Abstract
Objectives
Latvia has one of the highest numbers of new HIV cases in the EU. The latest SRH national survey confirmed low effective contraceptive prevalence in the general population, no data were available about women living with HIV (WLHIV). The study aimed to assess knowledge on the use of different contraceptives, to identify factors in choosing contraception, to assess the availability of family planning health care services, and to investigate contraception habits.
Methods
A cross-sectional study was conducted among WLHIV aged 18–49 recruited with assistance of non-governmental organisations addressing HIV issues. Interviews in Latvian and Russian languages were based on pre-tested questionnaire. Data were processed and analysed using IBM SPSS 22.0.
Results
102 WLHIV were interviewed and 99 of them met the inclusion criteria. Most women were aware of at least one effective contraceptive method yet around half of them had misconceptions about hormonal methods. Most of the women were able to evaluate the effectiveness of contraceptives. Sexually active women usually used male condoms (76.3%) although around 40% did not use them permanently especially if their partner was HIV-positive. Contraception usage after HIV infection decreased. Women mainly trusted medical professionals on information provided about contraceptives. Over 50% of women experienced situations they could not afford a visit to a gynaecologist or contraceptives.
Conclusions
The survey showed a wide prevalence of misconceptions and prejudice about hormonal contraceptives. There is a need for health education including sexuality education and financial support to make effective contraception available and affordable for WLHIV.
摘要
目的:拉脱维亚是欧盟新感染艾滋病毒人数最多的国家之一。最新的性健康和生殖健康全国调查证实, 总体人群中有效避孕的普及率很低, 且没有关于感染艾滋病毒妇女(WLHIV)的数据。这项研究的目的是评价使用不同避孕药具的知识, 确定选择避孕药具的因素, 评估计划生育保健服务的可获得性, 并调查避孕习惯。
方法:在非政府组织协助下, 招募18-49岁WLHIV患者进行横断面研究。基于预先测试的问卷, 以拉脱维亚语和俄语进行访谈。采用IBM SPSS 22.0软件对数据进行处理和分析。
结果:102例WLHIV患者进行了访谈, 其中99人符合纳入标准。大多数女性知道至少一种有效的避孕方法, 但约半数的人对激素避孕存在误解。大多数妇女能够评估避孕措施的有效性。有76.3%性活跃的女性会经常选择男用避孕套, 尤其当伴侣是艾滋病毒阳性时, 但约40%的女性不会长期使用。感染艾滋病毒后, 避孕药具的使用有所减少。妇女主要信任医疗专业人员提供的有关避孕药具的信息。超过50%的妇女经历过不能负担去妇科就诊或购买避孕药具的情况。
结论:调查显示, 对激素避孕普遍存在误解和偏见。有必要进行包括性教育在内的健康教育以及财政支持, 使艾滋病感染者能够获得并负担得起有效的避孕措施。
Keywords:
Introduction
Every year around 200 to 400 new cases of HIV infection are registered in Latvia [Citation1] leading to one of the highest rates of new HIV cases among the European Union countries. The highest HIV transmission in Latvia is via heterosexual relationships, followed by an unknown route of infection [Citation1]. In 2020, there were 257 new cases of HIV/AIDS of which 235 were for people aged 18–49 (). Around one third of cases were among women of childbearing age [Citation2].
Table 1. HIV/AIDS cases from 2018 to 2020 in Latvia [Citation2].
Table 2. Characteristics of HIV-infected women included in the focus group (n = 99).
It is important to note that the fertility of HIV-infected women is not significantly different from healthy women of reproductive age [Citation3], and most of the HIV-infected women are sexually active. Nowadays the availability of antiretroviral therapy (ART) and the prevention and treatment of opportunistic infections has significantly improved the quality of life in this group. Reduction of vertical transmission with ART and increasing life expectancy have also affected the opportunities and desires of reproductive potential for HIV-infected women [Citation4]. Some HIV-infected women have a low socioeconomic status, which correlates with a lack of knowledge and support related to sexual and reproductive health, including the choice of contraception. These women are at risk of unplanned pregnancies and abortion [Citation5].
Knowledge and access to effective methods of contraception play an important role in ensuring good sexual and reproductive health, achieving personal reproductive goals and preventing unintended pregnancies [Citation6]. Although effective methods of contraception are available in Latvia, the contraceptive prevalence in women living with HIV (WLHIV) is unknown. Other studies confirm low use of effective contraception among WLHIV [Citation7,Citation8].
The objectives of the study were to understand if WLHIV in Latvia receive adequate information on their contraceptive choices, use optimal methods of contraception according to their individual lifestyle and reproductive goals, and have access to health services and contraceptives. We also sought to investigate contraception use and habits before HIV infection and with HIV.
Methods
A cross-sectional study was conducted to assess the knowledge, attitude and use of contraception among HIV-positive women. The study population consisted of WLHIV aged 18–49 years. A focus group was recruited from non-governmental organisations: AGIHAS (www.agihas.lv) and DIA + LOGS (www.diacentrs.lv), based in Riga, Latvia. Both organisations are providing support for people living with HIV.
Data were collected using a pre-tested and structured questionnaire that was developed by a research team. The interview was conducted either in Latvian or Russian languages, depending on the participant’s preferences. After informed consent, together with trained interviewers, survey participants completed a questionnaire about their reproductive history, knowledge and attitudes about different contraceptive methods, past and present contraceptive use and access to healthcare services. The participants’ demographic data and partners’ HIV status were also recorded. Interviews took place from March 2019 until October 2020. Participants’ time was compensated with a 10 Euro gift card and booklet with information on available methods of contraception.
Data were processed and analysed using IBM SPSS 22.0, using descriptive analysis of population characteristics, contraception knowledge and use. Contraceptive methods used before and after HIV diagnosis were compared using McNemar-Bowker test. Data were considered statistically significant if p value was <.05. The study was approved by the Research Ethics Committee of Riga Stradins University.
Results
The demographic profile of the study group ()
In total 102 WLHIV were interviewed, 99 met the inclusion criteria (18–49 years old, HIV-positive women) and their responses were used for further analysis. The mean age of the study group participants was 33 years with the range from 19 to 47 years.
Most women had secondary education (52.5%, n = 52), almost one third (29.3%, n = 29) had completed elementary school and 10.1% (n = 10) had not finished elementary school. More than a half (52.1%, n = 51) were employed.
Most of the study group women (98.0%, n = 97) were heterosexual, 47.5% (n = 47) were in an unregistered relationship with one partner, 16.2% (n = 16) in a registered relationship (married), 12.1% (n = 12) were in relations with several partners and 10.1% (n = 10) had a casual relationship. Most of the partners (79.8%, n = 79) of women in the study group were informed about their HIV status.
One third of women were diagnosed with HIV during the last 5 years. The status of diagnosis and treatment of participants is presented in . Overall, 81.0% (n = 80) were on highly active antiretroviral therapy (HAART).
Table 3. The status of HIV diagnosis and treatment.
When summarising information from the study group about the HIV status of their partners, almost half (46.5%, n = 46) were HIV-negative, meanwhile 27.3% (n = 27) were HIV-positive and HIV status of 16.2% (n = 16) remained unknown.
Assessment of sexual and reproductive health
Most of participants (81%, n = 80) were sexually active during the last 12 months, having sexual intercourse from more than once a week (61.2%, n = 60) to more than once a month (15.3%, n = 15) or even less than once a month (11.3%, n = 11).
When asked about satisfaction with their current sex life, 44.9% (n = 44) were fully satisfied, 27.6% (n = 27) were rather satisfied, 8.2% (n = 8) were rather dissatisfied and 5.1% (n = 5) were not satisfied. Almost each fifth woman (16.5%, n = 16) noted they had problems with their sex life (decreased interest, inability to reach orgasm, etc.). Women were asked to rate their sexual and reproductive health during the last 12 months: 48.0% (n = 47) rated it as good, 31.6% (n = 31)- as average, 11.2% (n = 11)- as bad.
More than a half of women have been pregnant (64.3%, n = 63) in the past, including miscarriage and induced abortion, 49.5% (n = 48) have had birth. After HIV was diagnosed, 30.6% (n = 30) of women had pregnancy and 34.3% (n = 24) had birth. The vertical transmission of HIV occurred in 3 cases (12.5%). When asked if respondents would like to have children in the future, 33.3% (n = 33) answered they did not wish to have children, 23.2% (n = 23) were not sure and 19.2% (n = 19) would like to have children.
More than a half (54.1%, n = 53) of women stated that they are responsible for preventing pregnancy, 25.5% (n = 25) said that both partners were responsible.
Knowledge of WLHIV about methods of contraception and sources of information
When asked about what contraceptive methods women were aware of, 91.9% (n = 91) mentioned male condoms, 69.7% (n = 69) coitus interruptus, 68.7% (n = 68) hormonal contraceptive pills, 54.5% (n = 54) non-hormonal IUD, 42.4% (n = 42) hormonal IUD, 47.5% (n = 47) calendar method, 40.4% (n = 40) male sterilisation, 41.4% (n = 41) female sterilisation and 54.5% (n = 54) were aware of emergency contraception.
Almost a half (46.4%, n = 45) of the women in the study group were not aware of the effect of pills on the menstrual cycle, 58.8% (n = 57) women thought that taking pills causes weight gain, 46.9% (n = 45) thought that it was hard to remember to take birth control pills every day. More than one fourth of the WLHIV (26.8%, n = 26) agreed that the use of contraceptive pills dispels fear of unwanted pregnancy, while even more (30.9%, n = 30) disagreed. 39.2% (n = 38) of the study group women agreed that the use of contraception creates positive emotions during sexual intercourse.
In this study, the incorrect understanding about emergency contraceptives mechanism of action is common, as 35.1% (n = 34) considered emergency contraception as a method similar to an abortion and 47.9% (n = 46) considered emergency contraception being harmful for health. More than a half of women (54.6%, n = 53) did not know the effects of contraceptives on HIV infection and 59.2% (n = 58) agreed with statement that women who use hormonal contraception have an increased risk of oncological disease.
When women were asked to indicate what contraceptive methods they consider to be an effective, 86.6% (n = 84) noted male condoms as being effective contraceptive method, only half of WLHIV considered pills (56.3%, n = 54), non-hormonal IUD (55.3%, n = 52) and hormonal IUD (51.1%, n = 48) being effective contraceptive methods, 42.7% (n = 41) said that coitus interruptus was not an efficient method and 37.6% (n = 35) considered calendar method as ineffective. Most of study participants (85.7%, n = 84) were aware that condoms prevent sexually transmitted infections (STIs), including HIV.
The main source of information about contraception was a gynaecologist (59.6%, n = 59), followed by friends (56.5%, n = 56) and the internet (53.5%, n = 53). WLHIV would prefer to receive information from a gynaecologist (75.8%, n = 75), the internet (53.5%, n = 53) and from a general practitioner (46.5%, n = 46).
Contraceptive methods used by HIV-positive women and factors affecting choice of contraception
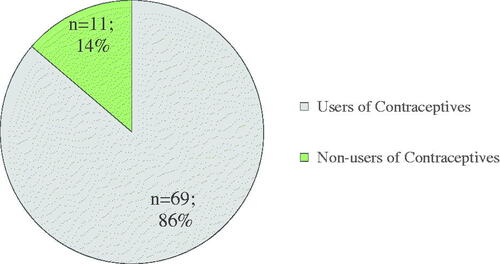
From 99 responders who participated in the survey, 80 (81%) self-reported as being sexually active. Among them, 86.3% (n = 69) women were currently using contraceptives ().
The most used method was male condoms (76.3%, n = 61). More than a half (63.9%, n = 39) of condom users reported it as their only method of contraception. Most (72.0%, n = 44) of the current condom users have used condoms during the last 12 months to prevent pregnancy, 65.6% (n = 40) to prevent HIV transmission and 44.3% (n = 27) to prevent other STIs. More than a half (60.7%, n = 37) of the condom users used them during each sexual intercourse, meanwhile the rest (39.3%, n = 24) of WLHIV were not using condoms permanently. Women who reported sexual relationships with HIV-negative partner were significantly more likely to use condoms consistently (33.3%) than those who reported their partner to be HIV-positive (5.1%), p = .015.
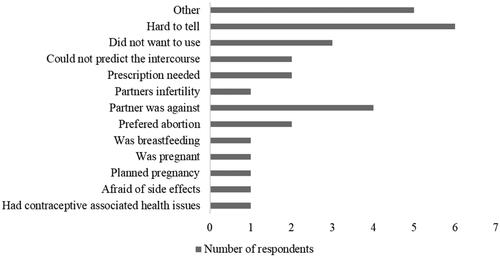
The second most used method of contraception was combined contraceptive pills (15.0%, n = 12), however, 22.6% (n = 18) of sexually active women were using natural contraceptive methods: 1.3% (n = 1) used calendar method and 17.5% (n = 14) coitus interruptus, but 3.8% (n = 3) were using ‘vaginal douching’ as a contraception. Only two WLHIV reported using non-hormonal IUD. No injectable, hormonal patch or ring were used. A total 17.5% (n = 14) of the contraceptive users reported using dual contraception (male condoms in combination with a more effective contraceptive method), but 13.7% (n = 11) of women who had sexual relations did not use any contraception. The reasons for not using contraception are presented in .
Contraceptive choices before and after diagnosis of HIV were compared (). Study participants reported significant changes in the methods of contraception they used. More women used combined oral contraceptive pills and other reversible hormonal contraception methods (hormonal IUDs, injections, rings) before they were diagnosed with HIV. The same tendency was seen in the use of emergency contraception, withdrawal and vaginal douching. Significantly fewer women used dual contraception (male condom with other method) after diagnosis of HIV. We could not determine which factors contributed to decreased condom use after HIV was diagnosed.
Table 4. Self-reported use of contraceptive methods among 80 sexually active women before and after HIV diagnosis.
Women were asked which factors other than prevention of pregnancy and HIV transmission were important for them when they made a contraceptive choice. For 72.0% (n = 54) of WLHIV the preference was given to over-the-counter methods. 67.1% (n = 51) noted the price and 76.3% (n = 58) ease of use as important factors, 34.7% (n = 26) made their choice in favour of methods that did not require partners' agreement while 53.4% (n = 39) considered the wishes of the partner. Also, an impact on health, such as not changing the body weight (52.7%, n = 39) and regulation of the menstrual cycle (40.0%, n = 30), were emphasised as important factors by WLHIV.
Access to health care services for HIV-positive women
For women living with HIV, it is fundamental to have access to reproductive health care services and to meet their family planning needs. More than half of WLHIV of the study group attend gynaecologist at least once a year (67.7%, n = 67). Unfortunately, 60.5% (n = 58) of them noted having a situation where they could not afford a visit to a gynaecologist and 54.3% (n = 52) a visit to a general practitioner. Additionally, 53.8% (n = 49) of women have had occasions when they could not afford contraceptives.
Discussion
Findings and interpretation
In this study, women’s awareness of contraception methods were incomplete, because the knowledge about the highly effective methods (mostly hormonal) was limited. A consideration that emergency contraception is a similar method to abortion uncovered the incorrect understanding about emergency contraceptives mechanism of action. This may be an important perception to counter in any education efforts.
Belief in different misconceptions about hormonal contraception effects on weight gain or risk of oncological diseases, indicates inaccurate representations of hormonal methods of contraception in the mass media. Efforts should be made to educate women about hormonal contraception to improve women’s knowledge.
The results of women’s awareness suggest that WLHIV in Latvia are generally poorly informed with regards to effectiveness about hormonal methods of contraception. However, most of WLHIV were well informed about the effectiveness of some methods to prevent STIs, HIV.
Our study showed that male condoms were the most used contraception method with more than a half of WLHIV reporting condoms as the only contraception. One of the reasons for that might be the free availability of condoms at non-governmental organisations.
A great proportion of participants of our study had primary education and were unemployed, we believe this may partly explain the use of less effective and cheaper methods of contraception as expenses related to contraception are not covered in Latvia for WLHIV and any other group.
Differences and similarities in relation to other studies
In studies from high and low-income countries, most WLHIV reported being sexually active [Citation4,Citation9,Citation10], so did the women from our study. There is no doubt that they have the same rights as HIV-negative women to get information and access to a wide range of effective contraception and reproductive health services to meet their fertility desires, contraception needs and wellbeing regardless of ART [Citation11].
Our study confirmed that the most reliable source of information about contraception for WLHIV was health professionals, similar to studies in other countries [Citation12]. Also, studies indicated the influence of family and peers regarding contraception knowledge [Citation13], others reported the importance of media [Citation14].
WLHIV in Latvia faces different myths and misconceptions about the effects of hormonal contraception on HIV treatment, health and wellbeing and the use of effective contraception in general. Some participants believed that IUDs are not suitable for nulliparous women, others agreed that hormonal contraception may lead to infertility or oncologic diseases. Similar misconceptions about side effects and health problems associated with contraceptive methods were reported by authors in other countries [Citation15,Citation16]. As a result, these misconceptions and fears about contraceptive safety and ART during pregnancy put WLHIV at increased risk for unintended pregnancy and HIV vertical transmission to their children.
The fact that condoms are the most commonly used contraceptive in the Latvian population was confirmed by the National SRH survey in 2011. According to the survey, it was used by 41% of sexually active women and 51% of men [Citation17]. However, we found that one third of WLHIV were not consistently using condoms during every sexual intercourse. Similar results were described in a large clinical trial in the US [Citation18]. The condom underuse has been noted among HIV-positive women not desiring to be pregnant in spite of continuous counselling [Citation4,Citation18,Citation19]. Several research studies have described the factors that shape inconsistent condom use [Citation18,Citation20]. As some of the WLHIV had not disclosed their HIV status to their partners, it can be hypothesised that they face fear and are more likely to accept their partners’ unwillingness to use condoms [Citation4]. It has been well described that in the case of ‘commonly used’, about 13 pregnancies occur per 100 women whose partners use male condoms over the first year, but it decreases to only 2 pregnancies per 100 women when used correctly with every act of sex [Citation9]. Needless to say, with inconsistent condom use the risk of unintended pregnancies for those women increases, making their contraception needs unmet.
This study demonstrated that HIV-positive women in Latvia are less likely to have used or currently use the most effective contraceptive methods despite being informed about IUDs and implants as effective methods. The same tendency among HIV-positive women was demonstrated in studies from other countries- WLHIV were less likely to use long-acting reversible contraceptives [Citation7,Citation8,Citation10]. The latest national SRH survey in Latvia from 2011 confirmed a similar attitude towards hormonal contraception in the general population [Citation17]. It also highlighted that an important reason for non-use of hormonal contraception is relatively difficult access, i.e., difficulties in getting a prescription, women have to visit a doctor [Citation17].
A number of studies have emphasised the need for systematic condom use together with other contraceptive methods (dual protection) for HIV-positive women and their partner(s) [Citation9,Citation21]. Less than 18% of our respondents used dual protection, which is a comparatively good indicator as some authors observed that dual protection was used only by 3.5% of WLHIV [Citation22] while others noticed dual protection among 18 to 27% of the target population [Citation20,Citation23,Citation24].
Strengths and weaknesses of the study
The strengths of this study was in the use of pre-tested questionnaires and method of an interview as the answers were acquired via face-to-face interviews by trained interviewers. Moreover, gift cards facilitated the involvement of respondents as WLHIV are still stigmatised and reluctant to disclose its HIV status to strangers. The study also made a contribution to the education of WLHIV in non-governmental organisations about the wide variety of contraceptive methods.
A major limitation of this study was limited access to the focus group. Our team of researchers faced unpredictable difficulties in getting permission to interview HIV-positive women in HIV patient health care centres. As the next step, the women were addressed through non-governmental organisations and to motivate women to participate in the study gift cards were offered. As we started our study, we noticed that a large proportion of people with HIV avoided participating or giving any sensitive information about themselves, and the main explanation is that in Latvia many still face negative attitudes and beliefs about people living with HIV. As a result, some participants experienced discomfort answering sensitive questions, and it might lead to bias in response.
COVID-19 has created a challenging environment for on-site surveys. Since many people experienced significant fear and anxiety during COVID-19 infection outbreak, the recruitment of WLHIV has decreased and the number of desired respondents has not been reached.
Unfortunately, we were not able to compare the results of this study with the up-to-date data from the general population as the latest representative national SRH survey including contraception in Latvia was carried out in 2011.
Finally, the study population was invited mainly from non-governmental organisations based in the capital city, one of which provides support mainly for HIV-positive current drug users, and this may not be generalisable for the HIV-positive female population in Latvia.
Implications for clinicians and policymakers
As women experience financial difficulties in accessing the most effective reversible methods of contraception such as IUDs or implants, it is very important to ensure support from Latvia’s policymakers and programme managers in achieving reproductive health goals for every WLHIV. It is crucial to provide WLHIV, especially from social risk groups (drug users, women engaged in sex work, etc.), with not only free of charge barrier methods but also with a long term effective reversible contraceptives. It is a critical and cost-effective approach in improving the quality of life of WLHIV and decreasing the risk of unintended pregnancy [Citation25,Citation26]. Since 2019 the Ministry of Health of Latvia has been developing regulations on the governmental support to vulnerable and disadvantaged population groups in improving access to contraception, COVID-19 has slowed down this activity.
Importantly, our study highlights the need to improve access to reproductive health services. Health care providers should pay attention to women’s, including WLHIV, fertility desires and provide competent preconception counselling for every woman to optimise effective contraception meeting the needs of a woman, proper medication use, maximise disease control and minimise the probability of HIV vertical transmission.
Introducing such improvements might help WLHIV to better understand the importance of effective contraception and to make informed choices.
Unanswered questions and future research
As the data showed inconsistent use of condoms, a more detailed evaluation of factors that shape male condom use should be made. It was also noted that WLHIV were informed about effective methods of contraception, but rarely used them.
After HIV diagnosis, WLHIV participating in this study reported a decrease in effective hormonal methods use. The reasons are not clear and might be attributed to the changes in sexual behaviours.
Healthcare providers were the first person of contact when WLHIV sought information about suitable contraception methods. However, there is growing evidence that provider-imposed restrictions and misconception or even ignorance of the method use may affect the highly effective method uptake [Citation19,Citation27]. The low usage of effective methods of contraception might be attributed to the poor counselling programs, but further research is needed to evaluate healthcare providers’ knowledge and perceptions regarding the use of highly effective contraception methods among HIV-positive women in Latvia.
Conclusions
WLHIV in Latvia are informed about different contraceptives. They are not fully aware of the efficiency of the methods. There is a high level of contraceptive use among sexually active WLHIV, however, every fifth uses contraception with low effectiveness and there is a high rate of condom users who does not use condoms permanently. Our survey showed the wide prevalence of misconceptions and prejudice about hormonal contraceptives. Contraceptive use after HIV infection decreased, but the reasons require further studies. Important factors influencing the choice of contraception are price, ease of use, no need for a prescription and agreement of partner, as well as partners’ wishes. WLHIV in Latvia experience situations when SRH care services are not available and face financial difficulties in obtaining contraception. There is a need for health education including sexuality education and financial support to make effective contraception available and affordable for every WLHIV in Latvia.
Acknowledgments
The authors would like to acknowledge the non-government organisations AGIHAS and DIA + LOGS for their support in recruiting participants for the study. We would also like to thank every woman for their participation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Spkc.gov.lv [Internet]. Latvia: CDPC of Latvia. 2020; [cited 2022 Jan 2]. Available from: https://www.spkc.gov.lv/lv/hivaids-statistika.
- Spkc.gov.lv [Internet]. Latvia: CDPC of Latvia. 2020; [cited 2022 Jan 2]. Available from: https://www.spkc.gov.lv/lv/infekcijas-slimibas-un-imunizacija.
- Haddad LB, Wall KM, Mehta CC, et al. Trends of and factors associated with live-birth and abortion rates among HIV-positive and HIV-negative women. Am J Obstet Gynecol. 2017;216(1):71.e1–71.e16.
- Stanwood NL, Cohn SE, Heiser JR, et al. Contraception and fertility plans in a cohort of HIV-positive women in care. Contraception. 2007;75(4):294–298.
- Sutton MY, Zhou W, Frazier EL. Unplanned pregnancies and contraceptive use among HIV-positive women in care. PLoS One. 2018;13(5):e0197216.
- Sherwood J, Lankiewicz E, Roose-Snyder B, et al. The role of contraception in preventing HIV-positive births: global estimates and projections. BMC Public Health. 2021;21:536.
- Massad LS, Evans CT, Wilson TE, et al. Contraceptive use among U.S. women with HIV. Journal of Women's Health. 2007;16(5):657–666.
- Badell ML, Lathrop E, Haddad LB, et al. Reproductive healthcare needs and desires in a cohort of HIV-positive women. Infect Dis Obstet Gynecol. 2012;2012:1–6.
- Apps.who.int [Internet]. Latvia: WHO; 2018; [cited 2022 Jan 29]. Available from: https://apps.who.int/iris/bitstream/handle/10665/260156/9780999203705-eng.pdf?sequence=1.
- Jones DL, Cook R, Potter JE, et al. Fertility desires among women living with HIV. PLoS One. 2016;11(9):e0160190.
- Refworld.org [Internet]. Latvia: WHO; 2006; [cited 2022 Jan 2]. Available from: https://www.refworld.org/docid/48abd5960.html.
- Wilson TE, Koenig LJ, Walter E, et al. Dual contraceptive method use for pregnancy and disease prevention among HIV infected and HIV uninfected women: the importance of an event-level focus for promoting safer sexual behaviors. Sex Transm Dis. 2003;30(11):809–812.
- Apps.who.int [Internet]. Latvia: WHO. 2019; [cited 2022 Jan 29]. Available from: https://apps.who.int/iris/bitstream/handle/10665/325859/WHO-CDS-HIV-19.19-eng.pdf.
- Mazzei A, Ingabire R, Karita E, et al. Cross-sectional assessment of government health center needs to implement long-acting reversible contraception services in rural Rwanda. BMC Women’s Health. 2021;21(1):3.
- Kaida A, Patterson S, Carter A, et al. Contraceptive choice and use of dual protection among women living with HIV in Canada: priorities for integrated care. Perspect Sex Repro H. 2017;49;(4):223–236.
- Nkwabong E, Minda V, Fomulu JN. Knowledge, attitudes and practices of contraception by HIV positive women followed in a Cameroon region with high illiteracy rate: a cross sectional study. Pan Afr Med J. 2015;20:e5252.
- Idris M, Wolday SJ, Hassan DN, et al. Contraception use among HIV-positive women attending ART clinic: a cross-sectional study in Halibet referral hospital. Global Reproductive Health. 2021;6(3):e55–e55.
- Melaku YA, Berhane Y, Kinsman J, et al. Sexual and reproductive health communication and awareness of contraceptive methods among secondary school female students, Northern Ethiopia: a cross-sectional study. BMC Public Health. 2014;14:252.
- Ngome E, Odimegwu C. The social context of adolescent women’s use of modern contraceptives in Zimbabwe: a multilevel analysis. Reprod Health. 2014;11:64.
- Mbachu CO, Agu IC, Obayi C, et al. Beliefs and misconceptions about contraception and condom use among adolescents in South-east Nigeria. Reprod Health. 2021;18(1):7.
- Eshak E. Myths about modern and traditional contraceptives held by women in Minia, Upper Egypt. East Mediterr Health J. 2020;26(04):417–425.
- Papardeszieds.lv [Internet]. Latvia: Papardes zieds; 2011; [cited 2022 Jan 29]. Available from: https://www.papardeszieds.lv/wp-content/uploads/2017/02/311_PapardesZieds_WEB.compressed.pdf.
- Sheth NN, Angert CD, Haddad LB, et al. Contraception methods used among women with HIV starting antiretroviral therapy in a large United States clinical trial, 2009–2011. Contraception. 2021;103(4):225–231.
- Teodoro N, Fu A, Ohly NT, et al. Long-acting reversible contraception knowledge, attitudes and use among HIV-infected and -uninfected women and their providers. Contraception. 2019;100;(4):269–274.
- Haddad LB, Brown JL, King C, et al. Contraceptive, condom and dual method use at last coitus among perinatally and horizontally HIV-infected young women in atlanta, Georgia. PLoS One. 2018;13(9):e0202946.
- Mesfin Y, Argaw M, Geze S, et al. Dual contraceptive use and factor associated with people living with HIV/AIDS: a systematic review and meta-analysis. Infect Dis Obstet Gynecol. 2021;2021:5440722.
- Heys J, Kipp W, Jhangri GS, et al. Fertility desires and infection with the HIV: results from a survey in rural Uganda. AIDS. 2009;23(Suppl 1):S37–S45.