Abstract
Objectives: People with dementia are more likely to fall and less likely to recover well after a fall than cognitively intact older people. Little is known about how best to deliver services to this patient group. This paper explores the importance of compensating for cognitive impairment when working with people with dementia.
Methods: Qualitative methods – interviews, focus groups and observation – were used to explore the views and experiences of people with dementia, family carers and professionals providing services to people with dementia following an injurious fall. A thematic, iterative analysis was undertaken in which emerging themes were identified from each individual dataset, prior to an integrative analysis.
Results: A key theme across all datasets was the need to deliver services in ways that compensate for cognitive impairment, such as negotiating meaningful activities that can be embedded into the routines of people with dementia. Professionals varied in their ability to adapt their practice to meet the needs of people with dementia. Negative attitudes towards dementia, a lack of knowledge and understanding of dementia limited the ability of some professionals to work in person-centred ways.
Conclusion: Improving outcomes for people with dementia following a fall requires the principles of person-centred care to be enacted by professionals with a generic role, as well as specialist staff. This requires additional training and support by specialist staff to address the wide variability in current practice.
Introduction
There are currently estimated to be 850,000 people living with dementia in the UK (Prince et al., Citation2014), 70% of whom live in the community. Falls are common in people with dementia, with those living in their own home having nearly ten times as many falls as other older people (Allan, Ballard, Rowan, & Kenny, Citation2009). While not all such falls result in injury, falls can lead to a loss of confidence which in turn can result in activity avoidance, loss of conditioning and increased risk of further falls (Delbaere, Close, Brodaty, Sachdev, & Lord, Citation2010; Jefferis et al., Citation2014). Where injuries are sustained, people with dementia are less likely to recover well than cognitively intact older people (Shaw, Citation2002).
Despite the scale of the problem and associated costs for health and social care, few trials have specifically addressed the management of fall-related injuries in people with dementia. Available studies have tended to focus on fractures (Cross et al., Citation2017; Huusko, Karppi, Avikainen, Kautiainen, & Sulkava, Citation2000; Kennie, Reid, Richardson, Kiamari, & Kelt, Citation1988; McGilton et al., Citation2013; Stenvall, Berggren, Lundström, Gustafson, & Olofsson, Citation2012; Watne et al., Citation2014) or on people with dementia presenting to the emergency department (Shaw et al., Citation2003), thus including only those with more serious injuries. The limited evidence base suggests that rehabilitation can be effective in improving physical functioning in people with cognitive impairment following hospital admission (Muir-Hunter, Fat, Mackenzie, Wells, & Montero-Odasso, Citation2016; Vassallo, Poynter, Kwan, Sharma, & Allen, Citation2016). It also suggests that exercise can reduce the risk of future falls for people with cognitive impairment (Burton et al., Citation2015).
Characteristic features of dementia such as spatial disorientation, attention and memory impairment, gait impairment and postural instability, poor judgment and reduced capacity to acknowledge and avoid hazards contribute to the increased risk of falls (Aliberti, Kikuchi, Magaldi, Paschoal, & Filho, Citation2007). Successful interventions for people with dementia in acute settings have incorporated dementia-friendly environments (Waller & Masterson, Citation2015) and staff education around these specific needs (Elvish et al., Citation2014; Moyle, Olorenshaw, Wallis, & Borbasi, Citation2008). However, the latter have been most effective when staff receive support from more experienced colleagues to understand the experiences of people with dementia (Handley, Bunn, & Goodman, Citation2017). Similarly, while the principles of person-centred care have long been established in occupational therapy and physiotherapy (Bright, Boland, Rutherford, Kayes, & McPherson, Citation2012; Gzil et al., Citation2007; Mudge, Stretton, & Kayes, Citation2014), staff may nevertheless find working with people with dementia challenging, particularly those whose communication skills are impaired or who are perceived as ‘disengaged’ or ‘non-compliant’ (Bright, Kayes, Worrall, & McPherson, Citation2015). This reflects a lack of specific training in dementia (Gill et al., Citation2017; Isbel & Jamieson, Citation2016), and may result in inexperienced therapists ‘writing off’ people with dementia (Hall, Watkins, Lang, Endacott, & Goodwin, Citation2017). A focus on biomedical (rather than more holistic) assessments and targets, as well as a lack of space, equipment and time all contribute to negative attitudes towards people with dementia and therapeutic nihilism among staff (Hall, et al., Citation2017; Staples & Killian, Citation2012).
This paper presents initial findings from a project whose overall aim is to develop a new intervention for people with dementia who sustain fall-related injuries. To inform the intervention, we aimed to understand existing service provision and to explore the views of a range of stakeholders on both current services and the content and delivery of a new intervention.
Methods
We used interviews and focus groups to explore the views and experiences of people with dementia who had experienced a fall, family carers and health and social care professionals. We supplemented these data with direct observation of care to help us understand the realities of delivering services to people with dementia following a fall.
Recruitment
Three contrasting research sites participated in this study. Newcastle upon Tyne has a city-based teaching hospital and high dementia diagnosis rates in local primary care (55%). Hartlepool and Stockton-on-Tees cover urban and rural areas with a district general hospital and high dementia diagnosis rate (54%). Norwich has a city-based teaching hospital and covers a largely rural area, with a low diagnosis rate of dementia (41%).
Professionals were identified through snowball sampling with a focus on recruiting staff from a diverse range of services and professional backgrounds. Services were initially identified through consultation with the study principal investigators at each site. Recruitment continued until data saturation was reached.
Patients and carers were recruited either through a prospective diary study (which collected data on service use by people with dementia following an injurious fall) or during observation. Patients and carers were invited to take part in a qualitative interview if they lived in their own home and had capacity to consent for themselves. Those who expressed interest were provided with a Participant Information Sheet and then followed up by telephone. A home visit was arranged and informed consent sought prior to the interview.
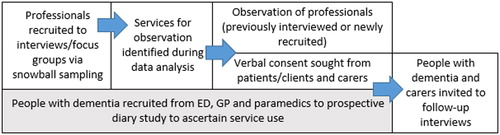
The interviews and focus groups with professionals were used to identify a diverse range of services across the three sites for observation. Observation was initially negotiated with professionals. Patients seen in clinic or at group exercise sessions were provided with an information sheet on arrival. Patients due to be seen at a home appointment were provided with an information sheet prior to the visit. Professionals then checked their willingness to be observed, either when confirming the appointment time or on the day of the visit. Patients who received unplanned visits (i.e. from paramedics or telecare services) were given information at the time of the visit, if deemed appropriate by the professional. Verbal consent from all patients and carers was sought prior to any observation. illustrates the study process; data from shaded stage are not included in this paper.
Data collection
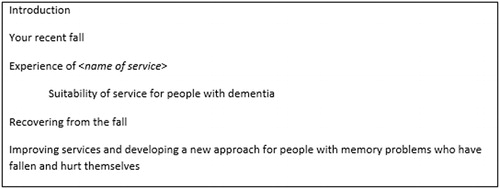
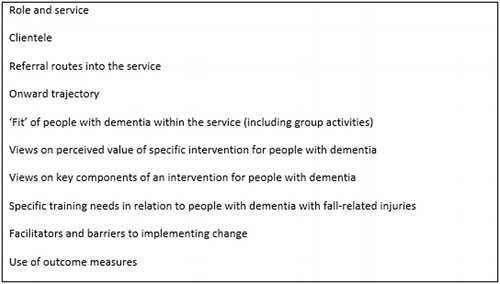
Interviews and focus groups were semi-structured with the aid of topic guides ( and ). Most professionals were interviewed by telephone (CB, MB, AW). A range of staff from some services participated in a face-to-face focus group instead (CB, MB). Interviews with patients and carers were conducted face-to-face, individually or jointly according to participant preference (CS, AW). Interviews lasted between 20 and 60 minutes and focus groups between 40 and 65 minutes.
Observations usually lasted for a single shift or clinic session (CB, CS, AW). We recorded anonymised details of the injuries sustained and the characteristics of the patient (e.g. age and gender). Where patients saw multiple professionals (e.g. in the ED), we recorded the sequence of events with approximate timings. Based on the findings from the interviews with professionals, we specifically paid attention to environmental issues such as distractions; interaction and communication between staff, patients and families; and whether and how any intervention was contextualised, embedded and made relevant to patients’ lives. Detailed ethnographic fieldnotes were recorded during and after each period of observation (Hammersley & Atkinson, Citation2007), including researchers’ reflections on ideas for intervention.
Data management and analysis
Interviews and focus groups were audio recorded. Analysis of professional interviews was conducted in stages; recordings were summarised onto a structured proforma by a team member (MB, AW) for initial analysis, followed by transcription of specific recordings in full for detailed analysis. All focus groups and interviews with patients and carers were transcribed. Transcripts were checked and anonymised by a team member (AW, CS) prior to analysis. Fieldnotes provided the data from observation.
An inductive thematic approach to analysis was adopted (Braun and Clarke Citation2006). Each dataset (interviews and focus groups with professionals; interviews with patients and carers; observation) was analysed separately to avoid assuming that themes from one dataset were necessarily relevant to another. Initially individual researchers read and reread one or two transcripts in detail to become familiar with the data, noting areas of interest and potential codes independently (CB, MB, CS, AW). We then compared ideas in data workshops and developed coding frames. These were applied to further transcripts and discussed collectively in a further data workshop.
We mapped themes across datasets to identify areas of consistency and discrepancy and create an integrated coding frame. This was applied to each dataset with the aid of QSR NVivo 11 by a team member (AW, CS). Output relating to each theme and subtheme was then reviewed and a narrative summary produced independently (CB, AW). This was thought to be a more effective way of scrutinising codes than simply checking coding or having two researchers code the data. The narratives were then compared and discussed to produce a combined narrative incorporating the insights and perspectives of different researchers.
Quotations and field note extracts presented in the findings are identified in this paper by a unique participant ID. Additionally, role and service type is provided for professionals. In extracts from joint interviews and focus groups, the speaker is highlighted in bold. All identifying information, including location, has been removed to maintain confidentiality.
Research governance
Ethical review was provided by Newcastle University for the initial interviews and focus groups with professionals. Approval for observation and interviews with patients and carers was given by Newcastle and North Tyneside 1 Ethics Committee (reference 15/NE/0397); Newcastle and North Tyneside 2 Ethics Committee (reference 16/NE/0011, prospective diary study); and the Health Research Authority. Additional approvals for all aspects of the study were sought from participating NHS Trusts and Social Services Departments as required. For non-statutory agencies, approval was sought from senior managers.
Results
Participants
In total, 112 professionals were approached for interview; of these, 53 were interviewed and a further 28 took part in focus groups. Participants were staff from a range of NHS services, social services and third-sector organisations ().
Table 1. Professionals participating in interviews or focus groups
Thirteen patients or patient-carer dyads were approached for interview following observation and eleven following the diary study, leading to interviews with four patients and nine carers. We observed 20 professionals delivering care or instruction to a total of 85 patients/clients ().
Table 2. Services observed.
Themes
The key overarching theme emerging from the data related to the ability of professionals to compensate for the cognitive impairment of people with dementia when providing rehabilitation or other services following a fall-related injury. Key skills required to achieve this in practice are described in detail below and include:
An understanding of dementia
Adapting communication style
Negotiating meaningful activities
Embedding activities into daily life
Involving carers to support rehabilitation activities
Understanding of dementia
An essential first step to working effectively with people with dementia was for professionals to have some knowledge and understanding of dementia. A lack of appropriate training could lead to negative staff attitudes and a perception that people with dementia had no potential for rehabilitation:
The problem with some of the people with dementia who are falling is their lack of memory makes them, sort of, untrainable.
(Interview, Prof 33, primary care GP)
And unfortunately the term “not rehabable” is not uncommon, used in relation to patients presenting with cognitive issues, which could be delirium as well as patients with diagnosed or undiagnosed dementia. And is used by all professionals and grades of staff, from consultant geriatricians down.
(Focus group, Prof 79, occupational therapist, mental health trust)
Such negative attitudes appeared to stem from associating dementia with the more severe stages of the illness. Specialist mental health workers additionally highlighted the tendency of some professionals to attribute all problems to dementia, without fully exploring other potential contributory factors:
As soon as you’ve got that label of dementia, you’re a totally non-person, you’re a non-patient. Everything is so much ‘Oh, they don’t need a scan for that, they don’t need a check for that because they’ve got dementia’. Well why not? Even something like podiatry and things like that everything can be so much harder, because perhaps the first time they go down, they don’t want anybody touching their feet, because they’re frightened of it. But they can’t walk because their toe nails are so long.
(Focus group, Prof 78, nurse specialist and clinical lead, elderly person's ward at mental health trust)
The extent to which staff understanding of dementia was perceived as problematic varied between different stakeholders. People with dementia and their families were often grateful for any help received, and appeared either to be unaware of gaps in staff understanding of dementia or reluctant to criticise staff. While professionals with a generic role rarely explicitly discussed their knowledge of dementia, we observed multiple occasions on which they struggled to successfully adapt their approach, such as when communicating instructions or assessing pain. This could leave people with dementia marginalised. Furthermore, staff with access to a local specialist for advice and co-working, clearly valued this support, suggesting that they did not always feel well equipped to work with people with dementia:
If you’re in the community and you had a very particular patient who was having unexplained falls or problematic falls, and they had dementia, then you can contact [local dementia & falls co-ordinator], and she will come out with the expert advice.
(Interview, Prof 64, physiotherapist, ED)
Adapting communication style
Being able to communicate effectively with people with dementia required staff to adapt their usual style of communication. Some professionals described the importance of taking time to establish rapport since people with dementia could be wary about staff intentions (for example, suspecting that their intention was to move them into long term care) and therefore unwilling to acknowledge their difficulties.
Pacing communication appropriately with people with dementia allows them sufficient time to first take in and process the information and then formulate a response. We observed several occasions on which patients were outpaced and unable to keep up when a series of questions were asked in rapid succession. This could lead to misunderstandings and lack of compliance:
[Prof 111, physiotherapist] then does some tests on the arm that is damaged from the stroke, including range of movement, grip etc. There’s bit of a misunderstanding about pain at this point. She asks the patient to “Let me know if it’s sore”, but I’m not sure he quite understands. She just says it and then goes straight in, without really giving him time to process it. It seems pretty clear that he is in pain from it, to the point where his granddaughter says, “Oh, granddad, say if it hurts”. Then [Prof 111] stops and rephrases the statement about the pain, and after that he is quite good about saying where the pain is.
(Fieldnotes from observation of domiciliary therapy 20160714)
This quotation also highlights the issue of pain recognition. Staff with a specialist dementia role emphasised the importance of attending to non-verbal communication and cues to facilitate the recognition of pain. However, despite the difficulties of assessing pain in people with dementia, only two participants described using a formal pain assessment tool designed for this patient group; both were paramedics who had researched tools on their own initiative.
We observed only one instance where a patient explicitly asked to go back to an earlier question in response to being outpaced. More typically, patients became passive and disengaged, so that staff rarely received direct feedback on the pace of their communication. Where professionals experienced difficulties with communication, they did not always seem to explore different strategies or try to adapt their communication style:
Sometimes a challenge that I find is that the physio or the OT will get back to me, saying, “Oh well, I don’t think that person’s understanding the exercises, or they’re not understanding my advice.” So, I think that there’s a definite need to really peel back the layers of how we communicate, and what the patient’s priority is. (…) That’s my goal, is to make sure that everyone becomes really aware of different ways to communicate, and finding what works for that person.
(Interview, Prof 35, occupational therapist, dementia & falls services co-ordinator)
Generic staff often relied heavily on verbal communication and did not always seem to recognise when patients were struggling to follow conversations, taking a lack of objection for agreement. While some generic staff used positive communication strategies (such as demonstrating equipment on themselves to allay patient anxieties), specialist staff tended to have a greater understanding of how to adapt their communication style to avoid overloading people with dementia with information. Some physiotherapists emphasised observation when introducing new equipment, rather than a strict adherence to ‘correct’ usage:
In terms of walking aids, I tend not to give a lot of instruction either. I would only give them the frame or the stick and see what they do with it. So try not to over-complicate it. Because they will go, “I’ve got a walking stick, how do I use it?” And I say, “Well you show me how you use it.” […] Because if you try to change someone’s gait or their dominant hand or whatever then that’s when everything becomes confusing.
(Focus group, Prof 77, physiotherapist, community mental health team and specialist dementia unit)
Some specialist staff recommended ‘walking through’ recent falls and ‘near misses’ rather than simply asking the patient about them. Being in close proximity to the site of recent falls could facilitate recall and allow the professional to understand the combination of factors contributing to the fall.
Negotiating a meaningful programme of activities
Since people with dementia could have difficulty in retaining abstract and unfamiliar exercises, making rehabilitation understandable and appealing to the individual was seen as essential by many professionals. This could be achieved by tailoring programmes to the individual’s goals and activities that they enjoy or have previously enjoyed. The following extract illustrates how linking activities to the patient’s interests proved successful in engaging him:
Then [Prof 51, physiotherapist] says “I wanted to test you, [name]”. She gets a large ball from the cupboard, about the size of a beach ball. The patient becomes very animated, much more engaged than he has been. He says “Oh, football.” […] They stand in the middle of the gym and do some bouncing and catching of the ball, and then throwing and catching. […] She then fetches cones and a plastic football from the cupboard, which the patient greets enthusiastically “That’s the way forward!”
(Fieldnotes from observation at day hospital 20160504)
Patients themselves also emphasised the importance of the intervention being fun and enjoyable:
You pick the things out that you would like to do. I think this is always part of the exercises. […] If you enjoy something and you think it’s doing you good then you concentrate more.
(Interview, Patient 8 and Carer 8)
Linking exercises to familiar movements was used to help people with dementia grasp new exercises:
We try and link the movement to activities that they’ll recognise – so say one of the planned exercises you have to sit back and your hand position – we’ll say it’s like pushing a wheelbarrow, so you push your arms forward and back […] I think it is good to link it to something that they know how to do anyway.
(Interview, Prof 23, exercise class instructor)
Not all professionals seemed to recognise the importance of finding ways of making rehabilitation meaningful for patients. When people with dementia were not engaged or compliant, these professionals sometimes were perceived as simply giving up:
Carer 9a: I mean, she did have a physio, but he sacked himself.
Carer 9b: He gave up.
Interviewer: Did he?
Carer 9a: Yes. Well, he just said, “Obviously, [Patient 9], you’re not doing”- he could tell that she wasn’t doing anything. He asked me, and I said, “No, she doesn’t do any.” She just said to me, “Oh, I can’t be bothered.”
Interviewer: She wasn’t doing the exercises herself.
Carer 9b: No.
Carer 9a: No. He said, “It’s pointless me coming.”
(Interview, Carer 9a and Carer 9b)
This underlines the importance of staff creativity and resourcefulness in treating people with dementia.
Embedding activities into daily life
Since many components of interventions need to be repeated regularly, finding ways of embedding them into daily life was seen as crucial, particularly for people with dementia who might otherwise not remember to practice activities. ‘Embedding’ refers to ways of designing interventions in order to make them less intrusive and more likely to become habitual. Elements of physiotherapy could be worked into existing routines:
There is quite a bit of evidence now if you incorporate your strength and balance exercises into your routines it can be as effective. For me that is where we need to work on with the dementia patients. If you can put it into their habits so it becomes habitual then you perhaps don’t need to be going to a programme that you have to do specific things at specific times.
(Interview, Prof 10, senior occupational therapist)
Building on the existing strategies of a person with dementia could similarly help to develop personalised, tailored methods of embedding:
Sometimes you get people who've got cognitive impairment, who write things down, and that's helpful to them. Now, for one person that might be great if you want to write down a sign that says, 'Use your Zimmer frame.' But for other people, that would just really increase their anxiety. If they're, say, having problems with reading […] that might be worse for them. But for some people, if they're using that strategy, and you notice that, then that can be something that you can pull into their care plan.
(Focus group, Prof 71-73, specialist in-patient rehabilitation)
While professionals sometimes simply provided written copies of exercise sheets, they questioned the value of this approach to embedding exercises without the contextualisation of daily routines and activities.
Involving carers in supporting rehabilitation
A common strategy used to compensate for the cognitive impairment of people with dementia was to try to engage other people in rehabilitation activities. A cascade model was identified as a useful way of embedding interventions. Relevant exercises would be identified by a physiotherapist or occupational therapist, but would then be integrated into daily visits by a support worker or into daily routines by a family member. This approach could prove successful, particularly if the person with dementia was reluctant to work with professionals:
I worked with somebody who had really, really bad dementia and who’d had lots of falls, and we thought he wouldn’t work with a therapist because they were scary. He didn’t understand what we were offering, so we taught his daughter all of his exercises and did all the risk assessments and that with her. Then, she did them with Dad and we just reviewed once a week, and he did really, really well.
(Interview, Prof 08, occupational therapist, manager, specialist inpatient rehabilitation)
However, carers dealing with high levels of stress, health problems, and other commitments such as work or other caring responsibilities, did not necessarily have the capacity to support rehabilitation. Despite the potential key role of family carers, our observations indicated that attention to the assessment of carer needs or signposting to other services who could provide this service was rare. Professionals sometimes talked disparagingly about family members who were not perceived to support interventions adequately:
They think, “Oh great, I can go and do the jobs that I need to do.” It gives them a little bit of time to do that, so they don’t want to be in part of the session and they don’t want to help out, which makes it quite difficult for me to go and do a good quality session.
(Interview, Prof 23, exercise class instructor)
This suggested that some professionals held unrealistic expectations of the ability of family members to engage with interventions and lacked understanding of the potential impacts of caring for a person with dementia.
A specific area where carers were sometimes thought to need education or support related to risk management. Some carers were perceived as undermining rehabilitation efforts by encouraging the person with dementia to do very little in an attempt to reduce the risk of further falls. Several participants emphasised the importance of educating carers about positive risk taking:
What I’ve tended to find is they’ve just wanted to wrap their loved one in cotton wool, tell them to sit down and not to move. So, a lot of it is that kind of mind-set work with the carers, to say, “I know that you’re doing this for the right reasons, but actually, get them up to make the cup of tea. Get them into the shower to do as much, as safely, as possible.” It’s really coaching them around how best to actively support that person, rather than just taking over.
(Interview, Prof 35, dementia & falls services co-ordinator)
While carers themselves did not discuss tensions regarding risk management, some commented on a lack of briefing or training on the use of equipment or aids. This could potentially pose a risk or result in reliance on equipment that was no longer appropriate:
Dad’s got a pressure pad under his chair there and a pressure pad under his bed but he no longer has pressure sores. We’re still using them but does he actually need them anymore? I don’t know.
(Interview, patient 8 and carer 8)
Discussion
Our findings highlight the range of skills professionals require when working with people with dementia with a fall-related injury. To compensate for the challenges of cognitive impairment, a more creative approach to communication, developing sustainable activity programmes, and engaging carers with rehabilitation is needed. There is a need for further training and support to ensure that professionals have the capability as well as the institutional support to engage in such approaches.
Despite unprecedented attention to dementia in the UK through the Prime Minister’s Challenge on Dementia (Department of Health, Citation2015) and the National Dementia Strategy (Department of Health, Citation2009), there was still considerable evidence of negative attitudes towards, and a lack of understanding of, dementia among professionals who were not specifically trained in dementia. As with previous studies of hip fracture in dementia, the majority of the professional participants had not received any formal training in dementia care (Gill, et al., Citation2017; Isbel & Jamieson, Citation2016; Patel et al., Citation2016). Our findings demonstrate the diversity of staff knowledge and skills regarding working with people with dementia. We found evidence of negative attitudes towards people with dementia and therapeutic nihilism among some staff, in line with findings of previous studies specific to physiotherapists treating people with dementia (Hall, et al., Citation2017; Staples & Killian, Citation2012). The observation in particular highlighted the continuing need for staff training in dementia, in terms of both knowledge of the disease and practical skills in how to communicate with and tailor an intervention to the specific circumstances of individual people with dementia.
There are a number of reasons why people with dementia may be unable to comply with interventions following a fall: confusion caused by dementia is one reason, but pain or exhaustion could also contribute (Bellelli, Frisoni, Pagani, Magnifico, & Trabucchi, Citation2007). Staff who were experienced at working with people with dementia were able to recognise this and employ strategies to help people with dementia gain the most from reablement and therapy. Inexperienced staff, however, may perceive such patients as disengaged and unable to participate in rehabilitation (Bright, et al., Citation2015; Hall, et al., Citation2017), rather than attempting to find a creative solution. Flexibility is required from staff in delivering services to people with dementia and finding personalised solutions to problems. It is important that these be tailored, as suggested approaches, such as ‘walking through’ falls and near misses, may not be possible or suitable in all circumstances. Expertise in engaging people with dementia should be applied to situations across the trajectory of care, in order to produce the kind of consistency and continuity of support that is important to people with dementia and their carers (Hynes et al., Citation2016).
Studies of interventions with people with dementia in care homes have been successful in engaging participants using person-centred care strategies, such as timing approaches to the individual, making use of reminiscence (Fjellman-Wiklund, Nordin, Skelton, & Lundin-Olsson, Citation2016; Galik, Resnick, & Pretzer-Aboff, Citation2009), or planning meaningful activities based on ‘values and beliefs related to their past roles, interests and routines’ (Harmer & Orrell, Citation2008, p. 552). However, the extent to which this expertise has been transferred to other settings is unclear. Only some services in our study were ‘dementia-friendly’ in their ethos and provided support for staff in engaging in person-centred care. Professionals with the expertise and experience to successfully engage people with dementia in rehabilitation, who also reported feeling empowered to do so, often worked in Mental Health Trusts rather than the acute healthcare services to which people with dementia who have fallen are likely to be referred. This suggests that improving care for people with dementia following a fall requires the support of system-level changes in service organisation, as well as training for individual staff. Additionally, access to specialist dementia expertise needs to be improved for non-specialist staff, perhaps through skill sharing programmes or the implementation of specific ‘dementia advisor’ roles. This is in line with findings from hospital settings, where the presence of such trained advisors has been shown to increase staff confidence and skill in caring for people with dementia (Handley, et al., Citation2017; Spencer, Foster, Whittamore, Goldberg, & Harwood, Citation2014).
Strengths and limitations
The use of observation alongside interviews and focus groups provided detailed insights into day to day practice in working with people with dementia and highlighted variability in practice. A further strength of the study relates to the diversity of professionals who participated: we were successful in recruiting staff working in health, social care and third sector organisations; those with generic and specialist roles; those involved with people with dementia at different points in the falls trajectory (i.e. first response services, such as paramedics, ED, telecare through to exercise classes which are typically focused on longer term input to maintain strength and reduce the likelihood of further falls).
Although concerns have been raised about whether practitioners alter their practice when being observed, our experience suggested that practitioners did not make noticeable efforts in their interactions with people with dementia when we were present.
We experienced some difficulties in recruiting people with dementia and family carers to participate in interviews; we are therefore not confident that we achieved data saturation in the perspectives of people with dementia and carers. It may be that a short interview at the end of observation may be more acceptable to people with dementia and carers. This would have the benefit of allowing the researchers to explore people with dementia and carer perspectives on particular aspects of a specific interaction. However, the ethical implications of such an approach would also need to be considered.
Conclusion
Successful rehabilitation of people with dementia requires professionals to actively compensate for the challenges of cognitive impairment. However, the extent to which professionals are equipped to do so varies widely. Despite a recent emphasis in the UK on improving dementia awareness among all health care staff, our findings revealed that a wide range of health and social care professionals lacked critical skills needed to care for individuals with dementia following an injurious fall. This suggests a need for dementia-related training and support to ensure that professionals are equipped with the necessary knowledge and skills to work effectively with people with dementia.
Acknowledgements
Additional data collection and analysis was conducted by Miriam Boyles.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aliberti, M. J. R., Kikuchi, E. L., Magaldi, R. M., Paschoal, S. M. P., & Filho, W. J. (2007). Comprehensive geriatric assessment in outpatients elderly with dementia. Dementia & Neuropsychologia, 1(3), 303–310.
- Allan, L. M., Ballard, C. G., Rowan, E. N., & Kenny, R. A. (2009). Incidence and prediction of falls in dementia: A prospective study in older people. PLoS One, 4(5), e5521. doi: 10.1371/journal.pone.0005521
- Bellelli, G., Frisoni, G. B., Pagani, M., Magnifico, F., & Trabucchi, M. (2007). Does cognitive performance affect physical therapy regimen after hip fracture surgery? Aging Clinical and Experimental Research, 19(2), 119–124.
- Braun, V., & V. Clarke. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77–101.
- Bright, F. A., Boland, P., Rutherford, S. J., Kayes, N. M., & McPherson, K. M. (2012). Implementing a client-centred approach in rehabilitation: An autoethnography. Disability and Rehabilitation, 34(12), 997–1004. doi: 10.3109/09638288.2011.629712
- Bright, F. A., Kayes, N. M., Worrall, L., & McPherson, K. M. (2015). A conceptual review of engagement in healthcare and rehabilitation. Disability and Rehabilitation, 37(8), 643–654. doi: 10.3109/09638288.2014.933899
- Burton, E., Cavalheri, V., Adams, R., Browne, C. O., Bovery-Spencer, P., Fenton, A. M., … Hill, K. D. (2015). Effectiveness of exercise programs to reduce falls in older people with dementia living in the community: A systematic review and meta-analysis. Clinical Interventions in Aging, 10, 421–434. doi: 10.2147/CIA.S71691
- Cross, J., Backhouse, T., Hammond, S. P., Poland, F., Penhale, B., Smith, T. O., … Varley, A. (2017). Implementation of the PERFECT-ED intervention designed to enhance recovery for people with hip fracture and cognitive impairment in acute trauma wards. Alzheimer's & Dementia: The Journal of the Alzheimer's Association, 13(7), P1158. doi: 10.1016/j.jalz.2017.06.1693
- Delbaere, K., Close, J. C. T., Brodaty, H., Sachdev, P., & Lord, S. R. (2010). Determinants of disparities between perceived and physiological risk of falling among elderly people: Cohort study. BMJ, 341, c4165–c4165. doi: 10.1136/bmj.c4165
- Department of Health. (2009). Living well with dementia: A national dementia strategy. Retrieved from https://www.gov.uk/government/publications/living-well-with-dementia-a-national-dementia-strategy.
- Department of Health. (2015). Prime Minister’s challenge on dementia 2020. Retrieved from https://www.gov.uk/government/publications/prime-ministers-challenge-on-dementia-2020.
- Elvish, R., Burrow, S., Cawley, R., Harney, K., Graham, P., Pilling, M., … Keady, J. (2014). ‘Getting to know me’: The development and evaluation of a training programme for enhancing skills in the care of people with dementia in general hospital settings. Aging & Mental Health, 18(4), 481–488. doi: 10.1080/13607863.2013.856860
- Fjellman-Wiklund, A., Nordin, E., Skelton, D. A., & Lundin-Olsson, L. (2016). Reach the person behind the dementia–physical therapists' reflections and strategies when composing physical training. PLoS One, 11(12), e0166686. doi: 10.1371/journal.pone.0166686
- Galik, E. M., Resnick, B., & Pretzer-Aboff, I. (2009). ‘Knowing what makes them tick’: Motivating cognitively impaired older adults to participate in restorative care. International Journal Of Nursing Practice, 15(1), 48–55. doi: 10.1111/j.1440-172X.2008.01721.x
- Gill, N., Hammond, S., Cross, J., Smith, T., Lambert, N., & Fox, C. (2017). Optimising care for patients with cognitive impairment and dementia following hip fracture. Zeitschrift Fur Gerontologie Und Geriatrie, 50, 39–43. doi: 10.1007/s00391-017-1224-4
- Gzil, F., Lefeve, C., Cammelli, M., Pachoud, B., Ravaud, J. F., & Leplege, A. (2007). Why is rehabilitation not yet fully person-centred and should it be more person-centred? Disabil Rehabil, 29(20–21), 1616–1624. doi: 10.1080/09638280701618620
- Hall, A. J., Watkins, R., Lang, I. A., Endacott, R., & Goodwin, V. A. (2017). The experiences of physiotherapists treating people with dementia who fracture their hip. BMC Geriatrics, 17(1), 91–91. doi: 10.1186/s12877-017-0474-8
- Hammersley, M., & Atkinson, P. (2007). Ethnography: Principles in practice (3rd ed.). London: Routledge.
- Handley, M., Bunn, F., & Goodman, C. (2017). Dementia-friendly interventions to improve the care of people living with dementia admitted to hospitals: A realist review. BMJ Open, 7(7), e015257.
- Harmer, B. J., & Orrell, M. (2008). What is meaningful activity for people with dementia living in care homes? A comparison of the views of older people with dementia, staff and family carers. Aging & Mental Health, 12(5), 548–558. doi: 10.1080/13607860802343019
- Huusko, T. M., Karppi, P., Avikainen, V., Kautiainen, H., & Sulkava, R. (2000). Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: Subgroup analysis of patients with dementia. BMJ: British Medical Journal, 321(7269), 1107–1111.
- Hynes, S. M., Field, B., Ledgerd, R., Swinson, T., Wenborn, J., di Bona, L., … Orrell, M. (2016). Exploring the need for a new UK occupational therapy intervention for people with dementia and family carers: Community Occupational Therapy in Dementia (COTiD). A focus group study. Aging & Mental Health, 20(7), 762–769. doi: 10.1080/13607863.2015.1037243
- Isbel, S. T., & Jamieson, M. I. (2016). Views from health professionals on accessing rehabilitation for people with dementia following a hip fracture. Dementia (London, England), 16(8), 1020–1031
- Jefferis, B. J., Iliffe, S., Kendrick, D., Kerse, N., Trost, S., Lennon, L. T., … Whincup, P. H. (2014). How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatrics, 14(1), 114. doi: 10.1186/1471-2318-14-114
- Kennie, D. C., Reid, J., Richardson, I. R., Kiamari, A. A., & Kelt, C. (1988). Effectiveness of geriatric rehabilitative care after fractures of the proximal femur in elderly women: A randomised clinical trial. BMJ: British Medical Journal, 297(6656), 1083–1086.
- McGilton, K. S., Davis, A. M., Naglie, G., Mahomed, N., Flannery, J., Jaglal, S., … Stewart, S. (2013). Evaluation of patient-centered rehabilitation model targeting older persons with a hip fracture, including those with cognitive impairment. BMC Geriatrics, 13(1), 136. doi: 10.1186/1471-2318-13-136
- Moyle, W., Olorenshaw, R., Wallis, M., & Borbasi, S. (2008). Best practice for the management of older people with dementia in the acute care setting: A review of the literature. International Journal of Older People Nursing, 3, 121–130.
- Mudge, S., Stretton, C., & Kayes, N. (2014). Are physiotherapists comfortable with person-centred practice? An autoethnographic insight. Disabil Rehabil, 36(6), 457–463. doi: 10.3109/09638288.2013.797515
- Muir-Hunter, S. W., Fat, G. L., Mackenzie, R., Wells, J., & Montero-Odasso, M. (2016). Defining rehabilitation success in older adults with dementia–results from an inpatient geriatric rehabilitation unit. The Journal Of Nutrition, Health & Aging, 20(4), 439–445. doi: 10.1007/s12603-015-0585-x
- Patel, M., Lee, S., Hammond, S., Fox, C., Poland, F., Lambert, N., … Backhouse, T. (2016). Caring for people with hip fracture and cognitive impairments: Qualitative findings from the PERFECTED research programme. Paper presented at the European Geriatric Medicine International Congress, Lisbon, Portugal. http://www.sciencedirect.com/science/article/pii/S1878764916301498
- Prince, M., Knapp, M., Guerchet, M., McCrone, P., Prina, M., Comas-Herrera, A., … Salimkumar, D. (2014). Dementia UK: Second edition–Overview. London: Alzheimer’s Society.
- Shaw, F. E. (2002). Falls in cognitive impairment and dementia. Clinics in Geriatric Medicine, 18(2), 159–173. doi: 10.1016/S0749-0690(02)00003-4
- Shaw, F. E., Bond, J., Richardson, D. A., Dawson, P., Nicholas Steen, I., McKeith, I. G., Kenny, R. A. (2003). Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: Randomised controlled trial. British Medical Journal, 326(7380), 73–75.
- Spencer, K., Foster, P. E. R., Whittamore, K. H., Goldberg, S. E., & Harwood, R. H. (2014). Staff confidence, morale and attitudes in a specialist unit for general hospital patients with dementia and delirium–A qualitative study. International Journal of Geriatric Psychiatry, 29(12), 1315–1317. doi: 10.1002/gps.4178
- Staples, W. H., & Killian, C. B. (2012). Development of an instrument to measure attitudes of physical therapy providers working with people with dementia. American Journal of Alzheimer's Disease And Other Dementias, 27(5), 331–338. doi: 10.1177/1533317512452041
- Stenvall, M., Berggren, M., Lundström, M., Gustafson, Y., & Olofsson, B. (2012). A multidisciplinary intervention program improved the outcome after hip fracture for people with dementia—Subgroup analyses of a randomized controlled trial. Archives of Gerontology and Geriatrics, 54(3), e284–e289. doi: 10.1016/j.archger.2011.08.013
- Vassallo, M., Poynter, L., Kwan, J., Sharma, J. C., & Allen, S. C. (2016). A prospective observational study of outcomes from rehabilitation of elderly patients with moderate to severe cognitive impairment. Clinical Rehabilitation, 30(9), 901–908. doi: 10.1177/0269215515611466
- Waller, S., & Masterson, A. (2015). Designing dementia-friendly hospital environments. Future Hospital Journal, 2(1), 63–68. doi: 10.7861/futurehosp.15.017
- Watne, L. O., Torbergsen, A. C., Conroy, S., Engedal, K., Frihagen, F., Hjorthaug, G. A., … Wyller, T. B. (2014). The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: Randomized controlled trial (Oslo Orthogeriatric Trial). BMC Medicine, 12, 63–63. doi: 10.1186/1741-7015-12-63