Abstract
Objective
Loneliness has been associated to a greater risk of cognitive decline and dementia in older individuals. However, evidence on whether this association also exists for older individuals who complain of cognitive problems is limited. We conducted a survey to examine the association between subjective cognitive decline in the working memory domain, perceived loneliness, depression, anxiety, and stress in older individuals with different profiles.
Methods
A total of 302 healthy, old individuals completed 3 questionnaires to assess subjective cognitive problems in attention, executive functions, storage, depression, anxiety, stress, and perceived loneliness.
Results
We conducted a cluster analysis and 3 clusters of individuals with different profiles emerged. Individuals with greater subjective cognitive problems (cluster 1) in the attention and storage domains, reported higher perceived loneliness and stress but not depression. In contrast, individuals with the least subjective cognitive problems (cluster 3) in the storage domain, reported lower perceived loneliness.
Conclusions
Individuals with higher subjective cognitive decline also report higher levels of perceived loneliness but not more depression than their peers. However, this correlation is present only for individuals with mild subjective cognitive decline (cluster 2). The implications for future research and interventions are discussed.
Introduction
Understanding what contributes to the emotional and cognitive wellbeing in ageing represents one of the key research challenges given the impact on society of the fast-growing number of older individuals. Considering the exposure to known dementia risks factors and the increase in population growth and ageing, Nichols et al. (Citation2022) estimated that by 2050 the number of people with dementia would increase by 102% in high income Countries, by 72% in Western Europe, and by 56% in Italy. It should not be surprising that improving our knowledge on how to contrast cognitive decline and dementia is among the top priorities identified by the World Health Organization (Citation2021). In fact, recent evidence shows that prevention measures aimed at reducing the impact of 12 known risks factors including low social contacts, could reduce by a good 40% the incidence of dementia onset (Baumgart et al., Citation2015; Livingston et al., Citation2020). This percentage could even be higher by contrasting the effects of perceived loneliness on cognition (e.g. Li et al., Citation2023), as the person’s needs for social contact may not always align with the frequency of contacts with others. That is, an individual may have few social contacts but be satisfied by them and not experience loneliness, whereas another individual may have many social contacts and yet feel lonely if these social connections are assessed as unfulfilling. This is because loneliness stems from the perception of being socially isolated and from being dissatisfied with current social relationships (Eisenberger & Lieberman, Citation2004). When individuals assess their need to belong as unfulfilled and their social relationships as lacking, loneliness (also known as emotional loneliness) is experienced as an aversive emotional state that acts as an alert signal for danger because it represents a higher risk to the individual’s survival. Therefore, loneliness motivates attempts at re-establishing satisfactory social contacts and triggers psychophysiological and psychological changes (Cacioppo, Cacioppo, Capitanio, & Cole, Citation2015; Cacioppo & Cacioppo, Citation2018; Hawkley & Cacioppo, Citation2010). Indeed, loneliness and the social pain it engenders rely on the same mechanisms and neural substrates as physical pain and this overlay occurs because the physical pain detection system was already developed when animals evolved to respond to social exclusion (e.g. Cacioppo & Cacioppo, Citation2018; Eisenberger & Lieberman, Citation2004). Accordingly, loneliness automatically triggers a set of neural, hormonal, behavioural and psychological interrelated changes including: (1) increased sleep fragmentation; (2) stress due to the increased activation of the hypothalamic-pituitary-adrenocortical (HPA) axis; (3) selective sympathetic immunity; (4) altered transcriptome dynamics; (5) decreased viral immunity; (6) increased inflammatory substrate; (7) increased prepotent responding, and (8) increased depressive symptomatology. Whereas such responses might be innocuous in the short term, in the long run they are associated with a 26% increase in the risk of premature mortality (Cacioppo & Hawkley, Citation2009; Hawkley & Cacioppo, Citation2010).
When considering the effects of perceived loneliness on cognition, evidence from young adults shows that it biases selective attention toward social threats, (e.g. Cacioppo et al., Citation2016), beyond the typical bias shown by young and old individuals (e.g. Viviani et al., Citation2022). In addition, perceived loneliness impairs memory for happy faces signalling social affiliation (e.g. Pizzio et al., Citation2022). In older individual, perceived loneliness enhances biological and psychological problems (e.g. Cacioppo, Cacioppo, Capitanio, Cole, Citation2015; Hawkley & Cacioppo, Citation2010), including the risk of cognitive decline (e.g. Duan et al., Citation2017; Lara et al., Citation2019; Luchetti et al., Citation2020; Tilvis et al., Citation2004; Wilson et al., Citation2007) and Alzheimer’s disease (e.g. Gow et al., Citation2007). Indeed, perceived loneliness has been linked to poorer processing speed, poorer memory (i.e. immediate, and delayed recall; for a review see Boss et al., Citation2015), poor planning and working memory, poor attention, and poor inhibition (e.g. Sin et al., Citation2021). Recent reviews of longitudinal and cross-sectional studies (Cardona & Andrés, Citation2023; Ren et al., Citation2023) conclude that there is evidence of a strong association between loneliness and poor cognition and that most likely changes in the activity of the HPA axis implicated in the stress response are involved (Ren et al., Citation2023). Moreover, Qiao et al. (Citation2022) in a recent meta-analysis of available studies concluded that evidence shows a link between loneliness and Alzheimer’s disease and dementia but not with mild cognitive impairment and vascular dementia. However, not only the directionality of the relationship might be bidirectional and complex, but the combination of cognitive and emotional problems can be very heterogeneous among older individuals, especially in the earlier phases before the impairment can be clinically detected. Indeed, it has been proposed that person-centred analyses, where participants are classified into profiles or clusters based on similar characteristics, may provide useful information on the common patterns of complaints within a person (e.g. Hanfelt et al., Citation2011). Finally, cognitive performance in older people has been typically assessed using different neuropsychological tests. However, older individuals who complain of cognitive problems often perform within the normal range on neuropsychological tests (Vannini et al., Citation2017). This phenomenon, known as subjective cognitive decline (SCD), refers to self-experienced persistent cognitive problems, compared to previously normal cognitive status, that are unrelated to an acute event and normal performance on standardised cognitive tests used to classify mild cognitive impairment, adjusted for age, sex, and education (Jessen et al., Citation2014, Citation2020; Neto & Nitrini Citation2016). Importantly, this operationalization has been proposed in the context of Alzheimer’s disease and it is not unanimous as different others are also used (Diaz-Galvan et al., Citation2021). Regardless of how subjective cognitive decline is assessed, there is some evidence of a link with perceived loneliness such that individuals who report higher loneliness also report higher subjective cognitive decline (e.g. Montejo et al., Citation2020; Pluim et al., Citation2023; Reynolds et al., Citation2022). However, some studies measured loneliness using a single item (e.g. Montejo et al., Citation2020), which may not be sensitive enough, leading to underreporting loneliness. Moreover, older individuals often present heterogenous combinations of cognitive and emotional complaints, especially in the earlier stages of cognitive changes. To fill this gap, we conducted a study to examine the relationship between perceived loneliness and subjective cognitive decline in attention, executive functions, and storage. As older individuals often report problems in maintaining information for short periods, we adopted a self-reported standardized instrument for working memory problems, which helps overcoming the limitations due to the little correspondence between how individuals perform at neuropsychological tests and how they perform in a real-world situation (e.g. Bottari et al., Citation2009). Therefore, in the present survey we used the Working Memory Questionnaire (WMQ: Vallat-Azouvi et al., Citation2012; Italian version: Guariglia et al., Citation2020), which taps on three dimensions of working memory, that is, short-term memory storage, attention, and executive control. Based on an opportunity sample of older individuals recruited through a wide network of retirement associations available on the territory, we adopted a clustering methodology based on self-reported cognitive problems as there are individual differences in the older population. This approach enabled us to define and characterise a group (cluster) profile of cognitive and emotional problems, as well as of living arrangements and pastime activities. By doing so in the present study, we built an empirical classification of the characteristics linked to greater self-reported emotional and cognitive difficulties in older individuals.
Method
Participants
An opportunistic sample of 820 older individuals (469 men and 320 women, 9 preferred not to say; age in year: M = 73.61; SD = 9.06; education in years: M = 8.56; SD = 4.02) who were members of Age Italia associations were invited to participate in the present study. Of these, 417 individuals agreed to complete the three questionnaires on loneliness, depression/anxiety/stress, and working memory (51% of the total sample). However, based on the health questionnaire, the data of 110 participants (13.41%) were excluded because of a) self-reported history of neurological or psychiatric disorders or substance use; b) been on anti-dementia medication. The data of 5 participants were also excluded because their age was 40 year or younger (0.6%). The final sample of healthy individuals consisted of 302 participants (177 men; 121 women, 4 preferred not to say), corresponding to the 36.83% of the total sample.
Measurements
We used a single questionnaire with 12 items on general health and 14 items on demographic, living arrangements, and pastimes, used by the AGE Italia association for their members. In addition, the Italian version of the WMQ (Guariglia et al., Citation2020), the Italian version of the Depression Anxiety Stress Scale (DASS, Bottesi et al., Citation2015), and the Italian version of the UCLA Loneliness Scale (Boffo et al., Citation2012) were used. There were 3 versions of the questionnaires to counterbalance the order of presentation of the WMQ, DASS, and UCLA Loneliness questionnaires. For WMQ, DASS, and UCLA Loneliness questionnaires, higher scores indicate more cognitive or emotional problems.
Procedure
The questionnaires were distributed through various pensioner associations linked to AGE Italia (for the complete list, please see Acknowledgments) in the period May-June 2021. Participants completed the demographic and general health questionnaire, and if they agreed to take part also in this survey, they completed the DASS, UCLA loneliness and WMQ questionnaires. All participants provided informed consent and were free to complete the questionnaires on site or take the questionnaires and bring them completed later on. The different associations collected the questionnaires, converted the paper questionnaires to pdf files, and sent them to the researchers. Data collections was completed by the end of September 2021.
Data analysis
Pre-processing
Two research assistants inputted the data in Excel and two researchers double checked for errors. Doubts and incongruencies were resolved together with the two research assistants.
Defining clusters
We implemented an exploratory cluster analysis to identify subgroups of participants with similar response patterns to the working memory questionnaire. Our cluster variables were working memory scores in three domains (attention domain, storage, and executive). We used k-means clustering, the most commonly unsupervised machine learning algorithm for partitioning a given data set into k groups. The basic idea of k-means clustering is to classify individuals based on high-intra-class similarity. We employed the standard algorithm for k-clustering, which defines the total within-cluster variation as the sum of squared distances Euclidean distances between items and the corresponding centroid (Hartigan & Wong, Citation1979).
We generated several models and contrasted them to determine the most appropriate structure for our data. Clusters were verified and evaluated by implementing an alternative clustering procedure (Fuzzy C-Means clustering) in which each data point could belong to more than one cluster. The graphical and clustering methods, validity criteria, and interpretability of each model were compared to determine the final cluster structure. They were also quantitatively evaluated on 30 cluster validity criteria within the ‘NbClust’ R package (Charrad, Ghazzali, Boiteau & Niknafs, Citation2014). We used the Bayesian Information Criterion (BIC) to validate the chosen cluster solution, which balances the number of model parameters and data points against the maximum likelihood function. We seek to find the number of model parameters that minimise the BIC (the clustering approach and results are detailed in Supplementary Materials, Note 1).
Cluster profiling
We started profiling by examining demographics, living arrangements and activities in each cluster. Next, we assessed Emotion state profiles for the clusters using a mixed ANOVA with Emotion state as a within-subject factor with three levels (Depression, Anxiety and Stress) and Cluster as a between-subject factor with Type III Sum of Squares. When the assumption of sphericity (as indicated by Mauchly’s test) was violated, we used Greenhouse-Geisser correction for degrees of freedom. Post Hoc comparisons were performed using Holmes correction for multiple comparisons. In addition, we performed corresponding Bayesian analysis to gain evidence for contrasts with pvalue ≥ .01. Similar, a mixed ANOVA with Working memory as a within-subject factor with three levels (Attention, Storage, Executive) and Cluster as a between-subject factor was carried out to examine working memory complaints in each cluster. Finally, we used a one-way between-subject ANOVA on loneliness scores to examine the loneliness profile in each cluster.
Results
Clustering
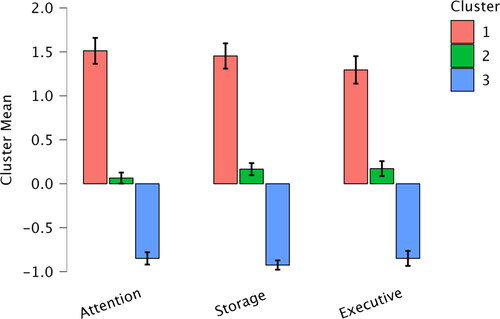
The results of our clustering procedures indicated that a three-cluster model appeared to be the most appropriate, accounting for 71.9% of the total variability in the model. Cluster 1 comprised 61 individuals, Cluster 2 consisted of 123 individuals and Cluster 3 included 118 participants. The input variables yielded a silhouette coefficient of 0.39, indicative of fair cluster homogeneity. To grasp an initial idea about how large the differences in each cluster are compared to the overall average of each working memory domain, we calculated the relative differences of each domain per cluster to the overall average (). Overall, Cluster 1 represents individuals who report more working memory problems and Cluster 3 represents individuals who report less working memory problems.
Demographic and living arrangement profiling
Overall, the three clusters represent individuals with similar age and education (elementary and medium school level) and a similar distribution of males and females, although Cluster 1 has slightly more individuals with high school education and fewer with university degree (see ). Cluster 1 has also a smaller group of individuals, fewer of which live with their partners. In contrast, Cluster 2 has more individuals who live with their partners and fewer who live alone. Cluster 3 has individuals whose characteristics are like those of individuals in Cluster 1 (e.g. living arrangements) and others that are similar to those of individuals in Cluster 2 (e.g. age).
Table 1. Demographic and living arrangement profiles* (percent).
Pastime profiling
The three clusters represent individuals with different profiles of pastime activities (see ). Cluster 1 represents older individuals with a few cultural or sports memberships, who report very few activities like dancing, exercising, or walking/trekking as their pastime. In contrast, Cluster 3 represents older individuals with several cultural or sports memberships but who report fewer pastime activities, somewhat similar to individuals in Cluster 1. Finally, Cluster 2 represents older individuals with many cultural or sports memberships who report often dancing, physical exercising, and walking/trekking as pastimes.
Table 2. Pastime profiles for the 3 clusters (values are percentages).
Emotion state profile
A mixed ANOVA with Emotion state (this term is used following the central concept of DASS to measure the negative emotional states of depression, anxiety and stress, Lovibond & Lovibond, Citation1995) as a within-subject factor with three levels (Depression, Anxiety and Stress) and Cluster as a between-subject factor revealed a main effect of Emotion state (F(1.94, 582.19) = 104.26, p < .001, ηp2 = 0.26), a main effect of Cluster (F(2,299) = 43.34, p < .001, ηp2 = 0.23). The interaction between Emotion state and Cluster was non-significant (F(3.89, 582.19) = 0.78, p = .53) ().
Figure 2. Mean scores on depression, anxiety, and stress in each Cluster. The error bars represent the standard error of the mean.
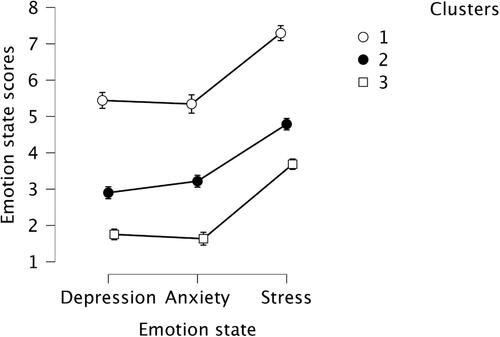
Post Hoc test showed that Cluster 1 yielded higher Emotional state scores compared to Cluster 2 (MD = 2.39, SE = 0.39, t = 6.11, pholm < .001, Cohen’s d = 0.83, 95% CI for Cohen’s d [0.49, 1.17]) and Cluster 3 (MD = 3.67, SE = 0.39, t = 9.31, pholm < .001, Cohen’s d = 1.27, 95% CI for Cohen’s d [0.92, 1.63]). Cluster 2 also showed higher scores on Emotional state than Cluster 3 (MD = 1.28, SE = 0.32, t = 3.97, pholm < .001, Cohen’s d = 0.44, 95% CI for Cohen’s d [0.17, 0.72]). Interestingly, across all clusters, the depression scores did not differ from anxiety scores (Cluster 1: MD = 0.09, SE = 0.32, t = .31, pholm = 1.0; Cluster 2: MD = 0.32, SE = 0.22, t = 1.42, pholm = .89; Cluster 3: MD = 0.12, SE = 0.23, t = .52, pholm = 1.0). Bayesian ANOVA confirmed the results of the classical ANOVA, showing evidence supporting the null hypothesis for no differences between depression and anxiety scores in each cluster (see details in Supplementary Materials, Note 2 (2.1)). Finally, stress scores were consistently higher than anxiety scores across the clusters (Cluster 1: MD = 1.95, SE = 0.32, t = 6.16, pholm < .001, Cohen’s d = 0.68, 95% CI for Cohen’s d [0.31, 1.04]; Cluster 2: MD = 1.57, SE = 0.22, t = 7.03, pholm < .001, Cohen’s d = 0.55, 95% CI for Cohen’s d [0.29, 0.81]; Cluster 3: MD = 2.05, SE = 0.23, t = 9.00, pholm < .001, Cohen’s d = 0.71, 95% CI for Cohen’s d [0.44, 0.98]). A Bayesian analysis provided evidence that the magnitude of these differences was similar across the clusters (BF01 = 8.91; see details in Supplementary Materials, Note 2 (2.2))
Working memory profile
A mixed ANOVA with Working memory domains (Attention, Storage, Executive) as a within-subject factor and Cluster as a between-subject factor revealed a main effect of Working memory (F(1.92, 574.06) = 3.64, pholm = .03, ηp2 = 0.01), a main effect of Cluster (F(2,299) = 660.27, pholm < .001, ηp2 = 0.82) and interaction between Working memory and Cluster (F(3.84, 574.06) = 9.78, pholm < .001, ηp2 = 0.06) ().
Figure 3. Mean scores of working memory problems in three domains (Attention, Storage and Executive). the error bars represent the standard error of the means.
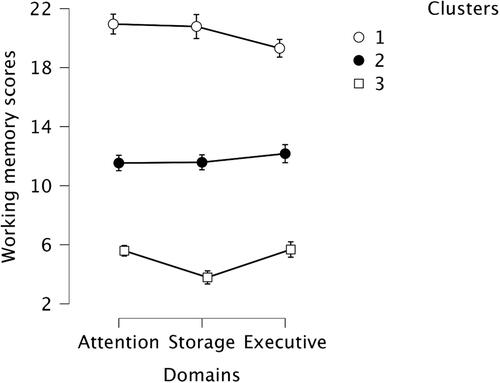
The interaction between Working memory and Cluster was driven by different patterns of working memory problems reported by individuals in Clusters 1 and 3. At the same time, no differences between Attention, Storage and Executive were found for individuals in Cluster 2 (MD = 0.63, SE = 0.35, t = 1.79, pholm = .37; MD = 0.59, SE = 0.35, t = 1.65, pholm = .39; MD = 0.05, SE = 0.35, t = 0.14, pholm = 1.0). It must be noted, however, that in Cluster 2, a Bayesian analysis was inconclusive in quantifying evidence to support the null hypothesis (BF01 = 2.49, BF01 = 2.33, BF01 = 2.85 respectively) (see details in Supplementary Materials, Note 2 (2.3)).
In Cluster 1, participants reported fewer problems in the Executive compared to the Storage (MD = −1.48, SE = 0.50, t = −2.94, pholm = .02, Cohen’s d = −0.42, 95% CI for Cohen’s d [0.88, 0.04]) and Attention domains (MD = −1.64, SE = 0.50, t = − 3.27, pholm = 0.008, Cohen’s d = − 0.47, 95% CI for Cohen’s d [-0.93, −0.04]) while there was no difference between Attention and Storage domains (MD = 0.65, SE = 0.50, t = 1.08, pholm = .57, BF01 = 4.61). In contrast, participants in Cluster 3 reported fewer problems in the Storage domain compared to the Attention domain (MD = −1.81, SE = 0.36, t = −5.0, pholm < .001, Cohen’s d = −0.51, 95% CI for Cohen’s d [-0.85, −0.18]) and Executive domain (MD = −1.89, SE = 0.36, t = −5.24, pholm < .001, Cohen’s d = −0.54, 95% CI for Cohen’s d [-0.87, −0.20]). The difference between Attention and Executive domains did not reach significance (MD = 0.09, SE = 0.36, t = 0.24, pholm = 1.0, BF01 = 9.46).
Overall, Cluster 3 showed significantly fewer problems in working memory compared to Cluster 1 (MD = −15.33, 95% CI for MD [-16.36, −14.31], SE = 0.43, t = − 36.02, pholm < .001, Cohen’s d = − 4.35 95% CI for Cohen’s d [-4.87, −3.83]) and Cluster 2 (MD = −6.74, 95% CI for MD [-7.58, −5.91], SE = 0.35, t = − 19.39, pholm < .001, Cohen’s d = − 1.92 95% CI for Cohen’s d [-2.22, −1.61]). Participants in Cluster 1 reported more working memory issues compared to Cluster 2 (MD = 8.59, 95% CI for MD [7.59, 9.60], SE = 0.42, t = 20.31, pholm < .001, Cohen’s d = 2.44 95% CI for Cohen’s d [2.06, 2.81]) ().
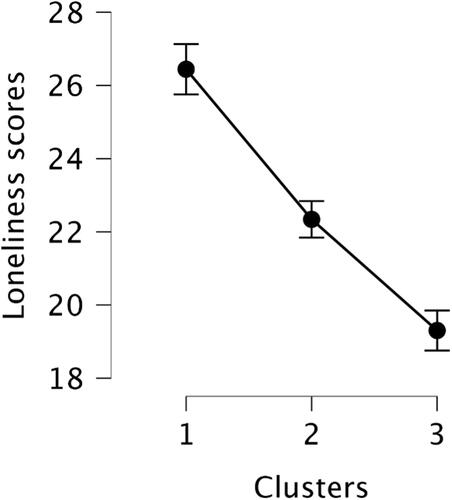
Loneliness profile
We calculated loneliness scores measured by UCLA for each cluster and submitted them to a one-way between-subject ANOVA. Levene’s test indicated that the assumption of equal variances for UCLA scores across the clusters was not violated (F(2,299) = 0.45, p = .64). There was a main effect of Cluster on UCLA scores (F(2,299) = 32.35, p < .001, ηp2 = 0.18), (). A bootstrapped Post Hoc test based on 1000 successful replicates showed that participants in Cluster 1 had the highest loneliness scores compared to participants in Cluster 2 (MD = 4.13, 95% CI for MD [2.43, 4.13], SE = 0.86, t = 4.62, pholm < .001, Cohen’s d = 0.72, 95% CI for Cohen’s d [0.34, 1.11]) and Cluster 3 (MD = 7.10, 95% CI for MD [5.47, 8.91], SE = 0.87, t = 7.99, pholm < .001, Cohen’s d = 1.26, 95% CI for Cohen’s d [0.86, 1.66]). Individuals in Cluster 3 had lower loneliness scores compared to Cluster 2 (MD = − 2.99, 95% CI for MD [-1.63, − 4.48], SE = 0.72, t = − 4.16, pholm < .001, Cohen’s d = − 0.54, 95% CI for Cohen’s d [-0.22, −0.85]).
The association between working memory, emotion state and loneliness profiles
To test the association between working memory, emotion state and loneliness profiles in each cluster, we carried out a Spearman’s correlation and assessed evidence for positive or negative associations using a Bayesian approach. displays the associations with reliable evidence (BF10 > 10). Full correlation analysis is reported in Supplementary Materials (Note 3). The results indicated a cluster-specific correlation pattern across the variables.
Figure 5. Spearman’s rho between working memory, emotion state and loneliness variables.
*BF10 > 10; **BF10 > 100; ***BF10 > 1000
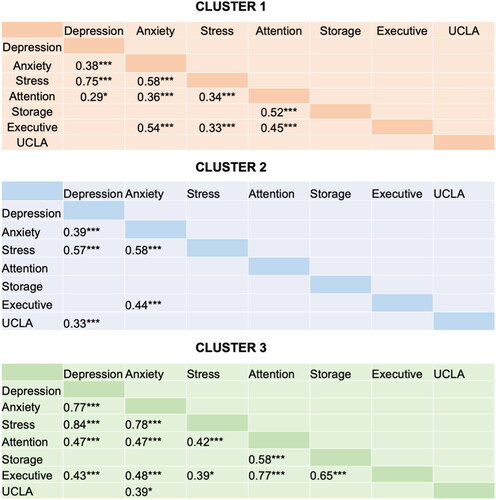
Clusters 1 and 3 showed similar association pattern between working memory and emotion state. Specifically, for these clusters all emotion dimensions positively correlated with problems in attention but not with problems in storage domain. However, Cluster 3 showed strong associations between problems in executive functioning and depression and between executive functioning and storage. These two associations were absent in Cluster 1, this is the cluster with individuals who report higher levels of working memory problems. Individuals in Cluster 2 showed no association between emotion state and working memory problems excluding a positive correlation between anxiety and executive functioning. The later relationship indicated that increasing anxiety was associated with reports of poorer executive functions. Moreover, individuals in Cluster 2 showed weak but reliable positive association between loneliness scores and depression whereas individuals in Cluster 3 showed weak, positive association between loneliness and anxiety ().
Discussion
Loneliness has been identified as one of the risk factors for cognitive decline in older individuals, but the available evidence has limitations, including that often cognitive performance is assessed using instruments that cannot detect subtle changes that may be precursors of more substantial problems. Most importantly, older individuals often present very heterogeneous cognitive and emotional complaints. Here, we aimed to fill this gap by providing insight into the association between subjective cognitive decline in the working memory domain, perceived loneliness, anxiety, depression, and stress for different profiles (i.e. clusters) of older, healthy individuals. Most previous studies into the relationship between these variables relaxed the assumption of heterogeneous subpopulations within a study sample, but it is reasonable to assume that self-reported cognitive problems may not appeal equally to the entire population. Therefore, we probed for the relationship between perceived loneliness, anxiety, depression, and stress by exploring patterns of individual differences within our sample using k-means clustering.
Based on self-reported cognitive problems, we could isolate clusters of individuals characterized by three different profiles. The profile of older individuals in cluster 1 with more problems overall, especially in the attention and storage domains, and higher perceived loneliness. However, despite these complaints, these individuals did not report more anxiety or depression than individuals in the other two clusters. This is important as past findings suggest that cognitive complaints—and especially memory and executive functions complaints—may reflect depressed mood rather than poor cognitive performance (e.g. Bolla et al., Citation1991; Lockwood et al., Citation2000; Philippot & Agrigoroaei, Citation2017). As the present findings show no differences in depression between the profile of older individuals with higher subjective cognitive decline and perceived loneliness (cluster 1) and the profile of older individuals with the lowest subjective cognitive decline and perceived loneliness (cluster 3), an account in terms of greater depression and anxiety for older individuals in cluster 1 seems unlikely. This is in keep with past findings showing that the relationship between loneliness and cognitive ability is significant after controlling for clinical depression (Holwerda et al., Citation2014; O’Luanaigh et al., Citation2012). Therefore, individuals in cluster 1 and cluster 3 have mirror profiles with regard to subjective cognitive decline and perceived loneliness, while they do not differ on depression. Importantly, this is not the case for older individuals in cluster 2, who had profiles of subjective cognitive decline, emotions and perceived loneliness that were in between those of their peers in the two other clusters as in this case depression correlated with perceived loneliness. Considering that depression and depressive symptomatology represent a risk factor for cognitive decline in older adults (Shahnawaz et al., Citation2013; Zlatar, Moore, Palmer, Thompson, & Jeste, 2014), future studies assessing the different developmental paths for individuals with this profile may provide useful insight.
In sum, the present findings point to three different profiles of subjective cognitive decline and perceived loneliness in older individuals, where only older individuals in cluster 2—representing more individuals who live with their partners, with some cultural and sport activities, and who report mild levels of subjective cognitive problems—show a positive relation between perceived loneliness and depression. The profiles of older individuals in cluster 3—i.e. fewer individuals living with their partners, with more cultural and sport activities, and who report the least subjective cognitive problems—show a positive relation between perceived loneliness and anxiety. By contrast, for the profile of older individuals in cluster 1—i.e. more individuals living alone, with some cultural and sport activities, and who report the most subjective cognitive problems and perceived loneliness –we did not find any meaningful relation between perceived loneliness and depression or anxiety. It is also interesting that for individuals in cluster 1 perceived loneliness did not correlate with cognitive and emotional problems. The only association present for older individuals with this profile is between anxiety, stress and subjective cognitive problems in the attention and executive domain, whereas depression had a small association (r= .29) only with problems in the attention domain. These links can be bidirectional as they may indicate that being emotionally distressed affects cognitive functions or that experiencing cognitive problems enhances emotional distress. In fact, as discussed earlier, it is well recognized in literature that cognitive functions—especially working memory, episodic memory, and executive functions—are affected by depression (Chen et al., Citation2022), stress (Guo et al., Citation2022) and anxiety (Chen et al., Citation2022). However, it is also well recognized that the presence of even mild cognitive problems is frequently associated with emotional distress (Apostolova & Cummings, Citation2008). That in the present study the correlations fail to show a direct relationship between perceived loneliness and subjective cognitive decline could be due to this being an indirect link, mediated by the sharpening effect of emotional distress. Such an account would be in keeping with the profile of perceived loneliness and depression for individuals in cluster 2 (i.e. with milder levels of self-reported cognitive problems) and the profile of perceived loneliness and anxiety for individuals in cluster 3 but no association with self-reported working memory problems in any clusters. Although past studies have shown that chronic loneliness increases the risks for depression and anxiety (Cacioppo et al., Citation2010) and that depression is a mediator for the relationship between loneliness and cognitive functions (McHugh Power et al., Citation2020; but see Sin et al., Citation2021 for the effect of loneliness on cognition even after controlling for depression), the present findings point an association with stress and anxiety rather than depression, at least for the two clusters (cluster 1 and cluster 3) with mirror profiles of subjective cognitive decline and perceived loneliness. The present findings are in line with Donovan and Blazer (Citation2020) who have isolated three categories of mediators—behavioural, psychological, and biological—that contribute to the impact of loneliness on healthy ageing, with stress being the main psychological moderator. This pattern points to a possible role of anxiety and stress response as a possible underlying mechanisms for the association between loneliness and poor cognition (Ren et al., Citation2023).
Finally, it should be noted that by using the clustering approach here, we did not intend to define unique profiling that could be generalised to the whole population. Instead, our results indicated that identifying groups of older people based on their subjective cognitive difficulties can be a way forward to address loneliness and mood disorder issues while accounting for heterogeneity in the older population. Therefore, the present findings could guide future studies—especially longitudinal studies—in establishing whether prolonged perceived loneliness can accentuate the progression from subjective cognitive decline, with un-impaired performance on neuropsychological tests, to a diagnosis of cognitive decline (e.g. Jessen et al., Citation2014; Reisberg et al., Citation2010). Similarly, the 3 clusters of different profiles may provide important insight for future research on the impact of intervention programs. For instance, recent findings show that the likelihood of years spent with healthy cognition decreases with increasing loneliness (Li et al., Citation2023). A key question for future research is to what extent measures aimed at contrasting or preventing loneliness may assist individuals with moderate levels of loneliness and subjective cognitive decline (i.e. similar to the profile of individuals in cluster 2) to progress toward a healthier profile (i.e. similar to the profile of individuals in cluster 3), with lower subjective cognitive decline. By the same token, interventions aimed at reducing the loneliness may help preventing a progression toward a poorer cognitive and emotional profile (i.e. similar to the profile of individuals in cluster 1), with the highest report of problems. Moreover, the success of potential intervention measures may well vary depending on the specific profile, as individuals with cluster 2 profiles may benefit more from interventions aimed at providing opportunities to establish new, meaningful relationships with people based on shared activities and interests (see Rodríguez-Romero et al., Citation2021). In contrast, individuals with cluster 1 profiles may benefit more from interventions that first provide support and then promote and encourage behaviours aimed at establishing new, meaningful relationships (for recent reviews, see Galvez-Hernandez et al., Citation2022; Thompson et al., Citation2023). The present findings could guide future research in planning interventions aimed at promoting healthy ageing and contrasting the progression from subjective cognitive decline to cognitive decline and dementia.
The present survey entails a few limitations that should be acknowledged. The findings represent individuals who are members of Age Italia associations, offering different services and assistance but also organizing activities in which members can take part. Therefore, it does not represent older individuals who do not have these possibilities and less occasions to connect with others and receive less support. In addition, the present findings represent only individuals who volunteered to complete the survey and were in good general health. This inevitably introduces a bias as individuals who are unwell and/or feel lonelier and for a longer time may be more withdrawn and less available to participate in various activities, including a survey. Our sample also represented more men than women and this may simply reflect the distribution of people who accessed the associations during that period of time. If at all, that our sample had more men than women may underestimate the effects we report as subjective cognitive decline is more common in women (Reynolds et al., Citation2022) whereas a recent met-analysis shows that there are no gender differences in reporting loneliness (Maes et al. Citation2019). However, our findings are limited to the attention and executive functions domains as we did not assess self-reported problems in other domains, including memory. Although, it should also be noted that a recent neuroimaging study using a large cohort of old individuals (N = 1468, over 60 years old) reported no association between loneliness and memory performance (Solé-Padullés et al., Citation2022). This study found no significant brain correlates of loneliness with hippocampal volume change or cortical thinning, indicating that the association between loneliness and memory does not characterise healthy ageing. In general, even with these limitations, the present s findings have the potential to help future longitudinal studies formulate data-driven hypotheses that help clarify the links between perceived loneliness, subjective cognitive decline, and emotional well-being.
In conclusion, the present study demonstrated that drawing inferences about the relationship between perceived loneliness and subjective cognitive functioning in older individuals extends beyond a common one-size-fits-all approach. The substantial variations in self-reported cognitive problems were associated with distinct emotional and loneliness profiles. We suggest that identifying the hidden patterns by clustering similarities within the older cohort may help to reconstruct a possible underlying data structure which is essential to draw conclusions and evaluating a prospective intervention. This is an important step in the process aimed at reducing the risk of cognitive decline and promoting healthy ageing, which must also involve contrasting the feeling of being lonely.
Supplemental Material
Download MS Word (2.5 MB)Acknowledgments
we would like to thank Maria Ruffino, who was president of AgeItalia during the study and the following associations, which are part of AgeItalia, for data collection: Federpensionati Coldiretti; Organizzazione ANP-CIA; Organizzazione ANPA Pensionati Confagricoltura; Organizzazione ANAP Confartigianato; Organizzazione CONFEURO; Associazione LAVORO - Over 40- APS; Associazione USCIRE Insieme onlus; Associazione ATDAL over 40; Associazione 50&più
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Apostolova, L. G., & Cummings, J. L. (2008). Neuropsychiatric manifestations in mild cognitive impairment: A systematic review of the literature. Dementia and Geriatric Cognitive Disorders, 25(2), 115–126. https://doi.org/10.1159/000112509[PMC]
- Baumgart, M., Snyder, H. M., Carrillo, M. C., Fazio, S., Kim, H., & Johns, H. (2015). Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 11(6), 718–726. https://doi.org/10.1016/j.jalz.2015.05.016
- Boffo, M., Mannarini, S., & Munari, C. (2012). Exploratory structure equation modelling of the UCLA loneliness scale: A contribution to the Italian adaptation. TPM Testing Psychometrics Methodology in Applied Psychology, 19(4), 345–363. https://doi.org/10.4473/TPM19.4.7
- Bolla, K. I., Lindgren, K. N., Bonaccorsy, C., & Bleecker, M. L. (1991). Memory complaints in older adults: Fact or fiction? Archives of Neurology, 48(1), 61–64. https://doi.org/10.1001/archneur.1991.00530130069022
- Boss, L., Kang, D. H., & Branson, S. (2015). Loneliness and cognitive function in the older adult: A systematic review. International Psychogeriatrics, 27(4), 541–553. https://doi.org/10.1017/S1041610214002749
- Bottari, C., Dassa, C., Rainville, C., & Dutil, E. (2009). The factorial validity and internal consistency of the Instrumental Activities of Daily Living Profile in individuals with a traumatic brain injury. Neuropsychological Rehabilitation, 19(2), 177–207. https://doi.org/10.1080/09602010802188435
- Bottesi, G., Ghisi, M., Altoè, G., Conforti, E., Melli, G., & Sica, C. (2015). The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Comprehensive Psychiatry, 60, 170–181. https://doi.org/10.1016/j.comppsych.2015.04.005
- Cacioppo, J. T., Cacioppo, S., Capitanio, J. P., & Cole, S. W. (2015). The neuroendocrinology of social isolation. Annual Review of Psychology, 66, 733–767. https://doi.org/10.1146/annurev-psych-010814-015240
- Cacioppo, J. T., Hawkley, L. C., & Thisted, R. A. (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. https://doi.org/10.1037/a0017216.
- Cacioppo, J. T., & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. https://doi.org/10.1016/j.tics.2009.06.005
- Cacioppo, J. T., & Cacioppo, S. (2018). The growing problem of loneliness. Lancet (London, England), 391(10119), 426. https://doi.org/10.1016/S0140-6736(18)30142-9
- Cacioppo, J. T., & Cacioppo, S. (2018). Loneliness in the modern age: An evolutionary theory of loneliness (ETL). In J. M. Olson (Ed.), Advances in Experimental Social Psychology (vol. 58, pp. 127–197). Academic Press. https://doi.org/10.1016/bs.aesp.2018.03.003
- Cacioppo, S., Bangee, M., Balogh, S., Cardenas-Iniguez, C., Qualter, P., & Cacioppo, J. T. (2016). Loneliness and implicit attention to social threat: A high-performance electrical neuroimaging study. Cognitive Neuroscience, 7(1-4), 138–159. https://doi.org/10.1080/17588928.2015.1070136
- Cardona, M., & Andrés, P. (2023). Are social isolation and loneliness associated with cognitive decline in ageing? Frontiers in Aging Neuroscience, 15, 1075563. https://doi.org/10.3389/fnagi.2023.1075563
- Charrad, M., Ghazzali, N., Boiteau, V., & Niknafs, A. (2014). NbClust: An R package for determining the relevant number of clusters in a data set. Journal of Statistical Software, 61(6), 1–36. https://doi.org/10.18637/jss.v061.i06
- Chen, Y., Hu, N., Yang, J., & Gao, T. (2022). Prefrontal cortical circuits in anxiety and fear: An overview. Frontiers of Medicine, 16(4), 518–539. https://doi.org/10.1007/s11684-022-0941-2
- Diaz-Galvan, P., Ferreira, D., Cedres, N., Falahati, F., Hernández-Cabrera, J. A., Ames, D., Barroso, J., & Westman, E. (2021). Comparing different approaches for operationalizing subjective cognitive decline: Impact on syndromic and biomarker profiles. Scientific Reports, 11(1), 4356. https://doi.org/10.1038/s41598-021-83428-1
- Donovan, N. J., & Blazer, D. (2020). Social isolation and loneliness in older adults: Review and commentary of a national academies report. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 28(12), 1233–1244. https://doi.org/10.1016/j.jagp.2020.08.005
- Duan, D., Dong, Y., Zhang, H., Zhao, Y., Diao, Y., Cui, Y., Wang, J., Chai, Q., & Liu, Z. (2017). Empty-nest-related psychological distress is associated with progression of brain white matter lesions and cognitive impairment in the elderly. Scientific Reports, 7, 43816. https://doi.org/10.1038/srep43816
- Eisenberger, N. I., & Lieberman, M. D. (2004). Why rejection hurts: A common neural alarm system for physical and social pain. Trends in Cognitive Sciences, 8(7), 294–300. https://doi.org/10.1016/j.tics.2004.05.010
- Galvez-Hernandez, P., González-de Paz, L., & Muntaner, C. (2022). Primary care-based interventions addressing social isolation and loneliness in older people: A scoping review. BMJ Open, 12(2), e057729. https://doi.org/10.1136/bmjopen-2021-057729
- Gow, A. J., Pattie, A., Whiteman, M. C., Whalley, L. J., & Deary, I. J. (2007). Social support and successful aging: Investigating the relationships between lifetime cognitive change and life satisfaction. Journal of Individual Differences, 28(3), 103–115. https://doi.org/10.1027/1614-0001.28.3.103
- Guariglia, P., Giaimo, F., Palmiero, M., & Piccardi, L. (2020). Normative data and validation of the Italian translation of the Working Memory Questionnaire (WMQ). Applied Neuropsychology. Adult, 27(4), 376–389. https://doi.org/10.1080/23279095.2018.1552147
- Guo, H., Zheng, L., Xu, H., Pang, Q., Ren, Z., Gao, Y., & Wang, T. (2022). Neurobiological links between stress, brain injury, and disease. Oxidative Medicine and Cellular Longevity, 2022, 8111022. https://doi.org/10.1155/2022/8111022
- Hanfelt, J. J., Wuu, J., Sollinger, A. B., Greenaway, M. C., Lah, J. J., Levey, A. I., & Goldstein, F. C. (2011). An exploration of subgroups of mild cognitive impairment based on cognitive, neuropsychiatric, and functional features: Analysis of data from the National Alzheimer’s Coordinating Center. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 19(11), 940–950. https://doi.org/10.1097/JGP.0b013e31820ee9d2
- Hartigan, J. A., & Wong, M. A. (1979). Algorithm AS 136: A K-means clustering algorithm. Journal of the Royal Statistical Society. Series C (Applied Statistics), 28(1), 100–108. https://doi.org/10.2307/2346830
- Hawkley, L. C., & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine: A publication of the Society of Behavioral Medicine, 40(2), 218–227. https://doi.org/10.1007/s12160-010-9210-8
- Holwerda, T. J., Deeg, D. J., Beekman, A. T., van Tilburg, T. G., Stek, M. L., Jonker, C., & Schoevers, R. A. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam Study of the Elderly (AMSTEL). Journal of Neurology, Neurosurgery, and Psychiatry, 85(2), 135–142. https://doi.org/10.1136/jnnp-2012-302755
- Jessen, F., Amariglio, R. E., van Boxtel, M., Breteler, M., Ceccaldi, M., Chételat, G., Dubois, B., Dufouil, C., Ellis, K. A., van der Flier, W. M., Glodzik, L., van Harten, A. C., de Leon, M. J., McHugh, P., Mielke, M. M., Molinuevo, J. L., Mosconi, L., Osorio, R. S., Perrotin, A., … Wagner, M. (2014). A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 10(6), 844–852. https://doi.org/10.1016/j.jalz.2014.01.001
- Jessen, F., Amariglio, R. E., Buckley, R. F., van der Flier, W. M., Han, Y., Molinuevo, J. L., Rabin, L., Rentz, D. M., Rodriguez-Gomez, O., Saykin, A. J., Sikkes, S. A. M., Smart, C. M., Wolfsgruber, S., & Wagner, M. (2020). The characterisation of subjective cognitive decline. The Lancet. Neurology, 19(3), 271–278. https://doi.org/10.1016/s1474-4422(19)30368-0
- Lara, E., Caballero, F. F., Rico-Uribe, L. A., Olaya, B., Haro, J. M., Ayuso-Mateos, J. L., & Miret, M. (2019). Are loneliness and social isolation associated with cognitive decline? International Journal of Geriatric Psychiatry, 34(11), 1613–1622. https://doi.org/10.1002/gps.5174
- Lara, E., Martín-María, N., De la Torre-Luque, A., Koyanagi, A., Vancampfort, D., Izquierdo, A., & Miret, M. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Research Reviews, 52, 7–16. https://doi.org/10.1016/j.arr.2019.03.002
- Li, S., Zhang, M., Han, D., Wu, Y., Zhao, J., Liao, H., Ma, Y., Yan, C., & Wang, J. (2023). The effects of loneliness and social isolation on cognitive impairment-free life expectancy in older adults. Aging & Mental Health, 1–8. https://doi.org/10.1080/13607863.2023.2191926
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (London, England), 396(10248), 413–446. https://doi.org/10.1016/s0140-6736(20)30367-6
- Lockwood, K. A., Alexopoulos, G. S., Kakuma, T., & Van Gorp, W. G. (2000). Subtypes of cognitive impairment in depressed older adults. The American Journal of Geriatric Psychiatry, 8(3), 201–208. https://doi.org/10.1097/00019442-200008000-00004
- Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-u
- Luchetti, M., Terracciano, A., Aschwanden, D., Lee, J. H., Stephan, Y., & Sutin, A. R. (2020). Loneliness is associated with risk of cognitive impairment in the survey of health, ageing and retirement in Europe. International Journal of Geriatric Psychiatry, 35(7), 794–801. https://doi.org/10.1002/gps.5304
- Maes, M., Qualter, P., Vanhalst, J., Van den Noortgate, W., & Goossens, L. (2019). Gender differences in loneliness across the lifespan: A meta–analysis. European Journal of Personality, 33(6), 642–654. https://doi.org/10.1002/per.2220
- McHugh Power, J., Tang, J., Kenny, R. A., Lawlor, B. A., & Kee, F. (2020). Mediating the relationship between loneliness and cognitive function: The role of depressive and anxiety symptoms. Aging & Mental Health, 24(7), 1071–1078. https://doi.org/10.1080/13607863.2019.1599816
- Montejo, P., Prada, D., Pedrero-Perez, E., & Montenegro-Pena, M. (2020). Subjective cognitive decline: Mental health, loneliness, pain and quality of life. Poblational study. Journal of Aging Science, 8, 218. https://doi.org/10.35248/2329-8847.20.08.218
- Neto, S. A., & Nitrini, R. (2016). Subjective cognitive decline: The first clinical manifestation of Alzheimer’s disease? Dementia & Neuropsychologia, 10(3), 170–177. https://doi.org/10.1590/s1980-5764-2016dn1003002
- Nichols, E., Steinmetz, J. D., Vollset, S. E., Fukutaki, K., Chalek, J., Abd-Allah, F., Abdoli, A., Abualhasan, A., Abu-Gharbieh, E., Akram, T. T., Al Hamad, H., Alahdab, F., Alanezi, F. M., Alipour, V., Almustanyir, S., Amu, H., Ansari, I., Arabloo, J., Ashraf, T., … Vos, T. (2022). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health, 7(2), e105–25–e125. https://doi.org/10.1016/S2468-2667(21)00249-8
- O’Luanaigh, C., O’Connell, H., Chin, A.-V., Hamilton, F., Coen, R., Walsh, C., Walsh, J. B., Caokley, D., Cunningham, C., & Lawlor, B. A. (2012). Loneliness and cognition in older people: The Dublin healthy ageing study. Aging & Mental Health, 16(3), 347–352. https://doi.org/10.1080/13607863.2011.628977
- Philippot, P., & Agrigoroaei, S. (2017). Repetitive thinking, executive functioning, and depressive mood in the elderly. Aging & Mental Health, 21(11), 1192–1196. https://doi.org/10.1080/13607863.2016.1211619
- Pizzio, A. P. G., Yankouskaya, A., Alessandri, G., Loreto, S., & Pecchinenda, A. (2022). Social contacts and loneliness affect the own age bias for emotional faces. Scientific Reports, 12(1), 16134. https://doi.org/10.1038/s41598-022-20220-9
- Pluim, C. F., Anzai, J. A. U., Martinez, J. E., Munera, D., Garza-Naveda, A. P., Vila-Castelar, C., Guzmán-Vélez, E., Ramirez-Gomez, L., Bustin, J., Serrano, C. M., Babulal, G. M., Okada de Oliveira, M., & Quiroz, Y. T. (2023). Associations among loneliness, purpose in life and subjective cognitive decline in ethnoracially diverse older adults living in the United States. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 42(3), 376–386. https://doi.org/10.1177/07334648221139479
- Qiao, L., Wang, G., Tang, Z., Zhou, S., Min, J., Yin, M., & Li, M. (2022). Association between loneliness and dementia risk: A systematic review and meta-analysis of cohort studies. Frontiers in Human Neuroscience, 16, 899814. https://doi.org/10.3389/fnhum.2022.899814
- Reynolds, G. O., Manning, L., Kirn, D., Klein, H., Hampton, O., Burke, O., Jr, Buckley, R., Rentz, D., Sperling, R., Marshall, G. A., & Amariglio, R. E. (2022). Subjective cognitive decline in a registry sample: Relation to psychiatric history, loneliness, and personality. The Journal of Prevention of Alzheimer’s Disease, 9(3), 435–440. https://doi.org/10.14283/jpad.2022.31
- Reisberg, B., Shulman, M. B., Torossian, C., Leng, L., & Zhu, W. (2010). Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 6(1), 11–24. https://doi.org/10.1016/j.jalz.2009.10.002
- Ren, Y., Savadlou, A., Park, S., Siska, P., Epp, J. R., & Sargin, D. (2023). The impact of loneliness and social isolation on the development of cognitive decline and Alzheimer’s Disease. Frontiers in Neuroendocrinology, 69, 101061. https://doi.org/10.1016/j.yfrne.2023.101061
- Rodríguez-Romero, R., Herranz-Rodríguez, C., Kostov, B., Gené-Badia, J., & Sisó-Almirall, A. (2021). Intervention to reduce perceived loneliness in community-dwelling older people. Scandinavian Journal of Caring Sciences, 35(2), 366–374. https://doi.org/10.1111/scs.12852
- Sin, E., Shao, R., & Lee, T. M. C. (2021). The executive control correlate of loneliness in healthy older people. Aging & Mental Health, 25(7), 1224–1231. https://doi.org/10.1080/13607863.2020.1749832
- Shahnawaz, Z., Reppermund, S., Brodaty, H., Crawford, J. D., Draper, B., Trollor, J. N., & Sachdev, P. S. (2013). Prevalence and characteristics of depression in mild cognitive impairment: The Sydney Memory and Ageing Study. Acta Psychiatrica Scandinavica, 127(5), 394–402. https://doi.org/10.1111/acps.12008
- Solé-Padullés, C., Macià, D., Andersson, M., Stiernstedt, M., Pudas, S., Düzel, S., Zsoldos, E., Ebmeier, K. P., Binnewies, J., Drevon, C. A., Brandmaier, A. M., Mowinckel, A. M., Fjell, A. M., Madsen, K. S., Baaré, W. F. C., Lindenberger, U., Nyberg, L., Walhovd, K. B., & Bartrés-Faz, D. (2022). No association between loneliness, episodic memory, and hippocampal Vol. change in young and healthy older adults: A longitudinal European multicenter study. Frontiers in Aging Neuroscience, 14, 795764. Article 795764. https://doi.org/10.3389/fnagi.2022.795764
- Tilvis, R. S., Kähönen-Väre, M. H., Jolkkonen, J., Valvanne, J., Pitkala, K. H., & Strandberg, T. E. (2004). Predictors of cognitive decline and mortality of 164 aged people over a 10-year period. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 59(3), 268–274. https://doi.org/10.1093/gerona/59.3.M268
- Thompson, C., Halcomb, E., & Masso, M. (2023). The contribution of primary care practitioners to interventions reducing loneliness and social isolation in older people—An integrative review. Scandinavian Journal of Caring Sciences, 00, 1– 17. https://doi.org/10.1111/scs.13151
- Vallat-Azouvi, C., Pradat-Diehl, P., & Azouvi, P. (2012). The Working Memory Questionnaire: A scale to assess everyday life problems related to deficits of working memory in brain injured patients. Neuropsychological Rehabilitation, 22(4), 634–649. https://doi.org/10.1080/09602011.2012.681110
- Vannini, P., Hanseeuw, B., Munro, C. E., Amariglio, R. E., Marshall, G. A., Rentz, D. M., Pascual-Leone, A., Johnson, K. A., & Sperling, R. A. (2017). Anosognosia for memory deficits in mild cognitive impairment: Insight into the neural mechanism using functional and molecular imaging. NeuroImage: Clinical, 15, 408–414. https://doi.org/10.1016/j.nicl.2017.05.020
- Viviani, G., De Luca, F., Antonucci, G., Yankouskaya, A., & Pecchinenda, A. (2022). It is not always positive: Emotional bias in young and older adults. Psychological Research, 86(6), 2045–2057. https://doi.org/10.1007/s00426-021-01614-2
- Wilson, R. S., Krueger, K. R., Arnold, S. E., Schneider, J. A., Kelly, J. F., Barnes, L. L., Tang, Y., & Bennett, D. A. (2007). Loneliness and risk of Alzheimer disease. Archives of General Psychiatry, 64(2), 234–240. https://doi.org/10.1001/archpsyc.64.2.234
- World Health Organization. (2021). New advocacy brief highlights serious consequences of social isolation and loneliness on the health of older people, calls for greater political priority to the issue. https://www.who.int/news/item/29-07-2021-new-advocacy-brief-highlights-serious-consequences-of-social-isolation-and-loneliness-on-the-health-of-older-people-calls-for-greater-political-priority-to-the-issue