Abstract
Objectives
To examine current UK practice in diagnosis of patients under 65 with young onset dementia, within 5 years of date of diagnosis, identified from electronic health records of 8 NHS mental health trusts.
Methods
Patients diagnosed with young onset dementia were assembled from the UK-Clinical Record Interactive System, (UK-CRIS) using diagnosis of dementia as the index date. A pre-designed proforma, derived by international Delphi consensus from experts in the field in previous work, was used to assess components of the diagnostic assessment in 402 electronic health records across 8 NHS sites. Information was extracted on key aspects of clinical and physical examination according to both a minimum and gold standard.
Results
Percentage compliance rates analysed by NHS site and statement, including compliance for site for minimum standard (11 statements), the additional 20 statements required for Gold standard, and the complete Gold standard set (31 statements) show that the additional 20 statements in the Gold standard had consistently higher compliance rates for every site compared to the minimum set.
Conclusion
Findings confirmed variation in clinical practice and identified commonly missed items in examination and enquiry compared to expert consensus. This suggests that a template proforma, which contains the key indicators for comprehensive assessment of dementia in young adults according to a quality standard could help support clinicians to improve record keeping and reduce gaps in knowledge.
Introduction
Young onset dementia (YOD) refers to dementia diagnosed in those aged 65 years and under. YOD is poorly recognised and often misdiagnosed (Konijnenberg et al., Citation2017; Salem et al., Citation2014) because presenting symptoms are complex, conditions are heterogenous in presentation and atypical compared to those of late onset disease (LOD). Alzheimer’s disease is common in YOD, accounting for a third of cases, but presentation is frequently atypical characterised by non-memory impairment, such as language, visuo-spatial, executive, behavioural or motor-led dysfunction (Graff-Radford et al, Citation2021, O’Malley et al, Citation2019, Koedam et al Citation2010). Frontotemporal dementia is more frequent, characterised by behavioural changes, for example inappropriate social interactions, lack of empathy, poor motivation, and reduced insight which can delay help-seeking (Kuruppu & Matthews Citation2013, Draper et al, Citation2016). Alcohol-related dementia and HIV-associated cognitive impairment require multidisciplinary and multi-agency approaches (Rao & Draper, Citation2018, Underwood & Winston, Citation2016).
Significant delays can arise in time to diagnosis from GP referral depending on service type (Hussey & Butler, Citation2019). Many younger people in the UK continue to be assessed and diagnosed in memory services where there is typically limited access to other multidisciplinary professionals (Rodda & Carter, Citation2016). Clear evidence about the best practice approach to diagnosis is lacking. This raises concern as many dementia and memory clinics continue to employ routine procedures, screening measures and cognitive tests tailored to older patients that are often insufficient to identify the complexity of presentation in YOD and result in under-investigation with limited use of crucial supplementary investigations. Indeed, evidence suggests that under-investigation is particularly common in non-specialist settings (Eriksson et al., Citation2014). Providing individuals with an accurate diagnosis allows them and their families access to suitable treatments, support and research opportunities. Timely diagnosis and improved recognition were rated by those with YOD as the highest priority for service improvement, placing it above post-diagnostic support (Armari, Jarmolowicz, & Panegyres, Citation2013).
A UK-based study, called The Angela Project, has focused on developing guidance on best practice in diagnosis of dementia in younger adults. The Angela Project included an international Delphi study with secondary care clinical experts (O’Malley, Parkes, Stamou, et al., Citation2020a) to establish the key indicators for comprehensive assessment of dementia in this patient group. The resulting consensus created two standards, a minimum standard and gold standard, which have provided a template for assessing the UK clinical practice in the current study. A knowledge exchange event was also conducted with the participating NHS Trust clinical leads to understand further common gaps in enquiry.
Our objectives were to identify differences in compliance with the minimum and gold standard a) at and between sites b) with dementia subtypes and c) to investigate possible explanations for commonly missed items of enquiry and examination
Materials and methods
Study setting and data source
To undertake the audit, the platform UK-CRIS (UK-Clinical Record Interactive System) through the CRIS Network, was utilised. The data for the study was extracted using the CRIS application, which renders anonymised data from over two million electronic health records (EHR) for use for research and audit purposes (https://crisnetwork. co). The CRIS data have been extensively supplemented through natural language processing applications using Generalised Architecture for Text Engineering software which apply information extraction techniques allowing users to derive structured information from the text fields held in mental health records (Perera et al., 2016).This methodology was employed across the EHR from eight separate Trusts in England from both rural and urban locations.
Ethics The Angela Project was approved by the Health Research Authority in England and by the South Central Berkshire Research Ethics Committee (REC ref 17/SC/0296). At each UK-CRIS site, a governance process with the CRIS oversight committee took place, to review the project as a CRIS-specific project and to agree to participation.
Sample All patients aged 65 years or younger who had received a diagnosis of dementia were identified from eight NHS trusts between September 2018 and November 2019. The date of the first recorded diagnosis before the age of 65 served as the index date for the retrospective search for the quality indicators. Patient records were excluded if it was apparent that the person was diagnosed later than 5 years ago (before 2014), if an individual was diagnosed in another NHS Trust and had since moved, so diagnostic information was not present in the files and if diagnostic information was in an associated, attached letter that the research team were unable to access. Patient data were denoted by a unique and stable pseudonym, (BRC_ID), consisting of a randomly generated string of characters to exclude use of any personally identifiable information from the patient records. Each individual entry record also included a document BRC_ID. These IDs do not allow researchers to identify specific patients and cannot be linked to the patient’s NHS number or individual Trust ID.
Quality indicators
Information was extracted relating to thirty-one key indicators from text fields of CRIS EHR of 402 anonymised patients with a diagnosis of dementia under the age of 65. Demographic data including gender, age at diagnosis, dementia type and time since diagnosis were also collected. The thirty-one indicators, highlighting key components of the comprehensive assessment of dementia in young adults were derived from an international Delphi study with expert secondary care clinicians in the field of young onset dementia. The Delphi study resulted in two standards that experts deemed as critical and essential. The minimum standards represent red flag indicators that were rated by all experts in the Delphi study as being absolutely essential or very important to diagnosis. The gold standard consists of a more comprehensive list of indicators that were rated as very important or absolutely essential by at least 80% of experts in the Delphi study.
Upon review, four statements from the original minimum and gold standards were deemed unascertainable from the free text case notes and others which had commonality were combined into one statement as indicated in Appendix 2. Some exceptions were made to the original scoring schedule.
For some indicators an intermediate score of 0.5 was assigned as indicated below
ACE-III – if the clinician used another screening tool, such as the Montreal Cognitive Assessment (MoCA) or Rowland Universal Dementia Assessment Scale (RUDAS) and provided appropriate reasons for using it, this was scored as 1.
MRI as initial assessment – if there was a contra-indication to MRI e.g. metal implants/pacemaker obesity or claustrophobia, then this was scored as 0.5
For complete list of 31 indicators see results section
Table 4. Percentage compliance rates broken down by site and statement on the Minimum and Gold Standard.
Data extraction
The key indicators were scored as present (1) or absent (0) in the text record according to a final template ().
Table 1. Minimum and Gold Standards that have been transformed into indicators. Please see the table below for more details, key words, and scoring information:
Information about the quality indicators was extracted from the EHR, primarily from unstructured free text case notes. No access was available to correspondence or investigations reported elsewhere unless recorded in the clinical notes.
Data collection
Data collection took place directly through an on-site NHS device, and through the virtual desktop interface (VDI). The pilot phase of the audit took place between September 2018 and January 2019. During this pilot phase period the query and search terms were refined. Data collection from all eight sites took place between January 2019 and November 2019.
Stage 1
A Structured Query Language (SQL) script was inputted into the local SQL client of UK-CRIS to produce a list of anonymised identifier codes for the patient records that met our inclusion and exclusion criteria. The SQL output also provided demographic information from the anonymised patient records.
Stage 2
The web client of UK-CRIS interrogates the anonymised patient records using key text terms for each of the indicators which are automatically highlighted to aid identification (see for key terms). Only EHR records from patients referred to and diagnosed in memory or cognitive disorders clinics in mental health trusts were included in the audit, to ensure the findings reflected the usual Trust care pathway.
Stage 3
A scoring proforma containing the minimum and gold standard indicators was prepared. The authors (MOM, JC) manually read through the records and used the proforma to score whether each indicator was met. Records were read retrospectively from date of confirmed diagnosis to point of referral. Only information available on the UK-CRIS platform was used when conducting the audit.
Statistical analysis
IBM SPSS v26 software was used in all statistical analyses. The threshold for null hypothesis significance testing was taken as p = 0.05.
Sample size. The sample size calculation was based on the requirement to estimate the compliance rate for each standard to within ±5% (95% confidence intervals). As there was no a priori information relating to the expected compliance estimates, the most conservative value of 50% was taken. Observed compliance rates greater or smaller than 50% will have smaller confidence intervals.
Inter-rater reliability
Two raters independently extracted the data and scored the standards for the first 50 records examined. As the selected two raters constituted a fixed effect and they each rated all of the random selection of 50 records (random effect), a two-way, mixed effects Intraclass Correlation Coefficient (ICC(3,1) (Shrout & Fleiss, Citation1979) absolute agreement) was used to assess overall agreement. This showed good to excellent reliability for both the gold (ICC = 0.851 (95%CI 0.751-0.912) and minimum (ICC = 0.858 (95% CI 0.763-0.917) standards with the residuals evenly distributed above and below the line of equal scores. Agreement between the two raters for each of the 31 items was analysed using a weighted Kappa coefficient. The mean weighted Kappa scores for all 31 items was 0.77 (sd = 0.15) and the lowest percentage agreement was 92%, indicating good consistency in the scoring between the two raters. The remaining records were therefore scored by one of the raters.
Tests of normality
Kolmogorov-Smirnov tests of normality indicated strong evidence for non-normality for both compliance percentages for the minimum standard (D(403) = 0.128, p’<’.001), and the gold standard (D(403) = 0.063, p <.001), therefore non-parametric tests were used.
Analysis of variation in compliance across groups
Independent-samples median tests (k-groups) were performed to examine compliance with the minimum standard at each of the sites. If the omnibus test showed a statistically significant difference, then pairwise comparison between sites, adjusted for multiple comparisons (28 comparisons), were conducted using a Bonferroni correction. Multiple regression analysis was used to investigate associations between the compliance rates and age, gender, years since diagnosis and diagnosis group (AD (including mixed dementia), Vascular dementia, Dementia in Pick’s disease, Other).
Results
Characteristics of cohort
A total of 402 records from the eight sites met the inclusion criteria and were included in the audit. Appendix 3 highlights the number of records collected from each of the sites.
Descriptive demographics
Demographic variables collected included gender, age, numbers of years since diagnosis, time from referral to service to diagnosis and dementia subtype as indicated by clinician-assigned ICD codes (see and ).
Table 2. Descriptive demographics from the 402 audited records (across all sites).
Table 3. Number of days from referral to diagnosis (all sites).
Percentage compliance rates analysed by site and statement, including compliance for site for minimum standard (11 statements), the additional 20 statements required for Gold standard, and the complete Gold standard set (31 statements) were calculated (see ).
Diagnosis Subtypes: 18 different ICD-10 codes were identified by the SQL query and 14 different dementia subtypes (See appendix 1 for the breakdown). For the purpose of the analysis, diagnoses were group into one of four broad categories: Alzheimer’s disease (including mixed dementia), Vascular dementia, Dementia in Pick’s disease and ‘Other’
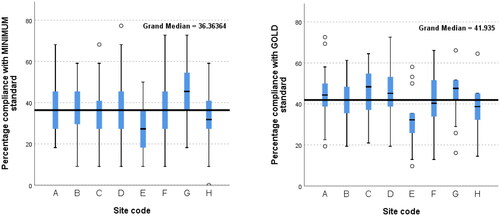
Variation in percentage compliance with minimum and gold standard between sites
Minimum standard: Independent-Samples Median tests showed that there were statistically significant differences (p<.05) between three pairs of sites: site E had lower Minimum Standard compliance than Site D (padj=.032, effect size r = 0.31, small) and Site G (padj=.001, r = 0.55, large), and Site C’s compliance was lower than Site G (padj=.016,r = 0.34, small) .
Gold standard: There were statistically significant differences between some sites; site E has lower median compliance percentage than all other sites (padj from <.001 to.036, effect sizes r = 0.58, large to r = 0.28, small) and there was also a statistically significant difference between the percentages for sites H and C, with C having the higher compliance (padj=.002, r = 0.38, medium). See for variation in percentage compliance with minimum and gold standard at sites.
Variation in percentage compliance for minimum and gold standard between dementia types
Minimum Standard: An Independent-Samples Median test was conducted which showed there were statistically significant differences in the percentage compliance between dementia types (test statistic = 9.09, df = 3, p=.028). Pairwise comparisons showed that there was a difference between those with Alzheimer’s disease and Dementia in Pick’s disease (padj=.043,effect size, r = 0.17, very small), with Pick’s disease being associated with higher compliance. There were no significant differences between the other dementia diagnoses. See for percentage compliance for minimum and gold standard across dementia types.
Figure 2. Variation in percentage compliance for minimum (left) and gold (right) standard across dementia types.
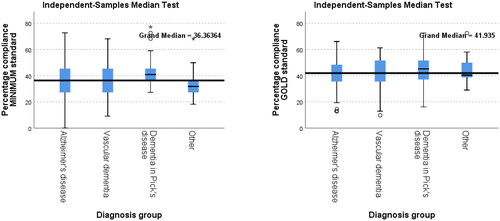
Gold Standard: There were no statistically significant differences between diagnostic groups and percentage compliance with the gold standard.
Associations between compliance rates and patient factors
As the Minimum standard compliance rate had been to vary between sites, a multi-level linear model, with site as the random, level 2 variable, was constructed to investigate associations between the compliance rates for the Minimum standard statements and age, gender, years since diagnosis and diagnosis group, clustered by site. Assumptions of multicollinearity, homoscedasticity and normality of residuals were tested and met. Only diagnosis group was a significant predictor (F(3,391.24)=4.126, p=.007). This confirms the results from the Independent-Samples Median test reported above.
This was repeated for the full Gold standard (31 items) which showed no associations with any of the predictor variables.
In summary, there were statistically significant compliance rates between the sites and there were also differences in the Minimum standard compliance rate between patients with different diagnoses, after age, gender and time since diagnosis had been accounted for. Gold standard compliance rates were not associated with any of these personal variables.
Percentage compliance with individual indicators
Percentage compliance rates analysed by site and statement, including compliance for site for minimum standard (11 statements), the additional 20 statements required for Gold standard, and the complete Gold standard set (31 statements) were calculated (). This clearly shows that the additional 20 statements in the Gold standard had consistently higher compliance rates for every site than the minimum set, hence the higher compliance for Gold compared to minimum overall.
The 31 indicators included in the Gold standard were ranked in order of percentage compliance across all sites and dementia types and are shown in .
Table 5. Percentage compliance for individual indicators of the Gold Standard across the whole dataset (402 records) ranked in order.
The results demonstrate wide variability in percentage compliance across the indicators regardless of diagnosis type or site with the top indicators yielding scores of over 90%. Low scoring indicators included assessment for neurological signs, preassessment counselling and ascertaining a history of learning disability. In some circumstances although there is clear agreement about the value of specific indicators e.g. structural imaging across all sites reaching 90% compliance, execution to an acceptable ‘expert consensus’ standard was less common.
Discussion
Quality of diagnosis and equity in access to specialists with expertise remains an issue for those with Young Onset Dementia (O’Malley, Parkes, Campbell, et al., Citation2020; Rabanal, Chatwin, Walker, O’Sullivan, & Williamson, Citation2018; Vernooij-Dassen, Citation2006). Misdiagnosis due to other causes, particularly psychiatric disorders are common because of complexity and heterogeneity in presenting symptoms (Vieira et al., Citation2013). Mitigation of these issues could be achieved by increased knowledge and rigorous and systematic approach to diagnosis (Millenaar et al., Citation2016; O’Malley et al., Citation2019; Sansoni et al., Citation2016). No research about current UK practice is available.
In order to understand current diagnostic practice for younger people with dementia in the UK memory services, compliance with expert-defined quality indicators (O’Malley, Parkes, Stamou, et al.) in an anonymised dataset of 402 patients with young onset dementia using the UK Clinical Research Interactive System (CRIS) across eight NHS trusts was investigated. This study is currently the largest to utilise the digital platform UK-CRIS and is a component of the largest UK study of young onset dementia. The study was carried out in mental health trusts as this is where the majority of young people with dementia are diagnosed (Stamou et al., Citation2020).
Percentage compliance rates were analysed by site and statement for a Minimum standard (11 statements, ranges 28–45%), the additional 20 statements required for Gold standard, ranges 33–52%), and the complete Gold standard set (31 statements, ranges 31–47%). This analysis shows that the additional 20 statements in the Gold standard had consistently higher compliance rates than the minimum set at every site, resulting in higher compliance for the Gold standard compared to Minimum standard overall.
In patients with a final diagnosis of Frontotemporal Dementia (ICD coding - Dementia in Pick’s Disease), percentage compliance with the minimum standard was higher than for Alzheimer’s disease (and no higher than for other diagnostic groups). Examination of the components of the minimum standard suggest that this may not be surprising since it contains two indicators that are arguably more specific to Frontotemporal Dementia (FTD) than other diagnoses; international criteria for FTD and a change in behaviour. There was no statistical difference in time to diagnosis from referral to site with diagnosis subtype.
Percentage compliance with the Gold Standard did not vary across diagnostic groups suggesting that this standard may be more useful as a clinical tool. Perhaps, not surprisingly, for assessments conducted in mental health trusts, items concerned with assessment of mental state, mood and risk were convincingly assessed within this standard, while assessment and/or recording of indicators requiring neurological examination for key signs was less common. Furthermore, discrepancies were apparent. For example, although conducting structural neuroimaging scored highly for all sites, performing this to a recognised standard such as an MRI ‘dementia protocol’ was rare.
The variable compliance rates across sites were evaluated further in a follow-up knowledge exchange session with representatives of the clinical teams whose notes informed the audit. The goal was to identify ‘on the ground’ experience and to understand further the barriers and facilitators to improving practice. Clinicians advised that use of a standard proforma in the clinics to guide enquiry was rare. One site indicated that a letter template sent to GPs acted as an aide memoire for recording key elements after the assessment. Clinical teams also identified that in cases where nurses were performing assessments, the proformas were relatively rudimentary and did not distinguish between YOD and LOD with regard to specific items of enquiry at a level of detail to reach the gold standard. With regard to some indicators, for example pre-assessment counselling, teams reported that often a scripted proforma was used to meet MSNAP (Memory Service National Accreditation Programme) standards rather than individually tailored counselling which takes account of age-specific needs.
In summary, initial analysis of anonymised data for patients with YOD using expert-defined quality indicators has provided a baseline about variation in the information that is currently recorded in EHR.
A major strength of our dataset is the comprehensive inclusion of the population of interest, across eight different NHS trusts. The analysed sample therefore encompasses differing care pathways and practice allowing highly generalisable results.
Furthermore, deriving structured information directly from the text fields held in mental health records allowed accurate representation of contemporaneous records. Keywords for our search query were aimed at identifying clinician-assigned constructs, rather than descriptions of experiences.
Limitations for the study included the level of detail within the notes which differed greatly between the sites. Whilst some sites followed usual clinical clerking, which included key queries to investigate and note during the initial and subsequent assessments, other sites summarised assessments concisely in a freehand manner. It should also be noted that the some of the consensus indicators required a level of subjectivity in assessment. For example, the indicator related to rapport was scored according to whether the term ‘rapport’ was used, or if the clinician’s language suggested that questions were directed more towards the person undergoing the assessment (rather than a family supporter) and if they described the personality of the person, suggesting that they attempted to get to know the patient as well as possible. Finally, the study includes records from Mental Health Trusts, so patients with YOD assessed in neurology centres/services, would not have been included and this limits generalisability of the findings. Ideally, capturing records from those assessed in neurology and specialist services would provide greater understanding of differences in patient initial complaints and profiles between mental health and neurology services.
In other fields of medicine, introduction of interventions such as aide memoire in addition to clinical education has been valuable in improving standards of good practice (Parwaiz, Perera, Creamer, Macdonald, & Hunter, Citation2017). The results obtained here, suggest that a template proforma, which contains the key indicators for comprehensive assessment of dementia in young adults according to a quality standard could help support less experienced clinicians to improve record keeping and reduce gaps in examination and enquiry.
Disclosure statement
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Author contribution
JC, JO and JP initiated, planned and co-ordinated the study for this paper. MOM and JC conducted the research, drafted and proof-read the paper and JP, JO, JLF and VS contributed to drafting, proof-reading and worked on the final draft of the paper
Data sharing statement
We the authors agree to sharing data from this work, upon reasonable request.
Acknowledgements
The authors wish to thank North East London NHS Foundation Trust, The Devon Partnership NHS Trust, Nottinghamshire Healthcare NHS Foundation Trust, Avon & Wiltshire Mental Health Partnership NHS Trust, West London NHS Trust, South West London & St George’s Mental Health NHS Trust – R&D Department. This study was supported by the UK Clinical Record Interactive Search (UK-CRIS) system funded by the National Institute for Health Research (NIHR) and the Medical Research Council, with the University of Oxford.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Armari, E., Jarmolowicz, A., & Panegyres, P. K. (2013). The needs of patients with early onset dementia. American Journal of Alzheimer’s Disease & Other Dementiasr, 28(1), 42–46. https://doi.org/10.1177/1533317512466690
- Draper, B., Cations, M., White, F., Trollor, J., Loy, C., Brodaty, H., Sachdev, P., Gonski, P., Demirkol, A., Cumming, R. G., & Withall, A. (2016). Time to diagnosis in young-onset dementia and its determinants: The INSPIRED study. International Journal of Geriatric Psychiatry, 31(11), 1217–1224. Novhttps://doi.org/10.1002/gps.4430
- Eriksson, H., Fereshtehnejad, S.-M., Falahati, F., Farahmand, B., Religa, D., & Eriksdotter, M. (2014). Differences in routine clinical practice between early and late onset Alzheimer’s disease: data from the Swedish Dementia Registry (SveDem). Journal of Alzheimer’s Disease : JAD, 41(2), 411–419., doi: 10.3233/JAD-132273J.
- Graff-Radford, J., Yong, K. X. X., Apostolova, L. G., Bouwman, F. H., Carrillo, M., Dickerson, B. C., Rabinovici, G. D., Schott, J. M., Jones, D. T., & Murray, M. E. (2021). New insights into atypical Alzheimer’s disease in the era of biomarkers. The Lancet Neurology, 20(3), 222–234. Mar https://doi.org/10.1016/S1474-4422(20)30440-3
- Hussey, J. S., & Butler, G. (2019). Delays in diagnosis for people with Young Onset Dementia. J Ment Health Aging, 3(1), 61–62.
- Koedam, E. L., Lauffer, V., van der Vlies, A. E., van der Flier, W. M., Scheltens, P., & Pijnenburg, Y. A. (2010). Early-versus late-onset Alzheimer’s disease: More than age alone. Journal of Alzheimer’s Disease, 19(4), 1401–1408. PMID: 20061618. https://doi.org/10.3233/JAD-2010-1337
- Konijnenberg, E., Fereshtehnejad, S. M., Ten Kate, M., Eriksdotter, M., Scheltens, P., Johannsen, P., Waldemar, G., & Visser, P. J. (2017). Early-onset dementia: Frequency, diagnostic procedures, and quality indicators in three European Tertiary Referral Centers. Alzheimer Disease and Associated Disorders, 31(2), 146–151. https://doi.org/10.1097/WAD.0000000000000152
- Kuruppu, D. K., & Matthews, B. R. (2013). Young-onset dementia. Seminars in Neurology, 33(4), 365–385. Sephttps://doi.org/10.1055/s-0033-1359320
- Millenaar, J. K., Bakker, C., Koopmans, R. T. C. M., Verhey, F. R. J., Kurz, A., & de Vugt, M. E. (2016). The care needs and experiences with the use of services of people with young-onset dementia and their caregivers: A systematic review. International Journal of Geriatric Psychiatry, 31(12), 1261–1276. https://doi.org/10.1002/gps.4502
- O’Malley, M., Parkes, J., Campbell, J., Stamou, V., LaFontaine, J., Oyebode, J. R., & Carter, J. (2020). Receiving a diagnosis of young onset dementia: Evidence-based statements to inform best practice. Dementia, 20(5), 1755-1771. https://doi.org/10.1177/1471301220969269
- O’Malley, M., Parkes, J., Stamou, V., LaFontaine, J., Oyebode, J., & Carter, J. (2019). Young-onset dementia: Scoping review of key pointers to diagnostic accuracy. BJPsych Open, 5(3), 1–9. https://doi.org/10.1192/bjo.2019.36
- O’Malley, M., Parkes, J., Stamou, V., LaFontaine, J., Oyebode, J., & Carter, J. (2020a). International consensus on quality indicators for comprehensive assessment of dementia in young adults using a modified e-Delphi approach. International Journal of Geriatric Psychiatry,35, 1309-1321. https://doi.org/10.1002/gps.5368
- Parwaiz, H., Perera, R., Creamer, J., Macdonald, H., & Hunter, I. (2017). Improving documentation in surgical operation notes. British Journal of Hospital Medicine, 78(2), 104–107. https://doi.org/10.12968/hmed.2017.78.2.104
- Perera, G., Broadbent, M., Callard, F., Chang, C. K., Downs, J., Dutta, R., Fernandes, A., Hayes, R. D., Henderson, M., Jackson, R., Jewell, A., Kadra, G., Little, R., Pritchard, M., Shetty, H., Tulloch, A., & Stewart, R. (2016). Cohort profile of the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Case Register: Current status and recent enhancement of an Electronic Mental Health Record-derived data resource. BMJ Open, 6(3), 1–22. https://doi.org/10.1136/bmjopen-2015-008721
- Rabanal, L. I., Chatwin, J., Walker, A., O’Sullivan, M., & Williamson, T. (2018). Understanding the needs and experiences of people with young onset dementia: A qualitative study. BMJ Open, 8(10), 1–9. https://doi.org/10.1136/bmjopen-2017-021166
- Rao, R. T., & Draper, B. (2018). Addressing alcohol-related dementia should involve better detection, not watchful waiting. The British Journal of Psychiatry : The Journal of Mental Science, 212(2), 67–68. Febhttps://doi.org/10.1192/bjp.2017.14 PMID: 29436326.
- Rodda, J., & Carter, J. E. (2016). A survey of UK services for younger people living with dementia. International Journal of Geriatric Psychiatry, 31(8), 957-9. https://doi.org/10.1002/gps.4402
- Salem, L. C., Andersen, B. B., Nielsen, T. R., Stokholm, J., Jørgensen, M. B., & Waldemar, G. (2014). Inadequate diagnostic evaluation in young patients registered with a diagnosis of dementia: A nationwide register-based study. Dementia and Geriatric Cognitive Disorders Extra, 4(1), 31–44. https://doi.org/10.1159/000358050
- Sansoni, J., Duncan, C., Grootemaat, P., Capell, J., Samsa, P., & Westera, a. (2016). Younger onset dementia: A review of the literature to inform service development. American Journal of Alzheimer’s Disease and Other Dementias, 31(8), 693–705. https://doi.org/10.1177/1533317515619481
- Shrout, P. E., & Fleiss, J. L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. https://doi.org/10.1037/0033-2909.86.2.420
- Stamou, V., La Fontaine, J., Gage, H., Jones, B., Williams, P., O’Malley, M., Parkes, J., Carter, J., & Oyebode, J. (2020). Services for people with young onset dementia: The ‘Angela’ project national UK survey of service use and satisfaction. International Journal of Geriatric Psychiatry,36(3), 411-422. https://doi.org/10.1002/gps.5437
- Underwood, J., & Winston, A. (2016). Guidelines for Evaluation and Management of Cognitive Disorders in HIV-Positive Individuals. Current HIV/AIDS Reports, 13(5), 235–240. https://doi.org/10.1007/s11904-016-0324-x
- Vernooij-Dassen, M., Derksen, E., Scheltens, P., & Moniz-Cook, E. (2006). Receiving a diagnosis of dementia: The experience over time. Dementia, 5(3), 397–410. https://doi.org/10.1177/1471301206067114
- Vieira, R. T., Caixeta, L., Machado, S., Cardoso Silva, A., Nardi, A. E., Arias-Carrión, O., & Giovanni Carta, M. (2013). Epidemiology of early-onset dementia: A review of the literature. Clinical Practice and Epidemiology in Mental Health: CP & EMH, 9(1), 88–95. https://doi.org/10.2174/1745017901309010088