Abstract
Background and objectives: People with dementia occupy around one quarter of general hospital beds, with concerns consistently raised about care quality. Improving workforce knowledge, skills and attitudes is a mechanism for addressing this. However little is known about effective ways of training healthcare staff about dementia. This study aimed to understand models of dementia training most likely to lead to improved practice and better care experiences for people with dementia, and to understand barriers and facilitators to implementation.
Method: A collective case study was conducted in three National Health Service Acute Hospital Trusts in England. Multiple data sources were used including interviews with training leads/facilitators, ward managers and staff who had attended training; satisfaction surveys with patients with dementia and/or carers; and observations of care using Dementia Care Mapping.
Results: Interactive face-to-face training designed for general hospital staff was valued. Simulation and experiential learning methods were felt to be beneficial by some staff and stressful and distressing by others. Skilled delivery by an experienced and enthusiastic facilitator was identified as important. Staff identified learning and practice changes made following their training. However, observations revealed not all staff had the knowledge, attitudes and skills needed to deliver good care. Patient and carer satisfaction with care was mixed. A major barrier to training implementation was lack of resources. Supportive managers, organisational culture and strong leadership were key facilitators.
Conclusion: Dementia training can lead to improved care practices. There are a range of key barriers and facilitators to implementation that must be considered.
Introduction
Many people with dementia have comorbidities requiring hospital treatment (Dewing & Dijk, Citation2016). People with dementia occupy 13–63% of general hospital beds internationally (Mukadam & Sampson, Citation2011; Timmons et al., Citation2015). The experience of general hospital care for people is consistently reported to be suboptimal due to a noisy and disorientating environment and poor communication approaches by staff (Royal College of Psychiatrists, Citation2011, Hood, Gandesha, Souza, & Royal College of Psychiatrists, Citation2013, Citation2017). It has been found to include task-focussed (rather than person-focused) care practices, and there is a lack of dementia specific or friendly pathways and services (Royal College of Psychiatrists, Citation2011, Citation2013, Citation2017). Often staff are unaware a patient has dementia and do not have the personal information needed to support good care (Royal College of Psychiatrists Citation2017). Poor quality general hospital care that does not accommodate the person’s dementia-related needs, may result in longer length of stay, reduced quality of life and decreased likelihood of being able to return home (Leung & Todd, Citation2010; Zekry et al., Citation2009). One potential causal factor for this is that general hospital staff are not adequately prepared to meet the potentially complex needs of this group (Chater & Hughes, Citation2013; Cowdell, Citation2010). They may lack skills, experience and knowledge about what good quality care looks like (Innes, Kelly, Scerri, & Abela, Citation2016) and cite a lack of available dementia training (Chater & Hughes, Citation2013).
Two systematic reviews (Scerri, Innes, & Scerri, Citation2017; Surr & Gates, Citation2017) have examined the evidence around dementia training programmes for general hospital staff. Collectively they discuss 17 programmes reported across 21 papers, demonstrating the dearth of published studies in this area. Both note variable study quality, including selection bias due to purposive sampling, small sample sizes, weak statistical analyses and the predominance of nurses within training cohorts. Programme content was varied ranging from medical aspects of dementia such as prevalence and diagnosis, to psychosocial care approaches. The most prevalent model adopted was person-centred care. Delivery methods commonly included a blend of face-to-face didactic content combined with interactive and experiential learning activities, work-based learning, practice placement/visits or use of decision-support tools. In some programmes this was accompanied by e-learning, which often suffered poor uptake due to lack of staff time and poor internet access. The length of programmes ranged from two-hours to 13 days delivered over 18-months. Overall there was a lack of consistency in programme content, delivery methods and depth.
Both reviews utilize Kirkpatrick’s (Citation1979, Citation1984) four level (learner reaction, extent of learning, staff behaviour change, practice results or outcomes) model for evaluation of education and training provision. They found few evaluated outcomes across all levels, with the majority focussing only on staff reactions and learning. Satisfaction levels with the training programmes were generally high and the majority showed significant improvements in learning, largely assessed using knowledge measures or tests. Few studies examined impact on behaviour change and practice outcomes. Where this was undertaken methodological weaknesses, such as reliance on staff self-report, limited the conclusions which could be drawn. There was also limited follow up of change over time. Surr and Gates (Citation2017) identified a range of training features most likely to lead to positive outcomes. They included: (a) delivery via face-to-face group teaching by a skilled facilitator; (b) tailoring training to learners’ role; (c) using direct involvement, through video or written vignettes to present the voice of people with dementia and carers; (d) duration of at least a day, with individual sessions of at least an hour; (e) and providing ongoing support via in-service experts or champions. They concluded that future research should further consider training design and delivery, and evaluate a broader range of outcomes. Scerri et al. (Citation2017) highlight that more high quality research with extended follow up is needed.
In summary, there is a limited body of research evidence on dementia education and training within general hospital settings, although some potential features of good quality training are emerging.
Aims and research questions
The 'What Works?' study (Surr et al., Citation2015) aimed to understand what constitutes an effective approach to education and training for the dementia workforce. It comprised four components: a systematic literature review (see [Surr, Gates et al., Citation2017]); a national audit of dementia training; a knowledge, attitudes and confidence survey of staff who had completed programmes reported in the audit; and multiple case studies (Mills, Durepos, & Wiebe, Citation2010) across a range of health and social care settings (general hospitals n = 3, mental health/community services n = 3, social care n = 3, general practitioner practices n = 1). The aim was to recruit three case study sites from each setting type. This ensured enough data could be collected at each site to provide an in-depth picture (Creswell, Citation2006) within the project resources but was sufficiently large to permit cross-case comparison. This paper reports a collective case study of the general hospital case study sites.
The aim of the case studies was to understand good practice regarding the design, delivery and impact on care practices of dementia education and training within general hospital settings, as well as factors affecting its implementation
Research questions were:
What models of dementia education and training were sites adopting? (Richards & DeVries, Citation2011)
How did staff perceive the training? (Kirkpatrick Citation1979, Citation1984 - Level 1)
How did the training impact on staff knowledge, attitudes and practices? (Kirkpatrick levels 2 and 3)
How did people with dementia and their family members experience care within wards where staff had received training? (Kirkpatrick Level 4)
What were the specific barriers and facilitators to effective training implementation?
Methods
An embedded (Yin, Citation2013), collective (Creswell, Citation2006) case study design was employed. It drew on the theoretical propositions (Yin, Citation2013) of Richards and DeVries’ (Citation2011) Conceptual Model for Dynamic Evaluation of Learning Activities, used to describe and explore the design and facilitation processes of training and Kirkpatrick’s (Citation1979, Citation1984) four-level model for evaluation of training interventions (see above).
Case selection
In this study a case was defined as a single National Health Service (NHS) Trust. Twenty-eight NHS acute/general hospital Trusts in England were considered for inclusion. All had responded to the national audit of content of dementia training and methods of its delivery, conducted as part of the larger study. Using a positive deviance approach (Marsh, Schroeder, Dearden, Sternin, & Sternin, Citation2004) respondents were ranked against good practice criteria identified via the literature review (Surr, Gates et al., Citation2017). These included how comprehensively they covered subject learning outcomes within the benchmark dementia training standards for England (Skills for Health, Health Education England, & Skills for Care, Citation2015), training length and delivery methods. Ranking was undertaken by researchers blinded to site identity. The three top ranking sites were approached to take part. One was unable to participate and so the fourth ranked site was approached and consented. The training lead at each site facilitated the research team’s approach to other participants.
Data collection
Multiple sources of data were collected at each site (see ), consistent with a multiple case study approach (Mills et al., Citation2010). Semi-structured interviews were carried out with the dementia training lead and staff who facilitated delivery of the training (to address research Q1, Q2, Q3, Q5). Individual, small group or focus group interviews (2–6 members) were undertaken with staff who had attended training (Q2, Q3, Q5). Interviews were conducted with ward managers of staff who had undertaken training (Q2, Q3, Q5). All used topic guides and were audio recorded and transcribed verbatim. Interviews lasted 30–60 minutes and focus group discussions around 60-minutes. Focus groups included case scenarios developed by experts with experience of living with, or caring for someone with dementia. In response to the scenarios, participants were asked to identify examples of good and poor practice to explore their knowledge and attitudes towards good dementia care. Training sessions were observed (Q1, Q2). Aspects of their delivery were noted using a qualitative observational framework developed by the researchers based on the Richards and DeVries’ (2011) and Kirkpatrick (Citation1979, Citation1984) models. Copies of the training materials were obtained from each site for analysis (Q1). Satisfaction cards were provided for completion by people with dementia and carers/supporters (Q4). These were developed by the research team, based on the format of the current NHS Friends and Family test (NHS England, Citation2015). They comprised three fixed and one open response question. Respondents were offered the opportunity to also take part in a telephone or face-to-face interview to discuss their care experiences. However, no respondents expressed an interest in taking part in an interview from any of the sites.
Table 1. Characteristics of case study sites.
Care was observed on up to two wards at each hospital (Q3, Q4, Q5) for up to eight hours, covering morning and afternoon periods. Dementia Care Mapping (DCM) (Bradford Dementia Group, Citation2005), a continuous observational tool capturing data on patient experience of care, was used. Every five-minutes the observer records the behaviour of the patient (from 23 possible codes; Behaviour Category Code – BCC) and their relative level of mood and engagement (from a six-point scale (−5, −3, −1, +1, +3, +5: Mood and Engagement Value – ME)). Good (Personal Enhancers) and poor (Personal Detractions) quality staff interactions are recorded when they occur. In keeping with our positive deviance approach, wards were selected by the site training lead as representing areas where a number of staff had attended dementia training and where they believed this had had the greatest impact on care practice. Most data sources contributed multi-level information across the Richards and DeVries and Kirkpatrick levels.
Consent and ethical issues
Ethical approval was given by the Yorkshire and the Humber – Bradford Leeds NHS Research Ethics panel [REC Ref 15/YH/0488]. Once sites were identified key staff (training lead, training facilitators, ward managers) were approached as part of the initial Trust consent process, to ensure they were happy to take part. Formal written informed consent was gained from all study participants. Following processes adopted in previous studies utilising general observations of care in hospital settings (Cowdell, Citation2010; Allen, Citation2000), verbal approval to record anonymised observational data was gained from staff and patients ahead of conducting DCM observations. Where the patient lacked capacity to give informed consent, in line with the Mental Capacity Act (Citation2005), advice was gained from a family member about taking part. Individuals were able to opt out of observations and the researchers assessed for ongoing consent in line with the principles of process consent (Dewing, Citation2007) throughout. Posters containing a photograph of the researcher and details about the study were displayed in prominent positions on the units during observation periods to notify patients not being directly observed, visitors and staff that observation was taking place. Individuals were invited to raise any questions or concerns about the observations with the researcher or a member of staff.
Data analysis
Analysis of each individual data source, for each case study site, was conducted initially. This included thematic analysis of the interview and focus group transcripts and training observations, using the template analysis approach (King, Citation1998; Brooks, McCluskey, Turley, and King, Citation2015) with data management supported by NVivo 11 (QSR Inernational Pty Ltd, Citation2017). A coding template was developed containing some a priori themes underpinned by the frameworks of Richards and DeVries and Kirkpatrick. Additional themes were developed and agreed through collaborative coding (by all authors) of a subset of three initial transcripts and discussion of the identified themes. The template was modified following coding of a further six transcripts (by CS, NB and MD) and assessment of their fit to the template themes. This modified version of the template was used to code the remaining data. Content of the training materials was mapped against the learning outcomes contained within the Dementia Core Skills Education and Training Framework (Skills for Health et al. Citation2015). It was also mapped against the Dementia Training Design and Delivery Audit Tool (DeTDAT) (Surr, Sass, et al., Citation2017) good practice training audit tool, developed by the authors as an outcome of the systematic review (Surr, Gates et al., Citation2017). DCM data was analysed according to standard guidelines, including producing individual and group summaries of behaviours and mood and engagement values. Quantitative and qualitative responses to the patient and carer satisfaction cards were summarised using descriptive statistics and thematic analysis was conducted manually.
Following analysis of each data source for a site, a within case analysis (Creswell, Citation2006) was undertaken. This involved producing summary reports from each data source in NVivo 11 followed by triangulation of the key findings for the site across sources. The data set related to each site was then synthesised into a written ‘story of the case’ (Simons, Citation2009) in a Word document, to gain an understanding of the emergent issues. Cross-case analysis (Creswell, Citation2006) of data across the three sites was then conducted. Data were synthesised using convergence coding (Farmer, Robinson, Elliott, & Eyles, Citation2006). This was achieved by creation of a grid of data themes and findings, permitting comparison of areas of agreement, partial agreement and dissonance (O'Cathain, Murphy, & Nicholl, Citation2010) around training design, delivery, impact and key barriers and facilitators to implementation.
Results
The three recruited NHS Trusts were geographically spread across England and varied in size and approach to training delivery (see ).
The results are presented according to the a priori areas of interest (training design, delivery, staff reaction, impact on learning, practice behaviour change, impact on care outcomes and experiences) and their related findings and themes. They are summarised in .
Table 2. Summary of key findings and themes across case study sites.
Training design
Two primary themes were identified related to training design: training tailored to general hospital staff; and ongoing training development and evaluation. All three sites used training packages specifically for general hospital staff. Two had developed bespoke training, whilst trainers from the third used freely available materials designed specifically for general hospital settings. The trainers at all three sites recognised the need for tailored training.
…it’s really bespoke to the hospital. It’s not a standard package, it has been designed around the hospital’s needs. What’s been happening, topically, that’s been affecting hospitals’ patient care, …. (Trainer AT438 021)
Ongoing evaluation and development of the provision in line with identified training needs and participant feedback was recognised as important, as was trialling and reviewing new materials. However, gaining meaningful feedback was a challenge with often limited opportunities for this beyond that that gathered immediately following a training session.
So, I would hope that it is making some kind of impact. … but I couldn’t say whether it’s having an impact because I just don’t go into the clinical areas after. (Trainer AT044 046)
Training delivery and staff reactions
Three themes were related to training delivery and staff reactions: interactive methods; presenting the experience of people with dementia; and skilled delivery. The delivery methods used were identified as important for learning and staff engagement. Engaging, interactive and memorable training methods, interspersed with frequent discussion and opportunities to ask questions, were favoured over didactic content delivery.
I think practical sessions speak volumes, rather than PowerPoint presentations. Everyone’s always like: ‘It’s death by PowerPoint, isn’t it?’ You sit there and you just think ‘another slide, another slide, another slide’ and you don’t get people to engage with it (Trainer AT044 046)
I think they’ve all found it quite fun because [trainer] makes it really interactive and she gets you up and doing things so I think it is one of the more ‘fun’ study days. I think people have really enjoyed it. (Ward Manager AT438 026)
The use of other interactive or immersive methods such as experiential learning and simulation were identified by some respondents as helpful, in supporting them or others to develop empathy and understanding.
… get a feel and understanding of the various types of dementia and what it’s sort of like to be in the shoes of a person who’s got dementia. (AT044 P01, Focus Group 1)
However, others in the same focus group described the training as emotionally ‘intense’ (P03), ‘frightening’ (P04) and ‘scary’ (P02). When similar methods were used in another site, consideration of participant vulnerability, the potential for causing distress and the possible impact this might have on participants appeared not to have been adequately considered. Learners, unless impacted negatively themselves, also lacked appreciation of this.
… and do you know what’s funny is actually one of the people within my group that I was working with, she got really upset like actually got upset because she felt so frustrated … and she was like “I feel so stupid”. (Ward Manager AT438 022)
Using approaches to present the experiences of people with dementia, for example through video content, or written scenarios was identified as particularly beneficial in helping staff to engage empathically with the experience of people with dementia.
… the videos really highlighted how – you know these patients can just feel really neglected and alone and scared. (Staff Member AT066 012)
Skilled delivery was also identified as an essential component of good training. Training facilitators needed training delivery and clinical skills and to be enthusiastic, to provide a good learning experience.
The facilitators were incredibly knowledgeable, empathic towards both the learners and people with dementia, engaging, and approachable (Training observations AT044)
The person that you want at the front of the class is somebody who is passionate about their subject, … you go away, hopefully, being rubbed off with a bit of that passion too. (Trainer AT438 021)
Where facilitators had clinical but not training expertise this could be a barrier to effective learning
They’re subject specialists in their areas but maybe they don’t have the same presentation skills as somebody who’s doing it day in, day out. (Training Facilitator AT066 011)
Learning
Themes related to learning included: understanding ways to deliver better care and development of empathy. Evidence from a range of sources indicated that staff gained confidence in their ability to support people with dementia by attending training, and acquired knowledge on a variety of topics, including: person-centred approaches, understanding and supporting individual differences and the importance of activity and engagement.
I think we are significantly better in recognising that people with dementia not only do they need their medical needs attending to (Trainer AT044 045)
A powerful area of learning identified across all sites was increased empathy for people living with dementia
A lot of people have said “I’ve come away and I’ve suddenly realised why people knock over their glasses and why people get angry if the door’s closed.” (Ward Manager AT438 026)
Behaviour
Key themes identified in relation to staff behaviour change were: improved understanding, improved communication, and provision of meaningful activity. There was evidence across all three sites that many staff responded sensitively to people with dementia, developed patience, tried to understand behaviours and needs and adopted unrestrictive practices.
For me, it’s about not presuming, it’s looking at the person as a whole, and trying to see, with the patients, when they are quite restless and confused, or very agitated, it’s about trying to, sort of, process through, actually, what is it that they want, what is it they’re looking for. And about trying to be helpful and not restrictive (Staff Member AT066 016)
Many staff and managers also described ways they felt communication approaches had been changed to positive effect.
… now I just approach them as me and talk to them as them. Before, I’d turn away thinking oh not my problem.” (AT044 P4, Focus Group1)
There was also recognition of the need sometimes to ‘be with’ individuals who might be expressing distress as a form of non-verbal communication.
And some people, when they’re frightened, they just need someone to sit there and hold their hand. You don’t have to say anything at all, you can just sit there. I sat there with someone, holding their hand for about 20 minutes on a night shift once. … at that moment in time, they did not want to be on their own. … Didn’t need to talk, just needed someone to hold her hand until she fell asleep. (Staff Member AT438 100)
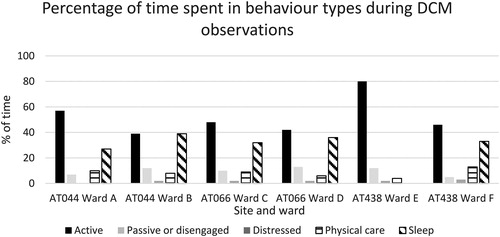
However, the DCM data showed that positive communication was not consistently practised by all staff. In half of the wards more negative than positive interactions were observed (see ) and the average number of positive interactions per patient was less than one per hour of observation.
Figure 1. Average number of personal detractions and enhancers per participant per hour of DCM observations.
Some of the accompanying notes made by the researchers during observations highlighted specific examples where staff did not have the knowledge, skills, attitudes or communication approaches needed to deliver good quality care.
Staff also used physical objects such as blankets to try and keep people in bed or their chair, for example by covering them up again. In one instance the patient was pushed back into the bed when they attempted to get out. These poor interactions resulted in the situation escalating. (DCM observations AT066 Ward C).
On Ward A, the majority (n = 9) of the negative interactions observed occurred during a single, extended incident as a member of staff supported a patient to eat. This incident, caused the patient to become very distressed and demonstrated the impact of even a single staff member not having the right knowledge, skills or approaches.
The need for meaningful activity and occupation was also recognised as important by many staff who had attended training. The interviews and focus groups identified a range of ways in which staff were trying to provide more opportunities for activity.
… there’s examples where staff have got special magazines for patients … and gone through sort of looking through them with them … (Ward Manager AT044 Unit Manager).
… rather than “your bed’s here, stay in bed, stay in bed, sit in the bed” you know, they’ll take them round the hospital in the wheelchair (Ward Manager AT438 034).
Experiences of care
Themes identified in relation to the care experience were: involvement and inclusion, and activity, occupation and well-being. Examples of positive involvement of relatives in the care of the person with dementia were identified by staff at all three sites.
… when we send people for test or they go the theatre we are much more understanding about relatives or a carer can go with the person to try and support them (AT044 Ward Manager).
… so for the family, to be allowed open visiting and things like that as well. So we encourage them to come in and help (Ward Manager AT438 033).
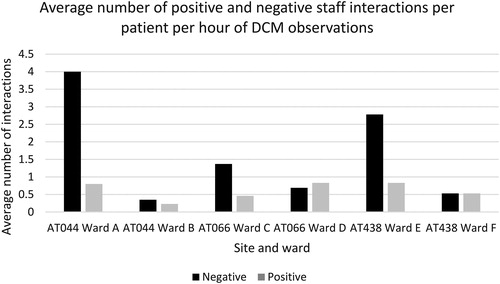
Feedback on the patient and carer satisfaction cards, however, was mixed, with one site (AT044) generally performing well across all questions (see ) and the other sites having more varied responses. Some responses indicated relatives did not always feel involved or included by staff.
Figure 2. Percentage of positive responses (quite/very satisfied) to patient and carer satisfaction survey.
Good care, I have good care. No complaints (Satisfaction Card Respondent AT066).
Very attentive to her/understand. Good care… Explain things well to family… (Satisfaction Card Respondent AT438).
Although staff are really good. There’s not enough staff working on the ward and they are so busy with other things. (Satisfaction Card Respondent AT044).
Staff should be more approachable (Satisfaction Card Respondent AT066).
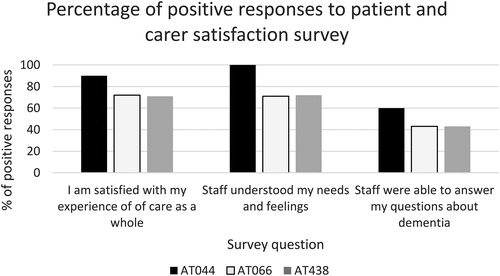
While staff were able to identify changes made to practice that they felt had led to benefits for patients and their family members, this was not necessarily realised in the DCM observations of care practice. They showed variable care across the sites, wards and between different patients with dementia, particularly with regard to activity and occupation. The percentage of time that people with dementia spent in active behaviours (talking to others, eating and drinking, leisure activities, walking) varied considerably between wards from less than 40% up to 80% of the observed period (See ).
With regard to well-being, whilst unattended distress was rare, shows that time spent in negative mood (−1, −3, −5) ranged between 26 and 49% for five of the six wards. This indicates that while those observed may have been actively engaged this was often in a state of distress. Time spent in neutral mood/engagement (+1) ranged from 24 to 57%, with time spent in positive mood and engagement (+3, +5) ranging from 0 to 50%. Therefore, levels of well-being were generally low across all sites and varied considerably across individuals with dementia, indicating a lack of consistency in the experience of care.
Table 3. Profile of participant well-being during DCM observations.
Application of training in practice
Barriers to training implementation
A range of contextual barriers and facilitators that could support or undermine training implementation in practice were identified. These included lack of resources, other staff, and the physical environment.
The biggest challenge across all three sites was lack of resources including time, competing priorities and lack of staff due to shortages caused by unfilled vacancies. Therefore, being able to release staff to attend training was often difficult.
Unfortunately, for Nursing staff, they don’t get protected study leave. So, if there is a demand in the clinical area, their study leave gets cancelled. (Trainer AT044 046).
…it’s a staffing issue. It’s because of my vacancies, …you know you’d like to send 3 people [on training] but you can’t. … the numbers would have an impact because of my vacancy level. (AT066 Unit Manager 019).
Yeh, we’ve had to withdraw staff from training. If the ward is short staffed we have to pull from study days. (Ward Manager AT438 033).
Staff members felt that understaffed wards affected their abilities to perform the most basic of care tasks:
You want to say … do you want a cup of tea but because you’re busy with someone else then you can’t offer because there’s no one around to delegate the task. (AT066 Staff Member 014).
I mean that’s not to do with the dementia training, that’s to do with not having enough staff. (Ward Manager AT438 034).
Having staff working on units who did not have the right knowledge, skills and attitudes caused problems for delivery of good quality care. In particular poor attitudes of agency staff towards people with dementia was identified as a challenge.
… but it’s fair to say that I don’t think a lot of them [agency staff] have had any dementia training. They’re very negative towards dementia. Really don’t know how to handle it. (Ward Manager AT438 034).
Certain staff groups such as doctors could also be difficult to engage with training and thus consistency of approaches was compromised.
One of the biggest barriers for us, and still to this day, is getting Medics interested and … to attend training. (Dementia Lead AT044).
The general hospital ward environment could also be problematic, for example a lack of dementia friendly recreational space could impede activities and occupation.
… it’s a difficult situation, because the ward environment isn’t as practical as it probably needs to be (Staff Member AT066 016).
Facilitators
A number of factors that supported successful training and implementation were identified including management support, organisational culture and leadership for dementia training. Supportive, committed ward managers were extremely important in creating a ward culture that valued training and supported staff to attend sessions and implement learning into practice. Managers also role modelled good practice and provided leadership for good quality care.
Because I’ve been on the Dementia Champions course, I’ve tried to like almost show them how I look after a patient with dementia. (Unit Manager AT066 020).
I really wanted people to do the training so I kept emailing people and telling them the dates and to book on and just reminding them that they’d get the hours back. (Ward Manager AT438 026).
Actually the crux of it is about the leadership on the ward because if staff are encouraged to share that knowledge when they get back to the shop floor you are more likely to see a change in the culture on the ward. (Trainer AT044 045).
It was also important to have a broader Trust culture supporting managers; one which valued dementia training and good quality care for people with dementia. This included creating a critical mass of staff across a range of roles and levels who could champion the training through leading by example.
What we’ve had agreed by the Chief Nurse is that all new nurses to the trust that are in their first year … they have to attend a course… it’s mandatory that they attend. (Trainer AT044 046).
I think sometimes it’s around the senior nurses sometimes leading and guiding staff. (Ward Manager AT044 Unit Manager).
Individual drive and leadership for dementia training and care was also a key contributing factor. At two of the sites the presence of a dementia training lead who had full-time responsibility for leading training across the site, who was assertive and had good leadership skills, was a key facilitator for supporting training attendance and subsequent implementation.
… you’re never off. I’m always thinking about stuff. … you have got to put in that extra time and effort of wanting to go network. People just don’t invite you to things, you’ve got to put yourself on people’s doorsteps; you’ve got to get yourself known, you’ve got to be proactive. (Dementia Lead AT044).
In one site where the lead was not a full-time employee, staff perceptions of the dementia training were more variable and the leadership presence was not as clear. This impacted on the prominence dementia training had and the value that staff placed on training attendance, as well as impeding the potential for flexibility within the site’s training provision.
Discussion
The case studies indicated a range of potential benefits of attending dementia training for general hospital staff. Common to the findings of previous research (Palmer et al., Citation2014; Schindel Martin et al., Citation2016) and systematic reviews (Scerri et al., Citation2017; Surr & Gates, Citation2017), all three sites utilised bespoke training designed for general hospital staff. There were clear indicators about the delivery methods that trained staff, ward managers and trainers felt were most effective. Again, similar to the findings of previous research reported in systematic reviews of the literature (Scerri et al., Citation2017; Surr & Gates, Citation2017), these included face-to-face small group delivery, utilising a blend of knowledge or theoretical content alongside interactive and practical activities, video or scenario-based exercises and experiential learning. Staff did not value teaching dominated by didactic delivery. All the Trusts utilised skilled training facilitators and highlighted the necessity of this expertise for effective training delivery, echoing the findings within the broader health and social care literature for dementia training and education (Surr et al., Citation2017).
Simulation or immersive techniques, while valued by some and found to be highly impactful, were distressing and anxiety provoking for others. Trainers did not appear to have always considered the safety and ethical issues associated with their use. The potential learner vulnerabilities created when using simulation, role play or experiential learning activities is highlighted in health simulation research (Bearman, Palermo, Allen, & Williams, Citation2015; Willhaus, Averette, Gates, Jackson, & Windnagel, Citation2014). The need to plan for adverse events within simulation education is identified by Marshall and McIntosh (Citation2018) who advise they are most likely to be avoided through adequate preparation of learners, the creation of a physically and psychologically safe learning environment and adequate time for debriefing. Given the often restricted time to deliver training in the general hospital setting, the time available for learner preparation and debriefing is likely to be limited, indicating that facilitators should carefully consider whether simulation is suitable, feasible and safe to undertake within the available time.
The largest barrier to implementing training in practice was lack of time and resources. All sites had vacancies, were short-staffed and often reliant on agency workers to cover shifts, who were consistently reported to lack the requisite knowledge, skills and attitudes to deliver good dementia care. This is a common finding among this workforce (Pham et al., Citation2011; Quinlan, Bohle, & Rawlings-Way, Citation2015), suggesting further consideration of and research on the training needs of agency staff is required. Additionally, lack of engagement in training from some staff groups such as medics, meant consistency in knowledge, skills and attitudes was difficult to achieve. All these factors were exacerbated by physical ward environments that were not conducive to good dementia care, which is a well-documented problem (Houghton, Murphy, Brooker, & Casey, Citation2016).
Despite the many challenges there were common facilitators that supported the staff across the case study sites to attend training and to be able to take learning back into practice. They included good leadership and support from ward managers and senior staff, a supportive organisational culture and a designated, proactive, dementia training lead. The importance of good leadership for implementation of evidence-based practice and innovation in healthcare is well known (Aarons, Ehrhart, Farahnak, & Hurlburt, Citation2015; Stetler, Ritchie, Rycroft‐Malone, & Charns, Citation2014), with ‘first-level leaders’ or front-line managers recognized as being particularly influential in this process (Fleiszer, Semenic, Ritchie, Richer, & Denis, Citation2016; Priestland & Hanig, Citation2005). This indicates that hospitals need to pay particular attention to leadership and support for training programmes, alongside design and delivery approaches.
This study is one of the first to examine the components of successful dementia education and training in general hospital settings and their impact across the four Kirkpatrick levels of evaluation. It provides more comprehensive evidence to support suggestions indicated in previous research about successful training in this setting and barriers to and facilitators to it. However, there were a number of limitations. Since staff at each site had already accessed a range of dementia training, it was not possible to collect data on staff knowledge, attitudes, behaviours or patient outcomes prior to any dementia training delivery. While the conducted case studies were in-depth, only three sites were included in the study who were the top performing of audit respondents. Likewise, only a relatively small sample of staff, wards and patients/relatives were included at each site. While they provide an in-depth picture of the impact, barriers and facilitators to training and its implementation in such settings, they are unlikely to be representative of average training practice and impact in general hospitals across England.
Conclusions and recommendations
In all of the case study sites we found evidence that it was possible to introduce and sustain comprehensive programmes of training, in general hospital settings, despite the many challenges identified to this in the existing literature. Hospital staff and managers saw value in training attendance and could identify specific benefits for improved care practices. Where staff lacked the knowledge, attitudes and skills needed to deliver person-centred care, there were observable negative impacts on patient experiences. Despite the success of the training programmes, a range of barriers to delivery and implementation existed, that continually challenged attendance and practice change. Further research is needed to understand more about how the barriers to training and its implementation can be overcome, and to assess the impact of successful training on outcomes for people with dementia and their family members. Based on the findings from this study the following recommendations can be made about training design, delivery and implementation within general hospital settings.
Training should:
Include small group, face-to-face delivery;
Keep didactic aspects to a minimum and maximise creative and interactive exercises;
Be tailored to the general hospital setting;
Ensure the experiences of people with dementia and their family caregivers are presented through direct involvement, video or written scenarios;
Ensure simulation or experiential aspects are only used if there is the time and resources to provide adequate support for staff and that consideration is given to the potential for learner distress;
Be delivered by experienced, enthusiastic facilitators who are also good clinical role models;
Be supported by hospital management;
Be led by a designated dementia training lead who is proactive in leading change;
Consider mechanisms to protect agreed training time and manage this in the context of staffing shortages;
Urgently consider how to ensure that agency or temporary staff know the basics of person-centred dementia care delivery.
Acknowledgements
We would like to thank all of the participating sites and individuals who gave their time freely to take part in this research. We would like to thank co-applicants Dr Andrea Capstick and Alison Dennison who were involved with study design and delivery and whom led the lay advisory input into the study. We would like to thank Andrew Hart for his involvement in data analysis.
Disclosure statement
None of the authors have any conflicts of interest to disclose.
Additional information
Funding
References
- Aarons, G. A., Ehrhart, M. G., Farahnak, L. R., & Hurlburt, M. S. (2015). Leadership and organizational change for implementation (LOCI): A randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implementation Science, 10(1), 11. doi:10.1186/s13012-014-0192-y
- Allen, D. (2000). Negotiating the role of expert carers on an adult hospital ward. Sociology of Health and Illness, 22(2), 149–171. doi:10.1111/1467-9566.00197
- Bearman, M., Palermo, C., Allen, L. M., & Williams, B. (2015). Learning empathy through simulation: A systematic literature review. Simulation in Healthcare, 10(5), 308–319. doi:10.1097/sih.0000000000000113
- Bradford Dementia Group. (2005). DCM 8 User's Manual. Bradford: University of Bradford.
- Brooks, J., McCluskey, S., Turley, E., & King, N. (2015). The utility of template analysis in qualitative psychology research. Qualitative Research in Psychology, 12(2), 202–222. doi:10.1080/14780887.2014.955224
- Chater, K., & Hughes, N. (2013). Strategies to deliver dementia training and education in the acute hospital setting. Journal of Research in Nursing, 18(6), 578–593. doi:10.1177/1744987112446242
- Cowdell, F. (2010). The care of older people with dementia in acute hospitals. International Journal of Older People Nursing, 5(2), 83–92. doi:10.1111/j.1748-3743.2010.00208.x
- Creswell, J. W. (2006). Qualitative inquiry and research design: Choosing among five approaches. London: Sage.
- Dewing, J. (2007). A method for process consent with persons who have dementia. Dementia, 6(1), 11–25. doi:10.1177/1471301207075625
- Dewing, J., & Dijk, S. (2016). What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia, 15(1), 106–124. doi:10.1177/1471301213520172
- Farmer, T., Robinson, K., Elliott, S. J., & Eyles, J. (2006). Developing and implementing a triangulation protocol for qualitative health research. Qualitative Health Research, 16(3), 377–394.
- Fleiszer, A. R., Semenic, S. E., Ritchie, J. A., Richer, M. C., & Denis, J. L. (2016). Nursing unit leaders' influence on the long‐term sustainability of evidence‐based practice improvements. Journal of Nursing Management, 24(3), 309–318. doi:10.1111/jonm.12320
- Houghton, C., Murphy, K., Brooker, D., & Casey, D. (2016). Healthcare staffs experiences and perceptions of caring for people with dementia in the acute setting: Qualitative evidence synthesis. International Journal of Nursing Studies, 61, 104–116. doi:10.1016/j.ijnurstu.2016.06.001
- Innes, A., Kelly, F., Scerri, C., & Abela, S. (2016). Living with dementia in hospital wards: A comparative study of staff perceptions of practice and observed patient experience. International Journal of Older People Nursing, 11(2), 94–106. doi:10.1111/opn.12102
- King, N. (1998). Template analysis. In G. Symon & C. Cassell (Eds.), Qualitative methods and analysis in organizational research: A practical guide (pp. 118–134). Thousand Oaks, CA,: Sage Publications Ltd.
- Kirkpatrick, D. L. (1979). Techniques for evaluating training programmes. Training and Development Journal, 33(6), 78–92.
- Kirkpatrick, D. L. (1984). Evaluating training programs: The four levels. San Francisco, CA: Berrett-Koehler.
- Leung, D., & Todd, J. (2010). Dementia care in the acute district general hospital. Clinical Medicine, 10(3), 220–222. doi:10.7861/clinmedicine.10-3-220
- Marsh, D. R., Schroeder, D. G., Dearden, K. A., Sternin, J., & Sternin, M. (2004). The power of positive deviance. BMJ (Clinical Research ed.), 329(7475), 1177–1179.
- Marshall, S., & McIntosh, C. (2018). Strategies for managing adverse events in healthcare simulations. In D. Nestel, B. Jolly, M. Kelly & M. Watson (Eds.), Healthcare simulation education: Evidence, theory and practice. Chichester: John Wley and Sons.
- Mental Capacity Act (2005). c.9.
- Mills, A. J., Durepos, G., & Wiebe, E. (2010). Encyclopedia of case study research (Vols. 1–0). Thousand Oaks, CA: SAGE Publications Ltd. doi:10.4135/9781412957397
- Mukadam, N., & Sampson, E. L. (2011). A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. International Psychogeriatrics, 23(3), 344–355. doi:10.1017/S1041610210001717
- NHS England. (2015). The friends and family test: Guidance. Redditch: NHS England. Available on-line from https://www.england.nhs.uk/wp-content/uploads/2015/07/fft-guidance-160615.pdf [Accessed 5.9.18].
- O'Cathain, A., Murphy, E., & Nicholl, J. (2010). Three techniques for integrating data in mixed methods studies. Bmj (Clinical Research ed.), 341, c4587.
- Palmer, J. L., Lach, H. W., McGillick, J., Murphy-White, M., Carroll, M. B., & Armstrong, J. L. (2014). The dementia friendly hospital initiative education program for acute care nurses and staff. The Journal of Continuing Education in Nursing, 45(9), 416–424. doi:10.3928/00220124-20140825-20
- Pham, J. C., Andrawis, M., Shore, A. D., Fahey, M., Morlock, L., & Pronovost, P. J. (2011). Are temporary staff associated with more severe Emergency Department Medication Errors? Journal for Healthcare Quality, 33(4), 9–18. doi:10.1111/j.1945-1474.2010.00116.x
- Priestland, A., & Hanig, R. (2005). Developing first-level leaders. Harvard Business Review, 83(6), 112–120.
- QSR Inernational Pty Ltd. (2017). NVivo qualitative data analysis Software.
- Quinlan, M., Bohle, P., & Rawlings-Way, O. (2015). Health and safety of homecare workers engaged by temporary employment agencies. Journal of Industrial Relations, 57(1), 94–114. doi:10.1177/0022185614541179
- Richards, G., & DeVries, I. (2011). Revisiting Formative Evaluation: Dynamic Monitoring for the Improvement of Learning Activity Design and Delivery. Paper presented at the LAK '11: Proceedings of the 1st International Conference on Learning Analytics and Knowledge Banff, Alberta, Canada.
- Royal College of Psychiatrists. (2017). National Audit of Dementia care in general hospitals 2016–2017: Third round of audit report. London: Royal College of Psychiatrists.
- Royal College of Psychiatrists. (2013). National Audit of Dementia Care in General Hospitals 2012-13: Second Round Audit Report and Update. Editors: Young J, Hood C, Gandesha A and Souza R. London: HQIP.
- Royal College of Psychiatrists. (2011). Report of the National Audit of Dementia Care in General Hospitals. Editors: Young J, Hood C, Woolley R, Gandesha A and Souza R. London: Healthcare Quality Improvement Partnership.
- Scerri, A., Innes, A., & Scerri, C. (2017). Dementia training programmes for staff working in general hospital settings – A systematic review of the literature. Aging & Mental Health, 21(8), 783–796. doi:10.1080/13607863.2016.1231170
- Schindel Martin, L., Gillies, L., Coker, E., Pizzacalla, A., Montemuro, M., Suva, G., & McLelland, V. (2016). An education intervention to enhance staff self-efficacy to provide dementia care in an acute care hospital in Canada: A nonrandomized controlled study. American Journal of Alzheimer's Disease & Other Dementias, 31(8), 664–677.
- Simons, H. (2009). Case study research in practice. London. Sage.
- Skills for Health, Health Education England, & Skills for Care. (2015). Dementia Core Skills Education and Training Framework, London.
- Stetler, C. B., Ritchie, J. A., Rycroft‐Malone, J., & Charns, M. P. (2014). Leadership for evidence‐based practice: Strategic and functional behaviors for institutionalizing EBP. Worldviews on Evidence-Based Nursing, 11(4), 219–226. doi:10.1111/wvn.12044
- Surr, C., & Gates, C. (2017). What works in delivering dementia education or training to hospital staff? A critical synthesis of the evidence. International Journal Nursing Studies, 75, 172–188. doi:10.1016/j.ijnurstu.2017.08.002
- Surr, C. A., Gates, C., Irving, D., Oyebode, J., Smith, S. J., Parveen, S., … Dennison, A. (2017). Effective dementia education and training for the health and social care workforce: A systematic review of the literature. Review of Educational Research, 87(5), 966–1002. doi:10.3102/0034654317723305
- Surr, C., Sass, C., Griffiths, A., Oyebode, J., Smith, S., Parveen, S., & Drury, M. (2017). Dementia Training Design and Delivery Audit Tool (DeTDAT) v4.0. Leeds: Leeds Beckett University. Retrieved on October 2, 2018, from http://www.leedsbeckett.ac.uk/school-of-health-and-community-studies/what-works/
- Surr, C., Oyebode, J., Parveen, S., Smith, S. J., Capstick, A. & Dennison, A. (2015). Understanding effective dementia workforce education and training: A formative evaluation. National Institute for Health Research Policy Research Programme, Ref PR-R10-0514-12006
- Timmons, S., Manning, E., Barrett, A., Brady, N. M., Browne, V., O’Shea, E., … Linehan, J. G. (2015). Dementia in older people admitted to hospital: A regional multi-hospital observational study of prevalence, associations and case recognition. Age and Ageing, 44(6), 993–999. doi.org/10.1093/ageing/afv131
- Willhaus, J., Averette, M., Gates, M., Jackson, J., & Windnagel, S. (2014). Proactive policy planning for unexpected student distress during simulation. Nurse Educator, 39(5), 232–235. doi:10.1097/nne.0000000000000062
- Yin, R. K. (2013). Case study research: Design and methods. London: Sage Publications.
- Zekry, D., Herrmann, F. R., Grandjean, R., Vitale, A.-M., De Pinho, M.-F., Michel, J.-P., … Krause, K.-H. (2009). Does dementia predict adverse hospitalization outcomes? A prospective study in aged inpatients. International Journal of Geriatric Psychiatry, 24(3), 283–291. doi:10.1002/gps.2104