Abstract
Objectives
Coping strategies may play an important role as facilitator or barrier for functional recovery after hip fracture. This study explored 1] active and passive coping strategies in hip fracture patients within inpatient geriatric rehabilitation (GR) 2] the association of these coping strategies with depression, anxiety, pain and health-related quality of life (HRQoL)
Method
Secondary data analysis (FIT-HIP trial). Participants were patients with hip fracture, aged 65+ years, admitted to post-acute GR units. Coping was assessed using the ‘Active Tackling’ and ‘Passive Reacting’ subscale of Utrecht Coping List (UCL). Depression, anxiety, pain and HRQoL was assessed using GDS-8, HADS-A, NPRS and EQ5D-VAS. Based on UCL norm tables - for both subscales - we dichotomized the group into (extremely) high use of this coping strategy i.e. ‘predominantly active coping’ (PAC), and ‘predominantly passive coping’ (PPC); versus their corresponding ‘residual groups’, i.e. the remaining participants.
Results
72 participants were included. Participants mostly used active coping (PAC: 33.3%), however those engaging in passive coping (23.6%) had significantly more depression and anxiety symptoms (GDS-8 ≥ 3: 31.1% respectively 9.1%, p = 0.040; HADS-A ≥ 7: 58.8% vs 10.9%; p = 0.00).
Conclusion
Active tackling and passive reacting coping strategies are used by up to one-third of patients with recent hip fracture. Passive coping was associated with more symptoms of depression and anxiety, which in turn may influence rehabilitation negatively. Screening of (passive) coping strategies could contribute to prompt identification of hip fracture patients at risk for negative health outcomes.
Trial registration:
Introduction
Hip fracture presents a major health challenge for older adults, with often far-reaching consequences for both physical health and psychosocial well-being (Proctor et al., Citation2008; Ziden, Wenestam, & Hansson-Scherman, Citation2008). The short- and long-term functional impairment and loss of independence associated with hip fracture is illustrated by the fact that only 30–40% of the patients regain their prior level of mobility, and 10–20% are unable to return home (Dyer et al., 2016). From a psychological perspective, symptoms of depression, anxiety and fear of falling (FoF) are frequently seen in patients with hip fracture (Burns et al., Citation2007; Gialanella, Prometti, Monguzzi, & Ferlucci, Citation2014; Visschedijk, Achterberg, Van Balen, & Hertogh, Citation2010; Visschedijk, van Balen, Hertogh, & Achterberg, Citation2013). Alongside the fact that such symptoms are burdensome for the individual patient, these potentially modifiable psychological factors are also known to have a negative effect on the rehabilitation process after hip fracture (Gialanella et al., Citation2014; Lenze et al., Citation2004; Oude Voshaar et al., Citation2006). Coping may be an important factor to consider within this context. Exposure to health problems can be considered a major stressor. The manner in which a patient deals with this distress, i.e. the coping strategy, may influence active participation in and receptiveness for treatment. Certain types of coping (passive or avoidant), have been associated with negative health outcomes, such as more physical impairment, higher levels of pain, and depression (Eisenberg, Shen, Schwarz, & Mallon, Citation2012; Ramírez-Maestre, Esteve, & López, Citation2008; Stoilkova, Wouters, Spruit, Franssen, & Janssen, Citation2013; Visser et al., Citation2015). Coping has also been associated to quality of life, specifically in relation to the long term consequences of health problems such as stroke (Darlington et al., Citation2007).
Coping has been defined by Lazarus & Folkman as “thoughts and behaviours that people use to manage the internal and external demands of situations that are appraised as stressful” (Lazarus, Citation1984). Although many types of coping strategies have been defined in the past years, in general two main categories of coping strategies are utilized, namely the ‘problem-focused coping’ and ‘emotion-focused coping’ (Folkman & Lazarus, Citation1988; Levasseur & Couture, Citation2015). Problem-focused coping is aimed at modifying or managing the source of distress, for example by making a plan of action to solve a problem; and emotion-focused coping is aimed at regulating the negative emotions associated with the problem. In general, active coping approaches will be more oriented towards problem-focused coping, while passive coping is characterized by avoidance and is more emotion-focused. Different types of coping strategies can be used for the same stressor, as individuals will have to deal with the demands of the stressor itself, and manage their emotions. The choice for type of strategy may depend on whether or not the problem is perceived as modifiable. When evaluating coping strategies, it is also important to keep in mind that the efficacy of the different approaches is situational, and may change within the course of time (duration of stressor) (Blum, Brow, & Silver, Citation2012).
Only one study has previously evaluated specific coping strategies within patients that have sustained a hip fracture (Roberto, Citation1992). The study population consisted solely of female patients, and found that older women used a variety of coping strategies, with ‘seeking social support’ being the strategy most frequently used. Several emotion-focused coping strategies were associated with poorer functional recovery after hip fracture. This study however is more than 25 years old, was not performed within a rehabilitation setting and took place long after hip fracture (on average 8 months). In a broader perspective, a recent systematic mixed methods review provided additional insight into how older adults deal with the consequences of hip fracture in daily life (Lind & Mahler, Citation2019). Important topics identified within this health promoting perspective were the battle for independence, active participation, and willingness to engage in their recovery. Within this regard, a patient’s ability to identify and use resources to manage with the challenges, and their motivation to influence decisions seem to be important to support the recovery process.
As coping may have a substantial role within the recovery process of a major health-related stressor such as hip fracture (Proctor et al., Citation2008), it is important to gain a better understanding of coping in the early stage of rehabilitation. The objectives of this study are therefore to i] explore the active and passive coping strategies used by older patients with a recent hip fracture participating in a multidisciplinary inpatient geriatric rehabilitation programme, and ii] evaluate the association between the above-mentioned coping strategies and the presence of symptoms of depression and anxiety, pain and patient’s health-related quality of life (HRQoL).
Methods
Study design
This explorative cross-sectional study is a secondary data analysis of the FIT-HIP trial, a cluster randomized controlled trial evaluating treatment of fear of falling (FoF) in older adults with hip fracture, within inpatient geriatric rehabilitation (GR) (the Netherlands). A full description of the study protocol has been published previously (Scheffers-Barnhoorn et al., Citation2017). In short, usual care for patients with hip fracture in GR is compared to the addition of the intervention aimed to reduce FoF, embedded in usual care. The FIT-HIP intervention is conducted by physiotherapists in GR and is based on various cognitive behavioural approaches.
Ethical approval for the trial was provided by the Ethics Committee of the Leiden University Medical Centre (LUMC), and the study was registered in the Netherlands Trial Register (NTR5695). All participants provided written informed consent prior to study procedures.
Participants and data collection
Recruitment and enrolment for the FIT-HIP trial took place from March 2016 - January 2017. Participants were older adults aged 65 years and above, with a recent hip fracture and FoF, admitted to one of the 11 participating GR units. FoF was assessed using a single question - ‘Are you concerned to fall?’ - with five answer categories (never - almost – never - sometimes - often - very often). Patients that reported being at least sometimes concerned to fall were eligible to participate. Key exclusion criteria included 1) conditions interfering with learnability (cognitive impairment, major psychiatric disease, insufficient mastery of the Dutch language) and 2) factors prognostic for limited functional recovery (pre-fracture Barthel index score < 15, presence of pathological hip fracture, life expectancy of < 3 months).
For the current analysis, we included all participants with complete ‘active tackling’ and ‘passive reacting’ subscales of the Utrecht Coping List (UCL) questionnaire (N = 72 of the 78 participants in the FIT-HIP trial).
Outcome measures
All outcome measures were assessed at baseline; the first week of inpatient geriatric rehabilitation programme. Coping strategies were assessed using the Utrecht Coping List (UCL) (Schreurs, V, Brosschot, Tellegen, & Graus, Citation1993; Turner, Bryant-Waugh, Peveler, & Bucks, Citation2012). This measurement instrument is validated for persons aged 14 years and older. The UCL consists of 47 questions categorized in the following seven subscales: ‘active tackling’, ‘passive reacting’, ‘palliative reacting’, ‘seeking social support’, ‘avoidance’, ‘expressing of emotions’ and ‘reassuring thoughts’. For this study we assessed the ‘active tackling’ and ‘passive reacting’ subscales of UCL, both comprising of 7 items. An overview of the items of the active tackling and passive reacting subscales is presented in Appendix 1. Each item can be answered on a four-point Likert scale, measuring how often an individual uses that particular strategy (1: never; 2: sometimes; 3: often and 4: very often). For both subscales, summed scores range from 7 to 28, with higher scores indicating a greater use of that strategy. Each UCL subscale has individual gender-specific norm tables.
To assess symptoms of depression, the 8-item Geriatric Depression Score (GDS-8) was used, a short version of GDS-30. GDS-8 has been validated for purposes of screening for depression in vulnerable older adults (Jongenelis et al., Citation2007). A higher score suggests more depressive symptoms (maximum score 8), and a score of three or more is indicative of relevant depressive symptoms. The Hospital Anxiety and Depression Scale - Anxiety subscale (HADS-A) was used to measure symptoms of anxiety in older adults (Spinhoven et al., Citation1997). HADS-A subscale consists of seven items, rated on a four-point Likert scale (maximum score: 21, higher score indicating more symptoms of anxiety). A cut-off value of seven is employed as a score that is suggestive of anxiety, which may require additional medical attention. In our study pain was assessed with the Numeric Pain Rating Scale (NPRS), a self-report measure used to assess the intensity of pain on a 11-point scale (0 representing no pain, up to 10 representing severe disabling pain) (Herr, Spratt, Mobily, & Richardson, Citation2004; Hjermstad et al., 2011). In general a cut-off value of ≥ four is handled as moderate pain. HRQoL was assessed with the EQ5D-VAS (scale 0-100, with a higher score indicating better perceived quality of life) ("EuroQol Research Foundation," 2020).
Other variables
Sociodemographic data were collected at baseline. Comorbidity was measured using Functional Comorbidity Index (FCI) (Groll, To, Bombardier, & Wright, Citation2005). Additionally we collected information regarding medication use (drug prescriptions at admission to GR).
Statistical analysis
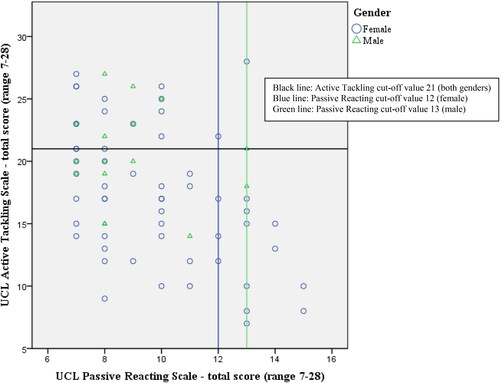
Descriptive statistics were used to present the general characteristics of the study population. Subsequently, we made a distinction between the study population as a whole, and the subgroups of participants with tendency to use active tackling and/or passive reacting coping strategies. For both subscales separately, we used the existing norm tables to dichotomize the group of participants into a group that: i] predominantly uses active tackling and/or passive reacting coping strategies, versus ii] the remaining part of the group that does not regularly engage in these coping strategies (i.e. the ‘residual group’). The norm tables comprise of five categories based on the summed score (range 7-28), namely: ‘extremely low’-, ‘low’-, ‘average’-, ‘high’- and ‘extremely high’ use of this coping strategy (Schreurs et al., Citation1993). Participants that scored high or extremely high on the active tackling and/or passive reacting subscale were defined as the group with ‘predominantly active coping (PAC)’ respectively ‘predominantly passive coping (PPC)’. The remaining part of the group, with participants that scored extremely low, low or average, was characterized as the ‘residual group’. For the active tackling subscale, a cut-off score of 21 was employed (both sexes). For the passive reacting subscale the cut-off value was 12 for female and 13 for male gender.
To categorize GDS-8, HADS-A and NPRS based on the presence of relevant symptom burden, we dichotomized the scores based the previously mentioned cut-off values. The Fisher exact test was performed to analyse the associations between coping strategies and depression, anxiety, pain (comparing proportions); the Mann Whitney test for the association with HLQoL as the distribution of this data was skewed. All analyses were conducted using SPSS for Windows (version 23.0). The significance threshold was set at 0.05 for all analyses.
Results
A total of 72 patients were included in this study. presents the baseline characteristics for all participants, the PAC and PPC group. Within the whole study population, the majority was female (77.8%) and lived alone prior to the hip fracture (63.8%). One third of the participants were categorized into the PAC group (N = 19 with high active coping and N = 5 very high active coping). Seventeen participants (23.6%) predominantly used passive reacting coping strategies ().
Table 1. Characteristics of the study population; additionally specified for participants with predominantly active and/or passive coping.
Table 2. Active Tackling and Passive Reacting coping at onset of inpatient geriatric rehabilitation.
Participants in the PPC group were slightly younger when compared to the total population (78.4 versus 82.3 years) and were predominantly female (88.2%). When comparing the PPC to the PAC group, participants with tendency for passive reacting coping reported a lower level of HLQoL but lower levels of pain. Use of pain medication, paracetamol in particular, was high in all participants.
To determine if high levels of active tackling and passive reacting coping can coincide within individual patients, we drafted a scatterplot presented in . Three participants (4.2%) scored high on both subscales.
With regard to the specific coping strategies (items per coping subscale), ‘thinking of different possibilities to solve problems’ and ‘staying calm in a difficult situation’ were the active tackling strategies that were reported most often (49% respectively 48% of all participants reported using this (very) often). For the passive reacting strategies, ‘being totally preoccupied with a problem’ was reported most often (12% of all participants), followed by ‘being worried about their past’ (11%). No participants reported substance abuse as a form of passive coping strategy when experiencing problems.
shows the associations between active tackling respectively passive reacting coping, and symptoms of depression and anxiety, pain and perceived quality of health. The PAC- and PPC groups were compared to their corresponding residual group; i.e. the remaining participants, that scored (very) low to average on the specific subscales. Significantly more participants in the PPC group had a GDS score ≥ 3 or HADS-A score of ≥ 7 when compared to the residual group (GDS-8 score ≥ 3: 31.1% respectively 9.1%, p = 0.040; and HADS-A score ≥ 7: 58.8% vs 10.9%; p = 0.00). No significant associations were found for the PAC group. Coping strategies were not associated with pain (NPRS ≥ 4) and HLQoL.
Table 3. Association between active and passive coping with symptoms of depression, anxiety, pain and health related quality of life.
Discussion
The findings of this study show that a reasonable proportion (one-third) of the older adults that have recently sustained a hip fracture and are at onset of an inpatient geriatric rehabilitation programme, use an active tackling coping approach. However, almost a quarter of the participants engage in passive reacting coping, and this group has significantly more symptoms of depression and anxiety. No associations were found for coping with pain or HRQoL.
To our knowledge detailed information regarding the use of specific coping strategies within the population of patients with hip fracture have only been reported in one previous study (Roberto, Citation1992). The study population differed from our study in that sense that all participants were women. A second noteworthy difference is the timing of the assessment of coping in relation to the stressor, on average eight months after hip fracture in contrast to 1-2 weeks post-fracture in our study. More specifically, the difference in timing represents a different phase of functional recovery after hip fracture; and accordingly distinct health challenges related to the hip fracture (Magaziner, Chiles, & Orwig, Citation2015). Although the coping data of the two studies does somewhat differ, in part due to the fact that the current study did not include all UCL subscales in order to reduce the burden for participants, some comparisons can be made. In Roberto’s study, coping was assessed with the Ways of Coping Questionnaire, and based on this evaluation the strategy ‘seeking social support’ was used most frequently, followed by ‘accepting responsibility’ and ‘self-controlling’ (both emotion-focused), and ‘planful problem-solving’ (problem-focused). In contrast to reasonable levels of active tackling in our study, ‘active confronting’ was used least in Roberto’s study. Although participants in both studies report regular use of some form of problem-focused coping, the discrepancies in the preference for type of coping strategy could largely be explained by the time-frame (i.e. timing of assessment of coping in relation to the stressor). For a better understanding of how a temporal factor contributes to differences in the choice of coping strategy, findings should be interpreted within the general principles of coping in older age.
Literature on coping in older adults describes the following principles. 1] Older adults are confronted by different stressors than younger individuals. With increasing age, adults will more frequently be confronted with health problems, disability and grief (Chen, Peng, Xu, & O'Brien, Citation2018; Nieto et al., Citation2020). The type of stressor(s) may also model or determine the choice of coping strategies; depending on whether the problem can be modified, or if it is more suitable to deal with the emotional consequences. 2] In general, older adults remain able to use the different types of coping strategies effectively. However, it has also been observed that they use less strategies, less frequently use active confrontive strategies, and often employ emotion-focused coping. Seeking social support is frequently reported in this population (Chen et al., Citation2018; Folkman, Lazarus, Pimley, & Novacek, Citation1987; Lau, Citation1994; Levasseur & Couture, Citation2015). 3] However, in light of dealing with health-problems and aging limitations, both problem-focused coping and emotion-focused approaches are commonly used (Levasseur & Couture, Citation2015; Löffler et al., Citation2012).
Thus, when faced with a health-related stressor, what determines an individual’s response and preference for a more problem-focused or emotion-focused approach? Folkman & Lazarus state that an individual’s appraisal of the event, either as negative and stressful, or as challenges to be handled, influence their choice of coping strategies (Folkman & Lazarus, Citation1980). We could argue that the time-frame of confrontation with the stressor affects patients’ appraisal of the stressor, through experience with and hence expectations regarding the impact of this problem. In other words is it realistic to expect improvement or functional recovery; or should this health condition be considered chronic, with permanent disabilities? Hip fracture is an acute event with sudden physical impairment. If older adults have the expectation to recover, following the surgical repair, it is likely that at the beginning of a rehabilitation programme patients have a greater focus on their recovery process. This in turn could influence their motivation for active engagement in therapy. As the time proceeds and patients come to appraise the consequences of the hip fracture as an enduring health problem, the focus may shift to more emotion-focused strategies, as also seen in the study performed by Roberto. This is also illustrated in a longitudinal study on rehabilitation after brain injury, which showed that patients used less active problem-focused and more passive emotion-focused coping within the course of the rehabilitation (Wolters, Stapert, Brands, & Van Heugten, Citation2010). Likewise, this may also explain why patients with a chronic condition such as COPD (chronic obstructive pulmonary disease) have lower levels of active tackling coping when admitted to inpatient rehabilitation (16.5% versus 33.3% in our study; both assessed with the UCL) (Stoilkova, Wouters, et al., Citation2013).
The second finding in the current study, that passive reacting coping was associated with more symptoms of depression and anxiety, confirm Roberto’s findings. There is a considerable amount of evidence in support of this association, both for the general geriatric population (Bjørkløf, Engedal, Selbaek, Kouwenhoven, & Helvik, Citation2013; Bjørkløf et al., Citation2016; Murayama, Yamazaki, Yamaguchi, Hasebe, & Fujiwara, Citation2020), and also specifically for patients within a rehabilitation setting (stroke, COPD) (Stoilkova, Wouters, et al., Citation2013; Visser et al., Citation2015). Although the causal relationship between coping and mood/anxiety has not yet been defined for patients with hip fracture, findings from this study show that a quarter of the patients use passive reacting strategies, which in turn may add to the risk of depression and anxiety. Prevalence rates for anxiety and depression are high among older adults with hip fracture (35.0% respectively 44.5%) (Gialanella et al., Citation2014) (Charles-Lozoya et al., Citation2019) (Feng et al., Citation2010), and these conditions are associated with a greater risk of poor outcomes of rehabilitation (Gialanella, Ferlucci, Monguzzi, & Prometti, Citation2015; Lenze et al., Citation2004; Proctor et al., Citation2008). Moreover, there is evidence to suggest that 10% of patients with hip fracture develop depressive symptoms after fracture, with a persistent high level of symptoms up to a year after fracture (Cristancho, Lenze, Avidan, & Rawson, Citation2016). Prompt identification of depressive symptoms and associated risk-factors for new-onset mood disorders are therefore important to facilitate recovery after fracture.
Depression in this population may however prove to be a challenge. At present, there is limited evidence for effective interventions to prevent or address depression in patients with hip fracture (Burns et al., Citation2007; Romeo et al., Citation2011). Moreover, current literature on late-life depression demonstrates that depression in older age has a more chronic course, and an increased risk to be treatment resistant (Schaakxs et al., Citation2018). From a biological perspective, certain factors related to the (neuro)biological aging process such as physical frailty and cognitive decline, may contribute to the development and expression of neuropsychiatric symptoms, and in part explain the impaired prognosis of late-life depression (Lugtenburg et al., Citation2021). How all these mechanisms relate to each other, is still unknown, and is at present subject to further research (Reynolds, Lenze, & Mulsant, Citation2019).
From a clinical perspective however, it is important to focus on modifiable factors that have potential to aid the recovery process. Within this regard, it may be beneficial to assess coping within the rehabilitation after hip fracture. Passive coping strategies, through their tendency for avoidance behaviour, could possibly complicate adherence and commitment to treatment (Choi, Hegel, Sirrianni, Marinucci, & Bruce, Citation2012). However, programmes based on cognitive behavioural approaches, such as problem-solving therapy (PST), may have potential to enhance adaptive problem-solving coping skills. Such approaches have proven to be effective in rehabilitation after stroke (Visser et al., Citation2016). More specifically, PST has proven to be effective to reduce depressive symptoms in older adults with passive coping (Choi et al., Citation2012). At present however, hip fracture rehabilitation programmes do not include assessment of coping or treatment programmes to enhance coping skills. This therefore remains an area of attention for further research and clinical practice.
Limitations of the present study
There are several limitations of the present study. First, it is important to acknowledge that we only assessed active and passive coping strategies. We limited the number of subscales, in order to limit the burden for participants. The choice for these two subscales was based on the fact that we expect these strategies to be most relevant for the inpatient rehabilitation setting; i.e. facilitating or hampering the early phase of recovery. This does however lead to a lack of insight into other potentially important coping strategies for the geriatric population, such as seeking social support. Secondly, due to the cross-sectional design it is not possible to demonstrate cause and effect in the association between coping strategies and symptoms of depression and anxiety. Accordingly, the direct effect of coping strategies on rehabilitation outcome remains uncertain. Third, data from this study was derived from FIT-HIP trial, which was not primarily designed to address the coping strategies. All participants had FoF, which may have biased the findings regarding symptoms of anxiety and depression. On the other hand, FoF has been reported in as much as 60% of the older patients with hip fracture (Visschedijk et al., Citation2013), and the level of anxiety reported in the study population was low (Scheffers-Barnhoorn et al., Citation2019). Also, FoF is not limited to patients with hip fracture; prevalence rates in the general geriatric population and in other geriatric rehabilitation patients are high too (Scheffer, Schuurmans, van Dijk, van der Hooft, & de Rooij, Citation2008; Visschedijk, Caljouw, Bakkers, van Balen, & Achterberg, Citation2015). Hence, the study population should be reasonably representative for hip patients in general. Fourth, the UCL norm tables are based on data of older adults with a maximum age limit of 65 years, and we can therefore question whether these are applicable for the oldest-old. However, at present there is no other alternative validated coping instrument specifically for older adults. Previous studies with older adults within a rehabilitation setting have used the UCL too (Stoilkova, Janssen, Franssen, Spruit, & Wouters, Citation2013). Last, the sample size was limited, which may affect the strength and certainty of associations. However, we may consider the study as an explorative study and hence the insights as an orientation on coping in this specific target population.
Conclusion and future implications
The findings of this study show that a reasonable proportion of patients with hip fracture engage in active tackling coping strategies at onset of inpatient rehabilitation. However, also roughly a quarter of the patients predominantly use passive coping strategies. Passive coping was associated more symptoms of depression and anxiety, which in turn may add to the risk of poorer functional recovery after hip fracture. To timely identify patients at risk for negative outcome(s) of rehabilitation, more specifically for psychological problems that may intervene with recovery, we advocate screening for (passive) coping strategies at onset of the rehabilitation. Future research is needed to gain insight into the relationship between coping and mood/anxiety for patients with hip fracture. Additionally, research should focus on intervention possibilities to enhance skills for more efficient coping.
Acknowledgements
The authors thank all participants and the staff of the participating post-acute geriatric rehabilitation units for their participation in this study. We are grateful for the team of independent research assistants for their role in the inclusion of participants and the data acquisition. This study was performed within the University Network for the Care Sector South Holland in the Netherlands (UNC-ZH), and we are grateful that this study was facilitated within this network.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Bjørkløf, G. H., Engedal, K., Selbaek, G., Kouwenhoven, S. E., & Helvik, A. S. (2013). Coping and depression in old age: A literature review. Dementia and Geriatric Cognitive Disorders, 35(3–4), 121–154. doi:https://doi.org/10.1159/000346633
- Bjørkløf, G. H., Engedal, K., Selbaek, G., Maia, D. B., Coutinho, E. S., & Helvik, A. S. (2016). Locus of control and coping strategies in older persons with and without depression. Aging & Mental Health, 20(8), 831–839. doi:https://doi.org/10.1080/13607863.2015.1040722
- Blum, S., Brow , M., & Silver, R. C. (2012). Coping. In Encyclopedia of human behavior (2nd ed., pp. 596–601). Elsevier. doi:https://doi.org/10.1016/B978-0-12-375000-6.00110-5
- Burns, A., Banerjee, S., Morris, J., Woodward, Y., Baldwin, R., Proctor, R., … Horan, M. (2007). Treatment and prevention of depression after surgery for hip fracture in older people: Randomized, controlled trials. Journal of the American Geriatrics Society, 55(1), 75–80. doi:https://doi.org/10.1111/j.1532-5415.2007.01016.x
- Charles-Lozoya, S., Cobos-Aguilar, H., Barba-Gutiérrez, E., Brizuela-Ventura, J. M., Chávez-Valenzuela, S., García-Hernández, A., & Tamez-Montes, J. C. (2019). Depression and geriatric assessment in older people admitted for hip fracture. Revista Médica de Chile, 147(8), 1005–1012. doi:https://doi.org/10.4067/S0034-98872019000801005
- Chen, Y., Peng, Y., Xu, H., & O'Brien, W. H. (2018). Age differences in stress and coping: Problem-focused strategies mediate the relationship between age and positive affect. International Journal of Aging & Human Development, 86(4), 347–363. doi:https://doi.org/10.1177/0091415017720890
- Choi, N. G., Hegel, M. T., Sirrianni, L., Marinucci, M. L., & Bruce, M. L. (2012). Passive coping response to depressive symptoms among low-income homebound older adults: Does it affect depression severity and treatment outcome? Behaviour Research and Therapy, 50(11), 668–674. doi:https://doi.org/10.1016/j.brat.2012.07.003
- Cristancho, P., Lenze, E. J., Avidan, M. S., & Rawson, K. S. (2016). Trajectories of depressive symptoms after hip fracture. Psychological Medicine, 46(7), 1413–1425. doi:https://doi.org/10.1017/S0033291715002974
- Darlington, A. S., Dippel, D. W., Ribbers, G. M., van Balen, R., Passchier, J., & Busschbach, J. J. (2007). Coping strategies as determinants of quality of life in stroke patients: A longitudinal study. Cerebrovascular Diseases (Basel, Switzerland), 23(5–6), 401–407. doi:https://doi.org/10.1159/000101463
- Dyer, S. M., Crotty, M., Fairhall, N., Magaziner, J., Beaupre, L. A., Cameron, I. D., & Sherrington, C., Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. (2016). A critical review of the long-term disability outcomes following hip fracture. BMC Geriatrics, 16, 158. doi:https://doi.org/10.1186/s12877-016-0332-0.
- Eisenberg, S. A., Shen, B. J., Schwarz, E. R., & Mallon, S. (2012). Jun). Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. Journal of Behavioral Medicine, 35(3), 253–261. doi:https://doi.org/10.1007/s10865-011-9358-0
- EuroQol Research Foundation. (2020). https://euroqol.org/.
- Feng, L., Scherer, S. C., Tan, B. Y., Chan, G., Fong, N. P., & Ng, T. P. (2010). Comorbid cognitive impairment and depression is a significant predictor of poor outcomes in hip fracture rehabilitation. International Psychogeriatrics, 22(2), 246–253. doi:https://doi.org/10.1017/S1041610209991487
- Folkman, S., & Lazarus, R. S. (1980). An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior, 21(3), 219–239. doi:https://doi.org/10.2307/2136617
- Folkman, S., & Lazarus, R. S. (1988). Manual for the ways of coping questionnaire. Palo Alto, CA: Consulting Psychologist Press.
- Folkman, S., Lazarus, R. S., Pimley, S., & Novacek, J. (1987). Age differences in stress and coping processes. Psychology and Aging, 2(2), 171–184. doi:https://doi.org/10.1037//0882-7974.2.2.171
- Gialanella, B., Ferlucci, C., Monguzzi, V., & Prometti, P. (2015). Determinants of functional outcome in hip fracture patients: The role of specific neuropsychiatric symptoms. Disability and Rehabilitation, 37(6), 517–522. doi:https://doi.org/10.3109/09638288.2014.932446
- Gialanella, B., Prometti, P., Monguzzi, V., & Ferlucci, C. (2014). Jul). Neuropsychiatric symptoms and rehabilitation outcomes in patients with hip fracture. American Journal of Physical Medicine & Rehabilitation, 93(7), 562–569. doi:https://doi.org/10.1097/PHM.0000000000000062
- Groll, D. L., To, T., Bombardier, C., & Wright, J. G. (2005). The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology, 58(6), 595–602. doi:https://doi.org/10.1016/j.jclinepi.2004.10.018
- Herr, K. A., Spratt, K., Mobily, P. R., & Richardson, G. (2004). Pain intensity assessment in older adults: Use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. The Clinical Journal of Pain, 20(4), 207–219. doi:https://doi.org/10.1097/00002508-200407000-00002
- Hjermstad, M. J., Fayers, P. M., Haugen, D. F., Caraceni, A., Hanks, G. W., Loge, J. H., … Kaasa, S., European Palliative Care Research Collaborative (EPCRC). (2011). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: A systematic literature review. Journal of Pain and Symptom Management, 41(6), 1073–1093. doi:https://doi.org/10.1016/j.jpainsymman.2010.08.016
- Jongenelis, K., Gerritsen, D. L., Pot, A. M., Beekman, A. T., Eisses, A. M., Kluiter, H., & Ribbe, M. W. (2007). Construction and validation of a patient- and user-friendly nursing home version of the Geriatric Depression Scale. International Journal of Geriatric Psychiatry, 22(9), 837–842. doi:https://doi.org/10.1002/gps.1748
- Lau, B. W. K. (1994). Stress, coping and ageing. J.H.K.C. Psychiatry, 4, 39–44.
- Lazarus, R. S. F., S. (1984). Stress, appraisal, and coping. New York: Springer, 141.
- Lenze, E. J., Munin, M. C., Dew, M. A., Rogers, J. C., Seligman, K., Mulsant, B. H., & Reynolds, C. F. 3rd. (2004). Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. International Journal of Geriatric Psychiatry, 19(5), 472–478. doi:https://doi.org/10.1002/gps.1116
- Levasseur, M., & Couture, M. (2015). Coping strategies associated with participation and quality of life in older adults. Canadian Journal of Occupational Therapy. Revue canadienne d'ergotherapie, 82(1), 44–53. doi:https://doi.org/10.1177/0008417414552188
- Lind, J., & Mahler, M. (2019). A systematic mixed methods review: Recovering from a hip fracture in a health promoting perspective. Nursing Open, 6(2), 313–329. doi:https://doi.org/10.1002/nop2.214
- Löffler, C., Kaduszkiewicz, H., Stolzenbach, C. O., Streich, W., Fuchs, A., van den Bussche, H., … Altiner, A. (2012). Coping with multimorbidity in old age-a qualitative study. BMC Family Practice, 13, 45. doi:https://doi.org/10.1186/1471-2296-13-45.
- Lugtenburg, A., Zuidersma, M., Wardenaar, K. J., Aprahamian, I., Rhebergen, D., Schoevers, R. A., & Oude Voshaar, R. C. (2021). Subtypes of late-life depression: A data-driven approach on cognitive domains and physical frailty. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 76(1), 141–150. doi:https://doi.org/10.1093/gerona/glaa110
- Magaziner, J., Chiles, N., & Orwig, D. (2015). Recovery after hip fracture: Interventions and their timing to address deficits and desired outcomes-evidence from the Baltimore hip studies. Nestle Nutrition Institute Workshop Series, 83, 71–81. doi:https://doi.org/10.1159/000382064.
- Murayama, Y., Yamazaki, S., Yamaguchi, J., Hasebe, M., & Fujiwara, Y. (2020). Chronic stressors, stress coping and depressive tendencies among older adults. Geriatrics & Gerontology International, 20(4), 297–303. doi:https://doi.org/10.1111/ggi.13870
- Nieto, M., Romero, D., Ros, L., Zabala, C., Martínez, M., Ricarte, J. J., … Latorre, J. M. (2020). Differences in coping strategies between young and older adults: The role of executive functions. International Journal of Aging & Human Development, 90(1), 28–49. doi:https://doi.org/10.1177/0091415018822040
- Oude Voshaar, R. C., Banerjee, S., Horan, M., Baldwin, R., Pendleton, N., Proctor, R., … Burns, A. (2006). Fear of falling more important than pain and depression for functional recovery after surgery for hip fracture in older people. Psychological Medicine, 36(11), 1635–1645. doi:https://doi.org/10.1017/S0033291706008270
- Proctor, R., Wade, R., Woodward, Y., Pendleton, N., Baldwin, R., Tarrier, N., … Burns, A. (2008). The impact of psychological factors in recovery following surgery for hip fracture. Disability and Rehabilitation, 30(9), 716–722. doi:https://doi.org/10.1080/09638280701403536
- Ramírez-Maestre, C., Esteve, R., & López, A. E. (2008). Cognitive appraisal and coping in chronic pain patients. European Journal of Pain (London, England), 12(6), 749–756. doi:https://doi.org/10.1016/j.ejpain.2007.11.004
- Reynolds, C. F., Lenze, E., & Mulsant, B. H. (2019). Assessment and treatment of major depression in older adults. Handbook of Clinical Neurology, 167, 429–435. doi:https://doi.org/10.1016/b978-0-12-804766-8.00023-6.
- Roberto, K. A. (1992). Coping strategies of older women with hip fractures: Resources and outcomes. Journal of Gerontology, 47(1), P21–26. doi:https://doi.org/10.1093/geronj/47.1.p21
- Romeo, R., Knapp, M., Banerjee, S., Morris, J., Baldwin, R., Tarrier, N., … Burns, A. (2011). Treatment and prevention of depression after surgery for hip fracture in older people: Cost-effectiveness analysis. Journal of Affective Disorders, 128(3), 211–219. doi:https://doi.org/10.1016/j.jad.2010.07.026
- Schaakxs, R., Comijs, H. C., Lamers, F., Kok, R. M., Beekman, A. T. F., & Penninx, B. (2018). Associations between age and the course of major depressive disorder: A 2-year longitudinal cohort study. The Lancet Psychiatry, 5(7), 581–590. doi:https://doi.org/https://doi.org/10.1016/S2215-0366(18)30166-4
- Scheffer, A. C., Schuurmans, M. J., van Dijk, N., van der Hooft, T., & de Rooij, S. E. (2008). Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing, 37(1), 19–24. doi:https://doi.org/10.1093/ageing/afm169
- Scheffers-Barnhoorn, M. N., van Eijk, M., van Haastregt, J. C. M., Schols, J., van Balen, R., van Geloven, N., … Achterberg, W. P. (2019). Effects of the FIT-HIP intervention for fear of falling after hip fracture: A cluster-randomized controlled trial in geriatric rehabilitation. Journal of the American Medical Directors Association, 20(7), 857–865. doi:https://doi.org/10.1016/j.jamda.2019.03.009
- Scheffers-Barnhoorn, M. N., van Haastregt, J. C., Schols, J. M., Kempen, G. I., van Balen, R., Visschedijk, J. H., … van Eijk, M. (2017). A multi-component cognitive behavioural intervention for the treatment of fear of falling after hip fracture (FIT-HIP): Protocol of a randomised controlled trial. BMC Geriatrics, 17(1), 71. doi:https://doi.org/10.1186/s12877-017-0465-9.
- Schreurs, P. J. G., V, D. W. G., Brosschot, J. F., Tellegen, B., & Graus, G. M. H. (1993). De Utrechtse Coping Lijst, UCL omgaang met problemen en gebeurtenissen [The Utrecht Coping List]. Lisse, The Netherlands: Swets en Zeitlinger.
- Spinhoven, P., Ormel, J., Sloekers, P. P., Kempen, G. I., Speckens, A. E., & Van Hemert, A. M. (1997). A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological medicine, 27(2), 363–370. doi:https://doi.org/10.1017/s0033291796004382
- Stoilkova, A., Janssen, D. J., Franssen, F. M., Spruit, M. A., & Wouters, E. F. (2013). Coping styles in patients with COPD before and after pulmonary rehabilitation. Respiratory Medicine, 107(6), 825–833. doi:https://doi.org/10.1016/j.rmed.2013.03.001
- Stoilkova, A., Wouters, E. F., Spruit, M. A., Franssen, F. M., & Janssen, D. J. (2013). The relationship between coping styles and clinical outcomes in patients with COPD entering pulmonary rehabilitation. COPD: Journal of Chronic Obstructive Pulmonary Disease, 10(3), 316–323. doi:https://doi.org/10.3109/15412555.2012.744389
- Turner, H., Bryant-Waugh, R., Peveler, R., & Bucks, R. S. (2012). A psychometric evaluation of an English version of the Utrecht coping list. European Eating Disorders Review: The Journal of the Eating Disorders Association, 20(4), 339–342. doi:https://doi.org/10.1002/erv.2173
- Visschedijk, J. H., Caljouw, M. A., Bakkers, E., van Balen, R., & Achterberg, W. P. (2015). Longitudinal follow-up study on fear of falling during and after rehabilitation in skilled nursing facilities. BMC Geriatrics, 15, 161. doi:https://doi.org/10.1186/s12877-015-0158-1.
- Visschedijk, J., Achterberg, W., Van Balen, R., & Hertogh, C. (2010). Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society, 58(9), 1739–1748. doi:https://doi.org/10.1111/j.1532-5415.2010.03036.x
- Visschedijk, J., van Balen, R., Hertogh, C., & Achterberg, W. (2013). Fear of falling in patients with hip fractures: prevalence and related psychological factors. Journal of the American Medical Directors Association, 14(3), 218–220. doi:https://doi.org/10.1016/j.jamda.2012.10.013
- Visser, M. M., Heijenbrok-Kal, M. H., Spijker, A. V., Oostra, K. M., Busschbach, J. J., & Ribbers, G. M. (2015). Coping, problem solving, depression, and health-related quality of life in patients receiving outpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation, 96(8), 1492–1498. doi:https://doi.org/10.1016/j.apmr.2015.04.007
- Visser, M. M., Heijenbrok-Kal, M. H., Van't Spijker, A., Lannoo, E., Busschbach, J. J., & Ribbers, G. M. (2016). Problem-solving therapy during outpatient stroke rehabilitation improves coping and health-related quality of life: Randomized controlled trial. Stroke, 47(1), 135–142. doi:https://doi.org/10.1161/STROKEAHA.115.010961
- Wolters, G., Stapert, S., Brands, I., & Van Heugten, C. (2010). Coping styles in relation to cognitive rehabilitation and quality of life after brain injury. Neuropsychological Rehabilitation, 20(4), 587–600. doi:https://doi.org/10.1080/09602011003683836
- Ziden, L., Wenestam, C. G., & Hansson-Scherman, M. (2008). A life-breaking event: Early experiences of the consequences of a hip fracture for elderly people. Clinical Rehabilitation, 22(9), 801–811. doi:https://doi.org/10.1177/0269215508090204