions in the prevalence for nonrighthandedness (p > 0.58). It is concluded that the critical age window for establishing hemispheric dominance in handedness includes the first 9 months of infancy and is in part determined by nurture.
Introduction
Controversy remains over whether breastfed and bottlefed infants have distinct neurodevelopmental life courses. Breastfed infants have been reported to have increased righthandedness, increased intelligence, increased head circumference, decreased speech problems, and decreased multiple sclerosis (Denny, Citation2012; Deoni et al., Citation2013; Isaacs et al., Citation2010; Ragnedda et al., Citation2015; Tomblin, Smith, & Zhang, Citation1997; Victora et al., Citation2015). Such associations have been interpreted as causal and explained on the biological basis that breastfeeding leads to increased myelinization and grey matter volume. (Deoni et al., Citation2013) These same associations however have also been interpreted as spurious; a reflection of the inability to disentangle breastfeeding from confounders such as socio-economic factors and health awareness (Girard, Doyle, & Tremblay, Citation2017). The aim of this report was to initiate a systematic search for existing data sources to conduct individual-participant-data meta-analyses on the assocation between breastfeeding and nonrighthandedness.
Materials and methods
Eligibility criteria for studies
A search was initiated for publications with information on the duration of breastfeeding as reported by the mother, and the handedness of their offspring. There was no a priori protocol, registration, or specification of entry criteria. The search criteria on pubmed (pubmed.gov) were ((handedness) AND breastfeeding) AND “(‘1920’[Date - Publication]: ‘3000’[Date - Publication])”. Individual Participant Data (IPD) for identified studies were requested. A search for additional sources of IPD of similar nature as those in the identified publication(s) followed. Common scales for duration of breastfeeding, handedness, and confounding variables were defined post hoc with the aim of maximizing the number of studies included, and maximizing the number of participants per study included. The risk of bias in the surveys was quantified using the 9-point Newcastle-Ottawa scale (Wells et al., Citation2000). Surveys in which breastfeeding and handedness information were collected at the same examination were considered case-control studies. A point was awarded for the representativeness of the series of cases when more than 80% of the population agreed to participate in the survey. Surveys in which breastfeeding was assessed in an examination which preceded the handedness assessment were considered cohort studies. A point was awarded for the representativeness of the exposed cohort when the survey response rate was above 80%. A follow-up rate in the cohort of > 80% was awarded a point. The primary exposure of interest were different durations of breastfeeding, including no breastfeeding.
Synthesis methods
The prevalence of nonrighthandedness was related to breastfeeding duration using a generalized linear model with a log link, a binomial error distribution, and a robust standard error for all studies combined (surveys as fixed effects and adjusting for within-family correlation of handedness) leading to a one-step meta-analysis (primary analysis) (Petersen & Deddens, Citation2008; Zeger & Liang, Citation1986). Probabilistic methods were employed to identify children within the same family (see Appendix for detail).
Dose-response relationships between breastfeeding duration and handedness were evaluated with the p-test for linear trend. The unequally spaced breastfeeding durations were interpolated to an approximate linear scale, and then transformed into an orthogonal polynomial. Details on the interpolation contrast matrices are provided in the appendix.
The prevalence of nonrighthandedness was also related to different levels of breastfeeding duration for each survey separately using the aforementioned statistical model. The survey-specific estimates were then summarized using a DerSimonian-Laird random-effects model leading to a two-step meta-analysis. For the two-step meta-analysis, the heterogeneity of the breastfeeding-handedness association across surveys was quantified with (i) the chi-square heterogeneity statistic, and (ii) the between-studies variance as a percent of total variance (r(i)).
Log-linear univariate regression models determined for each survey whether mother-child characteristics increased, decreased, or did not significantly affect the prevalence of breastfeeding. Breastfeeding in these analyses was defined as being of 1-month duration or more. Mother-child characteristics were dichotomized. The only exception to this dichotomization was birth outcomes which were classified into three groups; (1) premature or very low-birth-weight infants combined, (2) term-low-birth-weight infants, and (3) normal birth weight infants as the reference group. The associations between mother-child characteristics and the prevalence of breastfeeding were then summarized across surveys using a DerSimonian-Laird random-effects model. Heterogeneity across surveys was summarized by means of the (i) chi-square statistic for heterogeneity, and (ii) the between-studies variance as a percent of total variance (r(i)) (Hertzmark & Spiegelman, Citation2012).
Mother-child characteristics were interpreted as having a similar (i.e., non-heterogeneous or consistent) impact on the prevalence of breastfeeding across surveys when the chi-square statistic for heterogeneity across surveys was non-significant. Conversely, mother-child characteristics were interpreted as having heterogeneous (i.e., inconsistent) impact on the prevalence of breastfeeding across surveys when the chi-square statistic for heterogeneity was significant. This heterogeneity across surveys was further classified as qualitative or quantitative (Yusuf, Wittes, Probstfield, & Tyroler, Citation1991). The heterogeneity across surveys was termed qualitative when mother-child characteristics increased the prevalence of breastfeeding in one or more surveys and decreased the prevalence in other survey(s). The heterogeneity across surveys was termed quantitative when mother-child characteristics consistently increased or decreased the breastfeeding prevalence across surveys, but the magnitude of these prevalence increases or decreases varied significantly.
Risk of bias assessment
The potential biasing impact of mother-child characteristics on the breastfeeding-handedness association was assessed by calculating the percent change in the magnitude of the prevalence ratios between unadjusted (crude) and adjusted one-step and two-step models (((calculated as (PRadjusted−PRcrude)/PRcrude)*100). The potential biasing impact of mother-child characteristics was also evaluated by comparing the adjusted prevalence ratios of one-step and two-step meta-analyses. In the one-step meta-analyses, the quantitative or qualitative heterogeneity of mother-child characteristics and breastfeeding across surveys was ignored leading to a potential ecological bias. In the two-step meta-analyses, this ecological bias was automatically avoided by fitting a separate model for each study. Consistent results between one- and two-step meta-analyses thus suggest an absence of an ecological bias (and also an absence of other common reasons for one-step and two-step IPD meta-analyses to differ in their findings) (Burke, Ensor, & Riley, Citation2017). The impact of missing data was evaluated for the one-step meta-analysis using the methodology of Rubin (Rubin, Citation1987). The number of imputations was set to 25 and both missing nonrighthandedness (outcome variable) and missing explanatory variables were imputed (Rubin, Citation1987). The impact of ignoring the within-family correlations of observations of children from the same family was assessed by evaluating the change in the size of the standard error estimates when accounting for/ignoring the correlation.
Additional analyses
Mediation analyses evaluated whether the impact of mother-child characteristics on nonrighthandedness was mediated by breastfeeding (Valeri & Vanderweele, Citation2013). Breastfeeding for these mediation analyses was dichotomized as more or less than 1 month. Birth outcomes were classified into two groups; (1) premature or very low-birth-weight infants combined, versus (2) term-low-birth-weight and normal birth weight infants combined. The proportion explained by the mediator was not reported due to the inherent instability of such estimates (Mackinnon, Warsi, & Dwyer, Citation1995). The Attributable Risk percent (AR%) was calculated as the difference between the predicted probabilities of nonrighthandedness with exclusive bottle feeding and with breastfeeding for more than 6 months (Greenland & Drescher, Citation1993). These two prevalence estimates were adjusted for survey, birth year, infant sex, term-low-birth-weight infants, preterm infants, and very-low-birth-weight infants. None of these analyses were pre-specified.
Results
The Medline search specified in the Material and Methods section revealed 16 publications, 1 of which focused on the PICO question of interest (see Appendix IPD Flowchart). This study reported on two national surveys: the National Child Development Study (NCDS) which was started in 1958 in the United Kingdom (University of London, Citation2014), and the Growing Up in Ireland Study Child study (GUI-C), a cohort of 9-year-olds, which was started in 2007 (Department of Health-Ireland, Citation2010). A search was initiated for other national surveys with probability sampling. Sixteen National Health Examination Surveys conducted in the United States were screened, 10 continuous NHANES, NHES I-III, and NHANES I through III. Thirteen surveys did not contain information on the question of interest. Two continuous NHANES surveys (2011–2012 and 2013–2014) had limited information for a small subset of individuals and both these surveys were excluded. NHES II (1963–1965) planned to collect information on handedness and breastfeeding on all participants and was included. The NHES II survey was completed between 1963 and 1966, and about one-third of the participants were re-examined in the subsequent survey (United States Department of Health and Human Services, Citation1985). Four other national surveys were identified through other mechanisms. The Growing Up in Ireland Study Infant study (GUI-I) was started in 2008 (GUI-I), two Longitudinal Studies of Australian Children (LSAC) surveys were started in 2003-2004; a cohort of infants aged 0 to 1 (AUS-B), and a cohort of children aged 4 to 5 (AUS-K), and, the National Longitudinal Study Youth (NLSY) was started in 1979 (Frankel, McWilliams, & Spencer, Citation1983). IPD data were obtained for the 7 identified national surveys.
Study characteristics
Handedness was assessed by medical technologists, self-report, and psychologists in NHES II, by psychologists in AUS-K and AUS-B, by responsible household members in GUI-C and GUI-I, and by a mixture of self-report and responsible household member report in NLSY. Breastfeeding durations were self-reported in all surveys. Issues identified, and decisions made in checking and formatting IPD data across cohorts are detailed in the Appendix. Seven mother-child characteristics available for all cohorts were infant sex (male vs. female), non-singleton births (single vs. multiple births), parity (nulliparous vs. 1 to 3 prior births, and > 3 prior births), birth year (continuous), maternal age (continuous), a marker for socio-economic class (lowest quintile vs. others), and birth outcomes which was classified into 4 categories; premature infants (gestational length < 37 weeks and birthweight ≥ 1500 grams and < 2500 grams), very-low-birth-weight infants (birthweight < 1500 grams), term-low-birth-weight infants (gestational length ≥ 37 weeks, and birthweight < 2500 grams), and normal birthweight outcomes ( > 2500 grams). Mother's handedness, ancestry, and birth- and pregnancy-complications were available for a subset of the surveys.
Rules for data abstraction
Handedness in the identified cohorts was classified as righthanded and nonrighthanded. The latter category consisted of participants classified as lefthanded in two cohorts (GUI-C, GUI-I), and lefthanded or ambidextrous in the remaining five cohorts. Breastfeeding history was obtained from the responsible household member via interviews or questionnaires. Data analyses were limited to biological mother-child dyads. The primary analyses focused on 4 durations of breastfeeding identifiable in 6 cohorts: (i) no breastfeeding, (ii) breastfeeding ∼4 to 6 weeks (labeled as < 1 month), (iii) breastfeeding between 4 to 6 weeks and 6 months (labeled as 1 to 6 months), and (iv) breastfeeding for more than 6 months. Secondary analyses focused on breastfeeding durations of less than 1 month versus more than 1 month (identifiable in 7 surveys), and on breastfeeding durations of < 1 month, 1 to 6 months, 6 to 9 months, 9 to 12 months, and > 12 months (identifiable in 5 surveys).
Participant characteristics
There were 62,219 mother-child dyads in 7 surveys with questions which could be translated into the common scale of 3 levels of breastfeeding; less than one month, more than one month, and no breastfeeding. The birthyears of the infants/children ranged between 1951 and 2011. The prevalence of missing data for handedness and breast feeding was 10.6% and 2.9%, respectively. The prevalence of missing data for mother-child characteristics is shown in . There were 47,809 mother child-pairs where breastfeeding questions could be translated into the common scale of 4 levels of breastfeeding duration (no breastfeeding, < 1 month, 1 to 6 months, > 6 months). There were 40,971 mother child-pairs where breastfeeding questions could be translated into the common scale of 5 levels of breastfeeding duration (no breastfeeding, < 1 month, 1 to 6 months, 6 to 9 months, 9 to 12 months, and > 12 months).
Table 1. Prevalence of child handedness stratified by mother-child characteristics in 7 national representative cohorts (n = 62,129).
Risk of bias within studies ( and )
The average risk of bias measure for cohort and case-control surveys was 7 and 8 out of 9 possible points, respectively (the higher the score, the lower the bias).
Table 2. Risk of bias for surveys assessing breastfeeding prior to handedness.
Table 3. Risk of bias for surveys assessing breastfeeding history and handedness at same examination.
Table 4. Mother-child characteristics and their impact on the prevalence of breastfeeding across 7 national surveys.
Results of individuals studies
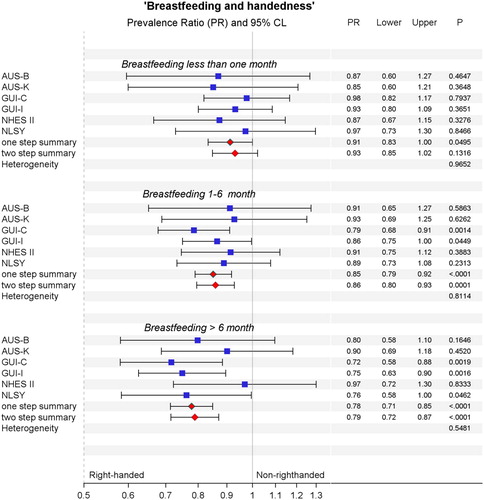
The number of nonrighthanders in each national survey is presented in , and the prevalence ratios and confidence intervals for nonrighthandedness in each cohort are presented in the forest plot ().
Results of syntheses
The results of the one-step meta-analysis on 47,809 mother-child pairs in 6 cohorts showed that breastfeeding for less than month, one to six months, and more than six months, when compared to exclusive bottle feeding, was associated with a 9%, 15% and 22% decreased prevalence for nonrighthandedness, respectively (). (Prevalence Ratio (PR) = 0.91, 95% confidence interval (CI): 0.83, 1.00; p-value = 0.05, PR = 0.85, 95% CI: 0.79, 0.92; p-value < 0.0001 and PR = 0.78; 95% CI: 0.71, 0.85; p-value < 0.0001). There was a significant linear dose-response relationship (p-value for linear trend: < 0.001). The summary estimates of the one-step and two-step meta-analyses and the chi-square measure of heterogeneity are presented in the forest plots of . The between-studies variance as a percent of total variance was zero for the three estimates relating breastfeeding duration to handedness.
These findings were robust when compared to the one-step (or two-step) meta-analysis on the full sample of 62,129 mother-child pairs which showed that breastfeeding for less than one month, and more than one month, had a 7% and 16% decreased prevalence of nonrighthandedness when compared to bottle feeding (PR = 0.93, 95% CI: 0.87, 0.99; p-value < 0.05; PR = 0.84, 95% CI: 0.79, 0.89; p-value < 0.0001) (Figure 1 in Appendix). There was a significant linear dose-response relationship between breastfeeding duration and handedness (p-value for linear trend: < 0.001).
These findings were also robust when compared to the one-step (or two-step) meta-analysis on the sample of 40,971 mother-child pairs available in 5 surveys. There was a significant dose-response relationship between breastfeeding duration of up to 9 months and handedness (p-value for linear trend < 0.02). The lack of a dose-response relationship between breastfeeding duration past 9 months and handedness is shown in three ways. First, there was no significant dose-response between breastfeeding for 6 to 9, 9 to 12, and > 12 months and handedness (p-value for linear trend > 0.55). Second, breastfeeding 9 to 12 months (PR = 0.76, 95% CI: 0.67–0.87), or more than 12 months (PR = 0.77, 95% CI: 0.68–0.87) was associated with roughly the same reduction in the prevalence of nonrighthandedness as breastfeeding 6 to 9 months (PR = 0.79, 95% CI: 0.69–0.89) (Figure 2 in Appendix). And, third, breastfeeding for longer than 9 months (9 to 12 months, and > 12 months combined), when compared to breastfeeding 6 to 9 months, was not associated with a significant reduction in the prevalence for non-righthandedness (PR = 0.97, 95% CI: 0.85, 1.12; p-value = 0.70).
Risk of bias across studies
Female infants had a significantly increased prevalence of being breastfed (PR ratio, 1.02; 95% CI, 1.01–1.04) (Table ). Infants with birth complications, and infants with pregnancy complications, had a significantly lower prevalence of being breastfed (PR, 0.95; 95% CI, 0.93–0.98 and PR, 0.91; 95% CI, 0.86–0.96, respectively). There was no evidence of heterogeneity across surveys for these trends. Handedness of mother did not significantly affect the prevalence of infants being breastfed. Non-singleton births, premature and very-low-birth-weight infants, and term-low-birth-weight infants had a lower prevalence in breastfeeding across all surveys, but the magnitude of the prevalence decrease differed significantly in magnitude (quantitative heterogeneity). Parity, socio-economic status, mother's age and African ancestry increased breastfeeding prevalence in at least one survey, while it decreased the prevalence in at least one other survey (qualitative heterogeneity).
Assessment of robustness
The change in prevalence ratios between crude and adjusted models (adjusted for 7 mother-child characteristics) of individual patient data meta-analysis models (both one-step and two-step) with 4 levels of breastfeeding duration was on average less 1% (range from −3% to +2%). The prevalence ratios changed less than 1.2% when four mother-child characteristics available for a subset of the surveys, were included (Table 1 in Appendix). The results between the one-step and two-step meta-analyses results differed minimally (see , and Figure 1 and 2 in appendix). Infant sex, African ancestry, mother handedness, premature infants, very-low-birth-weight infants, and birth complications were independent predictors for nonrighthandedness, whereas non-singleton births, pregnancy complications, and term-low-birth-weight were not. Imputation of missing data for the one-stage model with 4 levels of breastfeeding (displayed in ) had minimal impact on the prevalence ratios. Ignoring the within-family correlations led to neglible changes in the standard errors.
Additional analyses
Mediation analyses showed that the impact of non-singletons births, prematurity and very low-birth-weight, infant sex, and African ancestry was in a statistically significant way (p < 0.005) mediated by breastfeeding. The highly significant impact of mother-handedness on child-handedness, in contrast, was not mediated by breastfeeding (p < 0.32). The predicted prevalence of nonrighthandedness with breastfeeding over 6 months versus bottle feeding was 10.4% and 13.3%, respectively.
Discussion
Breastfeeding for more than 6 months, when compared to bottle feeding, was associated with an absolute 3% decreased prevalence for nonrighthandedness, from 13% to 10%, respectively. Twenty-two percent, or about 1 in 5 cases of nonrighthandedness among bottle-fed infants may thus be attributable to a lack of breast feeding for more than 6 months. A dose-response relationship was identified. Breastfeeding up until 9 months decreased the prevalence of nonrighthandedness in a linear dose-response fashion. Breastfeeding infants after 9 months was no longer associated with further reductions in the prevalence of nonrighthandedness. Current findings thus suggest that the critical period of cerebral lateralization, the time window wherein brain lateralization is susceptible to nurture, starts sometime before the 3rd month in utero (Hepper, Citation2013) and ends in infancy before the age of 9 months.
The reported findings furthermore suggest that some suspected causes for nonrighthandedness are in part mediated by breastfeeding. For instance, the increased prevalence of nonrighthandedness among non-singleton births reflected in part an increased prevalence of bottle feeding non-singletons (Springer & Searleman, Citation1980). The impact of prematurity on handedness was similarly in part mediated by a lower prevalence of breastfeeding of premature infants. A minute proportion of the increased prevalence of nonrighthandedness among males was similarly explained by the increased prevalence of breastfeeding female infants. It should be noted that an opposite trend may be true in the developing world where females may be less likely to be breastfed (Jayachandran & Kuziemko, Citation2011). Ignoring breastfeeding can thus lead to an over- or under-estimate of suspected causes for nonrighthandedness depending on the social patterning of breastfeeding in the studied population.
The main strength of this study is an apparent low risk of bias. The random sampling methods employed in the included surveys reduced selection bias, the trained examiners and standardized data collection methods reduced information bias, and the public availability of survey data allows for independent verification of reporting biases or mistakes. Recall bias on breastfeeding duration appears minimal given that breastfeeding history with 1 year after delivery, or obtained years later, led to similar results. Information bias on handedness appears to be minimal given that the findings were robust with respect to whom assessed the handedness, at what age handedness was assessed, and whether handedness assessment included ambidexterity as a separate outcome from left-handedness. Other strengths of this study include the lack of heterogeneity of the breastfeeding-handedness association across seven cohorts, and the robustness of the findings towards the biasing impact of mother-child characteristics.
These design-and-analysis strengths in combination with biological coherence argues for a causal interpretation between breastfeeding and handedness. Bottle feeding has been associated with lower verbal intelligence in a large randomized trial on breastfeeding (Kramer et al., Citation2008; Yang et al., Citation2018). Lower verbal intelligence in turn has been associated with non-right handedness in two epidemiological studies (D. W. Johnston, Nicholls, Shah, & Shields, Citation2009; D.W. Johnston, Nicholls, Shah, & Shields, Citation2013). Biological coherence therefore suggests that bottle-feeding may be a common causal factor for both handedness and verbal ability. If causal, current data do not allow further testing on whether breastfeeding increases the probability of right- and left-handed fetuses to become respectively righthanded and lefthanded in later life.
This suggestion of causality needs to be tempered with the non-transitivity of small correlation coefficients (Tao, Citation2014) and the inherent weaknesses of epidemiological evidence. The specific weaknesses of this study include the inconsistent definitions of mother-child characteristics across national surveys, the common reliance on mother's memory for mother-child characteristics such as birthweight, and the significant non-response rates in some national surveys. Furthermore, the nutritional content of both infant formula and breastmilk likely varied considerably across geography and history, and thereby created its own set of biases. The apparent robustness of the epidemiological findings across surveys is in a certain way remarkable. Possibly, the effect of breastfeeding on handedness is unrelated to nutrition, and instead mediated by the hormonal responses associated with mother-infant bonding during breastfeeding. An alternate interpretation of course is that another powerful hidden confounder, associated with breastfeeding, was missed. The safest conclusion may therefore be that handedness is related to nurture.
More reliable evidence on how breastfeeding affects lateralization requires the conduct of large randomized trials. This need for large sample sizes is mainly driven by an ethical consideration; women can be randomly assigned to breastfeeding promotion, but not to breastfeeding, and programmes based on promotion lead to small differences in the actual proportion of women bottlefeeding in the compared groups (Kramer et al., Citation2008). Due to the typically large non-compliance rates, it may well be that about 250,000 women need to be randomized to detect whether breastfeeding leads to 3% decreased prevalence of nonrighthandedness (details of calculations in Appendix). To determine whether half of the breastfeeding effect (i.e., a 1.5% decreased prevalence in nonrighthandedness) is due to the breastmilk itself (mother's breastmilk delivered via bottle only), as opposed to breastmilk combined with mother-child interactions (mother's breastmilk delivered with breastfeeding only), around 1 million women may need to be randomized (assuming similar non-compliance rates).
And even then, assuming the significant ethical and logistical challenges in the conduct of such large randomized controlled trials can be overcome, one still cannot exclude confounders such as the inactivation of bioactive components in stored breastmilk. While one may argue that the modelling of non-compliance rates in these sample size calculations is overly conservative, the calculations serve the point to illustrate the huge challenges in providing stronger evidence on the possible causal pathways which connect breastfeeding to brain lateralization.
In summary, the findings of this study offer an independent line of evidence that breastfeeding may enhance brain lateralization. This finding provides additional evidence to counter the arguments of those whom dismiss breastfeeding despite its evolutionary normality, and despite the precautionary principle. The counterpoint to this argument is that lifestyle recommendations should not be based on “the disastrous inadequacy of the lesser evidence” (lesser evidence being epidemiology) (Sackett, Citation2002). A universal breastfeeding recommendations for instance could cause more harm than good for vitamin B12 deficient mothers where breastfeeding may lead to cerebral atrophy of the infant (Kocaoglu et al., Citation2014). Considering such uncertainties, it appears unwise to make blanket clinical recommendations on the topic of breastfeeding and handedness.
Supplemental Material
Download MS Word (634.2 KB)Disclosure statement
No potential conflict of interest was reported by the author.
References
- Burke, D. L., Ensor, J., & Riley, R. D. (2017). Meta-analysis using individual participant data: One-stage and two-stage approaches, and why they may differ. Statistics in Medicine, 36(5), 855–875. doi: 10.1002/sim.7141
- Denny, K. (2012). Breastfeeding predicts handedness. Laterality: Asymmetries of Body, Brain and Cognition, 17(3), 361–368. doi: 10.1080/1357650X.2011.579131
- Deoni, S. C., Dean3rd.D. C., Piryatinsky, I., O’Muircheartaigh, J., Waskiewicz, N., Lehman, K., … Dirks, H. (2013). Breastfeeding and early white matter development: A cross-sectional study. Neuroimage, 82, 77–86. doi: 10.1016/j.neuroimage.2013.05.090
- Department of Health-Ireland. (2010). Growing up in Ireland: National longitudinal study of children. The Infants and their families - infant cohortother relevant documents [Online]. http://www.thehealthwell.info/node/773789
- Frankel, M., McWilliams, H., & Spencer, B. (1983). NLSY79 Technical sampling report. Retrieved from https://www.nlsinfo.org/sites/nlsinfo.org/files/attachments/130212/NLSY79%20Tech%20Samp%20Rpt.pdf
- Girard, L. C., Doyle, O., & Tremblay, R. E. (2017). Breastfeeding, cognitive and noncognitive development in early childhood: A population study. Pediatrics, 139(4), e20161848. doi: 10.1542/peds.2016-1848
- Greenland, S., & Drescher, K. (1993). Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics, 49(3), 865–872. doi: 10.2307/2532206
- Hepper, P. G. (2013). The developmental origins of laterality: Fetal handedness. Developmental Psychobiology, 55(6), 588–595. doi: 10.1002/dev.21119
- Hertzmark, E., & Spiegelman, D. (2012). The SAS METAANAL Macro. Retrieved from https://cdn1.sph.harvard.edu/wp-content/uploads/sites/271/2012/09/metaanal_user_manual_-_5-24-2012.pdf
- Isaacs, E. B., Fischl, B. R., Quinn, B. T., Chong, W. K., Gadian, D. G., & Lucas, A. (2010). Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatric Research, 67(4), 357–362. doi: 10.1203/PDR.0b013e3181d026da
- Jayachandran, S., & Kuziemko, I. (2011). Why do mothers breastfeed girls less than boys? Evidence and implications for child health in India. The Quarterly Journal of Economics, 126(3), 1485–1538. doi: 10.1093/qje/qjr029
- Johnston, D. W., Nicholls, M. E., Shah, M., & Shields, M. A. (2009). Nature’s experiment? Handedness and early childhood development. Demography, 46(2), 281–301. doi: 10.1353/dem.0.0053
- Johnston, D. W., Nicholls, M. E., Shah, M., & Shields, M. A. (2013). Handedness, health and cognitive development: Evidence from children in the National Longitudinal Survey of Youth. Journal of the Royal Statistical Society: Series A (Statistics in Society), 176, 841–860. doi: 10.1111/j.1467-985X.2012.01074.x
- Kocaoglu, C., Akin, F., Caksen, H., Boke, S. B., Arslan, S., & Aygun, S. (2014). Cerebral atrophy in a vitamin B12-deficient infant of a vegetarian mother. Journal of Health, Population, and Nutrition, 32(2), 367–371.
- Kramer, M. S., Aboud, F., Mironova, E., Vanilovich, I., Platt, R. W., Matush, L., … Promotion of Breastfeeding Intervention Trial Study, G. (2008). Breastfeeding and child cognitive development: New evidence from a large randomized trial. Archives of General Psychiatry, 65(5), 578–584. doi: 10.1001/archpsyc.65.5.578
- Mackinnon, D. P., Warsi, G., & Dwyer, J. H. (1995). A simulation study of mediated effect measures. Multivariate Behavioral Research, 30(1), 41–62. doi: 10.1207/s15327906mbr3001_3
- Petersen, M. R., & Deddens, J. A. (2008). A comparison of two methods for estimating prevalence ratios. BMC Medical Research Methodology, 8, 9. doi: 10.1186/1471-2288-8-9
- Ragnedda, G., Leoni, S., Parpinel, M., Casetta, I., Riise, T., Myhr, K. M., … Pugliatti, M. (2015). Reduced duration of breastfeeding is associated with a higher risk of multiple sclerosis in both Italian and Norwegian adult males: The EnvIMS study. Journal of Neurology, 262(5), 1271–1277. doi: 10.1007/s00415-015-7704-9
- Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. New York: Wiley.
- Sackett, D. L. (2002). The arrogance of preventive medicine. Canadian Medical Association Journal, 167(4), 363–364.
- Springer, S. P., & Searleman, A. (1980). Left-handedness in twins: Implications for the mechanism underlying cerebral asymmetry of function. In J. Herron (Ed.), Neuropsychology of left-handedness. Perspectives in neurolinguistics and psycholinguistics (pp. 139–156). New York: Academic Press.
- Tao, T. (2014). When is correlation transitive? Retrieved from https://terrytao.wordpress.com/2014/06/05/when-is-correlation-transitive/
- Tomblin, J. B., Smith, E., & Zhang, X. (1997). Epidemiology of specific language impairment: Prenatal and perinatal risk factors. Journal of Communication Disorders, 30(4), 325–344. quiz 343-324. doi: 10.1016/S0021-9924(97)00015-4
- United States Department of Health and Human Services. (1985). National Health Examination Survey, cycle II, 1963-1965 Ages 6-11 Years. doi:10.3886/ICPSR09551.v1
- University of London, I. o. E., Centre for Longitudinal Studies. (2014). National child development study: childhood data, Sweeps 0-3, 1958-1974. [data collection]. 3rd Edition. National Birthday Trust Fund, National Children’s Bureau, [original data producer(s)]. UK Data Service. SN: 5565. doi: 10.5255/UKDA-SN-5565-2
- Valeri, L., & Vanderweele, T. J. (2013). Mediation analysis allowing for exposure-mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods, 18(2), 137–150. doi: 10.1037/a0031034
- Victora, C. G., Horta, B. L., Loret de Mola, C., Quevedo, L., Pinheiro, R. T., Gigante, D. P., … Barros, F. C. (2015). Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: A prospective birth cohort study from Brazil. The Lancet Global Health, 3(4), e199–e205. doi: 10.1016/S2214-109X(15)70002-1
- Wells, G., Shea, B., O’Connell, D., Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2000). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Retrieved from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Yang, S., Martin, R. M., Oken, E., Hameza, M., Doniger, G., Amit, S., … Kramer, M. S. (2018). Breastfeeding during infancy and neurocognitive function in adolescence: 16-year follow-up of the PROBIT cluster-randomized trial. PLOS Medicine, 15(4), e1002554. doi: 10.1371/journal.pmed.1002554
- Yusuf, S., Wittes, J., Probstfield, J., & Tyroler, H. A. (1991). Analysis and interpretation of treatment effects in subgroups of patients in randomized clinical trials. The Journal of the American Medical Association, 266(1), 93–98. doi: 10.1001/jama.1991.03470010097038
- Zeger, S. L., & Liang, K. Y. (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42(1), 121–130. doi: 10.2307/2531248