Abstract
Objectives
Older carers play a vital role supporting population health and protecting health and social care systems, yet there has been little research on understanding the effect of the pandemic on this group. In this paper, we investigate caring as a factor contributing to mental and self-rated health.
Methods
We investigate cross-sectional and longitudinal associations between provision of family care and mental health and wellbeing using longitudinal data from 5,149 members of the English Longitudinal Study of Ageing who responded to Wave 9 (2018/2019) and two COVID-19 sub-studies (June/July 2020; November/December 2020). We use logistic or linear regression models depending on outcome measures, controlling for pre-pandemic socioeconomic, demographic, and health-related variables.
Results
Before the pandemic, 21% of respondents cared for family or friends. Older people caring for someone inside the household mostly continued to provide care during the pandemic, with more than a quarter reporting an increase in the amount of care provided. Co-resident carers were disproportionately female, older, in the lowest wealth quintile, and more likely to report disability and chronic conditions. Both cross-sectional and longitudinal analyses suggest that, compared to those caring for people living outside the household, co-resident carers were significantly more likely to report poorer mental health and self-rated health.
Conclusion
The health of older carers worsened disproportionately in the first year of the pandemic, a period also characterised by disruptions to support and closure of respite services. Support for carers’ mental and physical health requires greater policy attention, especially in pandemic conditions.
Introduction
Informal caregivers are generally defined as unpaid carers, often family members or friends, who provide help to people living with a long-term physical disability, mental health condition or chronic disease. Older caregivers play a vital social and economic role supporting population health and wellbeing and protecting health and social care systems, yet there has been little research or policy attention given to understanding the health effects of the COVID-19 pandemic on this vital group of carers. To mitigate the spread of COVID-19, the UK government announced its first lockdown in March 2020 that included the closure of educational institutions, community facilities (e.g. libraries), and all non-essential shops and services. For carers, the COVID-19 pandemic and lockdown restrictions often resulted in closure of day centres and respite facilities, reduced access to, and the delivery of, primary and specialist health and social care services (Giebel, Cannon, et al., Citation2021; Muldrew et al., Citation2022; Onwumere et al., Citation2021). Respite services closed or became much higher risk for families, with many fearing that if a family member went into respite in a residential home, they may never be seen again, or only in highly unsatisfactory circumstances (Giebel, Hanna, et al., Citation2022). Moreover, pressures on health services during the pandemic have meant fewer diagnoses of, for example, dementia, which means normal routes into support for carers have not been operating (Giebel, Hanna, et al., Citation2021; Liu et al., Citation2021).
In the first months of the pandemic, people were also instructed to stay indoors, to work from home and home school if possible, and to avoid or at least limit interactions with people outside of their immediate household, including relatives, friends, and the general public, particularly older people and those with health conditions who were considered at higher risks of COVID-related morbidity and mortality. For older carers, this represented a challenge that often resulted in the cessation or reduction of support and help to people outside their own household (Di Gessa et al., Citation2023), in order to avoid the transmission of the virus and/or to reduce their own risk of infection. However, for older people providing care within the same household the pandemic led to an intensification of caring responsibilities, as they received less support from formal care providers and additional family caregivers (Price et al., Citation2022). Moreover, older carers are likely to have been living with significant additional stress during the pandemic. They and those they care for typically have high health risks and, through age and/or increased clinical vulnerability to Covid, have suffered disproportionate mortality and morbidity impact of the SARS-Cov-2 virus (Booth et al., Citation2021; Ho et al., Citation2020). They were likely to be shielding or staying at home to protect themselves, with disrupted family relationships, and fearful of allowing formal carers into the household because of the risks that they posed (Derrer-Merk et al., Citation2022; Giebel et al., Citation2020). .
Although we know that there has been substantial deterioration in mental health and wellbeing for the over 50s during the pandemic, exacerbated by shielding for those identified as clinically vulnerable to COVID-19 (Di Gessa & Price, Citation2021, Citation2022; Steptoe & Di Gessa, Citation2021), we still know very little about how older carers have coped during the pandemic. Commonly, older informal carers themselves have challenges with activities of daily living, and provide more intensive care for longer hours with lower quality of life than younger carers (Carmichael & G. Ercolani, Citation2014; Greenwood & Smith, Citation2016). Often, these carers feel ambivalent about requesting support, are less inclined to seek help, and report being anxious, socially isolated and lonely (Greenwood, Pound, Brearley, et al., Citation2019). Moreover, since we know that prior to the pandemic carers are likely to have had poorer physical and mental health (Bauer & Sousa-Poza, Citation2015; Bom & Stöckel, Citation2021) and have been more isolated and lonely than non-carers (Muldrew et al., Citation2022) it is important to acknowledge and control for such differences.
To date, research on carers’ experiences during the pandemic has mostly focussed on caring for someone with dementia rather than on carers more widely, using non-representative surveys or small scale qualitative samples (Giebel, Hanna, et al., Citation2022; Giebel, Hanna, et al., Citation2021; Giebel, Lord, et al., Citation2021; Giebel, Pulford, et al., Citation2021; Giebel, Talbot, et al., Citation2023; Hanna et al., Citation2022; Hughes et al., Citation2021; Liu et al., Citation2021; Tuijt et al., Citation2021). This research is important in documenting lived experience of the impact of COVID-19 on people living with dementia at home and their family carers and showing that carers have faced, and continue to face, extreme challenges. However, the nature of the datasets used has not allowed us to understand the prevalence of care provision at population level for older people during the pandemic, nor its association with mental health and self-rated health. Moreover, as Giebel et al. noted in their recent systematic review (2022), previous studies on carer mental health during the pandemic have been limited by providing retrospective accounts from carers of their mental health prior to the pandemic, because pre-pandemic assessments were not available from carer surveys.
In this paper, we therefore aim to understand the extent to which caring has been an additional factor contributing to poorer mental health and wellbeing during the pandemic, and where relevant, to identify the characteristics of carers who have been disproportionately impacted. Although the whole population was subjected to the stresses of the pandemic and pandemic response, we hypothesise that carers would have had pre-existing vulnerabilities to poorer mental and physical health which are likely to have left them more susceptible to deterioration than those without caregiving responsibilities. We expect this susceptibility to be more extreme for co-resident caregivers because of the nature of 24-h care that this might entail, and the additional stress caused by likely social isolation for these families without any breaks from care. To assess these questions, we present evidence from a nationally representative quantitative study to consider mental health and self-rated health for older carers during the pandemic, using the English Longitudinal Study of Ageing (ELSA) where the longitudinal design allows us to account for pre-pandemic health characteristics. In this paper we can further distinguish between those who cared for someone outside their household and co-resident carers who may have been perceived by family and services as lower priority for support than people with high care needs living alone.
Materials and methods
We used the most recent pre-pandemic data (wave 9, collected in 2018/19) and the two waves of the COVID-19 sub-study (collected in June/July and November/December 2020 respectively) of the English Longitudinal Study of Ageing (Banks et al., Citation2021). ELSA is a longitudinal biennial survey representative of individuals aged 50 and over in private households. During the pandemic, ELSA members were invited to participate online or by CATI (Computer-Assisted Telephone Interviewing) to the COVID-19 sub-study (75% response rate in both waves, 94% longitudinal response rate). Analyses were based on core respondents with available information in Wave 9 who participated in both COVID-19 waves (N = 5,149—these respondents are referred to as ‘older’ people in the remainder of the manuscript). Additional analyses were performed on co-residing opposite-sex respondents with complete information on both partners’ caring, health, and demographic characteristics—we selected couples where at least one partner provided care for their spouse (N = 240) and the same number of couples (matched age, sex, education, and wealth of the carer) where neither provided care during the pandemic. Further details of the survey’s sampling frame and methodology can be found at www.elsa-project.ac.uk. ELSA was approved by the London Multicentre Research Ethics Committee (MREC/01/2/91). Informed consent was obtained from all participants. All data are available through the UK Data Service (SN 8688 and 5050).
Main measurements of interest
Caring
Information on caring was obtained from the first wave of the ELSA COVID-19 sub-study. In June/July 2020, respondents were asked whether just before the coronavirus outbreak began in February 2020, they looked after anyone once a week or more. Those who were providing care were then asked if the person (or people) they cared for before the coronavirus outbreak lived with them or in another household. They were then asked if the amount of care provided to those in and/or outside the household changed since the coronavirus outbreak (with options ‘increased’, ‘stayed the same’, ‘decreased’, or ‘stopped’). Finally, all respondents (regardless of whether they cared pre-pandemic or not) were asked whether they provide help for someone outside of their household who they had not cared for previously, due to the coronavirus outbreak. Respondents were not asked whether they had started caring since the beginning of the COVID-19 pandemic for someone they were living with. Full details of the ELSA COVID-19 Survey content and questions can be found at www.elsa-project.ac.uk/covid-19.
Based on these questions, for our multivariate analyses we created a variable that distinguished five categories of carers: those who did not care pre-pandemic and did not start caring during the pandemic (not carers); those who did not care pre-pandemic but started looking after people outside their household during the pandemic (new carers); those who stopped caring altogether; those who kept caring for someone living in the same household (co-resident carers); and those who kept caring for someone living outside the household.
Outcome health measures
We considered one outcome measure of general health and four outcome measures of mental health assessed both pre-pandemic and at the COVID-19 waves (depressive symptoms, anxiety, quality of life, and life satisfaction). Self-rated health (SRH) was measured using responses to a generic question (‘Would you say your health is …’) on a 5-point ordinal scale (excellent, very good, good, fair, or poor). The five SRH items were dichotomised into ‘fair or poor’ versus better health (Manderbacka et al., Citation1998).
Symptoms of depression were measured by an abbreviated version of the validated Centre for Epidemiologic Studies Depression (CES-D) Scale (Radloff, Citation1977). The CES-D scale is not a diagnostic instrument for clinical depression but can be used to identify people ‘at risk’ of depression in population-based studies. This short version has good internal consistency (Cronbach’s α > 0.95) and comparable psychometric properties to the full 20-item CES-D (Karim et al., Citation2015). The scale includes 8 binary (no/yes) questions that ask whether respondents experienced any depressive symptoms, such as feeling sad or having restless sleep, in the week prior to interview. In line with previous studies, we classified respondents who reported four or more depressive symptoms on the CES-D scale as with elevated depressive symptoms (Turvey et al., Citation1999; Zivin et al., Citation2010).
Anxiety was monitored with the Generalised Anxiety Disorder assessment (GAD-7), which evaluates the presence in the past two weeks of seven symptoms of anxiety, such as becoming easily annoyed or irritable or not being able to stop or control worrying, on a 4-point scale (‘Not at all’, ‘Several days’, ‘More than half the days’, ‘Nearly every day’). This is a well-validated tool, with a high scale reliability (Cronbach α = 0·90 in this study) used to screen for generalised anxiety disorder in clinical practice and research (Spitzer et al., Citation2006). A standard threshold score of 10 on the GAD-7 scale was used to define clinically significant symptoms.
Moreover, we considered subjective quality of life (QoL) evaluated using the 12-item Control, Autonomy, Self-realisation and Pleasure (CASP-12) scale. This is an abbreviated measure of the validated CASP-19 scale which was specifically designed for individuals in later life and used in a wide variety of ageing surveys (Hyde et al., Citation2003). CASP-12 contains 12 Likert-scaled questions measuring older people’s control and autonomy as well as self-realization through pleasurable activities. The possible range of CASP-12 scores is from 0 to 36, with higher scores indicating greater well-being; CASP-12 is treated as a continuous variable.
Finally, we considered life satisfaction as a measure of personal well-being assessed using the Office for National Statistics (ONS) well-being scale (‘On a scale of 0 to 10, where 0 is ‘not at all’ and 10 is ‘very’, how satisfied are you with your life nowadays?’). This allows respondents to integrate and weigh various life domains the way they choose (Pavot & Diener, Citation1993).
Covariates
Our analyses controlled for a wide range of demographic, socio-economic characteristics, health, and social support characteristics. We controlled for age-groups (50s; 60s; 70s; or 80 and older); sex; and ethnicity (White vs non-White participants due to data constraints in ELSA). To capture respondents’ socio-economic characteristics we controlled for pre-pandemic education, income, and wealth. Educational level was recoded into low (below secondary), middle, and high (university or above) following the International Standard Classification of Education (http://www.uis.unesco.org/). We categorised respondents by quintiles of wealth (total net non-pension non-housing wealth) and accounted for their equivalised total income (from paid work, state benefits, pensions and assets).
We further accounted for pre-pandemic health. In particular, we controlled for disability (impairments with basic and instrumental activities of daily living; or reporting a long-lasting illness) and clinical vulnerability to COVID-19 (defined irrespective of age as reporting chronic lung disease, asthma, coronary heart disease, Parkinson’s disease, multiple sclerosis, diabetes; weakened immune system as a result of cancer treatment in the previous two years; BMI of 40 or above; and/or having been advised to shield by their GP/NHS; Di Gessa & Price, Citation2021). We also controlled for pre-pandemic measures of general and mental health (see above for derivation). For GAD-7—not included in pre-pandemic waves—analyses were adjusted for pre-pandemic ratings on the ONS anxiety scale.
Finally, using the short version of the Revised UCLA loneliness scale with scores of 6 and higher indicating greater loneliness (M. E. Hughes et al., Citation2004), we created a variable indicating whether respondents felt lonely or not during the pandemic. Also, we controlled for whether the respondent had negative experiences of COVID-19 (proxied by whether respondents or any of their friends or relatives had been hospitalised or a friend or relative had died because of COVID-19) and whether they were shielding in the week prior the interview, that is if they reporting not leaving home for any reason, not going out to buy food and not seeing people outside of their household.
Statistical analysis
Following descriptive analysis, we investigated the cross-sectional and longitudinal associations between care provision and mental health using logistic or linear models depending on the outcome. We present two models for each outcome: first we control for demographic and socio-economic characteristics as well as for pre-pandemic physical health (Model 1) to then additionally control for the pre-pandemic relevant general or mental health measures (Model 2). Interactions between caring and age-groups were considered in preliminary analyses. However, since none of the interactions were statistically significant at p < .05, we omitted this term from the final models presented in this manuscript. Moreover, even when we investigated age-stratified relationships between care and health among two broader age groups (50–69 and 70+), results were similar in magnitude and directions and we decided to report results from the whole sample (see Supplementary Table S1). Then, focusing on married heterosexual couples where at least one partner provided care for their spouse, we also provide descriptive statistics of the health profile of both members (receiving and providing care) and compare them with couples (matched on age, sex, education, and wealth of the carer) where neither partner provided care during the pandemic. It was not possible also to include couples where one of the partners was caring for family and friends living outside of the household because of their generally younger age profile (see Results). All analyses were performed using Stata 16. Cross-sectional and longitudinal sampling weights were employed to account for different probabilities of being included in the sample and for nonresponse to the survey.
Results
Descriptive statistics
Just before the pandemic, 21.3% of ELSA respondents were providing care for family or friends, more or less evenly split between inside (9.5%) and outside (11.7%) of the household. A tiny number of carers (n = 15) reported caring simultaneously for people in and outside their household.
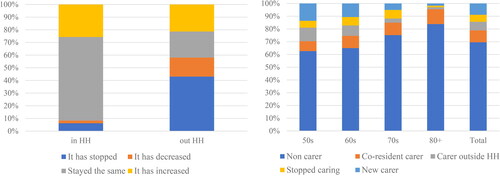
Since the pandemic, caring changed but differently depending on whether people were looking after someone in or out of the household (see ). For those caring for someone within their household prior to the pandemic, only 6% stopped caring altogether while for more than a quarter (26%) their provision of care increased and for two thirds it stayed the same. This was in marked contrast to those who had been caring for someone outside their household, where 43% stopped caring altogether, and a further 15% provided less care than before. About 21% provided either the same amount of care or more. During the pandemic, 9% of respondents started to provide care for someone outside of their households whom they had not previously looked after (‘new carers’). Most of these new carers (46%) looked after these people once a week, with about a quarter (22%) doing it only once/not regularly, and about 7% almost every day. New carers were largely younger people (in their 50s and 60s), whereas those who kept caring for someone within the household were more likely to be over 70.
Figure 1. Changes in care (by household) and caring responsibilities (by age groups) during the pandemic.
Source: ELSA COVID-19 Sub-Study Wave 1 (June/July 2020) – weighted data. Notes: HH stands for household.
Descriptive bivariate statistics in show that older people who continued to care for someone inside the household through the pandemic are disproportionately female, older (much more likely to be over 80), and in the lowest wealth quintile. They are substantially more likely to struggle with activities and instrumental activities of daily living; live with limiting long-standing illness; be themselves classified as clinically vulnerable to COVID-19; and shield. When health measures are considered, people caring for someone inside the household also report poorer scores compared to the other groups for all the variables considered. For instance, 38% reported poor or fair self-rated health and 15% high levels of anxiety compared to 16% and 8% respectively among those who cared for friends and family living outside of the household. Similarly, co-residing carers reported the lowest mean quality of life (mean CASP-12 = 23.31) and life satisfaction (mean = 6.57) whereas those caring for someone outside the household scored among the highest values (with mean CASP-12 = 26.67 and mean life satisfaction = 7.13). To more easily compare these mean scores, we found a similar difference of about 3 CASP-12 points between respondents who were classified as clinically vulnerable to COVID-19 and those who were not; and a difference of about 0.7 points in mean life satisfaction between respondents who reported no limiting long-standing illness and those who did.
Table 1. Percent distribution of sample characteristics by care during COVID-19, column percentages.
Multivariate findings
To investigate how care provision during the first months of the pandemic was associated with health we used logistic and linear regressions, depending on the outcome variable. shows the fully-adjusted models for the cross-sectional associations between provision of care during the pandemic and health measured at the first wave of the COVID-19 sub-study (June/July 2020). The full covariates for the complete models are available in Supplementary Table S2. Accounting for socio-demographic and economic characteristics as well as for health profile (Model 1) we found that carers who continued to care for a person in the same household were more likely to report poor self-rated health (OR = 2.30), lower quality of life (B = −1.923), and lower life satisfaction (B = −0.485) compared to those who cared for someone living outside of their household. The direction and strength of association was largely robust to pre-pandemic health (Model 2), although coefficients were attenuated.
Table 2. Associations between care and health measures in june/july 2020 (COVID-19 wave 1).
shows results obtained when we considered health outcomes measured at the second wave of the data collection (full results available in Supplementary Table S3). In this case, results suggest that compared to those providing care only outside the household, respondents who cared for someone inside the household reported worse outcomes on all five measures considered. Results, in this case, are robust to controlling for both socioeconomic and demographic factors (Model 1) and pre-pandemic health (Model 2). In the fully-adjusted model that also controls for pre-pandemic measures of health, compared to those caring outside of the household, respondents who cared for someone inside the household were more likely to be depressed (OR = 1.67, 95% CI = 1.07–2.62), to report poor self-rated health (OR = 1.73, 95% CI = 1.09–2.73), to have high anxiety (OR = 2.21, 95% CI = 1.20–4.06), as well as to report lower quality of life (b = –0.854, 95% CI = −1.66 to −0.05) and lower life satisfaction (b = –0.433, 95% CI = –0.78 to −0.09).
Table 3. Associations between care and health measures in november/december 2020 (COVID-19 wave 2). results from fully-adjusted logistic and linear regression models.
Focus on co-residing carers
Focussing our attention on couples where both respondents provided valid data on their health, shows the health profile of both members in ‘caring’ and ‘non-caring’ couples. For this analysis, couples were matched based on sex, age, education, and wealth of the carer (with 60% of carers being female, mean age 75). As expected, respondents in receipt of care have considerably poorer health than their partners (who provide care for them) whereas non-caring couples tend to have similar health profiles. Also, partners who are cared for report poorer mental health profiles (except for loneliness) than those who are not in receipt of care from a spouse. Importantly, however, shows that—sex, age, education and wealth being equal—carers themselves are much more likely than non-carers to report disability (30% vs 14%), limiting long-term illness (40% vs 31%), to be shielding (26% vs 15%), to be clinically vulnerable to COVID-19 (47% vs 36%) as well as to be depressed (21% vs 15%) and to report lower quality of life (mean CASP-12 of 24.6 vs 26) and life satisfaction (mean of 6.9 vs 7.4).
Table 4. Percent health profile of couples Comparing couples where at least one provides care for the other, and where neither provides care.
Discussion
This paper investigated health and wellbeing of older carers using nationally representative data from ELSA including data collected pre-pandemic and during two COVID-19 Waves in June/July and November/December 2020. Importantly, this study has demonstrated that there are important differences on aggregate between those who have cared for someone inside the household throughout the period under study, and those who cared for someone outside the household or who were new to providing care. Within-household carers are much more likely to be older, themselves to struggle with activities of daily living, live with limiting longstanding illness, be clinically vulnerable to COVID-19 and disproportionately in the lowest wealth quintile.
Multivariate analysis showed that co-resident carers were overall more likely to report poor self-rated health and poorer mental health, both cross-sectionally and longitudinally, even accounting for pre-pandemic physical and mental health. While we do not have individual level information to include in these models, these findings are consistent with the notion that the prolonged conditions of the pandemic as described by others with disruptions to family visits and formal and local services (Giebel, Cannon, et al., Citation2021; Giebel, Hanna, et al., Citation2022; Price et al., Citation2022), and the prolonged period at home caring for sick and frail family members likely with little respite (Giebel, Lord, et al., Citation2021; Giebel, Pulford, et al., Citation2021; Giebel et al., Citation2020; Price et al., Citation2022), is likely to have contributed to the disproportionate deterioration in carers’ mental and general health on a number of dimensions. Reviews have also attributed poorer mental health to a range of potential contextual factors including worry about the health conditions of the person cared for, lack of access to health and care professionals and respite for carers, as well as more general feelings of fear, loss of control, and freedom (Giebel, Cannon, et al., Citation2021; Hanna et al., Citation2022; Sriram et al., Citation2021).
Recent reviews assessing the impact of the pandemic on those who cared for people living with dementia have found that they have experienced poor mental health during the pandemic (Giebel, Talbot, et al., Citation2023; Hughes et al., Citation2021). These results extend the empirical results to a wider group of older carers, adding needed longitudinal controls for pre-pandemic health to these analyses.
Given that those caring for someone inside the household seem to be reporting worse health among carers, in this paper we considered it important to gain a better understanding of who the older carers are caring for inside the household, and in particular how both their and their partner’s health compared to demographically similar households where no-one is providing care. Further investigation of the characteristics of co-resident spousal carers also shows that, compared with similar non-carers, they are also more likely to report poorer mental and physical health.
Strengths and limitations
We investigated associations between changes in informal care provision and mental health during the pandemic using a longitudinal approach. To our knowledge, this was the first study to investigate this issue drawing strength from using longitudinal data from the nationally-representative English Longitudinal Study of Ageing. Even controlling for demographic, socioeconomic factors, and pre-pandemic health, our analysis supports the idea that having to provide care to family members during the first months of the pandemic when social care and social support were limited was negatively associated with general health and mental health. This might relate to worries about the health of those cared for, lack of formal support, as well as uncertainty of not knowing how long this care burden would last (dictated by the pandemic itself and government responses that are largely beyond people’s control).
Our contribution, however, should be considered in light of some limitations. First, ELSA does not collect in the COVID-19 waves detailed information on caregiving activities and responsibilities (including personal care, general companionship, or practical help) nor on the changes in care needs of the care-recipient during the pandemic. Similarly, no information was collected on: the recipient of care; the reasons for informal care provision; the duration, regularity, and intensity of care provided; nor whether respondents started to care for someone living in the household since the start of the COVID-19 pandemic. Future studies, both quantitative and qualitative, are encouraged to investigate these aspects of care and how they relate to carers’ health. Second, in our study we used information only from the first wave of the COVID-19 sub-study because of inconsistencies in the questions asked in the second COVID-19 wave. Questions asked in November/December 2020 were restricted to those reporting informal care in June/July 2020 and referred to qualitative changes in amount of care since then (de facto, ‘changes’ of ‘changes’). Therefore, it was not possible to create meaningful patterns of care throughout the first nine months of the pandemic to assess whether and to what extent changes in caring commitments during the pandemic were associated with mental health. Third, although availability and access to formal care and social support services might have given respite to carers, ELSA did not collect this information nor asked whether respondents replaced paid care visits with help from other family members. Finally, as with all longitudinal surveys, ELSA also suffers from non-random cumulative attrition, with participants interviewed during the COVID-19 waves being more socioeconomically advantaged and having better health (based on pre-pandemic data) than those who were not. This is an unavoidable problem in longitudinal studies which was only partially corrected by using longitudinal weights in the analysis.
In summary, this study has highlighted an especially vulnerable group of older carers who are often understood to be somewhat invisible to policymakers and services (Carmichael & Ercolani, 2014; Greenwood, Pound, Smith, et al., Citation2019; Price et al., Citation2022). Yet their caring roles underpin much of the health and social care system, and are essential to the functioning of wider systems such as discharge from hospital (Limb, Citation2022). A breakdown of family care in these households is likely to lead to crisis admissions to hospital and residential care, all of which have been under extreme stress in the pandemic (Gray et al., Citation2022). It is therefore very important to address the needs of older carers in policy and services. This is so not only for reviews of Coronavirus legislation and professional and public understanding of unmet need, but also for us to understand appropriate responses to uses of guidance and regulation, access to health and social care, funding priorities, and systemic understanding of social care in the pandemic.
Author contributions
D Price had the initial idea for the study. Both authors equally contributed to the study design. G Di Gessa conducted the analyses. Both authors co-led the interpretation of results and revision of the analyses. D Price provided the initial draft of the manuscript; G Di Gessa contributed substantially to the manuscript drafting. Both authors contributed to revisions of the manuscript. Both authors have seen and approved the final version of the manuscript.
Supplemental Material
Download MS Word (57.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Banks, J., Batty, D., Breedvelt, J. J. F., Coughlin, K., Crawford, R., Marmot, M., Nazroo, J., Oldfield, Z., Steel, N., Steptoe, A., Wood, M., & Zaninotto, P. (2021). English longitudinal study of ageing: Waves 0–9, 1998–2019. (Version 36th Edition).UK Data Service. https://doi.org/10.5255/UKDA-SN-5050-23
- Bauer, J. M., & Sousa-Poza, A. (2015). Impacts of informal caregiving on caregiver employment, health, and family. Journal of Population Ageing, 8(3), 113–145. https://doi.org/10.1007/s12062-015-9116-0
- Bom, J., & Stöckel, J. (2021). Is the grass greener on the other side? The health impact of providing informal care in the UK and the Netherlands. Social Science & Medicine, 269, 113562. https://doi.org/10.1016/j.socscimed.2020.113562
- Booth, A., Reed, A. B., Ponzo, S., Yassaee, A., Aral, M., Plans, D., Labrique, A., & Mohan, D. (2021). Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PloS One, 16(3), e0247461. https://doi.org/10.1371/journal.pone.0247461
- Carmichael, F., & G. Ercolani, M. (2014). Overlooked and undervalued: The caring contribution of older people. International Journal of Social Economics, 41(5), 397–419. https://doi.org/10.1108/IJSE-02-2012-0046
- Derrer-Merk, E., Ferson, S., Mannis, A., Bentall, R., & Bennett, K. M. (2022). Older people’s family relationships in disequilibrium during the COVID-19 pandemic. What really matters? Ageing and Society, 2022, 1–18. https://doi.org/10.1017/S0144686X22000435
- Di Gessa, G., Bordone, V., & Arpino, B. (2023). Changes in grandparental childcare during the pandemic and mental health: Evidence from England. The Journals of Gerontology, 78(2), 319–329. https://doi.org/10.1093/geronb/gbac104
- Di Gessa, G., & Price, D. (2021). Changes in health and social well-being in the COVID-19 clinically vulnerable older English population during the pandemic. Journal of Epidemiology and Community Health, 75(11), 1070–1077. https://doi.org/10.1136/jech-2021-216405
- Di Gessa, G., & Price, D. (2022). The impact of shielding during the COVID-19 pandemic on mental health: Evidence from the English Longitudinal Study of Ageing. The British Journal of Psychiatry, 221(4), 637–643. https://doi.org/10.1192/bjp.2022.44
- Giebel, C., Cannon, J., Hanna, K., Butchard, S., Eley, R., Gaughan, A., Komuravelli, A., Shenton, J., Callaghan, S., Tetlow, H., Limbert, S., Whittington, R., Rogers, C., Rajagopal, M., Ward, K., Shaw, L., Corcoran, R., Bennett, K., & Gabbay, M. (2021). Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: A qualitative study. Aging & Mental Health, 25(7), 1281–1288. https://doi.org/10.1080/13607863.2020.1822292
- Giebel, C., Hanna, K., Callaghan, S., Cannon, J., Butchard, S., Shenton, J., Komuravelli, A., Limbert, S., Tetlow, H., Rogers, C., Eley, R., Rajagopal, M., Ward, K., & Gabbay, M. (2022). Navigating the new normal: Accessing community and institutionalised care for dementia during COVID-19. Aging & Mental Health, 26(5), 905–910. https://doi.org/10.1080/13607863.2021.1914545
- Giebel, C., Hanna, K., Cannon, J., Eley, R., Tetlow, H., Gaughan, A., Komuravelli, A., Shenton, J., Rogers, C., Butchard, S., Callaghan, S., Limbert, S., Rajagopal, M., Ward, K., Shaw, L., Whittington, R., Hughes, M., & Gabbay, M. (2020). Decision-making for receiving paid home care for dementia in the time of COVID-19: A qualitative study. BMC Geriatrics, 20(1), 333. https://doi.org/10.1186/s12877-020-01719-0
- Giebel, C., Hanna, K., Tetlow, H., Ward, K., Shenton, J., Cannon, J., Butchard, S., Komuravelli, A., Gaughan, A., Eley, R., Rogers, C., Rajagopal, M., Limbert, S., Callaghan, S., Whittington, R., Shaw, L., & Gabbay, M. (2021). “A piece of paper is not the same as having someone to talk to”: Accessing post-diagnostic dementia care before and since COVID-19 and associated inequalities. International Journal for Equity in Health, 20(1), 76. https://doi.org/10.1186/s12939-021-01418-1
- Giebel, C., Lord, K., Cooper, C., Shenton, J., Cannon, J., Pulford, D., Shaw, L., Gaughan, A., Tetlow, H., Butchard, S., Limbert, S., Callaghan, S., Whittington, R., Rogers, C., Komuravelli, A., Rajagopal, M., Eley, R., Watkins, C., Downs, M., … Gabbay, M. (2021). A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. International Journal of Geriatric Psychiatry, 36(3), 393–402. https://doi.org/10.1002/gps.5434
- Giebel, C., Pulford, D., Cooper, C., Lord, K., Shenton, J., Cannon, J., Shaw, L., Tetlow, H., Limbert, S., Callaghan, S., Whittington, R., Rogers, C., Komuravelli, A., Rajagopal, M., Eley, R., Downs, M., Reilly, S., Ward, K., Gaughan, A., … Gabbay, M. (2021). COVID-19-related social support service closures and mental well-being in older adults and those affected by dementia: A UK longitudinal survey. BMJ Open, 11(1), e045889. https://doi.org/10.1136/bmjopen-2020-045889
- Giebel, C., Talbot, C. V., Wharton, E., Lorenz-Dant, K., Suárez-González, A., Cannon, J., Tetlow, H., Lion, K. M., & Thyrian, J. R. (2023). The early impacts of COVID-19 on unpaid carers of people living with dementia: Part II of a mixed-methods systematic review. Aging & Mental Health, 27(3), 547–562. https://doi.org/10.1080/13607863.2022.2084510
- Gray, K. L., Birtles, H., Reichelt, K., & James, I. A. (2022). The experiences of care home staff during the COVID-19 pandemic: A systematic review. Aging & Mental Health, 26(10), 2080–2089. https://doi.org/10.1080/13607863.2021.2013433
- Greenwood, N., Pound, C., Brearley, S., & Smith, R. (2019). A qualitative study of older informal carers’ experiences and perceptions of their caring role. Maturitas, 124, 1–7. https://doi.org/10.1016/j.maturitas.2019.03.006
- Greenwood, N., Pound, C., Smith, R., & Brearley, S. (2019). Experiences and support needs of older carers: A focus group study of perceptions from the voluntary and statutory sectors. Maturitas, 123, 40–44. https://doi.org/10.1016/j.maturitas.2019.02.003
- Greenwood, N., & Smith, R. (2016). The oldest carers: A narrative review and synthesis of the experiences of carers aged over 75 years. Maturitas, 94, 161–172. https://doi.org/10.1016/j.maturitas.2016.10.001
- Hanna, K., Giebel, C., Tetlow, H., Ward, K., Shenton, J., Cannon, J., Komuravelli, A., Gaughan, A., Eley, R., Rogers, C., Rajagopal, M., Limbert, S., Callaghan, S., Whittington, R., Butchard, S., Shaw, L., & Gabbay, M. (2022). Emotional and mental wellbeing following COVID-19 public health measures on people living with dementia and carers. Journal of Geriatric Psychiatry and Neurology, 35(3), 344–352. https://doi.org/10.1177/0891988721996816
- Ho, F. K., Petermann-Rocha, F., Gray, S. R., Jani, B. D., Katikireddi, S. V., Niedzwiedz, C. L., Foster, H., Hastie, C. E., Mackay, D. F., Gill, J. M. R., O’Donnell, C., Welsh, P., Mair, F., Sattar, N., Celis-Morales, C. A., & Pell, J. P. (2020). Is older age associated with COVID-19 mortality in the absence of other risk factors? General population cohort study of 470,034 participants. PLoS One, 15(11), e0241824. https://doi.org/10.1371/journal.pone.0241824
- Hughes, M. C., Liu, Y., & Baumbach, A. (2021). Impact of COVID-19 on the health and well-being of informal caregivers of people with dementia: A rapid systematic review. Gerontology & Geriatric Medicine, 7, 23337214211020164. https://doi.org/10.1177/23337214211020164
- Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. https://doi.org/10.1177/0164027504268574
- Hyde, M., Wiggins, R. D., Higgs, P., & Blane, D. B. (2003). A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging & Mental Health, 7(3), 186–194. https://doi.org/10.1080/1360786031000101157
- Karim, J., Weisz, R., Bibi, Z., & Ur Rehman, S. (2015). Validation of the eight-item Center for Epidemiologic Studies Depression Scale (CES-D) among older adults. Current Psychology, 34(4), 681–692. https://doi.org/10.1007/s12144-014-9281-y
- Limb, M. (2022). Delayed discharge: How are services and patients being affected? BMJ, 376, o118. https://doi.org/10.1136/bmj.o118
- Liu, K. Y., Howard, R., Banerjee, S., Comas-Herrera, A., Goddard, J., Knapp, M., Livingston, G., Manthorpe, J., O’Brien, J. T., Paterson, R. W., Robinson, L., Rossor, M., Rowe, J. B., Sharp, D. J., Sommerlad, A., Suárez-González, A., & Burns, A. (2021). Dementia wellbeing and COVID-19: Review and expert consensus on current research and knowledge gaps. International Journal of Geriatric Psychiatry, 36(11), 1597–1639. https://doi.org/10.1002/gps.5567
- Manderbacka, K., Lahelma, E., & Martikainen, P. (1998). Examining the continuity of self-rated health. International Journal of Epidemiology, 27(2), 208–213. https://doi.org/10.1093/ije/27.2.208
- Muldrew, D. H. L., Fee, A., & Coates, V. (2022). Impact of the COVID-19 pandemic on family carers in the community: A scoping review. Health & Social Care in the Community, 30(4), 1275–1285. https://doi.org/10.1111/hsc.13677
- Onwumere, J., Creswell, C., Livingston, G., Shiers, D., Tchanturia, K., Charman, T., Russell, A., Treasure, J., Di Forti, M., Wildman, E., Minnis, H., Young, A., Davis, A., & Kuipers, E. (2021). COVID-19 and UK family carers: Policy implications. The Lancet, 8(10), 929–936. https://doi.org/10.1016/s2215-0366(21)00206-6
- Pavot, W., & Diener, E. (1993). Review of the satisfaction with life scale. Psychological Assessment, 5(2), 164–172. https://doi.org/10.1037/1040-3590.5.2.164
- Price, D., Drake, P., Allen, N., & Astbury, J. (2022). The impact of Care Act Easements under the Coronavirus Act 2020 on older carers supporting family members living with dementia at home. University of Manchester, NIHR Older People and Frailty Policy Research Unit.
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Sriram, V., Jenkinson, C., & Peters, M. (2021). Impact of COVID-19 restrictions on carers of persons with dementia in the UK: A qualitative study. Age and Ageing, 50(6), 1876–1885. https://doi.org/10.1093/ageing/afab156
- Steptoe, A., & Di Gessa, G. (2021). Mental health and social interactions of older people with physical disabilities in England during the COVID-19 pandemic: A longitudinal cohort study. The Lancet. Public Health, 6(6), e365–e373. https://doi.org/10.1016/S2468-2667(21)00069-4
- Tuijt, R., Frost, R., Wilcock, J., Robinson, L., Manthorpe, J., Rait, G., & Walters, K. (2021). Life under lockdown and social restrictions – The experiences of people living with dementia and their carers during the COVID-19 pandemic in England. BMC Geriatrics, 21(1), 301. https://doi.org/10.1186/s12877-021-02257-z
- Turvey, C. L., Wallace, R. B., & Herzog, R. (1999). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics, 11(2), 139–148. https://doi.org/10.1017/s1041610299005694
- Zivin, K., Llewellyn, D. J., Lang, I. A., Vijan, S., Kabeto, M. U., Miller, E. M., & Langa, K. M. (2010). Depression among older adults in the United States and England. The American Journal of Geriatric Psychiatry, 18(11), 1036–1044. https://doi.org/10.1097/JGP.0b013e3181dba6d2
