Abstract
Objectives: The primary objective of the study was to investigate whether the choice of long-acting reversible contraception (LARC) was associated with the risk of abortion over a period of 24 months postpartum. The secondary objective was to analyse whether other significant factors were affecting the risk of abortion during this period.
Methods: In this retrospective cohort study, we analysed 11,066 women who had delivered in three Swedish cities during 2013 and 2014. Demographic and medical variables were obtained from medical records. Attendance at the postpartum visit, choice of postpartum contraception and history of abortion was noted. Logistic regression analysis was performed to assess factors associated with the risk of abortion. The main outcome measure was the proportion of women with abortion up to 24 months postpartum.
Results: Data from 11,066 women were included in the final analysis. Within 12–24 months after delivery 2.5% of women had an abortion. The choice of LARC after childbirth reduced the risk of subsequent abortion (odds ratio 0.74; 95% confidence interval [CI] 0.60, 0.91; p = .005). Smoking, age <25 years and have had a previous abortion significantly increased the risk of abortion during follow-up, whereas exclusive breastfeeding decreased the risk.
Conclusions: Increasing the proportion of women who choose LARC postpartum could decrease the risk of abortion for up to 2 years after childbirth.
目的:本研究主要目的是调查在产后24个月内选择长效可逆避孕(LARC)是否与流产风险相关。次要目标是分析此期间是否有其他重要因素影响流产风险。
方法:在此项回顾性队列研究中, 我们分析了2013年至2014年在瑞典三个城市分娩的11066名女性。人口统计学和医学变量从医疗记录中获得。记录了产后访视、产后避孕的选择和流产史。进行逻辑回归分析以评估与流产风险相关的因素。主要结局指标是产后24个月内的女性流产比例。
结果:最终分析11,066名女性的数据。分娩后的12-24个月内, 有2.5%的女性流产。分娩后选择LARC可以降低随后流产的风险(比值比0.74;95%置信区间[CI] 0.60, 0.91;p = 0.005)。吸烟、年龄小于25岁且有流产史显著增加了随访期间流产的风险, 而纯母乳喂养则降低了风险。
结论:增加产后选择LARC的女性比例可以降低分娩后长达2年的流产风险。
Introduction
It has been increasingly acknowledged that the need for effective contraception after childbirth is underestimated [Citation1]. The magnitude of the risk of unintended pregnancy and possible subsequent abortion is not known. Young women seem to be the most vulnerable group for unintended pregnancy after childbirth [Citation2,Citation3]. Short interpregnancy intervals and unintended childbirth have been associated with a negative impact on maternal health [Citation4,Citation5] and a negative obstetric outcome [Citation6]. Moreover, most women do not plan a new pregnancy within the year after delivery [Citation7].
Fertility may return from as early as 4 weeks after delivery [Citation8] and close to half of all women have resumed sexual activity at 6 weeks postpartum [Citation9]. Intrauterine contraceptive devices (IUCDs), including copper-bearing intrauterine devices and hormonal intrauterine systems, as well as contraceptive implants, are termed long-acting reversible contraception (LARC) methods. LARC methods have been shown to significantly lower the risk of subsequent abortion in women who have already had an abortion [Citation10–12].
In Sweden, women have the right to request an abortion up to 18 weeks of gestation, which is provided through the public health care system. Women pay approximately €20–45 for an abortion.
In Sweden, contraception is currently not provided as part of routine care in hospital after delivery. The antenatal health care programme recommends a follow-up visit to the hospital at 6–12 weeks postpartum [Citation13], when contraception can be provided by the midwife. If the midwife and the woman have already agreed on the use of a LARC method postpartum, it can often be placed at that same appointment. If LARC is not chosen until this visits an additional visit is often needed for insertion. A note of the intended choice of postpartum contraception is made on the medical record form used for the postpartum visit. All methods of contraception are thus available and are provided by midwives. Local guidelines recommend starting any contraceptive method, including intrauterine contraception, at 6–12 weeks postpartum.
In 2017, 22% of women in Sweden did not attend the postnatal visit after delivery, thus missing the opportunity for contraceptive counselling and prescription [Citation14]. Consequently, a substantial number of women remained at risk of unintended pregnancy in the postpartum period, which might have led to abortion. Post-abortion studies show that initiation of LARC should not be delayed for a follow-up visit, as up to 50% of women do not attend a scheduled follow-up visit [Citation10,Citation15,Citation16]. Similarly, up to 30% of women do not attend a scheduled visit for placement of an IUCD up to 6 weeks postpartum [Citation17]. Furthermore, there is good evidence that LARC should be the first-line recommendation for women in the postpartum period, to avoid early repeat pregnancy and abortion [Citation18]. The impact of attendance at the postnatal visit and the choice of contraceptive method on the risk of abortion after childbirth remain unexplored.
This study aimed to investigate the proportion of women who have an abortion within 24 months after delivery and to determine whether the choice of a LARC method postpartum significantly lowered the risk of abortion in this period. The secondary objective was to analyse whether other significant factors were affecting the risk of abortion in the same period.
Methods
All women who delivered at Linköping, Norrköping, and Västervik hospitals in Sweden between 1 January 2013 and 31 December 2014 were included in this retrospective cohort study. The catchment areas of these hospitals cover both urban and rural populations. Women were excluded from the study if they had moved out of the catchment area, had a missing personal identification number or were re-registering for antenatal care because of another pregnancy during the follow-up period (n = 1081). Demographic data, attendance at the postpartum visit, choice of postpartum contraception and self-reported breastfeeding status were noted at the postpartum visit on the woman’s obstetric electronic medical record (Obstetrix; Cerner, Lund, Sweden). Data regarding actual insertion of LARC could not be extracted. Abortion was verified by scrutinising patient records (Cosmic; Cambio, Stockholm, Sweden); possible abortion was indicated by an appointment for abortion counselling and ICD-10 diagnosis code Z64.0. Registration of diagnosis codes is mandatory in Sweden and is reported to the Swedish National Board of Health and Welfare. According to Swedish guidelines, code Z64.0 should be used for all women requesting counselling for or provision of abortion. Depending on the time of delivery during the index year (2013 or 2014), the follow-up period varied between 12 and 24 months.
The sample size was calculated based on the results of a pilot study of 350 postpartum women, which revealed that 6% had an appointment for abortion within the following 1–2 years. We expected that close to 30% of women would choose a LARC method, and we expected 50% fewer abortions in this group compared with the group of women choosing other contraceptive methods or no method at all. Based on assumptions from the pilot study, to achieve 80% power and a 5% significance level the study needed to include 10,000 delivered women.
Data reporting follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (www.strobe-statement.org).
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 24.0 (IBM, Armonk, NY). The analyses used the full dataset, and all results were based on observed outcomes without imputation of missing data. Non-parametric continuous variables are presented as medians with minimum and maximum values; differences between groups were analysed by the Mann–Whitney U test. Dichotomous variables are presented as proportions and percentages; differences between groups were analysed by the χ2 test or Fisher’s exact test, as appropriate. Odds ratios (ORs) for abortion are presented. For analysis of significant factors affecting risk of abortion, continuous variables were dichotomised and used in a backward elimination method for logistic regression as follows: age <25 and ≥25 years, body mass index (BMI) <30 and ≥30 kg/m2, postpartum visit <13 and ≥13 weeks after childbirth. Results are presented as adjusted ORs with 95% confidence interval (CI). All differences between groups were considered as statistically significant if they had a p-value ≤.05.
Ethics approval
The study was approved by the regional ethics review board in Linköping, Sweden (no. 2016/84-31, 16 March 2016).
Results
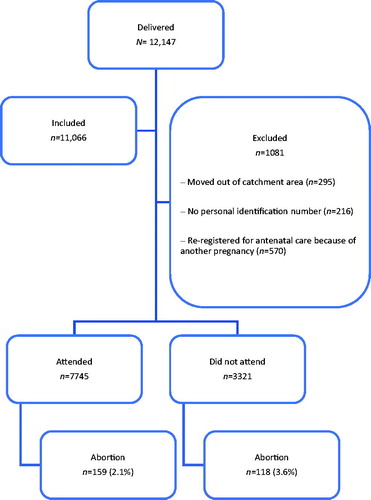
There were 225,485 deliveries in Sweden during 2013 and 2014 [Citation19]. Of the 12,147 women who delivered at the study centres between 1 January 2013 and 31 December 2014, 1081 were excluded, leaving 11,066 women in the final analysis (). Of these women, 847 (7.7%) became pregnant within 12–24 months. A total of 277/11,066 (2.5%) had an abortion and 570/11,066 (5.2%) chose to continue their pregnancy. The abortion rate was 16.7/1000 per year. The mean observation time was 18 months.
Figure 1. Flow chart presenting the study group, attendance at the postpartum visit and number of induced abortions during follow-up.
The demographic characteristics of women with and without abortion during the follow-up period are shown in . A total of 2080/11,066 (18.8%) women had had a previous abortion. Women with abortion during follow-up had a higher number of previously reported abortions and miscarriages and had higher parity. These women were also significantly younger. There was no significant difference in BMI ().
Table 1. Demographic characteristics of included women.
A total of 7745 (70%) women attended the postpartum visit at a mean of 9.4 weeks after delivery. Of all attendees, 76% had a decision registered in their patient record regarding future wish for a specific contraceptive method. The remainder either had no documentation regarding contraception or had documentation that they did not wish to use any contraceptive method. The choice of method at the postpartum visit and number of abortions during the 24 months of follow-up are shown in .
Table 2. Proportion of women who had at least one abortion during follow-up in relation to the choice of contraceptive method.
A higher proportion of women who did not attend the postpartum visit had an abortion during follow-up (118/3321, 3.6%), compared with women who did attend (159/7745, 2.1%). Women aged 20–24 years were at highest risk of abortion during follow-up (76/1492, 5.1%), followed by women aged 15–19 years (5/117, 4.3%). LARC methods were chosen by 1945/11,066 (17.6%) women. Younger women tended to choose the implant more often compared with women ≥25 years of age (93/1609 [5.8%] vs. 255/9457 [2.7%]; p< .001) and intrauterine contraception less often (206/1609 [12.8%] vs. 1391/9457 [14.7%]; p = .049).
Multiple logistic regression analysis was performed to determine which factors significantly influenced the risk of abortion (). The decision to use a LARC method postpartum significantly decreased the risk (OR 0.74; 95% CI 0.60, 0.91; p = .005). Exclusive breastfeeding at the time of the postpartum visit also decreased the risk (p < .001). Certain demographic characteristics (smoking, age <25 and previous abortion) significantly increased the risk of abortion during follow-up, whereas a high BMI (≥30 kg/m2) or attending the postpartum visit had no significant influence on the risk of abortion.
Table 3. Factors influencing risk of abortion during follow-up.
Discussion
Findings and interpretation
We found that 2.5% of women had an abortion within 12–24 months after delivery. The choice of LARC after childbirth reduced the risk of subsequent abortion. Smoking, age <25 years and have had a previous abortion significantly increased the risk of abortion during follow-up, whereas exclusive breastfeeding at the time of the postpartum visit decreased the risk.
A possible reason for the low abortion rate in our study might be the high proportion of women who decided during follow-up to continue their pregnancy (67.3%). Another possible reason might be the high level of breastfeeding in Sweden. Between 2013 and 2014 as many as 63% of newborns were exclusively or partially breastfed at 6 months postpartum [Citation20]. Women who were exclusively breastfeeding at the postpartum visit had a significantly lower rate of abortion during follow-up in our study. Exclusive breastfeeding in the first months postpartum may lead to anovulation and delayed return of fertility; it may also reflect higher socioeconomic status, which would be consistent with the 2018 findings of Sarki et al. [Citation21].
Subgroup analyses in our study could have added information about any differences in the proportion of pregnancy continuations in the group of women who attended the postpartum visit compared with those who did not. As abortion was a variable used as a marker for unintended pregnancy, and thus the main focus of interest, we did not go further into subgroup analysis regarding pregnancy continuation. The high proportion of women deciding to continue their pregnancy cannot be explained by abortion stigma, as Sweden is a country with low abortion stigma, where unwanted pregnancies generally do not lead to birth.
Thirty percent of all women did not attend the follow-up visit. This proportion is slightly higher than the data reported in the Swedish pregnancy register [Citation14]. The reason for this high figure remains obscure. The proportion of non-attendees has remained stable in Sweden over recent years. Our figures are, however, in accordance with data from the USA [Citation22], where socioeconomic factors have been shown to be the most important reasons for non-attendance. We do not have information on the socioeconomic status of the women in our study, but it seems reasonable that also in Sweden socioeconomic factors may play a part in non-attendance at postpartum follow-up. These women miss an important opportunity to discuss and initiate contraceptive methods.
Differences and similarities in relation to other studies
In our study, 7.7% of all women became pregnant during follow-up, which is in accordance with UK data [Citation7], where approximately 7% of women presenting for abortion or to give birth conceived again within 12 months. However, we found a surprisingly low abortion rate of 16.7/1000 per year in the time frame of the study, which is lower than the national Swedish abortion rate of 20.2/1000 in the corresponding year [Citation23]. It is also lower than the number of repeat abortions after an index abortion. In a 2016 Swedish study, Kilander et al. [Citation11] found that 239/987 (24%) returned for another abortion after an index abortion, and the median time until the first repeat abortion was 17 months.
An American study conducted in 2019 estimated the prevalence of postpartum LARC use among 147,747 women and found that women attending the postpartum visit had significantly greater use of contraception, specifically LARC methods [Citation24].
The timing of the postpartum visit seems to be of importance. In a recent study conducted in California, approximately 90% of women completed a scheduled visit at 2–3 weeks postpartum compared with approximately 80% completing a scheduled visit at 6 weeks postpartum [Citation25]. Immediate initiation of contraception has been shown to be superior to additional visits for contraceptive uptake in studies of both the post-abortion [Citation26] and postpartum period [Citation27].
Studies from the UK indicate that antenatal counselling for postpartum contraception is both feasible and acceptable [Citation28,Citation29]. In these two studies, women were positive towards antenatal counselling and 43% and 68%, respectively, were planning to use LARC after delivery. In spite of this antenatal plan only 9% and 32%, respectively, received LARC prior to discharge from hospital. Thus, providing contraception and LARC to women before discharge from hospital appears to be a challenge. There may be several reasons for not providing LARC in the maternity department, but heavy workload was reported as the greatest obstacle.
Our findings highlight that although the postpartum visit is a prerequisite for provision of postpartum contraception it is, in fact, the choice of contraception that has the greatest importance. Efforts to increase attendance at the postpartum visit would most likely reduce the proportion of women with abortion within 12–24 months after childbirth because some of those women would choose LARC methods. Our finding of the importance of choice of contraceptive method is in accordance with earlier findings [Citation1,Citation30]. In our study, 18 (1.1%) women who opted for intrauterine contraception after childbirth had an abortion during follow-up. If these women had had an IUCD inserted either immediately postpartum or at the follow-up visit, conception would most likely have been avoided.
Strengths and weaknesses
We have no data on subfertility or assisted reproduction among the women in our cohort. As women above 24 years of age are more likely to have a diagnosis of subfertility or infertility in addition to lower fertility because of their higher age, they may, therefore, have an inherently lower risk of abortion. These factors may partly explain the lower risk of abortion in the older age group.
The major strength of our study is the large cohort with data gathered on more than 11,000 women in the final analysis. The data emanating from a large Swedish region with an academic centre as well as urban and rural areas. All patient records with diagnoses related to abortion were scrutinised. Thus, we can be certain that women with abortion had an unwanted pregnancy and followed through with an abortion. As there are not many clinics providing abortions that are close to the region and stigma surrounding abortion is low in Sweden, we can be reasonably sure that all women in the catchment area who had an abortion were included in the data.
As we had to exclude women who did not have a personal identification number, most of whom are refugees without residence permits, all parts of Swedish society were likely not fully represented in the study. In addition, the nature of a retrospective cohort study implies limitations due to missing data in patient records, but in fact, few data were missing. Furthermore, it should be noted that we only had information regarding the choice of contraceptive method at the follow-up visit and the figures may not necessarily represent actual initiation and use of that method; however, it is clearly shown that the choice of contraceptive method had a significant impact regardless of data on future use. Thus, the impact of actual initiation of a contraceptive method cannot be assessed and the actual use might be underestimated in this study.
The database lacks data on previous infertility or subfertility. There may be a substantial portion of women with infertility or subfertility among attendees at the postpartum visit, who did not make an active choice about contraceptive method. This may explain the low rate of abortion in this group.
Depending on the time of delivery during the index year, the follow-up period varied between 12 and 24 months meaning that the observation time differed between women in the cohort.
Conclusion
The proportion of women with abortion during the study period was surprisingly low (2.5%). The decision to use a LARC method postpartum and exclusive breastfeeding at the time of the postpartum visit significantly decreased the risk of abortion in the study period, whereas smoking, age <25 years and have had a previous abortion significantly increased the risk.
Relevance of the findings: implications for clinicians and policy-makers/health care providers
The results highlight the importance of emphasising the superiority of LARC methods and increasing the proportion of women deciding to use LARC postpartum for prevention of unintended pregnancy and abortion. Improving attendance at postpartum follow-up is a prerequisite for LARC uptake. However, immediate postpartum insertion of intrauterine contraceptives might have an even higher impact on LARC uptake in women who would otherwise not have chosen these methods.
Unanswered questions and future research
There is a need for more research on the timing of counselling; effective methods of counselling; and factors affecting the choice, use, and continued use of contraception in the postpartum period.
Author contributions
K.L.L. and J.B. made substantial contributions to the conception and design of the study, analysis and interpretation of the data and drafting of the article. H.K.K. contributed to the analysis and interpretation of the data and drafting of the article. All authors approved the final version to be published.
Acknowledgements
The authors thank Mats Fredrikson (Linköping University, Linköping, Sweden) and Fredrik Johansson (Danderyd Hospital, Stockholm, Sweden) for providing statistical advice.
Disclosure statement
The authors declare that there is no duality of interest associated with this manuscript.
Additional information
Funding
References
- Cameron S. Postabortal and postpartum contraception. Best Pract Res Clin Obstet Gynaecol. 2014;28:871–880.
- Falk G, Ostlund I, Magnuson A, et al. Teenage mothers – a high-risk group for new unintended pregnancies. Contraception. 2006;74:471–475.
- Haider S, Stoffel C, Dude A. Adolescent contraception use after pregnancy, an opportunity for improvement. J Pediatr Adolescent Gynecol. 2018;31:388–393.
- Barber JS, Axinn WG, Thornton A. Unwanted childbearing, health, and mother-child relationships. J Health Soc Behav. 1999;40:231–257.
- Mercier RJ, Garrett J, Thorp J, et al. Pregnancy intention and postpartum depression: secondary data analysis from a prospective cohort. BJOG. 2013;120:1116–1122.
- Smith GC, Pell JP, Dobbie R. Interpregnancy interval and risk of preterm birth and neonatal death: retrospective cohort study. BMJ. 2003;327:313–310.
- Heller R, Cameron S, Briggs R, et al. Postpartum contraception: a missed opportunity to prevent unintended pregnancy and short inter-pregnancy intervals. J Fam Plann Reprod Health Care. 2016;42:93–98.
- Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactating women: a systematic review. Obstet Gynecol. 2011;117:657–662.
- McDonald EA, Brown SJ. Does method of birth make a difference to when women resume sex after childbirth? BJOG. 2013;120:823–830.
- Peipert JF, Madden T, Allsworth JE, et al. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120:1291–1297.
- Kilander H, Alehagen S, Svedlund L, et al. Likelihood of repeat abortion in a Swedish cohort according to the choice of post-abortion contraception: a longitudinal study. Acta Obstet Gynecol Scand. 2016;95:565–571.
- Korjamo R, Heikinheimo O, Mentula M. Risk factors and the choice of long-acting reversible contraception following medical abortion: effect on subsequent induced abortion and unwanted pregnancy. Eur J Contracept Reprod Health Care. 2018;23:89–96.
- Bäckström A, Glantz A, Johansson AC, et al. Revised web version 2016. Maternal, sexual and reproductive health [in Swedish]. 2008. [cited 2019 Sep 15]. Available from: www.sfog.se/natupplaga/ARG76web43658b6c2-849e-47ab-99fa-52e8ac993b7d.pdf
- Petersson K, Conner P, Wikström AK. 2017. The yearly report of the register of pregnancy [in Swedish]. [cited 2019 Oct 10]. Available from: www.medscinet.com/GR/uploads/hemsida/dokumentarkiv/GR_Årsrrapport_2017_4.0.pdf
- Grossman D, Ellertson C, Grimes DA, et al. Routine follow-up visits after first-trimester induced abortion. Obstet Gynecol. 2004;103:738–745.
- Hognert H, Kopp Kallner H, Cameron S, et al. Immediate versus delayed insertion of an etonogestrel releasing implant at medical abortion – a randomized controlled equivalence trial. Hum Reprod. 2016;31:2484–2490.
- Baldwin MK, Edelman AB, Lim JY, et al. Intrauterine device placement at 3 versus 6 weeks postpartum: a randomized trial. Contraception. 2016;93:356–363.
- Brunson MR, Klein DA, Olsen CH, et al. Postpartum contraception: initiation and effectiveness in a large universal healthcare system. Am J Obstet Gynecol. 2017;217:55e1–55e9.
- Statistics of pregnancies, births and newborns [in Swedish]. [cited 2019 Aug 20]. Available from: https://sdb.socialstyrelsen.se/if_mfr_004/val.aspx
- Lundqvist E. Statistics database for breast feeding [in Swedish]. 2016. [cited 2019 May 4]. Available from: https://sdb.socialstyrelsen.se/if_amn/val.aspx
- Sarki M, Parlesak A, Robertson A. Comparison of national cross-sectional breast-feeding surveys by maternal education in Europe (2006–2016). Public Health Nutr. 2019;22:848–861.
- Baldwin MK, Hart KD, Rodriguez MI. Predictors for follow-up among postpartum patients enrolled in a clinical trial. Contraception. 2018;98:228–231.
- Öman M, Lundqvist E, Karin K. 2015. Statistics on induced abortions 2014 [in Swedish]. [cited 2019 Jun 7]. Available from: www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2015-9-4.pdf
- Oduyebo T, Zapata LB, Boutot ME, et al. Factors associated with postpartum use of long-acting reversible contraception. Am J Obstet Gynecol. 2019;221:43.e1–43.e11.
- Chen MJ, Hou MY, Hsia JK, et al. Long-acting reversible contraception initiation with a 2- to 3-week compared with a 6-week postpartum visit. Obstet Gynecol. 2017;130:788–794.
- Goodman S, Hendlish SK, Benedict C, et al. Increasing intrauterine contraception use by reducing barriers to post-abortal and interval insertion. Contraception. 2008;78:136–142.
- Gurtcheff SE, Turok DK, Stoddard G, et al. Lactogenesis after early postpartum use of the contraceptive implant: a randomized controlled trial. Obstet Gynecol. 2011;117:1114–1121.
- Cameron ST, Craig A, Sim J, et al. Feasibility and acceptability of introducing routine antenatal contraceptive counselling and provision of contraception after delivery: the APPLES pilot evaluation. BJOG. 2017;124:2009–2015.
- Gallagher B, Cameron ST, Craig A, et al. Antenatal contraception counselling and provision of contraception after delivery for first-time young mothers enrolled with a Family Nurse Partnership programme. BMJ Sex Reprod Health. 2019;45:243–248.
- Whaley N, Burke A. Contraception in the postpartum period: immediate options for long-acting success. Womens Health (Lond). 2015;11:97–99.
