Abstract
Objectives
As the life expectancy of individuals with intellectual disabilities (ID) continues to increase, there is an increased risk of developing dementia. While psychosocial interventions are gaining prominence, evidence is limited for people with both dementia and ID. This review discusses the effectiveness of direct psychosocial interventions and adaptations to facilitate delivery within this population.
Methods
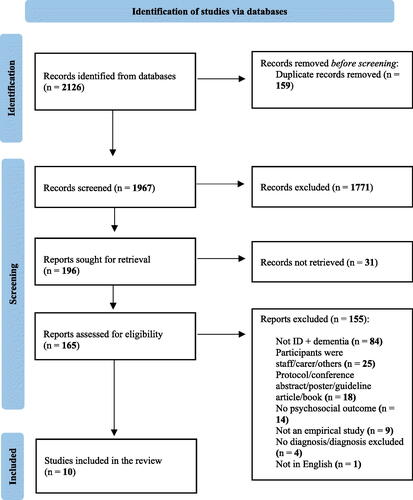
The review followed the PRISMA guidelines. Five electronic databases, grey literature, and reference lists of included articles were searched for relevant studies. 10 eligible studies were appraised and analysed by narrative synthesis.
Results
Ten distinct interventions were identified and categorised based on their purpose and delivery. All interventions were beneficial in improving a range of outcomes, though some studies were of low quality and most had small samples. Common adaptations included simplification of tasks and material, higher staff-to-client ratio, and alternative communication methods.
Conclusion
There is emerging evidence for several psychosocial interventions for people with ID and dementia, though further research is required on effectiveness and generalisability. The adaptations discussed may guide implementation into routine care and contribute to current policies and guidelines on improving ID and dementia care.
Introduction
Increasing life expectancy of people with intellectual disabilities (ID) is accompanied by an increased risk of several health conditions in the ageing ID population (Coppus, Citation2013). Individuals with ID tend to be at greater risk of developing dementia, and at an earlier age, compared to the general population (Strydom et al., Citation2009). According to the cognitive reserve hypothesis (Stern, Citation2002), higher reserves (greater cognitive capabilities and rich environment) should act as a protective factor in delaying dementia onset, whereas lower reserves would increase vulnerability to it. Considering this rationale, ID comprises significant functional and cognitive impairments which may therefore, increase the risk of developing dementia, and at an early onset (Silverman et al., Citation2013).
The management of ID and dementia includes substantial focus on long-term goals, and psychological and environmental interventions are recommended, especially for managing non-cognitive symptoms (NICE, 2018). Similarly, medication is suggested only in combination with psychosocial interventions to manage behaviour that challenges in people with ID (NICE, 2015).
Psychosocial interventions aim to improve symptomatology, emotional and psychological wellbeing, and overall quality of life (MacDonald & Summers, Citation2020). Research has examined a range of psychosocial interventions for dementia and there is increasing evidence for the effectiveness of cognitive stimulation therapy, cognitive rehabilitation therapy, occupational therapy and group reminiscence therapy, as suggested by the NICE guidelines for management of dementia (NICE, 2018). While psychosocial interventions are progressively being implemented, research has predominantly focused on individuals with dementia in the general population, maintaining uncertainty regarding the effectiveness and applicability of these interventions for people with ID.
The combined diagnosis and distinct presentations may render some interventions as effective for one but not the other. Furthermore, individual, service, and system level barriers to treatment (Willner, Citation2009) question how acceptable psychosocial interventions for dementia would be among the ID population. To abide by person-centred treatment, adaptations for people with ID need to be considered. Widely practised adaptations include simplifying tasks and language, using flexible methods, and considering developmental level (Whitehouse et al., Citation2006). Two systematic reviews have presented evidence on psychosocial interventions for people with ID and dementia; MacDonald and Summers (Citation2020) examined current interventions and their outcomes for people with ID and dementia; however, these included staff and carer focused (i.e. non-direct) interventions and discussed the lack of direct interventions tested and outcomes measured in this population. Moreover, the paper did not discuss intervention adaptations. Thalen et al. (Citation2022) reviewed the focus of psychosocial interventions for older people with ID and the role of staff support in applying these interventions. This review discussed factors that could optimise interventions for older people with ID but limited insight was given on dementia in ID or assessing intervention effectiveness for this population.
Therefore, this systematic review aims to extend current knowledge, with the following questions:
What is the evidence for the effectiveness of direct psychosocial interventions in ID and dementia?
What specific adaptations have been made to facilitate the use of these interventions with this population?
Methods
This review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist (Page et al., Citation2021).
Study protocol
The review protocol was published online on the PROSPERO website (CRD42022314605).
Inclusion criteria
Studies were included if: (1) participants had a diagnosis of ID and dementia, of any severity and duration, (2) they evaluated a direct psychosocial intervention delivered to people with ID and dementia (in clinical or non-clinical settings, including community and online modes, to account for COVID-19), (3) outcomes related to cognition, behaviour, psychiatric symptoms, adaptive functioning, and quality of life (all measured by validated scales), and (4) the study was published in English.
There was no limit on: (1) participants age, as people with ID may have an earlier onset of dementia, (2) country of study, (3) study design, and (4) publication date.
Exclusion criteria
Papers were excluded if: (1) participants (a) did not have a clinical diagnosis of ID and dementia or (b) had sub-clinical cognitive impairment; (2) the outcomes measures were collected only from carer/staff/others; (3) they were protocols, conference abstracts, and books.
Search strategy
Five electronic databases, Medline (OVID), Embase (OVID), PsychInfo (OVID), Web of Science (Core), and Google Scholar were used. Grey literature including unpublished studies and PhD theses (ProQuest Dissertations and Theses Global) were included. An initial search was conducted between March and April 2022 by the main researcher MM ().
Table 1. Search strategy for all databases.
Additionally, reference lists of included full-text articles and the two systematic reviews (MacDonald & Summers, Citation2020; Thalen et al., Citation2022) were checked for further relevant studies. The database searches were re-run in May 2022 before the final analyses.
Data extraction and synthesis
The database search results were deduplicated and papers were imported into Endnote. The first reviewer MM screened titles and abstracts based on the inclusion and exclusion criteria. Full texts were retrieved and checked for relevance alongside a second reviewer.
Data extraction examined key characteristics including information on the author, year, country, sample size, study design, demographics, and intervention details (type, modality, duration, number of planned sessions, length of session, treatment period, control condition, dropout rates, and retention), outcomes and findings. This was combined into a table, and narrative synthesis was carried out by summarising the studies, comparing their similarities and differences, and assessing quality.
Risk of bias assessment
Studies were assessed for quality using the Mixed Methods Appraisal Tool (MMAT), a critical appraisal tool suitable for systematic reviews that include quantitative, qualitative, and mixed-method studies (Hong et al., Citation2018b). It has five sets of methodological quality criteria for (1) qualitative (2) quantitative randomised controlled trials (3) quantitative non-randomised (4) quantitative descriptive, and (5) mixed-methods studies, with each criterion covering a specific attribute of the respective study design. Each category has five questions, with ‘Yes’, ‘No’, and ‘Can’t tell’ as responses. Two independent reviewers were involved in the quality assessment, and disagreements were resolved with discussion.
Results
Characteristics of included studies
A total of 2126 papers were identified from the database search and 1967 were screened after deduplication. Subsequently, 165 full texts were retrieved and assessed for eligibility. 10 papers met the eligibility criteria and were included in the review. The PRISMA flowchart () shows the process of study selection.
Four quantitative (one RCT, one non-randomised, and two descriptive), four qualitative (case studies) and two mixed-methods studies were included (). The studies were carried out between 2008 and 2019, across five different countries. Sample characteristics varied in terms of gender distribution and ethnicity, sample sizes ranged from 1 to 97 participants. The studies included ID and dementia of mild to profound/advanced severities, with four focusing on Down Syndrome and the remaining either had a sample with diverse aetiologies or did not specify the type of ID.
Table 2. Summary of included studies.
A range of outcomes were examined, including quality of life, behavioural changes, functioning, cognition, and symptom deterioration.
Quality assessment
depicts the quality assessment. A low-quality study met 0%–20%, medium quality met 40%–60%, and high-quality met 80%–100% of the criteria under the respective study design in the MMAT. Three studies were rated as high quality—Watchman et al. (Citation2021; quality score 100%), De Vreese et al. (Citation2012; 80%), and Ali et al. (Citation2022; 80%); three were of medium quality—Crook et al. (Citation2016; 60%), Hawkes et al. (Citation2019; 60%), and Lifshitz and Klein (Citation2011; 40%); one of low quality (Kiddle et al., Citation2016; 20%). Finally, three studies (Horovitz et al. Citation2010; Nichols, Citation2011; Vogl & Rapp, Citation2011) did not satisfy the screening criteria, so further appraisal was not conducted (i.e. total quality score N/A).
Table 3. Quality assessment of included studies.
What is the evidence for the effectiveness of direct psychosocial interventions in ID and dementia?
The studies varied in method, outcomes, and measures. provides further details on the 10 included studies, categorised as (1) behavioural, (2) structured (manualised), and (3) personalised interventions, based on their targets and delivery method.
Behavioural interventions
Two case studies used distinct behavioural interventions, each targeting specific behaviours that challenge. Horovitz et al. (Citation2010) implemented contingent reinforcement of compliance, which is based on the rationale that providing contingencies on compliance, rather than the undesired behaviour itself, could minimise the disadvantages of negative contingencies such as punishment. In this case study, contingent reinforcement was used to alleviate noncompliance with staff and inappropriate sexual behaviours, with a 61.1% decrease in average noncompliance post-interventions and lasting improvement at 1-month follow up.
Vogl and Rapp (Citation2011) used differential reinforcement of other behaviour (DRO) wherein reinforcement is provided for any response apart from the specific target behaviour, ultimately reducing the target behaviour due to lack of reinforcement (Zane et al., Citation2013). In this case, DRO was implemented for 22 days, to reduce loitering and stealing showing to decrease both behaviours post intervention.
Structured interventions
Five studies used manualised interventions, all of which varied in content and method.
Memory café
Memory cafes have commonly facilitated open conversations for people with dementia and their carers and helped them feel less isolated (Protoolis et al., Citation2022). Kiddle et al. (Citation2016) piloted a memory café facilitated by professionals with expertise in working with individuals with ID, challenging behaviours, and communication problems. Over 12 wk (each having a distinct theme), several physical, cognitive, and creative group activities were carried out, alongside individual activities where needed. There was a significant improvement in affect scores in weeks 7–12 compared to weeks 1–6, with a large effect size (T = 37, p < 0.05, r = −0.7). Positive feedback was gained from feedback questionnaires, alongside reports of improvements in communication, interaction, participation and alertness in people with ID and dementia during and after attending the café. However, no significant change was seen in clients’ physical wellbeing and broadening of interests.
Reminiscence
Reminiscence therapy (RT) involves discussing past activities, events, and experiences, generally facilitated by several memory prompts (Subramaniam & Woods, Citation2012). Emphasising on looking back at one’s life as a healthy occurrence rather than focusing on psychopathology (Butler, Citation1963), RT has shown some benefit in improving mood, wellbeing, and cognition. Crook et al. (Citation2016) conducted a randomised single case series experiment and compared the effectiveness of life story books and rummage boxes with no intervention, alongside examining any differences between the two interventions. Participants took part in each of the three conditions on thrice. Both reminiscence conditions significantly increased wellbeing scores and improved communicative, intellectual, and expressive behaviours. There was no significant difference between life story books and rummage boxes.
Cognitive stimulation therapy (CST)
CST is a group psychosocial intervention implemented as a structured program incorporating mental stimulation, reminiscence, and orientation activities (Morley & Cruz-Oliver, Citation2014). Individual cognitive stimulation therapy (iCST) aims to improve accessibility where group therapy may not be feasible or preferred (Orrell et al., Citation2017). While CST and iCST were originally developed for people with dementia, Ali et al. (Citation2022) adapted iCST for people with ID and dementia and conducted a feasibility RCT where carers were trained to carry out 40 sessions of manualised iCST over 20 weeks. Outcomes including cognition, quality of life, and caregiver wellbeing, were measured. Compared to usual care, quality of life was significantly higher in the iCST group at 21 weeks, with a large effect size (Cohen’s d = 0.89). However, no significant difference was found on other outcomes, and the fidelity assessment indicated that the sessions were not delivered to the intended standard.
Occupational therapy
Occupational therapy aims to promote wellbeing and overall functioning and is a suggested intervention for mild to moderate dementia (NICE, 2018). Hawkes et al. (Citation2019) examined the effectiveness of a person-centred Person, Interaction, Environment, or PIE programme (Young et al., Citation2011) that included a manual, observation tool, and self-reflection form. Experiences were measured as ‘enriching’, ‘depriving’, or ‘neutral’, in context to (1) staff knowledge of the person, (2) staff interaction with the person, and (3) the physical environment and culture of care. A range of activities and life story books were offered alongside the PIE programme, and four cycles of observations and reflections were carried out (repeated action research cycle) over two months, with a mixed-methods approach. Compared to baseline, there were more ‘enriching’ events for residents, with increased engagement, better communication and movement, and more resident interaction post-intervention.
Combined psychosocial interventions
One study (De Vreese et al., Citation2012) investigated the effectiveness of a multicomponent nonpharmacological approach in a special care unit (SCU) compared to treatment as usual in day centre (DC) and nursing home (NH) groups. The components included staff-oriented, environment-oriented, miscellaneous environmental considerations, and client-oriented interventions. Post-intervention, they found some improvement in cognition and stabilisation of everyday functioning and behaviour in SCU residents, and deterioration in the control groups. The improvement, however, was only significant when the participants had Down Syndrome.
Personalised interventions
These are multicomponent interventions tailored to individual needs, rather than a manualised intervention delivered uniformly. Three studies, one mixed-method and two case studies, examined the effectiveness of individualised interventions.
Watchman et al. (Citation2021) carried out a mixed-methods study on person-centred approaches to care, examining the impact of individualised goal-setting on behaviour and quality of life for people with ID and dementia. Participants set goals themselves, largely focused on improving mood, reducing anxiety, wanting to feel more like themselves, engagement in activities, and personal safety. They chose interventions relevant to their needs from a range of offered interventions; data collected over 10 months found that 74% of individual goals were met or exceeded expectations and qualitative interviews with staff echoed these positive effects. However, no significant change was found on individual measures of symptom severity and quality of life.
One case study (Nichols, Citation2011) discussed the efficacy of personalised technology in promoting independent and safe living in a local residential care home. Four distinct technological adaptations or interventions were implemented for individual cases; these included bedroom door sensors, talking photo album, fingerprint lock, and Being Alert (mark low and high-risk areas to prevent wandering off site into unsafe areas). Being Alert, specifically, was trialled for 12 weeks with two individuals, who often left the site without support staff. While there was no quantitative finding or statistical analysis conducted, all participants benefitted from personalised technology, primarily retaining their independence and leading a fulfilling life with minimal restrictions. Broader effects included economic benefits and family wellbeing, due to the reassurance of their relatives’ safety.
Mediational Intervention for Sensitizing Caregivers (MISC) was originally developed as an early intervention to improve child-caregiver relations, subsequently enhancing the child’s cognitive, behavioural, and emotional functioning (Klein, Citation2000). Another case study (Lifshitz & Klein, Citation2011), of an individual with Down Syndrome and early Alzheimer’s Disease dementia, investigated whether MISC mediation parameters were applicable for caregivers of people with ID and Alzheimer’s, and how it may affect the quality of interactions between the caregiver and individual. A tailored program with five parameters was implemented with the given case, and effects were measured through DMR scores (higher the score, greater the deterioration) and staff observations. Although memory difficulties remained, there were improvements in daily life and capacity and motivation to learn new skills, and deterioration was minimal. However, specific outcomes were not measured.
What specific adaptations have been made to facilitate the use of these interventions with this population?
Adapting techniques is crucial when delivering interventions for people with ID, to meet individual cognitive abilities, subjective presentations, and ensure that they can gain and retain treatment benefits. Five out of the 10 included studies discussed adaptations made at varying stages of the study.
Photovoice is a participatory research approach wherein photographs are used to depict the research questions; participants observe the study procedure, take photographs that are meaningful to them, and elaborate on the observations through interviews (Povee et al., Citation2014). Watchman et al. (Citation2021)’s study included five co-researchers with ID, who attended seven workshops over 10 months to learn about dementia, photovoice, using cameras, and data analysis. Participatory action research helped address one of their research questions on enabling co-researchers with ID to reflect on personal experiences and build a novel and inclusive dialogue on dementia; here, it included themes on peer support, future planning, and fear of dementia and its progression.
Furthermore, Kiddle et al. (Citation2016) piloted an adapted memory café for people with ID by simplifying cognitive tasks and broadening the time period for reminiscence, considering the possibility of early onset dementia. Other adaptations included higher ratio of staff to attendees to maximise one-to-one support, inclusion, and engagement of attendees in each activity. The staff was skilled in alternative communication methods such as Makaton, which aids communication by combining signs and symbols with speech (Tuffrey-Wijne & McEnhill, Citation2008). This knowledge promoted inclusion, alongside being beneficial in managing challenging behaviour. Lastly, the information provided at the café was specific to people with ID. Ali et al. (Citation2022)’s study on iCST simplified some activities or substituted them with alternative ones to better suit people with ID, while aiming to retain the original themes. This involved consultations from a speech and language therapist, alongside a focus group consisting of health and social care professionals, carers, and individuals with ID, who reviewed the activities and provided feedback. The adapted manual was piloted, and feedback sought (Ali et al., Citation2018).
To promote inclusivity during recruitment, Crook et al. (Citation2016) included a short demonstration of reminiscence during recruitment and provided red- and green-coloured cards to indicate agreement or disagreement. However, on trying this process and discussing with staff, they concluded that none of the participants had capacity; consultees were therefore invited. Hawkes et al. (Citation2019) supplemented their manualised intervention with activity resources and explained that staff were ‘encouraged’ to use flexible methods and adapt the activity to person-centred goals. While no further detail was provided, flexible methods are commonly used when implementing psychotherapy techniques with individuals with ID (Whitehouse et al., Citation2006).
Discussion
This review aimed to summarize the evidence for effectiveness of direct psychosocial interventions for ID and dementia, while discussing adaptations that facilitate their use. Based on the ten included studies of distinct interventions, there is emerging but limited evidence on the effectiveness of psychosocial interventions for this population. Given the small sample sizes in all studies, and absence of large-scale RCTs, caution is needed while interpreting effectiveness. Behavioural interventions may reduce occurrences of stealing, loitering, and inappropriate sexual behaviours. Studies of structured interventions suggested improvements in several outcomes, including affect, communication, engagement, cognition, daily functioning, and quality of life. Personalised interventions were beneficial for achieving personal goals, largely pertaining to improving mood, increasing engagement, and ensuring safety and independence. Furthermore, several interventions were adapted through reasonable adjustments and flexible delivery. Other adaptations promoted accessibility by collaborating with co-researchers with ID and promoting participant autonomy and individual decision-making during recruitment, where possible.
To our knowledge, this is the first review focused on direct interventions and outcomes for people with ID and dementia, and specific adaptations that facilitate these interventions, therefore alleviating limitations identified by previous reviews.
Prior research has largely focused on either ID or dementia. DRO has been effective in reducing challenging behaviour in adults with ID (Lloyd & Kennedy, Citation2014) while other functional-analysis-based behavioural therapy for dementia has effectively reduced wandering (Douglas et al., Citation2004). Reminiscence has shown positive effects on mood and cognitive abilities in people with dementia (Cotelli et al., Citation2012), with suggestions of including it in routine care (Huang et al., Citation2015). Similar acceptability was found among people with ID, though less common in practice (Stueber & Hassiotis, Citation2012). There is substantial evidence of the effectiveness of CST and iCST in improving cognition and quality of life in dementia in individuals without ID (Gibbor et al., Citation2021), with recommendations of group CST for mild to moderate dementia (NICE, 2018). Similar improvements in cognition were observed among participants with Down Syndrome (Shanahan, Citation2014), though these were not significant compared to control groups, and research on CST for people with ID is limited. Furthermore, multicomponent interventions may target multiple modifiable risk factors and slow cognitive decline in dementia (Chalfont et al., Citation2020), while tailored interventions have been effective in improving quality of life for people with dementia living at home (Cooper et al., Citation2012).
Strengths and limitations
Including grey literature reduced publication bias and improved the comprehensiveness of the review (Paez, Citation2017). On screening, none of these papers met the inclusion criteria for the final review however, as they either did not include participants with both ID and dementia or did not assess a psychosocial intervention or outcomes. Screening and quality assessment of papers was undertaken by two independent researchers, which ensured that relevant papers were not missed. Another strength is the systematic mixed studies review design, which includes quantitative, qualitative, and mixed-methods studies. While quantitative research is useful to determine the effectiveness of interventions, and the magnitude and direction of the relationship between the intervention and outcome, qualitative findings may explain how, why, and in what context an intervention is effective (Cerigo & Quesnel-Vallée, Citation2020). Considering the limited evidence on interventions for the ID and dementia population, broadening the study designs provides a more holistic view of current interventions.
However, there are several limitations to consider. Only including English language papers may increase bias. Furthermore, there was no co-production or consultation with service users. While six out of ten papers were of high or medium quality, three papers did not satisfy the screening criteria, thus questioning credibility surrounding the interventions’ effectiveness. Large RCTs, studies with medium to long-term follow-ups, and studies examining outcomes related to cost-effectiveness were all absent. Moreover, inadequate data collection methods form a source of methodological bias. For example, staff observations may not be a sensitive measure of change. However, most quantitative studies used adapted measures relevant to the population or cultural context. Behavioural interventions were investigated through low-quality case studies, which tend to have low generalisability and are difficult to make causal inferences from (Simon & Goes, Citation2013). The interventions were categorised as behavioural, structured, and personalised, though individual differences create uncertainty on their external validity. While some adaptations provided a rationale and were overseen by consultation, others were not justified by an evidence-base, thus highlighting the need for further research in this area.
Implications
This review provides some evidence for the benefits of psychosocial interventions in this population, which could be implemented in clinical practice. While behavioural interventions may improve behavioural problems, structured interventions, including multicomponent interventions, target several areas and may therefore, provide multiple benefits. Individualised interventions seem to have notable potential in meeting complex needs, including sensory impairments, which require adaptations and tailoring interventions to individual needs. However, the issue of access persists as most community ID teams do not provide these interventions. Lack of resources and staff who are trained to provide dementia-specific interventions are common barriers to person-centred care in health and social care settings (Martin et al., Citation2020).
The benefits of psychosocial interventions discussed in this review may furthermore, contribute towards alleviating increased antipsychotic prescription in people with ID and dementia (Sheehan et al., Citation2015), and support measures of reducing overmedication within ID and dementia populations, respectively.
Future research needs to focus on samples of people with both ID and dementia. RCTs or other experimental designs may help establish a cause-and-effect relationship, while follow-ups would indicate whether the intervention’s benefits are maintained (Llewellyn-Bennett et al., Citation2016). Co-production in adapting interventions may further provide insight from lived experiences (Acton et al., Citation2022), through increased involvement and engagement in feedback and consultation, as opposed to researcher-led methods. Larger sample sizes and comparative research would increase validity and reduce bias. Previous studies have acknowledged small sample sizes, recruitment difficulties, need for multi-site involvement, and longer recruitment periods (Ali et al., Citation2022; De Vreese et al., Citation2012; Watchman et al., Citation2021). Implementing these measures is however, accompanied by logistical issues; feasible methods that explore the acceptability of the intervention, while maintaining cost-effectiveness, therefore need to be discussed.
Conclusion
This review has analysed direct psychosocial interventions for people with ID and dementia, alongside adaptations to facilitate their implementation. While some interventions have emerging evidence supporting their potential to address complex individual needs, large RCTs and follow-ups are required to counter methodological limitations. Suggestions have been made for future research, with implications for accessibility in clinical practice and national initiatives on ID and dementia care, aimed at strengthening person-centred care.
Disclosure statement
There are no relevant financial or non-financial competing interests to report.
Additional information
Funding
References
- Acton, D., Duncan, C., & Jaydeokar, S. (2022). Co-production of post-diagnostic psychosocial intervention with carers of people with intellectual disability and dementia. Advances in Mental Health and Intellectual Disabilities, 16(3), 169–178. https://doi.org/10.1108/AMHID-01-2022-0006
- Ali, A., Brown, E., Spector, A., Aguirre, E., & Hassiotis, A. (2018). Individual cognitive stimulation therapy for people with intellectual disability and dementia: Protocol of a feasibility randomised controlled trial. BMJ Open, 8(12), e022136. https://doi.org/10.1136/bmjopen-2018-022136
- Ali, A., Brown, E., Tsang, W., Spector, A., Aguirre, E., Hoare, S., & Hassiotis, A. (2022). Individual cognitive stimulation therapy (iCST) for people with intellectual disability and dementia: A feasibility randomised controlled trial. Aging & Mental Health, 26(4), 698–708. https://doi.org/10.1080/13607863.2020.1869180
- Butler, R. N. (1963). The life review: An interpretation of reminiscence in the aged. Psychiatry, 26(1), 65–76. https://doi.org/10.1080/00332747.1963.11023339
- Cerigo, H., & Quesnel-Vallée, A. (2020). Systematic mixed studies reviews: Leveraging the literature to answer complex questions through the integration of quantitative and qualitative evidence. International Journal of Public Health, 65(5), 699–703. https://doi.org/10.1007/s00038-020-01386-3
- Chalfont, G., Milligan, C., & Simpson, J. (2020). A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with dementia. Dementia (London, England), 19(4), 1086–1130. https://doi.org/10.1177/1471301218795289
- Cooper, C., Mukadam, N., Katona, C., Lyketsos, C. G., Ames, D., Rabins, P., Engedal, K., de Mendonça Lima, C., Blazer, D., Teri, L., Brodaty, H., & Livingston, G, World Federation of Biological Psychiatry – Old Age Taskforce. (2012). Systematic review of the effectiveness of non-pharmacological interventions to improve quality of life of people with dementia. International Psychogeriatrics, 24(6), 856–870. https://doi.org/10.1017/S1041610211002614
- Coppus, A. M. (2013). People with intellectual disability: What do we know about adulthood and life expectancy? Developmental Disabilities Research Reviews, 18(1), 6–16. https://doi.org/10.1002/ddrr.1123
- Cotelli, M., Manenti, R., & Zanetti, O. (2012). Reminiscence therapy in dementia: A review. Maturitas, 72(3), 203–205. https://doi.org/10.1016/j.maturitas.2012.04.008
- Crook, N., Adams, M., Shorten, N., & Langdon, P. E. (2016). Does the well-being of individuals with down syndrome and dementia improve when using life story books and rummage boxes? A randomized single case series experiment [Randomized Controlled Trial Research Support, Non-U.S. Gov’t]. Journal of Applied Research in Intellectual Disabilities: JARID, 29(1), 1–10. https://doi.org/10.1111/jar.12151
- De Vreese, L. P., Mantesso, U., De Bastiani, E., Weger, E., Marangoni, A. C., & Gomiero, T. (2012). Impact of dementia‐derived nonpharmacological intervention procedures on cognition and behavior in older adults with intellectual disabilities: A 3‐year follow‐up study. Journal of Policy and Practice in Intellectual Disabilities, 9(2), 92–102. https://doi.org/10.1111/j.1741-1130.2012.00344.x
- Douglas, S., James, I., & Ballard, C. (2004). Non-pharmacological interventions in dementia. Advances in Psychiatric Treatment, 10(3), 171–177. https://doi.org/10.1192/apt.10.3.171
- Gibbor, L., Yates, L., Volkmer, A., & Spector, A. (2021). Cognitive stimulation therapy (CST) for dementia: A systematic review of qualitative research. Aging & Mental Health, 25(6), 980–990. https://doi.org/10.1080/13607863.2020.1746741
- Hawkes, T., Luff, T., & Gee, S. B. (2019). Supporting person-centred dementia care for people with intellectual disabilities using the person, interaction, environment programme. New Zealand Journal of Occupational Therapy, 66(1), 12–18.
- Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., Gagnon, M.-P., Griffiths, F., & Nicolau, B. (2018b). Mixed methods appraisal tool (MMAT), version 2018. Registration of Copyright, (10), 1148552.
- Horovitz, M., Kozlowski, A. M., & Matson, J. L. (2010). Compliance training in an adult with dementia of the Alzheimer’s type and Down syndrome. Clinical Case Studies, 9(2), 95–105. https://doi.org/10.1177/1534650109357784
- Huang, H.-C., Chen, Y.-T., Chen, P.-Y., Hu, S. H.-L., Liu, F., Kuo, Y.-L., & Chiu, H.-Y. (2015). Reminiscence therapy improves cognitive functions and reduces depressive symptoms in elderly people with dementia: A meta-analysis of randomized controlled trials. Journal of the American Medical Directors Association, 16(12), 1087–1094. https://doi.org/10.1016/j.jamda.2015.07.010
- Jarrott, S. E., Kwack, H. R., & Relf, D. ( 2002). An observational assessment of a dementia-specific horticultural therapy program. HortTechnology, 12(3), 403-410. https://doi.org/10.21273/HORTTECH.12.3.403
- Kiddle, H., Drew, N., Crabbe, P., & Wigmore, J. (2016). A pilot memory cafe for people with learning disabilities and memory difficulties [Empirical Study; Quantitative Study]. British Journal of Learning Disabilities, 44(3), 175–181. https://doi.org/10.1111/bld.12135
- Klein, P. S. (2000). A developmental mediation approach to early intervention; mediational intervention for sensitising caregivers (MISC). Educational and Child Psychology, 17(3), 19–31. https://doi.org/10.53841/bpsecp.2000.17.3.19
- Lifshitz, H., & Klein, P. S. (2011). Mediation between staff and elderly persons with intellectual disability with Alzheimer disease as a means of enhancing their daily functioning. Education and Training in Autism and Developmental Disabilities, 106–115.
- Llewellyn-Bennett, R., Bowman, L., & Bulbulia, R. (2016). Post-trial follow-up methodology in large randomized controlled trials: A systematic review protocol. Systematic Reviews, 5(1), 214. https://doi.org/10.1186/s13643-016-0393-3
- Lloyd, B. P., & Kennedy, C. H. (2014). Assessment and treatment of challenging behaviour for individuals with intellectual disability: A research review. Journal of Applied Research in Intellectual Disabilities : JARID, 27(3), 187–199. https://doi.org/10.1111/jar.12089
- MacDonald, S., & Summers, S. J. (2020). Psychosocial interventions for people with intellectual disabilities and dementia: A systematic review. Journal of Applied Research in Intellectual Disabilities: JARID, 33(5), 839–855. https://doi.org/10.1111/jar.12722
- Martin, A., O’Connor, S., & Jackson, C. (2020). A scoping review of gaps and priorities in dementia care in Europe. Dementia (London, England), 19(7), 2135–2151. https://doi.org/10.1177/1471301218816250
- Morley, J. E., & Cruz-Oliver, D. M. (2014). Cognitive stimulation therapy. Journal of the American Medical Directors Association, 15(10), 689–691. https://doi.org/10.1016/j.jamda.2014.07.015
- National Institute for Health and Care Excellence. (2015). Challenging behaviour and learning disabilities: Prevention and interventions for people with learning disabilities whose behaviour challenges [NICE Guideline No. 11]. https://www.nice.org.uk/guidance/ng11/chapter/Recommendations
- National Institute for Health and Care Excellence. (2018). Dementia: Assessment, management and support for people living with dementia and their carers [NICE Guideline No. 97]. https://www.nice.org.uk/guidance/ng97/chapter/Recommendations
- Nichols, E. (2011). How personalised technology can play an important role in supporting people with learning disabilities as they age and face the onset of dementia. Journal of Assistive Technologies, 5(3), 158–163. https://doi.org/10.1108/17549451111173532
- Orrell, M., Yates, L., Leung, P., Kang, S., Hoare, Z., Whitaker, C., Burns, A., Knapp, M., Leroi, I., Moniz-Cook, E., Pearson, S., Simpson, S., Spector, A., Roberts, S., Russell, I., de Waal, H., Woods, R. T., & Orgeta, V. (2017). The impact of individual Cognitive Stimulation Therapy (iCST) on cognition, quality of life, caregiver health, and family relationships in dementia: A randomised controlled trial. PLoS Medicine, 14(3), e1002269. https://doi.org/10.1371/journal.pmed.1002269
- Paez, A. (2017). Gray literature: An important resource in systematic reviews. Journal of Evidence-Based Medicine, 10(3), 233–240. https://doi.org/10.1111/jebm.12266
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery (London, England), 88, 105906. https://doi.org/10.1016/j.ijsu.2021.105906
- Povee, K., Bishop, B. J., & Roberts, L. D. (2014). The use of photovoice with people with intellectual disabilities: Reflections, challenges and opportunities. Disability & Society, 29(6), 893–907. https://doi.org/10.1080/09687599.2013.874331
- Protoolis, H. A., Burton, J., Riley, L., & Jancey, J. (2022). More than memory: A qualitative analysis of carer‐reported psychosocial benefits of Memory Cafés. Health Promotion Journal of Australia : official Journal of Australian Association of Health Promotion Professionals, 33 Suppl 1(Suppl 1), 358–366. https://doi.org/10.1002/hpja.573
- Shanahan, S. F. (2014). Efficacy of a cognitive stimulation therapy programme with adults with Down syndrome: A randomised study. University of Essex.
- Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A., & Horsfall, L. (2015). Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ (Clinical Research ed.), 351, h4326. https://doi.org/10.1136/bmj.h4326
- Silverman, W. P., Zigman, W. B., Krinsky‐McHale, S. J., Ryan, R., & Schupf, N. (2013). Intellectual disability, mild cognitive impairment, and risk for dementia. Journal of Policy and Practice in Intellectual Disabilities, 10(3), 245–251. https://doi.org/10.1111/jppi.12042
- Simon, M. K., & Goes, J. (2013). Scope, limitations, and delimitations.
- Stern, Y. (2002). What is cognitive reserve? Theory and research application of the reserve concept. Journal of the International Neuropsychological Society, 8(3), 448–460. https://doi.org/10.1017/S1355617702813248
- Strydom, A., Hassiotis, A., King, M., & Livingston, G. (2009). The relationship of dementia prevalence in older adults with intellectual disability (ID) to age and severity of ID. Psychological Medicine, 39(1), 13–21. https://doi.org/10.1017/S0033291708003334
- Stueber, K., & Hassiotis, A. (2012). Reminiscence therapy for older service users. Learning Disability Practice, 15(2), 12–16. https://doi.org/10.7748/ldp2012.03.15.2.12.c8965
- Subramaniam, P., & Woods, B. (2012). The impact of individual reminiscence therapy for people with dementia: Systematic review. Expert Review of Neurotherapeutics, 12(5), 545–555. https://doi.org/10.1586/ern.12.35
- Thalen, M., Volkers, K. M., van Oorsouw, W. M., & Embregts, P. J. (2022). Psychosocial interventions for older people with intellectual disabilities and the role of support staff: A systematic review. Journal of Applied Research in Intellectual Disabilities: JARID, 35(2), 312–337. https://doi.org/10.1111/jar.12953
- Tuffrey-Wijne, I., & McEnhill, L. (2008). Communication difficulties and intellectual disability in end-of-life care. International Journal of Palliative Nursing, 14(4), 189–194. https://doi.org/10.12968/ijpn.2008.14.4.29133
- Vogl, M., & Rapp, J. T. (2011). Differential reinforcement of other behavior and extinction to reduce loitering and stealing for an adult with an intellectual disability and dementia. Clinical Case Studies, 10(3), 229–235. https://doi.org/10.1177/1534650111405188
- Watchman, K., Mattheys, K., McKernon, M., Strachan, H., Andreis, F., & Murdoch, J. (2021). A person‐centred approach to implementation of psychosocial interventions with people who have an intellectual disability and dementia—A participatory action study. Journal of Applied Research in Intellectual Disabilities : JARID, 34(1), 164–177. https://doi.org/10.1111/jar.12795
- Whitehouse, R. M., Tudway, J. A., Look, R., & Kroese, B. S. (2006). Adapting individual psychotherapy for adults with intellectual disabilities: A comparative review of the cognitive–behavioural and psychodynamic literature. Journal of Applied Research in Intellectual Disabilities, 19(1), 55–65. https://doi.org/10.1111/j.1468-3148.2005.00281.x
- Willner, P. (2009). Psychotherapeutic interventions in learning disability: Focus on cognitive behavioural therapy and mental health. Psychiatry, 8(10), 416–419. https://doi.org/10.1016/j.mppsy.2009.06.018
- Young, J., C., H., Woolley, R., Gandesha, A., Souza, R. (2011). Report of the National Audit of Dementia Care in General Hospitals. Royal College of Psychiatrists & Healthcare Quality Improvement Partnership. https://www.rcpsych.ac.uk/docs/default-source/improving-care/ccqi/national-clinical-audits/national-audit-of-dementia/r1/nad-round-1-national-report-full-report.pdf?sfvrsn=11ce826d_6
- Zane, T., Davis, C., & Volkmar, F. R. (2013). Differential reinforcement procedures of other behavior (DRO). In Encyclopedia of autism spectrum disorders (pp. 962–966). Springer New York. https://doi.org/10.1007/978-1-4419-1698-3_1903