Abstract
Objectives
The population of Latin America and Caribbean (LAC) is ageing rapidly, presenting the highest prevalence rates of dementia in the world. Mild cognitive impairment (MCI) is an intermediate condition between normal ageing, Alzheimer’s disease, and related dementias. We conducted a systematic review to evaluate the prevalence of MCI in LAC countries and explore factors associated with MCI (i.e. age, sex/gender, and education).
Method
A database search was conducted in September 2020 using PubMed, Web of Science, Scopus, Lilacs, SciELO, EMBASE, and medRxiv for population- or community-based studies, published in English, Spanish, or Portuguese.
Results
From 2,155 screened studies, we selected reports including subjects with a precise diagnosis of MCI. A total of 11 studies met the inclusion criteria, adding up to 20,220 participants in nine countries: Brazil, Mexico, Argentina, Colombia, Peru, Cuba, Dominican Republic, Venezuela, and Costa Rica. Estimates for all-type MCI prevalence ranged from 6.8% to 25.5% and amnestic MCI between 3.1% and 10.5%. Estimates differed by age and education, with oldest and lower-educated adults presenting higher MCI prevalence.
Conclusion
This first systematic review of the prevalence of MCI discusses the population strata with the highest potential to benefit from dementia risk reduction interventions in LAC countries.
Introduction
Over the last two decades, life expectancy in Latin America and the Caribbean (LAC) region has increased by approximately five years (WHO, Citation2020), and currently, 9% of the population in this region is aged 65 or older. Although the increase in life expectancy is a positive development, one must consider that individuals in LAC countries often present more unfavourable modifiable risk factor profiles than those in high-income countries, which translates to a higher risk of cognitive impairment (Mukadam et al., Citation2019). In fact, the prevalence of dementia in LAC countries is high and still increasing compared with estimates in Europe and United States (Ibáñez et al., Citation2018; Parra et al., Citation2021). For this reason, it is essential to comprehend transitional states, such as mild cognitive impairment (MCI) and underlying factors that can lead to dementia (Mathers & Loncar, Citation2006; Murray & Lopez, Citation1997). Furthermore, knowledge about the prevalence of MCI defines the population strata to potentially benefit most from dementia risk reduction interventions to which public health resources can be allocated, ideally counteracting further increases of the already considerable challenges of dementia for the public health systems of low- and middle-income LAC countries from a socioeconomic and health care system perspective (Figliuoli et al., Citation2018).
MCI is considered a transitional state between normal ageing and dementia (Levey et al., Citation2006; Petersen, Citation2004). The diagnosis of MCI was proposed by Petersen et al. (Citation1999) based on five criteria: (1) episodic memory complaint, reported by the person and preferably confirmed by an informant; (2) mild memory deficit confirmed by cognitive assessment; (3) preserved general cognition; (4) preserved activities of daily living; and (5) absence of dementia. Petersen (Citation2004) later proposed four MCI subtypes: amnestic MCI-single domain, non-amnestic MCI-single domain, amnestic MCI-multiple domain, and non-amnestic MCI-multiple domain. Petersen (Citation2004) argued that the most common subtype is the amnestic MCI-single domain, in which patients present episodic memory impairment without damage in other areas of cognitive functioning. It is essential to point out that not all individuals with MCI will develop dementia. Still, substantial evidence suggests that 10–15% of those with MCI over the age of 65 years develop dementia every year (Petersen et al., Citation2018; Roberts & Knopman, Citation2013). From a public health perspective, to be timely and cost-efficient, interventions aiming at reducing the risk of dementia should focus on at-risk individuals. While other studies have focused on interventions to eliminate or reduce dementia risk factors (Mukadam et al., Citation2020), defining the at-risk population with MCI is important to provide better projections of dementia prevalence and identify the population strata with the highest potential to benefit from risk reduction interventions.
Although the last published systematic review exploring the prevalence of MCI had no country restriction, it did not include any studies written in Spanish or Portuguese language (Ward et al., Citation2012). The majority of the included studies were carried out in Europe and North America. This systematic review found that the prevalence for general MCI was between 3% and 42% and for amnestic MCI between 0.5% to 12% (Ward et al., Citation2012). No LAC country studies were included.
Regarding the risk factors associated with MCI, substantial evidence exists for three major factors being associated with the development of MCI: (i) age, with MCI being more common in the oldest adults (Pankratz et al., Citation2015; Petersen et al., Citation2010; Sánchez et al., Citation2019); (ii) educational level, with illiteracy and low educational levels being risk factors (Langa et al., Citation2017; Rentería et al., Citation2020); and (iii) sex/gender, which remains controversial since some studies found no sex/gender differences (Au et al., Citation2017; Nie et al., Citation2011), while others indicated a higher prevalence of MCI in men (Ganguli et al., Citation2004; Petersen et al., Citation2010).
As the previous systematic review on the prevalence of MCI in the older population provided limited results on prevalence in LAC countries, the aim of the present study was to review evidence on the prevalence of MCI in LAC countries published in the predominantly spoken languages in this region and to provide precise estimates of MCI prevalence overall and by age, educational level, and sex/gender.
Method
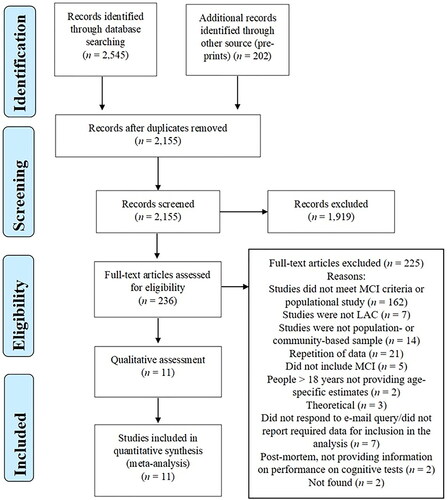
This systematic review was conducted according to the PRISMA guidelines (Moher et al., Citation2010). shows the scores on the PRISMA 2020.
Table 1. Study characteristics.
Moreover, the protocol of this review was preregistered in PROSPERO under registration number CRD42020170924.
Literature search strategy
We conducted a systematic search in the relevant electronic databases of published literature to detect articles fulfilling our criteria: PubMed, Web of Science, Scopus, Lilacs, SciELO, the EMBASE databases, and a preprint server (medRxiv). The search was carried out on February 14, 2020, and updated on September 25, 2020, in three languages: English, Portuguese, and Spanish. No data restriction was applied. The search terms used were: ‘mild cognitive impairment’ or ‘cognitive impairment’ and prevalence or epidemiology and ‘Latin America’ or ‘South America’ or Caribbean or Argentina or Bolivia or Brazil or Chile or Colombia or ‘Costa Rica’ or Cuba or Ecuador or ‘El Salvador’ or Guatemala or Haiti or Honduras or Mexico or Nicaragua or Panama or Paraguay or Peru or Dominican Republic or Uruguay or Venezuela or Jamaica or ‘Trinidad and Tobago’ or Guyana or Suriname or Belize or Bahamas or Barbados or ‘Saint Lucia’ or Grenada or ‘St. Vincent and Grenadines’ or ‘Antigua and Barbuda’ or Dominica or ‘Saint Kitts and Nevis’, adapted according to the databases (the search terms that were employed for each database are available in the supplementary material).
Study inclusion and exclusion criteria
The eligibility criteria of the articles were applied as follows: (i) cohort, case-control or cross-sectional study designs reporting population- or community-based data, from population surveys or patients identified in samples of LAC countries; (ii) studies including frequency of MCI with clearly defined diagnosis criteria, independent of MCI type; (iii) those articles including the term ‘cognitive impairment’ or ‘cognitive impairment no dementia’ without rigorously determined MCI were excluded as our goal was to include the most precise estimates; (iv) studies including hospital or clinical-based samples were also excluded to avoid selection bias; (v) population-based studies, including the prevalence of MCI in participants aged ≥50 years old, since most of the screening instruments have been validated for this age range in LAC countries.
Quality assessment and data extraction
The critical appraisal of the studies was assessed by two independent reviewers (FR and ACT) using the JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data (Munn et al., Citation2015), a 9-item checklist designed to evaluate the methodological quality of the studies and to establish possible bias in design, conduct, and analysis. Incongruence between reviewers about the methodological quality of included studies was resolved by consensus (assessments of both reviewers are provided in Table S2, supplementary material).
Once the articles were included in this review, the variables were independently extracted by two different reviewers (FR and ACT) into an Excel spreadsheet for each article. Data collected from each study included all-type of MCI, amnestic MCI (aMCI), and/or non-amnestic MCI (naMCI). Moreover, when available, we also gathered year of data collection, the number of participants based on the total sample size, age, sex/gender, education, diagnostic criteria, and instruments for MCI screening, study design, prevalence rates with 95% confidence interval and any adjustment performed, and information regarding the rurality of the sample and the socioeconomic level of study participants based on income.
Data analysis
We conducted separate meta-analyses for all-type MCI and aMCI by using the total sample and the number of patients diagnosed with MCI. Prevalence with a 95% confidence interval was estimated via the inverse variance method. Although our inclusion criteria comprised a precise diagnosis of MCI, based on previous systematic reviews including MCI prevalence, a high heterogeneity across studies was expected (Alexander et al., Citation2015; Au et al., Citation2017). For this reason, our data were pooled using random-effects models. The heterogeneity was estimated using I2 in which values ≥75% were considered an indicator of substantial heterogeneity. Sensitivity analyses were performed by removing outlier data from the analysis to explore the robustness of the findings. The leave-one-out method was also performed. We evaluated publication bias by applying Egger’s regression test and visually by creating funnel plots.
As the percentage of women was reported in 10 of the selected articles, we carried out a meta-regression to explore whether there is a correlation between the MCI prevalence estimates and women’s percentage. However, age and education were not included in the meta-regression models because fewer than 50% of the studies reported data on subgroups by age or education. For this reason, we assessed possible effects by age or education through qualitative analysis. All statistical analyses were performed using STATA 16 (Stata metaprop command, StataCorp, Citation2019).
Results
Study selection process
As displayed in the flow diagram presented in , we retrieved 2,747 entries. All retrieved reports were imported into Zotero after the literature database searches, and the duplicate studies were filtered. After removal of duplicates, a total of 2,155 records were independently screened by title and abstract by two independent reviewers (FR and ACT), according to the defined inclusion and exclusion criteria. After the abstract screening, 1,919 studies were excluded and 236 were screened in the full text. Disagreements were solved by consensus between the two reviewers. Authors of six articles were contacted for further data. Finally, a total of 11 records met the inclusion criteria for this systematic review. Initially, an agreement over all the records screened (n = 2,155) between the reviewers was 91%, with a kappa value of 0.50, indicating moderate agreement. However, following further discussion, an agreement was reached for all discrepancies.
Characteristics of the selected studies
summarises the characteristics of the 10 articles and one poster selected for this systematic review, comprising a total of 15 different studies. Sample sizes ranged from 201 to 2,944 participants, which correspond to 20,220 participants in total. Nine of the 20 LAC countries were covered. In addition, there were two studies from Brazil, three from Mexico, one from Argentina, two from Colombia, two from Peru, two from Cuba, one from the Dominican Republic, one from Venezuela, and one from Costa Rica. Ten studies specified amnestic MCI, two non-MCI, and seven reported all-type of MCI. Four studies did not distinguish MCI subtypes.
Pedraza et al. (Citation2017) and Barcelos-Ferreira et al. (Citation2015) applied a two-phase diagnosis, while Wesseling et al. (Citation2013) used a three-phase diagnosis. None of the included studies explored incidence rates. Regarding the published language, three articles were in Spanish, and seven articles and the poster were written in English. Additionally, the poster (Barcelos-Ferreira et al., Citation2015) was not a peer-reviewed study, however, a Google Scholar search confirmed that this study was later published as a doctoral dissertation (Folquitto, Citation2014) from which we retrieved the data. Furthermore, to include the César et al. (2016) study in our meta-analysis, we contacted the authors for additional information regarding MCI prevalence; these authors also suggested a doctoral thesis (César, Citation2014). The language of both doctoral dissertations included in our systematic review is Portuguese (Cesar, Citation2014; Folquitto, Citation2014).
Quantitative analyses
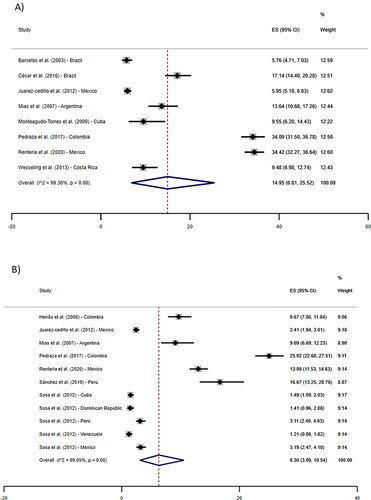
As depicted in , the pooled prevalence of all-type MCI across the eight included studies revealed a prevalence of 14.95% (95% CI: 6.81%–25.52%). Six articles, including 10 different samples, were included in the meta-analysis and showed a pooled prevalence of aMCI estimated of 6.30% (95% CI: 3.09%–10.54%). Sensitivity analyses, where one study at a time was removed from the analysis, showed that the results were quite similar in all situations, revealing no significant influence of a single study in the final results.
The meta-regression did not reveal any correlation between women’s participation rate and MCI or aMCI prevalence.
Publication bias and methodological quality of the studies
Publication bias was not significant for the prevalence of amnestic MCI (t = 1.83, p = 0.08) or all-type MCI (t = −0.15, p = .88) according to Eggers’s test. The corresponding funnel plots are provided in Figure S1 in the supplementary material. The included studies were of high methodological quality. Specifically, each study’s methodological rigour was evaluated by applying nine criteria and only those studies meeting a minimum of five criteria were included in this systematic review (see Table S2, supplementary material). All included papers presented an adequate sample size and a thorough description of the setting.
Furthermore, all but one (Sánchez et al., Citation2019) had appropriate sample frame to address the target population. Sánchez et al. (Citation2019) did not fulfil this criterion because participants had at least six years of schooling, which limited the sample’s representativeness of the local population, since the average educational level in LAC countries is rather low, and education is a factor strongly associated with MCI (Langa et al., Citation2017). Five of the 11 included studies reported random sampling from the population and described how the sampling was performed. Only three studies did not report sufficient coverage of the sample in data analysis, i.e. not all subgroups responded at the same rate. All studies used valid methods for the identification of MCI, except for Wesseling et al. (Citation2013). Six of the 11 papers did not describe the standardisation of measurements. All studies reported the appropriate statistical analyses, apart from Monteagudo-Torres et al. (Citation2009), who did not present confidence intervals. Finally, five articles did not report on response rate.
Qualitative findings
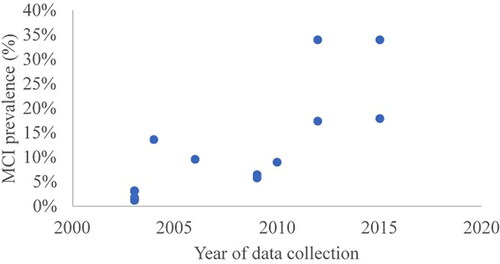
We detected that MCI prevalence was higher for studies with more recent data collection (Pedraza et al., Citation2017; Rentería et al., Citation2020; Sánchez et al., Citation2019). This trend was observed for both aMCI and all-type MCI (see for the growth of all-type MCI prevalence over time).
Regarding the diagnosis protocol used by the included studies, most of them applied a clinical inventory or interviews to assess subjective impairment. To evaluate objective cognitive impairment, most of the studies applied the Mini-Mental State Examination (MMSE) together with different batteries and tests (presented in ). To assess independence in functional abilities, studies used the Bayer ADL, IQCODE, FAQ, Lawton and Brody IADL, Katz Basic Activities of Daily Living Scale, IADL, and the Barthel Index Questionnaire. Finally, the absence of dementia was assessed by clinical interview and neurological examination.
Finally, we detected differences in inclusion criteria regarding age across studies. Five of the articles selected for the review included participants over the age of 60 years. Specifically, three studies included participants older than 50 years, one study included participants older than 55 years, and two studies were comprised of participants above 65 years of age (see ). This point is essential as the prevalence of MCI tends to increase with age (between the ages of 65 and 85 years old) (Petersen et al., Citation2014; Ward et al., Citation2012). However, we did not identify any pattern in which the studies, including younger-old adults, would have a lower prevalence rate or vice versa.
Table 2. Number and percentage of participants with MCI stratified by age.
Discussion
The main goal of this systematic review was to update and summarise the published studies of MCI prevalence estimated in LAC countries using restrictive inclusion criteria regarding MCI diagnosis. Recent estimates suggest a significant increase of dementia worldwide, especially in the LAC region where it is projected that the number of people living with dementia will surpass that of North America by 2030 (Alzheimer’s Disease International, Citation2013). Thus, it is crucial to assess the prevalence of MCI, which is a transitional state between normative ageing and dementia, during which it is still possible to develop and promote strategies to prevent or delay the transition to dementia. Earlier identification of MCI cases could enable the development and promotion of strategies to prevent the rapid transition to dementia.
The results of this meta-analysis showed that the overall prevalence rate for all-type MCI was 14.95%, which is comparable with recent estimates found in low or middle-income countries, e.g. China (Xue et al., Citation2018), but higher when compared to high-income countries, for instance, England (Richardson et al., 2019) or the USA (Petersen et al., Citation2018). It is essential to mention that the latter studies were more conservative in terms of age, only including ageing individuals older than 65 years. Among the LAC studies, some of them included participants as young as 50 years of age, who are at lower risk to present MCI. Nevertheless, the prevalence rate that we found in this review was higher than the prevalence found in high-income countries, which we speculate as being due to socioeconomic and cultural factors linked to cognitive reserve (Prince et al., Citation2012). Recently, however, Pais et al. (Citation2020) claimed that the lower prevalence at higher ages might be due to the conversion rate from healthy cognition to MCI that might occur between the ages of 60 and 70 years. In this context, subjects older than 70 years with a seemingly lower prevalence of MCI may, in fact, have partly already transitioned to dementia.
Moreover, the prevalence of amnestic MCI was 6.30%, which is also higher when compared to community samples from the U.S. (Petersen et al., Citation2018) and from Europe, e.g. France (Ritchie et al., Citation2001), Italy (Tognoni et al., Citation2005), or Germany (Busse et al., Citation2003). More specifically, the higher prevalence of MCI found in the LAC countries could be associated with socioeconomic factors. For example, we observed lower levels of education in LAC countries and the MCI prevalence is lower in higher-educated individuals (Petersen et al., Citation2018). Further, we observed that less advantaged economic conditions, as found in the LAC countries, have been shown to be associated with MCI prevalence (Liu et al., Citation2018). More unfavorable modifiable risk factor profiles may also play a role (Mukadam et al., Citation2019). Notwithstanding an increase in life expectancy in LAC countries due to improved social and economic conditions, earlier studies observed a simultaneous increase in unhealthy lifestyle behaviours, specifically by adopting a more sedentary lifestyle and a diet based on saturated fat, sugar, and refined foods. These factors both contribute to the burden of cardiovascular diseases (Dominguez et al., Citation2006) and diabetes (Bommer et al., Citation2017), and consequently MCI (Luchsinger et al., Citation2007; Zou et al., Citation2014).
Moreover, observing carefully, the studies with the highest prevalence of MCI selected in this systematic review (Barcelos-Ferreira et al., Citation2015; Pedraza et al., Citation2017; Rentería et al., Citation2020) were the most current ones, which may be associated with the rise in life expectancy. For instance, the life expectancy in Columbia has increased by 2.5 years between 2005 and 2012 (OECD, Citationn.d.). This potential trend of higher MCI incidence estimates corresponding to more recent years of data collection was observed for all-type MCI and amnestic MCI. However, the small numbers uncovered here have limited the systematic exploration of this potential association.
Although we applied strict criteria for study inclusion in our systematic review, in which all the studies selected were in congruence with the diagnosis standards proposed by Petersen et al. (2014) and included adequate and representative samples, as proposed by the JBI Critical Appraisal Checklist, heterogeneity remained across the MCI prevalence studies.
Heterogeneity of the included studies extended beyond the described methodological differences in the assessment of MCI, for instance, studies used different protocols or number of testing phases. However, variability seems to be difficult to reduce even within consortia as even the highly renowned 10/66 study has verified a high level of between-site variability (Sosa, Citation2012). Nonetheless, different prevalence of MCI across regions and countries may partly provide us with an accurate picture of heterogeneity in cognitive health, as LAC countries have the most persistent health inequalities in the world, with life expectancy varying between 62 and 79 years (Cardona et al., Citation2013), a fact which may underlie those heterogeneities in MCI prevalence.
Of the studies included in this review, only Rentería et al. (Citation2020) investigated the influence of rurality on MCI prevalence, revealing that it was associated with a higher risk of MCI. In fact, research in high-income countries has identified rural or urban residence as determinants of dementia prevalence, which is partly linked to the differing education levels found for urban and rural residents (Nakamura et al., Citation2016; Weden et al., Citation2018). We suspected similar gradients in the LAC countries but did not have enough studies with information on type of residence (rural vs. urban) available, and most of our included studies were conducted in large urban areas. Further data collection incorporating this variable would help to narrow down the at-risk population of people with MCI.
Finally, we included sex/gender in the meta-regression analysis but failed to find a sex/gender effect. In line with this, findings from Au et al.’s (Citation2017) meta-analysis did not identify any relationship between sex/gender and MCI.
Strengths and limitations
One strength of our study relies on the fact that population or community-based samples were the basis of the included studies. We excluded papers with institutionalised patients to decrease the possibility of bias by selection. This design increases the generalisation and accuracy of our findings to LAC community-dwelling older adults. Moreover, since the prevalence of MCI may vary depending on the diagnostic criteria adopted, such as tests, cut-off values, age, and educational level of the population under study (Gillis et al., Citation2019; Ward et al., Citation2012), we included only high-quality research outputs and clearly defined MCI diagnoses following Petersen’s (2014) criteria, which allows distinguishing MCI from both cognitively normal individuals and those with dementia. It is also important to mention that the studies selected for this review comprised nine countries representing more than 75% of the LAC countries’ total population.
Finally, we highlight the importance of including languages other than English, i.e. Portuguese, and Spanish, when searching databases for MCI articles in Latin America and the Caribbean, as a substantial proportion of the included studies were written in those languages.
In general, a scarcity of research with similar study protocols was observed, and our strict inclusion criteria led to a total of only 10 articles and one poster considered in this review. This is not surprising, as both research funding and infrastructure in the LAC countries are less developed than in high-income countries. However, we ensured that all included research met high-quality standards, assessed by the JBI Critical Appraisal Checklist for prevalence studies (and all studies fulfilled at least five of the nine recommended criteria) (Munn et al., Citation2015).
Future studies should report relevant indicators, such as response rate and standardisation of MCI assessment. Additionally, we suggest random instead of convenience sampling to avoid selection bias. One puzzling finding was the significant heterogeneity that we found in the meta-analyses referring to both all-type MCI and aMCI, the reasons for which are not entirely clear. More studies should be carried out by employing research consortia using harmonised study protocols in concomitant longitudinal studies across Latin America and the Caribbean countries.
Another point that must be mentioned here is the possibly improved diagnosis of MCI in the future through the use of biomarkers, such as magnetic resonance imaging, positron emission tomography, cerebrospinal fluid analyses, and blood-based and genetic markers (Dubois et al., Citation2007; Van Giau et al., Citation2019). The development of a combination of different biomarkers to assess MCI could strengthen the robustness of MCI assessment. No specific biomarkers for the diagnosis of MCI were available in the studies selected for this systematic review.
Additionally, as most of the data of the studies included in this review are from large urban areas of the LAC, it would be essential to carry out studies with more representative samples, including native people (i.e. indigenous) and small villages from more remote areas to gain a more complete picture of the prevalence of MCI in the LAC countries.
Conclusion
This is the first systematic review to investigate and estimate the prevalence of MCI in the LAC countries using strict inclusion criteria for MCI diagnosis and including research published in the predominant languages of this region. These results allow us, for the first time, to provide estimates on the size of the population strata with the highest potential to benefit from dementia risk reduction interventions in LAC countries. We observed a higher prevalence of MCI in comparison to high-income countries. Further, we qualitatively noticed that older and lower educated participants had increased risk for MCI, whereas sex/gender, evaluated quantitatively, was not associated with risk of MCI. Moreover, our analysis revealed that recently published studies reported higher MCI prevalence, providing an impetus for future research to explore the reasons for this more closely.
Supplemental Material
Download PDF (179.4 KB)Disclosure statement
The authors report no conflict of interest.
Funding
This work was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (Grant number No. 803239 to AKL).
Additional information
Funding
References
- Alexander, M., Perera, G., Ford, L., Arrighi, H. M., Foskett, N., Debove, C., Novak, G., & Gordon, M. F. (2015). Age-Stratified Prevalence of Mild Cognitive Impairment and Dementia in European Populations: A Systematic Review. Journal of Alzheimer’s disease: JAD, 48(2), 355–359. https://doi.org/10.3233/JAD-150168
- Alzheimer’s Disease International. (2013). World Alzheimer report 2013. Journey of caring: An analysis of long-term care for dementia. http://www.alz.co.uk/research/WorldAlzheimerReport2013.pdf.
- Au, B., Dale-McGrath, S., & Tierney, M. C. (2017). Sex differences in the prevalence and incidence of mild cognitive impairment: A meta-analysis. Ageing Research Reviews, 35, 176–199. https://doi.org/10.1016/j.arr.2016.09.005
- Barcelos-Ferreira, R., Folquitto, J. C., Tascone, L. S., & Bottino, C. M. C. (2015). Mild behavioral impairment associated to higher prevalence of dementia in community-dwelling elderly subjects. Alzheimer’s and Dementia 11, 521. https://doi.org/10.13140/RG.2.1.1080.7128
- Bommer, C., Heesemann, E., Sagalova, V., Manne-Goehler, J., Atun, R., Bärnighausen, T., & Vollmer, S. (2017). The global economic burden of diabetes in adults aged 20–79 years: A cost-of-illness study. The Lancet Diabetes & Endocrinology, 5(6), 423–430. https://doi.org/10.1016/S2213-8587(17)30097-9
- Busse, A., Bischkopf, J., Riedel-Heller, S. G., & Angermeyer, M. C., & Leipzig Longitudinal Study of the Aged LEILA75+. (2003). Mild cognitive impairment: Prevalence and predictive validity according to current approaches. Acta Neurologica Scandinavica, 108(2), 71–81. https://doi.org/10.1034/j.1600-0404.2003.00118.x
- Cardona, D., Acosta, L. D., & Bertone, C. L. (2013). Inequidades en salud entre países de Latinoamérica y el Caribe (2005–2010). Gaceta Sanitaria, 27(4), 292–297. https://doi.org/10.1016/j.gaceta.2012.12.007
- César, K. G. (2014). Estudo da prevalência de comprometimento cognitivo leve e demência na cidade de Tremembé [estado de São Paulo] [Doctoral dissertation]. University of São Paulo Repository. https://doi.org/10.1016/j.jns.2015.08.396
- César, K. G., Brucki, S. M. D., Takada, L. T., Nascimento, L. F. C., Gomes, C. M. S., Almeida, M. C. S., Oliveira, M. O., Porto, F. H. G., Senaha, M. L. H., Bahia, V. S., Silva, T. B. L., Ianof, J. N., Spíndola, L., Schmidt, M. T., Jorge, M. S., Vale, P. H. F., Cecchini, M. A., Cassimiro, L., Soares, R. T., … Nitrini, R. (2016). Prevalence of cognitive impairment without dementia and dementia in Tremembé, Brazil. Alzheimer Disease & Associated Disorders, 30(3), 264–271. https://doi.org/10.1097/WAD.0000000000000122
- Dominguez, L. J., Galioto, A., Ferlisi, A., Pineo, A., Putignano, E., Belvedere, M., Costanza, G., & Barbagallo, M. (2006). Ageing, lifestyle modifications, and cardiovascular disease in developing countries. The Journal of Nutrition, Health & Aging, 10(2), 143–149.
- Dubois, B., Feldman, H. H., Jacova, C., Dekosky, S. T., Barberger-Gateau, P., Cummings, J., Delacourte, A., Galasko, D., Gauthier, S., Jicha, G., Meguro, K., O’Brien, J., Pasquier, F., Robert, P., Rossor, M., Salloway, S., Stern, Y., Visser, P. J., & Scheltens, P. (2007). Research criteria for the diagnosis of Alzheimer’s disease: Revising the NINCDS-ADRDA criteria. The Lancet Neurology, 6(8), 734–746. https://doi.org/10.1016/S1474-4422(07)70178-3
- Figliuoli, L., Flamini, V., Lambert, F., & Mowatt, R. (2018). Is Latin America prepared for an aging population? https://www.imf.org/en/News/Articles/2018/12/11/blog-is-latin-america-prepared-for-an-aging-population
- Folquitto, J. C. (2014). Prevalência de sintomas depressivos em pacientes com demência: correlação com sintomas neuropsiquiátricos e déficits nas atividades de vida diária [Doctoral dissertation]. University of São Paulo Repository. https://doi.org/10.11606/T.5.2015.tde-11052015-143031.
- Ganguli, M., Dodge, H. H., Shen, C., & DeKosky, S. T. (2004). Mild cognitive impairment, amnestic type: An epidemiologic study. Neurology, 63(1), 115–121. https://doi.org/10.1212/01.WNL.0000132523.27540.81
- Gillis, C., Mirzaei, F., Potashman, M., Ikram, M. A., & Maserejian, N. (2019). The incidence of mild cognitive impairment: A systematic review and data synthesis. Alzheimer’s & Dementia (Amsterdam, Netherlands), 11, 248–256. https://doi.org/10.1016/j.dadm.2019.01.004
- Henao-Arboleda, E., Aguirre-Acevedo, D. C., Muñoz, C., Pineda, D. A., & Lopera, F. (2008). Prevalencia de deterioro cognitivo leve de tipo amnésico en una población colombiana. Revista de Neurología, 46(12), 709–713. https://doi.org/10.33588/rn.4612.2007569
- Ibáñez, A., Sedeño, L., García, A. M., Deacon, R., & Cogram, P. (2018). Editorial: Human and animal models for translational research on neurodegeneration: Challenges and opportunities from South America. Frontiers in Aging Neuroscience, 10, 95. https://doi.org/10.3389/fnagi.2018.00095
- Juarez-Cedillo, T., Sanchez-Arenas, R., Sanchez-Garcia, S., Garcia-Peña, C., Hsiung, G.-Y R., Sepehry, A. A., Beattie, B. L., & Jacova, C. (2012). Prevalence of mild cognitive impairment and its subtypes in the Mexican population. Dementia and Geriatric Cognitive Disorders, 34(5–6), 271–281. https://doi.org/10.1159/000345251
- Langa, K. M., Larson, E. B., Crimmins, E. M., Faul, J. D., Levine, D. A., Kabeto, M. U., & Weir, D. R. (2017). A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Internal Medicine, 177(1), 51–58. https://doi.org/10.1001/jamainternmed.2016.6807
- Levey, A., Lah, J., Goldstein, F., Steenland, K., & Bliwise, D. (2006). Mild cognitive impairment: An opportunity to identify patients at high risk for progression to Alzheimer’s disease. Clinical Therapeutics, 28(7), 991–1001. https://doi.org/10.1016/j.clinthera.2006.07.006
- Liu, X., Yin, X., Tan, A., He, M., Jiang, D., Hou, Y., Lu, Y., & Mao, Z. (2018). Correlates of mild cognitive impairment of community-dwelling older adults in Wuhan, China. International Journal of Environmental Research and Public Health, 15(12), 2705. https://doi.org/10.3390/ijerph15122705
- Luchsinger, J. A., Reitz, C., Patel, B., Tang, M. X., Manly, J. J., & Mayeux, R. (2007). Relation of diabetes to mild cognitive impairment. Archives of Neurology, 64(4), 570–575. https://doi.org/10.1001/archneur.64.4.570
- Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine, 3(11), e442. https://doi.org/10.1371/journal.pmed.0030442
- Mías, C. D., Sassi, M., Masih, M. E., Querejeta, A., & Krawchik, R. (2007). Deterioro cognitivo leve: Estúdio de prevalência y factores sociodemográficos en la ciudad de Córdoba, Argentina [Mild cognitive impairment: A prevalence and sociodemographic factors study in the city of Córdoba, Argentina]. Revista de Neurología, 44(12), 733–738. https://doi.org/10.33588/rn.4412.2006206
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery (London, England), 8(5), 336–341. https://doi.org/10.1371/journal.pmed.1000097
- Monteagudo-Torres, M., Gómez-Viera, N., Martín-Labrador, M., Jiménez-Fontao, L., Mc Cook, E., & Ruiz-García, D. (2009). Evaluación del estado cognitivo de los adultos mayores de 60 años, en un área de salud del Policlínico Docente Plaza de la Revolución. Revista Cubana de Medicina, 48, 59–70. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232009000300006&lng=es&tlng=es.
- Mukadam, N., Anderson, R., Knapp, M., Wittenberg, R., Karagiannidou, M., Costafreda, S. G., Tutton, M., Alessi, C., & Livingston, G. (2020). Effective interventions for potentially modifiable late-onset dementia risk factors: Their costs and cost-effectiveness. The Lancet Healthy Longevity, 1(1), E13–320. https://doi.org/10.1016/S2666-7568(20)30004-0
- Mukadam, N., Sommerlad, A., Huntley, J., & Livingston, G. (2019). Population attributable fractions for risk factors for dementia in low-income and middle-income countries: An analysis using cross-sectional survey data. The Lancet Global Health, 7(5), e596–e603. https://doi.org/10.1016/S2214-109X(19)30074-9
- Munn, Z., Moola, S., Lisy, K., Riitano, D., & Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence-Based Healthcare, 13(3), 147–153. https://doi.org/10.1097/XEB.0000000000000054
- Murray, C. J., & Lopez, A. D. (1997). Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. The Lancet, 349(9064), 1498–1504. https://doi.org/10.1016/S0140-6736(96)07492-2
- Nakamura, K., Kitamura, K., Watanabe, Y., Shinoda, H., Sato, H., & Someya, T. (2016). Rural–urban differences in the prevalence of cognitive impairment in independent community-dwelling elderly residents of Ojiya city, Niigata Prefecture, Japan. Environmental Health and Preventive Medicine, 21(6), 422–429. https://doi.org/10.1007/s12199-016-0542-2
- Nie, H., Xu, Y., Liu, B., Zhang, Y., Lei, T., Hui, X., Zhang, L., & Wu, Y. (2011). The prevalence of mild cognitive impairment about elderly population in China: A meta-analysis. International Journal of Geriatric Psychiatry, 26(6), 558–563. https://doi.org/10.1002/gps.2579
- OECD. (n.d.). Country statistical profiles: Key tables from OECD. http://www.oecd.org/colombia/. Accessed 14 December 2020.
- Pais, R., Ruano, L., P Carvalho, O., & Barros, H. (2020). Global cognitive impairment prevalence and incidence in community dwelling older adults - A systematic review. Geriatrics, 5(4), 84. https://doi.org/10.3390/geriatrics5040084
- Pankratz, V. S., Roberts, R. O., Mielke, M. M., Knopman, D. S., Jack, C. R., Jr., Geda, Y. E., Rocca, W. A., & Petersen, R. C. (2015). Predicting the risk of mild cognitive impairment in the Mayo Clinic Study of Aging. Neurology, 84(14), 1433–1442. https://doi.org/10.1212/WNL.0000000000001437
- Parra, M. A., Baez, S., Sedeño, L., Gonzalez Campo, C., Santamaría-García, H., Aprahamian, I., Bertolucci, P. H., Bustin, J., Camargos Bicalho, M. A., Cano-Gutierrez, C., Caramelli, P., Chaves, M. L. F., Cogram, P., Beber, B. C., Court, F. A., de Souza, L. C., Custodio, N., Damian, A., de la Cruz, M., … Ibanez, A. (2021). Dementia in Latin America: Paving the way toward a regional action plan. Alzheimer’s & Dementia, 17(2), 295–313. https://doi.org/10.1002/alz.12202
- Pedraza, O. L., Montes, A. M. S., Sierra, F. A., Montalvo, M. C., Muñoz, Y., Díaz, J. M., Lozano, A., & Piñeros, C. (2017). Mild cognitive impairment (MCI) and dementia in a sample of adults in the city of Bogotá. Dementia & Neuropsychologia, 11(3), 262–269. https://doi.org/10.1590/1980-57642016dn11-030008
- Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256(3), 183–194. https://doi.org/10.1111/j.1365-2796.2004.01388.x
- Petersen, R. C., Caracciolo, B., Brayne, C., Gauthier, S., Jelic, V., & Fratiglioni, L. (2014). Mild cognitive impairment: a concept in evolution. Journal of internal medicine, 275(3), 214–228. https://doi.org/10.1111/joim.12190
- Petersen, R. C., Lopez, O., Armstrong, M. J., Getchius, T. S. D., Ganguli, M., Gloss, D., Gronseth, G. S., Marson, D., Pringsheim, T., Day, G. S., Sager, M., Stevens, J., & Rae-Grant, A. (2018). Practice guideline update summary: Mild cognitive impairment: Report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology, 90(3), 126–135. https://doi.org/10.1212/WNL.0000000000004826
- Petersen, R. C., Roberts, R. O., Knopman, D. S., Geda, Y. E., Cha, R. H., Pankratz, V. S., Boeve, B. F., Tangalos, E. G., Ivnik, R. J., & Rocca, W. A. (2010). Prevalence of mild cognitive impairment is higher in men. The Mayo Clinic Study of Aging. Neurology, 75(10), 889–897. https://doi.org/10.1212/WNL.0b013e3181f11d85
- Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Tangalos, E. G., & Kokmen, E. (1999). Mild cognitive impairment: Clinical characterization and outcome. Archives of Neurology, 56(3), 303–308. https://doi.org/10.1001/archneur.56.3.303
- Prince, M., Acosta, D., Ferri, C. P., Guerra, M., Huang, Y., Rodriguez, J. J. L., Salas, A., Sosa, A. L., Williams, J. D., Dewey, M. E., Acosta, I., Jotheeswaran, A. T., & Liu, Z. (2012). Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: A 10/66 Dementia Research Group population-based cohort study. The Lancet, 380(9836), 50–58. https://doi.org/10.1016/S0140-6736(12)60399-7
- Rentería, M. C., Mainly, J. J., Vonk, J. M., Arango, S. M., Obregon, A. M., Samper-Ternent, R., Wong, R., Mayeux, R., Barral, S., & Tosto, G. (2020). Prevalence of mild cognitive impairment in Mexican older adults: Data from the Mexican Health and Aging Study (MHAS). medRxiv. https://doi.org/10.1101/2020.01.03.20016345
- Richardson, C., Stephan, B. C. M., Robinson, L., Brayne, C., Matthews, F. E., & Cognitive Function and Ageing Study Collaboration. (2019). Two-decade change in prevalence of cognitive impairment in the UK. European Journal of Epidemiology, 34(11), 1085–1092. https://doi.org/10.1007/s10654-019-00554-x
- Ritchie, K., Artero, S., & Touchon, J. (2001). Classification criteria for mild cognitive impairment: A population-based validation study. Neurology, 56(1), 37–42. https://doi.org/10.1212/wnl.56.1.37
- Roberts, R., & Knopman, D. S. (2013). Classification and epidemiology of MCI. Clinics in Geriatric Medicine, 29(4), 753–772. https://doi.org/10.1016/j.cger.2013.07.003
- Sánchez, S. S., Abanto, J., Sanchez-Boluarte, A., Boluarte-Carbajal, A., Sanchez-Coronel, D., Custodio-Capuñay, N., & Samalvides-Cuba, F. (2019). Frequency and associated factors of amnestic mild cognitive impairment at four senior citizen clubs in Lima, Peru. Dementia & Neuropsychologia, 13(3), 321–328. https://doi.org/10.1590/1980-57642018dn13-030009
- Sosa, A. L., Albanese, E., Stephan, B. C., Dewey, M., Acosta, D., Ferri, C. P., Guerra, M., Huang, Y., Jacob, K. S., Jiménez-Velázquez, I. Z., Rodriguez, J. J., Salas, A., Williams, J., Acosta, I., González-Viruet, M., Hernandez, M. A., Shuran, L., Prince, M. J., & Stewart, R. (2012). Prevalence, distribution, and impact of mild cognitive impairment in Latin America, China, and India: A 10/66 population-based study. PLoS Medicine, 9(2), e1001170. https://doi.org/10.1371/journal.pmed.1001170
- StataCorp. (2019). Stata Statistical Software: Release 16. College Station, T X: StataCorp LLC.
- Tognoni, G., Ceravolo, R., Nucciarone, B., Bianchi, F., Dell’Agnello, G., Ghicopulos, I., Siciliano, G., & Murri, L. (2005). From mild cognitive impairment to dementia: A prevalence study in a district of Tuscany, Italy. Acta Neurologica Scandinavica, 112(2), 65–71. https://doi.org/10.1111/j.1600-0404.2005.00444.x
- Van Giau, V., Bagyinszky, E., & An, S. S. A. (2019). Potential fluid biomarkers for the diagnosis of mild cognitive impairment. International Journal of Molecular Sciences, 20(17), 4149. https://doi.org/10.3390/ijms20174149
- Ward, A., Arrighi, H. M., Michels, S., & Cedarbaum, J. M. (2012). Mild cognitive impairment: Disparity of incidence and prevalence estimates. Alzheimer’s & Dementia, 8(1), 14–21. https://doi.org/10.1016/j.jalz.2011.01.002
- Weden, M. M., Shih, R. A., Kabeto, M. U., & Langa, K. M. (2018). Secular trends in dementia and cognitive impairment of U.S. rural and urban older adults. American Journal of Preventive Medicine, 54(2), 164–172. https://doi.org/10.1016/j.amepre.2017.10.021
- Wesseling, C., Román, N., Quirós, I., Páez, L., García, V., Mora, A. M., Juncos, J. L., & Steenland, K. N. (2013). Parkinson’s and Alzheimer’s diseases in Costa Rica: A feasibility study toward a national screening program. Global Health Action, 6, 23061. https://doi.org/10.3402/gha.v6i0.23061
- World Health Organization – WHO. (2020). Ageing. https://www.who.int/health-topics/ageing#tab=tab_1. Accessed 15 December 2020.
- Xue, J., Li, J., Liang, J., & Chen, S. (2018). The prevalence of mild cognitive impairment in China: A systematic review. Aging and Disease, 9(4), 706. https://doi.org/10.14336/AD.2017.0928
- Zou, Y., Zhu, Q., Deng, Y., Duan, J., Pan, L., Tu, Q., Dai, R., Zhang, X., Chu, L., & Lü, Y. (2014). Vascular risk factors and mild cognitive impairment in the elderly population in southwest China. American Journal of Alzheimer’s Disease and Other Dementias, 29(3), 242–247. https://doi.org/10.1177/1533317513517042