Abstract
Objectives
To investigate the prevalence and prognostic significance of post-hip fracture depressive symptoms.
Methods
A naturalistic clinical cohort study. Data were collected on admission to hospital, geriatric assessment 4–6 months post-fracture and by telephone interview one-year post fracture. Depressive symptoms were assessed at the geriatric assessment using the 15-item Geriatric Depression Scale (GDS-15). Logistic regression analyses with multivariable models were conducted to examine the association of depressive symptoms with changes in mobility and living arrangements and Cox proportional hazards models for mortality between the geriatric assessment and one-year follow-up.
Results
Of the 1070 patients, 22% (n = 238) had mild and 6% (n = 67) moderate to severe depressive symptoms. Patients with depressive symptoms had poorer nutritional status at baseline, lower scores on the cognitive and physical performance tests and poorer functional abilities in the geriatric assessment than those without. No association was observed between depressive symptoms and any of the outcomes at one-year follow-up. Poor nutritional status and physical functioning remained significant prognostic indicators.
Conclusion
Post-hip fracture depressive symptoms are common and deserve attention during post-hip fracture recovery and rehabilitation. Nonetheless, depressive symptoms have no impact on the change in mobility or living arrangements or mortality. These latter outcomes are mainly explained by poor nutritional status and functioning.
Introduction
Hip fractures are the most common serious trauma in older people leading to disability, increased risk of institutionalization and death (Veronese & Maggi, Citation2018). Moreover, they are known to severely impair patients’ quality of life, have a negative effect on the lives of their families and increase the burden of caregivers (Alexiou et al., Citation2018). With rapid ageing of population worldwide, the number of hip fractures is expected to rise, challenging the health and social care systems of modern societies.
Recovery from hip fracture is often complicated by subjective symptoms, such as pain, cognitive impairment, fear of falling or depressive symptoms (Lenze et al., Citation2007; Oude Voshaar et al., Citation2006). The absence of a comprehensive global consensus regarding the definitions and variety of tools available for assessment hinders the perception of relationships between these conditions (Bennett & Thomas, Citation2014; Bingham et al., Citation2019; Holmes & House, Citation2000). Nevertheless, mental health status always affects the overall somatic condition. Neuropsychiatric symptoms have a high prevalence in hip fracture patients (Radinovic et al., Citation2014). In a study by Gialanella and colleagues, three out of four patients were reported to have such problems on admission. Depression was present in 45.5% of the patients (Gialanella et al., Citation2014). Another study by Feng and coworkers reported the prevalence of depressive symptoms to be up to 57.5% within 72 h of admission (Feng et al., Citation2010). In fact, depression has been repeatedly reported as the most common psychological condition in hip fracture rehabilitation (Atay et al., Citation2016; Holmes & House, Citation2000; Nightingale et al., Citation2001).
The relationship between depression and hip fractures has been studied several times, with mixed results. Depression has been associated individually with higher relative risk for falls than cognitive impairment or age itself (American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention, 2001; Pan et al., Citation2018; Wu et al., Citation2018). Most hip fracture patients do not regain their pre-fracture physical or mental status (Alexiou et al., Citation2018). A study by Demakakos and colleagues reported a reciprocal relationship between gait speed and depressive symptoms, each affecting the other (Demakakos et al., Citation2013). Since most hip fractures occur as a result of a fall (Parkkari et al., Citation1999), this common problem deserves closer attention. Post-hip fracture depressive symptoms often go unrecognized (Müller-Thomsen et al., Citation2002) although they have been associated with poorer functional performance (Atay et al., Citation2016; Cristancho et al., Citation2016; Rathbun et al., Citation2016) and are known to negatively affect both operative outcomes and post-operative quality of life (Iolascon et al., Citation2011; Langer et al., Citation2015; Maharlouei et al., Citation2019). It should be noted, however, that not all studies have found such relationships (Kelly-Pettersson et al., Citation2019; Lenze et al., Citation2007). Studies so far on the subject of hip fracture and depressive symptoms differ in many aspects, such as the tools used for assessment of depressive symptoms, timing of the assessments, follow-up-time and so on. Patients with cognitive impairment are often excluded.
Depression, cognitive impairment and dementia are related in a complex and bi-directional manner. These conditions are both common in older population and related through common risk factors, shared physiological pathways and similar clinical manifestations (Bennett & Thomas, Citation2014; Ganguli, Citation2009). Depression and cognitive decline, which often occur in combination, are in a key role in predicting poorer functional outcomes and quality of life after hip fracture (Givens et al., Citation2008; Lenze et al., Citation2004; Mossey et al., Citation1989), especially when acting together (Feng et al., Citation2010). Givens and co-workers reported a clear majority (59%) of hip fracture patients to have at least one cognitive or mood disorder (Givens et al., Citation2008). Both depression and cognitive impairment reduce participation in rehabilitation and are therefore likely to impair the functional outcomes (Lenze et al., Citation2004).
Consequently, understanding the effect of depressive symptoms on rehabilitation outcomes is complicated by considerable variation in study designs. There seem to be several clinical features that simultaneously influence the patients’ post-fracture physiological and psychological status, and subsequently, the rehabilitation outcomes. Previous studies fail to cover some of the clinical characteristics that may contribute to this process. Also, timing of the assessment of depressive symptoms may produce imprecise results.
In this real-life sample derived from a large cohort of hip fracture patients, we describe the prevalence and severity of depressive symptoms detected with the 15-item version of the Geriatric Depression Scale (GDS-15) in a comprehensive geriatric assessment (CGA) arranged 4–6 months after the fracture in an outpatient setting. In particular, we investigate the prognostic significance of depressive symptoms in changes in mobility and living arrangements and mortality in a one-year post-hip fracture follow-up, adjusted in the final multivariable analyses for a number of baseline factors and domains of the CGA, including nutritional status, cognition and physical performance.
Materials and methods
Study design
The study material was collected from a geographically defined area covering a total population of 200,000. All patients who sustained a hip fracture inside the referral area were treated at the same central hospital. In this hospital, a care pathway has been designed for hip fracture patients aged ≥65 years. This has been described in detail in earlier publications (Nuotio & Luukkaala, Citation2016; Pajulammi et al., Citation2017). During the perioperative phase, the patients are treated with orthogeriatric collaboration initiated in 2007 and constantly evolving and updated thereafter. After a median length of 6 days (interquartile range, IQR, 6–7 days) (Pajulammi et al., Citation2017) on the acute hospital ward, most of the patients are discharged to local health-care centres’ inpatient facilities in seven health care regions for postoperative rehabilitation.
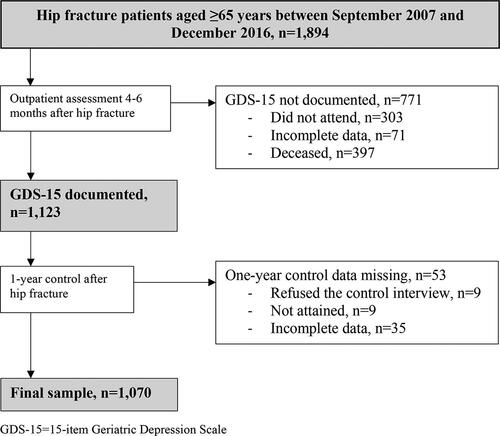
The data for the present study comprised consecutive patients aged 65 years and over sustaining their first hip fracture between September 2007 and December 2016. Pathological and periprosthetic fractures were excluded. For the purposes of this research, we included patients on whom documented data of the required variables were available ().
Data were collected at three time points:
Hospital admission
Baseline characteristics were collected on hospitalization by a geriatric nurse. Besides age and gender, comorbidity was registered according to the American Society of Anesthesiologist (ASA)-score (Haynes & Lawler, Citation1995) (ASA 1 = Normal healthy patient, ASA 2 = Mild systemic disease, ASA 3 = Severe systemic disease, ASA 4 = Severe systemic disease, constant threat to life, ASA 5 = Morbid patient, unlikely to survive) and categorized into two groups: 1–3 and 4–5. Known pre-fracture cognitive disorder diagnosed according to the national guidelines by a specialist in neurology or geriatrics was documented. Nutritional status was measured using the short form of the Mini-Nutritional Assessment (MNA-SF) (Kaiser et al., 2009; Rubenstein et al., Citation2001), which is a screening tool for nutritional status with solid clinical relevance and validation in older populations (Guigoz et al., Citation2006; Kaiser et al., 2009; Vellas et al., Citation2006). It contains six questions related to nutritional and health conditions, mobility and cognition. The MNA-SF result ranges from zero to fourteen. In our study, categorization was into three groups: normal (12–14), at risk of malnutrition (8–11), or malnourished (0–7). Mobility and living arrangements were assessed by the geriatric nurse together with the patient, the next of kin or caregiver, or a nurse in a care home. Mobility was categorized as independent or non-independent according to assistance needed. Needing any personal assistance in moving either outside and/or inside was interpreted as non-independent mobility. Living arrangements were categorized as living in own home without organized home care or in assisted living arrangements or institution providing 24-hour care. Again, needing any support was counted as non-independent living arrangements.
Outpatient assessment 4–6 months after the hip fracture
A comprehensive geriatric assessment was carried out at the geriatric outpatient clinic. All patients were invited to this appointment regardless of age, health status or living arrangements. A geriatric nurse conducted a telephone interview preceding the outpatient assessment to document current mobility and living arrangements. Assessment and categorization of these were accomplished as mentioned above. To assess depressive symptoms, we used the GDS-15 developed by Yesavage and Sheikh (Citation1986), which has since been validated as both a sensitive and a specific screening tool for depressive symptoms in geriatric settings. The assessment was carried out at the outpatient assessment. The short version of GDS-15 covers dimensions related to self-esteem, stressful thoughts, positive attitudes to life and judgements. It consists of 15 questions, all answered yes or no, giving a total score from 0 to 15. Patients with a score of 6 or above are categorized as depressed. For the purposes of the present study, mild depressive symptoms were defined as scoring 6–9 points out of 15, while moderate to severe depressive symptoms were defined as scoring at least 10 of the 15 (Alden et al., Citation1989; Friedman et al., Citation2005).
For the purposes of this study, data collected from the outpatient assessment also included Mini-Mental State examination (MMSE) to assess cognition. Basic and Instrumental Activities of Daily Living (BADL and IADL) scores according to Katz et al. (Citation1963) and Lawton and Brody (Citation1969) were registered to illustrate functional capability. The BADL and IADL forms were sent to the patients to be completed by them or with help from the next of kin or caregiver prior to the appointment at the outpatient assessment. If not completed beforehand, the forms were completed at the geriatric clinic. The MMSE test was carried out by an experienced geriatric nurse of the outpatient clinic. Physiotherapists’ examinations preceded the clinical assessment. Here, data on the Timed Up and Go (TUG) test (Beauchet et al., Citation2011) and the Elderly Mobility Scale (EMS) (Prosser & Canby, Citation1997) were included. The categorization of the cognitive, functional and physical performance according to severity of depressive symptoms is described in .
Table 1. Distribution of baseline characteristics and domains of the outpatient assessment according to severity of depressive symptoms at the follow-up visit 4-6 months after hip fracture (n = 1070).
One-year follow-up interview
The follow-up data were collected in a telephone interview by the geriatric nurse. The information was obtained from the patient and, if necessary, with the support of a caregiver, next of kin or staff of the care facility. Again, mobility and living arrangements were elicited in the same way as at baseline and before the outpatient appointment. Changes in mobility and living arrangements from the outpatient assessment to one-year follow-up were defined as more deteriorated versus same or better mobility level and more supported versus same or less supported living arrangements respectively.
Information on mortality was obtained from the Population Register Center and the electronic patient files. The Population Register Center is a national institution which holds up-to-date information on dates of deaths. These are automatically updated to electronic medical records.
A cross-tabulation of the baseline variables and the outpatient control domains according to the depressive symptoms classified by the GDS-15 was executed. The statistical differences between depressive symptoms groups were tested with Pearson’s χ2 test or Fisher’s exact test for the categorical variables. Logistic regression analyses with unadjusted, age- and gender-adjusted and multivariable-adjusted models were conducted to examine the association of mild and moderate to severe depressive symptoms with deterioration in mobility and need for more supported living arrangements from the outpatient assessment to one-year post-hip fracture (). Mortality was likewise analysed by Cox proportional hazard regression model. Model 1 was adjusted for age, gender and baseline mobility and living arrangements. Model 2 was further adjusted for ASA, MMSE, TUG, EMS, BADL and IADL. Results were shown as odds ratios (OR) or hazard ratios (HR) with 95% confidence intervals (CI). IBM SPSS Statistics version 26.0 for Windows software (SPSS Inc. Chicago, IL) was used for statistical analyses. p values under 0.05 were considered statistically significant.
Table 2. The effect of depressive symptoms according to Geriatric Depressive scale (GDS-15) on changes in mobility and living arrangements and mortality from 4 months to one-year follow-up.
The data collection commenced as a part of a development project. The original study design was reviewed and approved in the meeting of the Ethics Committee of the Hospital District of Southern Ostrobothnia on 1st November 2007. All participants or their representatives (legal guardian or next of kin) gave written consent to participate the study.
Results
The flow-chart of the study population is shown in . Patients with documented GDS-15 and available follow-up data were included. A total of 1070 patients fulfilled the inclusion criteria and formed the final sample. Of these 22% (n = 238) were evaluated to have mild depressive symptoms, while 6% (n = 67) were evaluated to have moderate to severe depressive symptoms.
The distribution of the baseline variables and domains of the outpatient assessment 4–6 months post-hip fracture is shown in . There were no significant differences in the distribution of gender or ASA score in patients with or without depressive symptoms but patients with depressive symptoms were more likely to be older, to have a pre-fracture diagnosis of cognitive disorder, poor nutritional status, non-independent mobility level or more supported living arrangements compared to the patients without depressive symptoms. Patients with depressive symptoms were also significantly more likely to have more decline in mobility from baseline to outpatient assessment than patients with no depressive symptoms. No statistically significant difference was observed between patients with or without depressive symptoms in moving to a more supported living accommodation from the time of the fracture to the outpatient assessment.
Of the 1070 patients, 45 (4%) had died between the outpatient assessment and the one-year post-hip fracture follow-up. Within this time frame, mobility had declined in 129 (13%) of the remaining 1018 patients on whom this information was documented. Living arrangements were more supported in 124 (12%) patients of the 1012 patients from whom this information was available.
In the unadjusted logistic regression analysis, neither mild nor moderate to severe depressive symptoms showed any significant association with decline in mobility level from the outpatient assessment to one-year post-hip fracture (OR 1.35; 95% CI 0.88–2.08 and OR 1.25; 95% CI 0.60–2.63, respectively). No associations were observed in the further adjusted models (). Depressive symptoms were not significantly associated with moving to more supported living accommodation in any of the analyses. Neither were mild or moderate to severe depressive symptoms associated with one-year mortality.
Characteristics that showed statistically significant association with change in mobility or living arrangements in the final multivariable analysis were old age (90 years or more: OR 2.49, 95% CI 1.31–4.76), poor physical functioning (PADL 0–5: OR 1.77, 95% CI 1.03–3.05 and poor nutritional status (MNA 0–7: OR 2.10, 95% CI 1.07–4.14). Markedly abnormal TUG-test score (OR 9.06, 95% CI 1.99–41.18) and poor nutritional status (MNA 0–7: OR 3.62, 95% CI 1.42–9.20) were associated with mortality.
Discussion
This study demonstrated that almost one third of the hip fracture patients suffered from depressive symptoms at post-hip fracture assessment. However, moderate to severe depressive symptoms were detected in less than 10% of the patients. Patients with depressive symptoms were significantly older and they were more likely to have a known pre-fracture cognitive disorder, poorer nutritional status, poorer mobility and more supported living arrangements at baseline compared to patients without depressive symptoms. They were also more likely to score lower on almost all physical, cognitive and functional parameters documented at the outpatient assessment. However, the effect of the depressive symptoms on the one-year post-hip fracture outcomes appeared to be insignificant as neither mild nor moderate to severe depressive symptoms as measured by the GDS-15 were significantly associated with deterioration in mobility, moving to more supported living arrangements or mortality in any of the models.
In previous studies, the prevalence of post-hip fracture depressive symptoms has been reported to vary from 9 to 47% (Heidari et al., Citation2020; Holmes & House, Citation2000; Iolascon et al., Citation2011). In studies using the GDS-15, the prevalence has been similar to the figures reported in the present study, ranging from 24 to 46% (Morghen et al., Citation2011; Oude Voshaar et al., Citation2007).
In our earlier study, we reported an association between poor nutritional status measured by the MNA-SF with most of the domains of the post-hip fracture CGA, including depressive symptoms (Helminen et al., Citation2017). In that study, 49% of the patients had poor nutritional status according to the MNA-SF at the time of the hip fracture and 35% of the patients had developed poor nutritional status during follow-up. It is noteworthy that in the present study, while depressive symptoms had no significant effect, poor nutritional status and impaired physical performance remained independent prognostic factors for the outcomes in the final multivariable analyses.
Post-hip fracture depressive symptoms have been associated with impaired mobility, need for more assisted living arrangements and increased mortality (Cullum et al., Citation2008; Lenze et al., Citation2004; Morghen et al., Citation2011; Nightingale et al., Citation2001) but no such finding were apparent in our study. On the contrary, the absence of an association between depressive symptoms and rehabilitation outcomes has also been observed (Gialanella et al., Citation2018; Kelly-Pettersson et al., Citation2019; Oude Voshaar et al., Citation2006).
Our findings emphasize the multifactorial and syndromic nature of depressive symptoms in older hip fracture patients and in older people in general. New traumatic disability may result in the onset of depressive symptoms which may subsequently impair the recovery process (Givens et al., Citation2008). High preoperative comorbidity and common comorbidities of older patients related to hospitalization (cognitive impairments, delirium and depressive mood) have been studied separately with each in association with adverse rehabilitation outcomes (Dubljanin Raspopović et al., Citation2014; Gialanella et al., Citation2018; Givens et al., Citation2008; Lenze et al., Citation2007). It is understandable that the traumatic injury, pain, sudden loss of autonomy and the need for assistance in daily activities can be mentally demanding. Loss of confidence and self-efficacy together with potentially long rehabilitation in health care facilities away from the immediate family most likely influenced these study results. However, depressive symptoms themselves may not be the mediating factor for poor outcomes. As suggested by M. Chang and coworkers, disability may have a greater impact on depressive symptoms rather than depressive symptoms having an effect on disability (Chang et al., Citation2009). In fact, the results of the present study support this hypothesis as patients with pre-fracture mobility impairment were more likely to report depressive symptoms at the outpatient appointment. Moreover, depressive symptoms were significantly more common in patients with decline in mobility between the time of the index fracture and the outpatient assessment.
Some studies assess depressive symptoms during the acute phase of the injury, i.e. on admission or immediately after the operative care (Charles-Lozoya et al., Citation2019; Cristancho et al., Citation2016; Gialanella et al., Citation2014; Kelly-Pettersson et al., Citation2019; Lenze et al., Citation2004). Recent trauma, pain, the hospital environment, medications and symptoms of delirium may affect the results at this time point. The follow-up time of depressive symptoms after the initial assessment may also be short (Maharlouei et al., Citation2019; Rathbun et al., Citation2019), which may increase the possibility of confounding factors during the rehabilitation process. It should be noted that depressive symptoms have been reported to affect outcomes for up to two years after a hip fracture (Nightingale et al., Citation2001). A follow-up study by Chang and co-workers found that the majority of the depressive symptoms arose during the first 200 days post-fracture (Chang et al., Citation2014). Our clinical assessment target frame of 4–6 months post-hip fracture was based on earlier clinical evidence. Studies suggest that post-hip fracture rehabilitation improves a patient’s condition most significantly during the first 2 to 6 months after the incident (Fredman et al., Citation2006; Hongisto et al., Citation2016; Young et al., Citation2010). A time frame of 4–6 months was also believed to be beyond the confounding influence of the trauma care and hospitalization thus allowing an undisturbed opportunity for cognitive assessment. The scope was to maximize the value of the comprehensive assessment in favour of the rehabilitation process and the patients’ overall well-being.
The relationship between dementia and depression is still controversial since depression has been reported to be an independent risk factor for dementia, a prodromal symptom of dementia, a consequence of cognitive impairment or a common comorbidity due to many shared factors in ageing population (Bennett & Thomas, Citation2014). Interaction between these conditions requires more research. Interestingly, in our study, the significance of cognitive impairment appeared to decrease when the analyses were adjusted for other clinical parameters. This also illustrates the diversity and complexity of hip fracture recovery in a geriatric setting: patients with already impaired compensatory physiological mechanisms are faced with a significant trauma, hospitalization, surgery and medications. Multiple factors interact with one another during the rehabilitation process reducing the importance of a single attribute. Moreover, the older patient population is a heterogenous group with markedly different individual strengths and resources to recover and regain functional and physical capabilities.
The strength of our study is a large sample derived from a major clinical prospective cohort of older hip fracture patients. Our systematic approach and measurement of depressive symptoms and other domains of the geriatric assessment using standardized instruments are also obvious strengths of this study. We included all patients, i.e. we did not exclude patients due to living arrangements, medical history, current health status, cognitive or physical functioning. Therefore, the results represent well the actual effect of depressive symptoms on the chosen outcomes. Another strength was that we could include a number of relevant baseline factors and domains of the outpatient assessment, in particular those related to cognitive and physical functioning, in the final multivariable analyses. Finally, the outcomes measures used in our study were extremely relevant with regard to examining hip fracture recovery in terms of rehabilitation outcomes.
A number of limitations of the study deserve attention. First, we only focused on depressive symptoms occurring post-hip fracture. Pre-fracture depressive symptoms were not documented, nor were the depressive symptoms in the acute phase. Evaluating depressive symptoms during hospitalization is questionable due to the several potentially confounding factors mentioned earlier. Second, depressive symptoms were assessed only at one time-point after hip fracture, thus, the potential changes in depressive symptoms and above all the effect of the change on outcomes could not be examined. A study by Magaziner and colleagues found that recovery from a hip fracture progresses in different patterns depending on the functional domain assessed (Magaziner et al., Citation2000). Depressive symptoms are most prominent in the acute phase but decline significantly during the first year after hip fracture. Third, based on our previous observations (Nuotio & Luukkaala, Citation2016), we assume that the non-attendees at the outpatient assessment were more likely to be more cognitively impaired than the attendees and more likely to be living in assisted living arrangements or an institution. Due to the known association between depressive symptoms and cognitive and physical functioning, this could bias our result in a direction of underreporting depressive symptoms. Finally, the reliability of the GDS-15 evaluation in patients with more severe cognitive decline may be jeopardized (Conradsson et al., Citation2013). Nevertheless, Conradsson and colleagues reported that the GDS-15 can be used reliably even on very old patients with MMSE score 10 and over. According to our own clinical experience, patients on whom the MMSE test can be carried out are indeed able to answer the questions of the GDS screening to a satisfactory extent unless suffering from significant dysphasia.
Conclusion
Post-hip fracture depressive symptoms are common but mostly mild. Patients with depressive symptoms are likely to have poorer nutritional status, less independent mobility, and more supported living arrangements at baseline and to score lower on tests of physical performance, cognition and functioning in clinical post-fracture assessment. Moreover, the mobility level of the patients reporting depressive symptoms post-fracture is likely to have deteriorated from the time of the fracture to the 4–6 months follow-up. However, there seems to be no effect whatsoever of post-hip fracture depressive symptoms on rehabilitation outcomes of change in mobility or living arrangements or mortality when the follow-up reaches one year. Interestingly, cognitive impairment was likewise not independently associated with the outcomes. By contrast, poor pre-fracture nutritional status, poor physical performance and problems with activities of daily living remained the most significant prognostic indicators of the outcomes. Nevertheless, the cumulative effect of multiple comorbidities is especially dangerous for older patients due to the depleted functional reserves. Recovery from hip fracture demands significant physical stamina, the capability to commit to the instructions of the rehabilitation process and motivation for improvement, and depression and cognitive decline interfere in all of these (Givens et al., Citation2008). Therefore, we believe that post-hip fracture rehabilitation should include both physical exercise as well as psychological support. Also, cognitive and nutritional status as well as other comorbid conditions need to be addressed throughout comprehensive hip fracture care.
Acknowledgements
Ms. Kaisu Haanpää, RN, is gratefully acknowledged for her expert collection and storage of the data.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
The data used in the present study are a part of a local quality register and therefore not publicly available. Further enquiries can be directed to the principal investigator (MSN, [email protected]).
Additional information
Funding
References
- Alden, D., Austin, C., & Sturgeon, R. (1989). A correlation between the Geriatric Depression Scale long and short forms. Journal of Gerontology, 44(4), P124–5. https://doi.org/10.1093/geronj/44.4.p124
- Alexiou, K. I., Roushias, A., Varitimidis, S. E., & Malizos, K. N. (2018). Quality of life and psychological consequences in elderly patients after a hip fracture: A review. Clinical Interventions in Aging, 13, 143–150. https://doi.org/10.2147/CIA.S150067
- Atay, I. M., Aslan, A., Burç, H., Demirci, D., & Atay, T. (2016). Is depression associated with functional recovery after hip fracture in the elderly? Journal of Orthopaedics, 13(2), 115–118. https://doi.org/10.1016/j.jor.2015.02.001
- Beauchet, O., Fantino, B., Allali, G., Muir, S. W., & Annweiler, C. (2011). Timed up and go test and risk of falls in older adults. Journal of Nutrition, Health and Aging, 15(10), 6–11.
- Bennett, S., & Thomas, A. J. (2014). Depression and dementia: Cause, consequence or coincidence? Maturitas, 79(2), 184–190. https://doi.org/10.1016/j.maturitas.2014.05.009
- Bingham, K. S., Flint, A. J., & Mulsant, B. H. (2019). Management of late-life depression in the context of cognitive impairment: A review of the recent literature. Current Psychiatry Reports, 21(8). https://doi.org/10.1007/s11920-019-1047-7.
- Chang, C. Y., Chen, W. L., Liou, Y. F., Ke, C. C., Lee, H. C., Huang, H. L., Ciou, L. P., Chou, C. C., Yang, M. C., Ho, S. Y., & Lin, Y. R. (2014). Increased risk of major depression in the three years following a femoral neck fracture-a national population-based follow-up study. PLoS One, 9(3), 1–8. https://doi.org/10.1371/journal.pone.0089867
- Chang, M., Abel, B., Coppin, A. K., Van Der Linden, M., Ferrucci, L., Fried, L., & Guralnik, J. M. (2009). An association between incident disability and depressive symptoms over 3 years of follow-up among older women: The Women’s Health and Aging Study. Aging Clinical and Experimental Research, 21(2), 191–197. https://doi.org/10.1007/BF03325228
- Charles-Lozoya, S., Cobos-Aguilar, H., Barba-Gutiérrez, E., Brizuela-Ventura, J. M., Chávez-Valenzuela, S., Hernández, A. G., & Montes, J. C. T. (2019). Depression and geriatric assessment in older people admitted for hip fracture. Revista Medica de Chile, 147(8), 1005–1012. https://doi.org/10.4067/S0034-98872019000801005
- Conradsson, M., Rosendahla, E., Littbranda, H., Gustafson, Y., Olofsson, B., & Lövheim, H. (2013). Usefulness of the Geriatric Depression Scale 15-item version among very old people with and without cognitive impairment. Aging and Mental Health, 17(5), 638–645. https://doi.org/10.1080/13607863.2012.758231
- Cristancho, P., Lenze, E. J., Avidan, M. S., Rawson, K. S., & Louis, S. (2016). Trajectories of depressive symptoms after hip fracture. Psychological Medicine, 46(7), 1413–1425. https://doi.org/10.1017/S0033291715002974.Trajectories
- Cullum, S., Metcalfe, C., Todd, C., & Brayne, C. (2008). Does depression predict adverse outcomes for older medical inpatients? A prospective cohort study of individuals screened for a trial. Age and Ageing, 37(6), 690–695. https://doi.org/10.1093/ageing/afn193
- Demakakos, P., Cooper, R., Hamer, M., de Oliveira, C., Hardy, R., & Breeze, E. (2013). The bidirectional association between depressive symptoms and gait speed: Evidence from the English Longitudinal Study of Ageing (ELSA). PLoS One, 8(7), 14–18. https://doi.org/10.1371/journal.pone.0068632
- Dubljanin Raspopović, E., Marić, N., Nedeljković, U., Ilić, N., Tomanović Vujadinović, S., & Bumbaširević, M. (2014). Do depressive symptoms on hospital admission impact early functional outcome in elderly patients with hip fracture? Psychogeriatrics: The Official Journal of the Japanese Psychogeriatric Society, 14(2), 118–123. https://doi.org/10.1111/psyg.12049
- Feng, L., Scherer, S. C., Tan, B. Y., Chan, G., Fong, N. P., & Ng, T. P. (2010). Comorbid cognitive impairment and depression is a significant predictor of poor outcomes in hip fracture rehabilitation. International Psychogeriatrics, 22(2), 246–253. https://doi.org/10.1017/S1041610209991487
- Fredman, L., Hawkes, W. G., Black, S., Bertrand, R. M., & Magaziner, J. (2006). Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. Journal of the American Geriatrics Society, 54(7), 1074–1081. https://doi.org/10.1111/j.1532-5415.2006.00786.x
- Friedman, B., Heisel, M. J., & Delavan, R. L. (2005). Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. Journal of the American Geriatrics Society, 53(9), 1570–1576. https://doi.org/10.1111/j.1532-5415.2005.53461.x
- Ganguli, M. (2009). Depression, cognitive impairment and dementia: Why should clinicians care about the web of causation?. Indian Journal of Psychiatry, 51(Suppl 1), S29–S34. http://www.ncbi.nlm.nih.gov/pubmed/21416013%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3038544
- Gialanella, B., Prometti, P., Monguzzi, V., & Ferlucci, C. (2014). Neuropsychiatric symptoms and rehabilitation outcomes in patients with hip fracture. American Journal of Physical Medicine & Rehabilitation, 93(7), 562–569. https://doi.org/10.1097/PHM.0000000000000062
- Gialanella, B., Prometti, P., Monguzzi, V., Ferlucci, C., Baiardi, P., & Comini, L. (2018). Determinants of functional outcome in hip fracture: The role of comorbidity. Aging Clinical and Experimental Research, 30(6), 643–650. https://doi.org/10.1007/s40520-017-0812-x
- Givens, J., Sanft, T., & Marcantonio, E. (2008). Functional recovery after hip fracture: The combined effects of depressive symptoms, cognitive impairment, and delirium. Journal of the American Geriatrics Society, 56(6), 1075–1079. https://doi.org/10.1111/j.1532-5415.2008.01711.x
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. (2001). Guideline for the prevention of falls in older persons. Journal of the American Geriatrics Society, 49(5), 664–672. https://doi.org/10.1046/j.1532-5415.2001.49115.x
- Guigoz, Y., Jensen, G., Thomas, D., & Vellas, B. (2006). The Mini Nutritional Assessment (MNA®) review of the literature - What does it tell us? The Journal of Nutrition, Health & Aging, 10(6), 466–485.
- Haynes, S. R., & Lawler, P. G. P. (1995). An assessment of the consistency of ASA physical status classification allocation. Anaesthesia, 50(3), 195–199. https://doi.org/10.1111/j.1365-2044.1995.tb04554.x
- Heidari, M. E., Naghibi Irvani, S. S., Dalvand, P., Khadem, M., Eskandari, F., Torabi, F., & Shahsavari, H. (2020). Prevalence of depression in older people with hip fracture: A systematic review and meta-analysis. International Journal of Orthopaedic and Trauma Nursing, 40, 100813. https://doi.org/10.1016/j.ijotn.2020.100813
- Helminen, H., Luukkaala, T., Saarnio, J., & Nuotio, M. S. (2017). Changes in nutritional status and associated factors in a geriatric post-hip fracture assessment. European Geriatric Medicine, 8(2), 134–139. https://doi.org/10.1016/j.eurger.2017.02.002
- Holmes, J. D., & House, A. O. (2000). Psychiatric illness in hip fracture. Age and Ageing, 29(6), 537–546. https://doi.org/10.1093/ageing/29.6.537
- Hongisto, M. T., Nuotio, M., Luukkaala, T., Väistö, O., & Pihlajamäki, H. K. (2016). Does cognitive/physical screening in an outpatient setting predict institutionalization after hip fracture? BMC Musculoskeletal Disorders, 17(1), 1–11. https://doi.org/10.1186/s12891-016-1272-8
- Iolascon, G., Cervone, M., Gimigliano, R., Di Pietro, G., & Gimigliano, F. (2011). Neuropsychiatric disorders in hip fracture. Clinical Cases in Mineral and Bone Metabolism: The Official Journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases, 8(3), 49–53.
- Kaiser, M. J., Bauer, J. M., Ramsch, C., Uter, W., Guigoz, Y., Cederholm, T., Thomas, D. R., Anthony, P., Charlton, K. E., Maggio, M., Tsai, A. C., Grathwohl, D., Vellas, B., Sieber, C. C.; MNA-International Group. (2009). Validation of the Mini Nutritional Assessment Short-Form (MNA-SF): A practical tool for identification of nutritional status. The Journal of Nutrition, Health & Aging, 13(9), 782–788. https://doi.org/10.1007/s12603-009-0214-7
- Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A., & Jaffe, M. W. (1963). Studies of illness in the aged. The Index of ADL: A standardized measure of biological and psychosocial functioning. JAMA, 185, 914–919.
- Kelly-Pettersson, P., Samuelsson, B., Unbeck, M., Muren, O., Magnéli, M., Gordon, M., Stark, A., & Sköldenberg, O. (2019). The influence of depression on patient-reported outcomes for hip-fracture patients 1 year after surgery: A prospective cohort study. Aging Clinical and Experimental Research, 32, 247–255. https://doi.org/10.1007/s40520-019-01207-5.
- Langer, J. K., Weisman, J. S., Rodebaugh, T. L., Binder, E. F., & Lenze, E. J. (2015). Short-term affective recovery from hip fracture prospectively predicts depression and physical functioning. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 34(1), 30–39. https://doi.org/10.1037/hea0000111.Short-Term
- Lawton, M. P., & Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3), 179–186. https://doi.org/10.1093/geront/9.3_Part_1.179
- Lenze, E. J., Munin, M. C., Dew, M. A., Rogers, J. C., Seligman, K., Mulsant, B. H., & Reynolds, C. F. (2004). Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. International Journal of Geriatric Psychiatry, 19(5), 472–478. https://doi.org/10.1002/gps.1116
- Lenze, E. J., Skidmore, E. R., Dew, M. A., Butters, M. A., Rogers, J. C., Begley, A., Reynolds, C. F., & Munin, M. C. (2007). Does depression, apathy or cognitive impairment reduce the benefit of inpatient rehabilitation facilities for elderly hip fracture patients? General Hospital Psychiatry, 29(2), 141–146. https://doi.org/10.1016/j.genhosppsych.2007.01.001
- Magaziner, J., Hawkes, W., Hebel, J. R., Zimmerman, S. I., Fox, K. M., Dolan, M., Felsenthal, G., & Kenzora, J. (2000). Recovery from hip fracture in eight areas of function. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 55(9), M498–M1991. https://doi.org/10.1093/gerona/55.9.m498
- Maharlouei, N., Jafarzadeh, F., & Lankarani, K. B. (2019). Factors affecting recovery during the first 6 months after hip fracture, using the decision tree model. Archives of Osteoporosis, 14(1), 61–69. https://doi.org/10.1007/s11657-019-0611-4
- Morghen, S., Bellelli, G., Manuele, S., Guerini, F., Frisoni, G., & Trabucchi, M. (2011). Moderate to severe depressive symptoms and rehabilitation outcome in older adults with hip fracture. International Journal of Geriatric Psychiatry, 26(11), 1136–1143. https://doi.org/10.1002/gps.2651
- Mossey, J. M., Mutran, E., Knott, K., & Craik, R. (1989). Determinants of recovery 12 months after hip fracture: The importance of psychosocial factors. American Journal of Public Health, 79(3), 279–286. https://doi.org/10.2105/ajph.79.3.279
- Müller-Thomsen, T., Mittermeier, O., & Ganzer, S. (2002). Unrecognised and untreated depression in geriatric patients with hip fractures. International Journal of Geriatric Psychiatry, 17(7), 683–684. https://doi.org/10.1002/gps.661
- Nightingale, S., Holmes, J., Mason, J., & House, A. (2001). Psychiatric illness and mortality after hip fracture. Lancet, 357(9264), 1264–1265. https://doi.org/10.1016/S0140-6736(00)04421-4
- Nuotio, M., & Luukkaala, T. (2016). Factors associated with changes in mobility and living arrangements in a comprehensive geriatric outpatient assessment after hip fracture. Disability and Rehabilitation, 38(12), 1125–1133.
- Oude Voshaar, R. C., Banerjee, S., Horan, M., Baldwin, R., Pendleton, N., Proctor, R., Tarrier, N., Woodward, Y., & Burns, A. (2006). Fear of falling more important than pain and depression for functional recovery after surgery for hip fracture in older people. Psychological Medicine, 36(11), 1635–1645. https://doi.org/10.1017/S0033291706008270
- Oude Voshaar, R. C., Banerjee, S., Horan, M., Pendelton, N., Tarrier, N., & Burns, A. (2007). Predictors of Incident Depression After Hip Fracture Surgery. American Journal of Geriatric Psychiatry, 15(9), 807–814.
- Pajulammi, H. M., Pihlajamäki, H. K., Luukkaala, T. H., Jousmäki, J. J., Jokipii, P. H., & Nuotio, M. S. (2017). The effect of an in-hospital comprehensive geriatric assessment on short-term mortality during Orthogeriatric Hip Fracture Program—Which patients benefit the most? Geriatric Orthopaedic Surgery & Rehabilitation, 8(4), 183–191. https://doi.org/10.1177/2151458517716516
- Pan, C. C., Hu, L. Y., Lu, T., Tu, M. S., Shen, C. C., & Chen, Z. J. (2018). Risk of hip fractures in patients with depressive disorders: A nationwide, population-based, retrospective, cohort study. PLoS One, 13(4), 1–12. https://doi.org/10.1371/journal.pone.0194961
- Parkkari, J., Kannus, P., Palvanen, M., Natri, A., Vainio, J., Aho, H., Vuori, I., & Ja, M. (1999). Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: A prospective controlled hip fracture study with 206 consecutive patients. Calcified Tissue International, 65, 183–187. https://doi.org/10.1007/s002239900679
- Prosser, L., & Canby, A. (1997). Further validation of the Elderly Mobility Scale for measurement of mobility of hospitalized elderly people. Clinical Rehabilitation, 11(4), 338–343. https://doi.org/10.1177/026921559701100412
- Radinovic, K. S., Markovic-Denic, L., Dubljanin-Raspopovic, E., Marinkovic, J., Jovanovic, L. B., & Bumbasirevic, V. (2014). Effect of the overlap syndrome of depressive symptoms and delirium on outcomes in elderly adults with hip fracture: A prospective cohort study. Journal of the American Geriatrics Society, 62(9), 1640–1648. https://doi.org/10.1111/jgs.12992
- Rathbun, A. M., Shardell, M. D., Stuart, E. A., Gruber-Baldini, A. L., Orwig, D., Ostir, G. V., Hicks, G. E., Hochberg, M. C., & Magaziner, J. (2019). Persistence of depressive symptoms and gait speed recovery in older adults after hip fracture. International Journal of Geriatric Psychiatry, 33(7), 875–882. https://doi.org/10.1002/gps.4864.Persistence
- Rathbun, A. M., Shardell, M., Orwig, D., Gruber-Baldini, A. L., Ostir, G., Hicks, G. E., Miller, R. R., Hochberg, M. C., & Magaziner, J. (2016). Effects of prefracture depressive illness and postfracture depressive symptoms on physical performance after hip fracture. Journal of the American Geriatrics Society, 64(11), e171–e176. https://doi.org/10.1111/jgs.14487
- Rubenstein, L. Z., Harker, J. O., Salvà, A., Guigoz, Y., & Vellas, B. (2001). Screening for undernutrition in geriatric practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56(6), M366–372. https://doi.org/10.1093/gerona/56.6.m366
- Vellas, B., Villars, H., Abellan, G., Soto, M. E., Rolland, Y., Guigoz, Y., Morley, J. E., Chumlea, W., Salva, A., Rubenstein, L. Z., & Garry, P. (2006). Overview of the MNA® - Its history and challenges. Journal of Nutrition, Health and Aging, 10(6), 456–463.
- Veronese, N., & Maggi, S. (2018). Epidemiology and social costs of hip fracture. Injury, 49(8), 1458–1460. https://doi.org/10.1016/j.injury.2018.04.015
- Wu, Q., Liu, B., & Tonmoy, S. (2018). Depression and risk of fracture and bone loss: An updated meta-analysis of prospective studies. Osteoporosis International, 29(6), 1303–1312. https://doi.org/10.1007/s00198-018-4420-1
- Yesavage, J. A., & Sheikh, J. I. (1986). Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist, 5(1–2), 165–173. https://doi.org/10.1300/J018v05n01_09
- Young, Y., Xiong, K., Pruzek, R. M., & Brant, L. J. (2010). Examining heterogeneity of functional recovery among older adults with hip fractures. Journal of the American Medical Directors Association, 11(2), 132–139. https://doi.org/10.1016/j.jamda.2009.11.007