Abstract
Introduction: Electrosurgery is used in 80% of surgical procedures. The technique allows surgeons to skilfully dissect tissues and achieve haemostasis. Since improper use of electrosurgery can lead to serious adverse events, training is required to potentially reduce the number and severity of these events. In this study we evaluate education and training in electrosurgery for surgical residents.
Material and methods: Residents from six surgical subspecialties in the Netherlands were invited to anonymously complete a digital questionnaire about training, supervision and adverse events regarding electrosurgery.
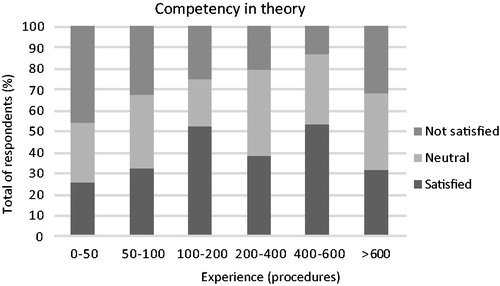
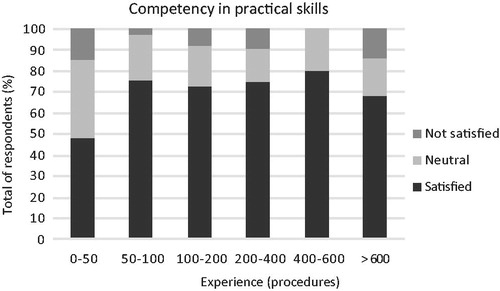
Results: Of the 197 respondents, 69% had received some form of training; mostly a single theoretical lecture. The feeling of competence in theory and practical skills was positively rated by 39% and 71%, respectively. Moreover, 35% judged the theoretical knowledge of their supervisors as insufficient and 65% changed their electrosurgical application technique to the preference of the supervisor. 30% of the residents had encountered a serious adverse event (e.g., burn wounds) related to the application of electrosurgery.
Conclusions: The training of residents in theoretical aspects of electrosurgery is limited. Residents are not satisfied with the acquired theoretical knowledge of themselves and of their supervisors. Since adverse events related to electrosurgery occur frequently, more extensive education for both residents and their supervisors is needed to enhance patient safety.
Introduction
Electrosurgery is used in over 80% of procedures across surgical specialities. The technique allows surgeons to skilfully dissect tissue and achieve rapid haemostasis. Especially in minimally invasive procedures, electrosurgery offers precise haemostatic control during complicated surgeries on structures that are highly vascular in nature. However, difficulties in predicting the effects of combinations of the magnitude of electrical current, heat generation, numerous patient factors, and the interactions with other surgical tools can lead to severe complications.
Complications from electrosurgical devices come in reproducible patterns, such as faulty direct application and insulation failure [Citation1]. A direct application injury can result in spreading thermal heat beyond the tissue that the surgeon intended to treat. Hence vulnerable tissue, such as the bowel, can be harmed and this could seriously influence a patient’s outcome. Insulation failure is a defect in the insulating material that covers the instrument. Such defects occur in 13–39% of laparoscopic instruments [Citation1]. Generally, the incidence of complications due to unintended surgical energy is 1–2 per 1000 procedures [Citation2]. This is comparable to other high-profile surgical safety issues, such as retained surgical foreign bodies, which has an incidence of 0.7–1 per 1000 abdominal surgeries [Citation3]. Since it is easy to misdiagnose surgical burns or thermal injuries, the prevalence of complications is likely to be under-reported by the surgical community [Citation4]. To use electrosurgical devices to their fullest potential, it is necessary for the clinicians to have a thorough understanding of the working principles, the potential risks, and the appropriate settings for each procedure and each type of device. However, studies have shown that among clinicians this knowledge is insufficient [Citation5–11].
The problem of insufficient training on operating room technologies is also ranked fifth on the list of 2016 Top 10 Health Technology Hazards, published by the Emergency Care Research Institute (ECRI) institute [Citation12]. The Institute estimates that approximately 70% of accidents involving a medical device can be attributed to user error or the technique of use. Many of these incidents could have been avoided if the user had a better understanding of the instructions and operation principle of the device. However, currently there is no official training curriculum about electrosurgery available for surgeons, nurses, and other operating staff [Citation5]. Although some excellent resources are available, such as the recommendations from the Association of periOperative Registered Nurses (AORN) on the safe use of electrosurgery, these do not address the full range of devices and have no assessment component [Citation13]. Brill et al. suggested that medical societies should set standards of practice for laparoscopic monopolar electrosurgery [Citation4]. Feldman et al. made an initial analysis of the demands and wishes for training, as well as of the present status of physician’s knowledge regarding surgical energy [Citation14]. Together with the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), Feldman developed the Fundamental Use of Surgical Energy (FUSE) program [Citation15–17], which is an online educational teaching module complemented with an exam.
Limited training opportunities for physicians are not only recognized in the field of electrosurgery, but are present on a large scale. Recently, the Dutch Healthcare Inspectorate (DHI) published its concerns on the rapid increase of medical technology in hospitals and related risk for patient safety [Citation18]. According to this report, training of personnel is generally unstructured and uniformity across the country is lacking. Moreover, no high-quality structured assessment system that guarantees qualified and competent staff is available. In response to these findings, the DHI demanded a discipline-exceeding approach to these problems [Citation19]. This included a demand for structured training programs for high-risk medical technology and its implementation into specialist training programs. However, three years later, a subsequent report revealed that the proposed measures to ensure the safe use of medical technology have not been fully executed yet [Citation20].
The relatively slow implementation of improvements may be due to the lack of insight in how electrosurgical training is currently organised, and what the exact needs are to achieve better outcomes. In this paper, we investigate how theoretical and practical training of electrosurgery is balanced during the residency of surgical residents. We question how residents judge their own competences and those of their supervisors. We further study how often they encounter incidents or near misses due to a lack of competences during the use of electrosurgery. We did so by conducting a digital survey among surgical residents.
Material and methods
Participants
All Dutch residents from six surgical subspecialties (general surgery, gynaecology, urology, thoracic surgery, plastic surgery and orthopaedic surgery) were invited to fill out anonymously a digital questionnaire about electrosurgery between August and December 2015. They were approached by the affiliated resident associations through e-mail or newsletter.
Questionnaire
The survey was developed in Collector (Version 6.7, Zurich, Austria) and contained 31 questions, both open-end and close-end. The first questions were of general content and informed about the respondent’s background. Then the current situation of education in electrosurgery was investigated by ten questions about the character, frequency, practical and theoretical aspects of the training. Subsequently, through a five-point Likert scale (1: strongly disagree, 5: strongly agree), the respondents could evaluate on statements about their own electrosurgical competences and their use in the OR [Citation21]. In addition, the residents were asked to share any incidents concerning electrosurgery, and the way it was dealt with by the attending personnel. The final part covered the competences of the supervisors and other OR staff, and the general importance of electrosurgery. In Textbox 1 a summary of the survey questions can be found.
For seven questions, a category ‘other’ was used in addition to the given answers. For example, the question ‘Which training did you receive?’ was accompanied with the answers ‘CASH 1.1’, ‘basis laparoscopic course (BLC)’, ‘training by industrial representatives’, ‘training by hospital/department’ or ‘other; please describe below.’ CASH 1.1 is an annually three-day course for surgical residents, organized by the Dutch Society of Surgery. This course covers a range of subjects, such as basic techniques, wound treatment, infections, trauma, and also electrosurgery.
Textbox 1. A summary of the survey questions.
Questions
General
Sex, age, function, specialty, year of residency, experience
Training
Did you receive any training in electrosurgery?
If yes; please indicate for each training:
What kind of training?
What type?
Frequency
Obligatory
For practical training: indicate the material you worked with
For theoretical training: indicate the elements and risks that are covered
How did you gather the most practical knowledge?
How did you gather the most theoretical knowledge?
If you did not receive any training; please describe if you have missed this
Competences
Indicate your extent of agreement, from 0 (I strongly disagree) to 5 (I strongly agree) with the following statements:
I feel competent in the theory about electrosurgery
I feel competent in the practical skills of electrosurgery
The theory of electrosurgery is easy to learn
The use of electrosurgery is easy to learn
With the knowledge you possess now, would you know which setting to use for which procedure?
In what extent are you allowed to work without supervision?
Practical use
Which form of electrosurgery is used in the OR you work at?
In how many per cent of procedures is monopolar or bipolar electrosurgery used?
Indicate your extent of agreement, from 0 (I strongly disagree) to 5 (I strongly agree) with the following statements:
The use of electrosurgery varies per surgeon
My personal use of electrosurgery is influenced by the supervisors
My personal use of electrosurgery is influenced by the supervisor of the day
My personal use of electrosurgery will change when I’m a specialist
Incidents
Did you ever experience an adverse event regarding electrosurgery?
If yes, please explain
In how many per cent of procedures in the Netherlands does this type of incident happen?
Which measures did the personnel take after the event?
Importance of electrosurgery
Indicate your rating of the following competences, from bad - excellent
The theoretical knowledge of surgeons
The practical skills of surgeons
The theoretical knowledge of OR assistants
The practical skills of OR assistants
Indicate the level of importance, from 0 (not at all important) to 5 (very important) for the following aspects:
Enough theoretical knowledge about electrosurgery
The right way of using electrosurgery
General interest of electrosurgery in the OR
Results
Approximately 1,540 residents of the six surgical specialties were approached. A total of 217 responses were collected and 197 respondents completely filled out the survey, a response rate of 13%. A summary of the data is shown in .
Table 1. A summary of the characteristics of the respondents.
Training program
Of the 197 respondents, 69% had received training. The most frequently attended training program was the BLC course (89%) followed by the CASH 1.1 course (42%), and training given by industrial representatives (35%).
Respondents stated that their theoretical knowledge was mostly gained through educational programs (74%). Practical skills were primarily gained during supervised surgical procedures (76%). The questionnaire provided space for additional remarks about the training they had experienced so far. A total of 49 respondents expressed their concerns about the low frequency and the content of the training. The vast majority (60%) of residents who did not receive training experience this as a shortcoming in their education.
Competences
In response to the item, ‘I feel competent about the theory’, 39% of residents agreed. The rate of agreement for the item ‘I feel competent about my practical skills’ was higher with 71%. The relationship between the competency and the experience of the residents is depicted in and . In daily practice, 67% of the residents are allowed to perform surgery, thus using electrosurgical devices without supervision. When evaluating their supervisors, 75% of respondents claim that the use of electrosurgery differs per supervisor, and 72% state that their own handling is influenced by the preference of the supervisor. For 64% of respondents their use of electrosurgery even differs per day. More than one-third of residents (36%) are not satisfied with the theoretical knowledge of their supervisors. At the same time, 68% of respondents are content about the practical skills of supervisors.
Incidents
Respondents were asked about their experiences with any incidents or complications regarding electrosurgery. A total of 53 respondents (27%) encountered such an incident. From the 59 events reported, 31 were described as superficial burn wounds and 12 as lesions in intestines, vagina, or liver. Due to one of the two technical defects described, the procedure had to be cancelled. In 40 of 59 incidents the patient was harmed. And in 50% of these cases, no post-operative explanation was given to the patient. More detailed information about the incidents is shown in .
Table 2. Details of the incidents described by the residents.
Discussion
In this study, the current status of training in electrosurgery was investigated through a digital questionnaire among surgical residents. The survey also investigated the level of satisfaction in the acquired theoretical knowledge and practical skills during the residency. Moreover, opinions were asked about the use and knowledge of electrosurgery of their surgical supervisors. In addition, we asked for any encountered incidents or near misses regarding electrosurgical devices.
Since a national training curriculum does not exist, not everybody had received some form of training in surgical energy use. Mostly offered was either a single, obligatory, theoretical lecture during the CASH 1.1 course, or a more practical training during the basic laparoscopic course. Both are offered only once during the residency. Respondents complained about the low frequency of training and requested more repetition of the theory. Also, more detailed explanation of the devices’ settings was requested.
With regard to the acquired theoretical knowledge and practical skills residents do not feel fully competent. However, almost 70% of respondents are allowed to perform surgery and also use surgical energy without supervision. When it comes to the competences of the supervisors, one-third of respondents qualify the theoretical knowledge of their supervisors as poor or bad. Nevertheless, they are more satisfied with the practical skills of their superiors. Residents agree with the statement that the use of electrosurgery differs per surgeon. This could explain that the way of using electrosurgery is altered per day according to the supervisor they work with.
A wide range of incidents was reported. The majority of incidents were labelled as burn wounds, either inflicted on the patient or the surgeon. But also very severe bowel perforations were described, some resulting in long hospital stays and re-operations. In the cases described as ‘light’, no action was taken after the incident happened. In the case of serious incidents, an explanation was given to the patient, and OR personnel discussed the case together. However, an extra training or change in application of electrosurgery was rarely seen.
The respondents’ opinion about the low theoretical knowledge of their supervisors is remarkable, and of great importance when setting up a training curriculum. Transmission of knowledge and skills is essential in surgical training. In the medical field, this traditionally takes place according to the apprenticeship model (learning on the job). This means that the resident initially performs small steps of an operation under continuous supervision and is gradually allowed to expand this as the intensity of supervision decreases [Citation22]. Over the course of years, surgical training has evolved and more training programmes have been added. However, this has not been the case for electrosurgery. As long as residents question the capabilities of their supervisors, they will not get the education they need. Moreover, because of the hierarchy present in ORs, it is not likely that the safety of surgical approaches is openly discussed [Citation23]. This suggests that active participation of supervisors and experienced surgeons training programmes may be a prerequisite for success.
The results of this survey are in line with the studies from Feldman [Citation14] and Modaffari [Citation7]. They found that only a small percentage of specialists consider themselves experts in the field of electrosurgery. Other studies analysed the level of knowledge in surgical residents or specialists by tests and determined that clinicians are not sufficiently trained in electrosurgery [Citation6,Citation7,Citation11,Citation15]. It is often suggested that more hands-on training is necessary, while this survey shows that respondents would rather have more frequent theoretical sessions. Moreover, this study adds the opinion of residents about their supervisors and the way the hierarchical situation in the OR influences their daily work.
In our opinion, a reorganisation of the current training curriculum is necessary. At this point, residents do not learn enough about electrosurgery and, more important, do not feel competent. This feeling of incompetence could result from an incomplete training program. Furthermore, it is worrisome that those who do not feel competent enough are allowed to operate without supervision. This is a potentially dangerous situation for both patient and personnel. The need to monitor the competency of employees has also been recognized by the Dutch Healthcare Inspectorate [Citation19,Citation20]. They encourage hospitals to incorporate a qualified & competent system for employees. This system should include training modules and assessments to secure that personnel retain their skills and knowledge. Through up-to-date in-service training they can also improve these competences. When looking at the results of this survey, we can suggest the following for electrosurgery: A frequent mandatory training programme is needed in which the theory is fully covered, and practical use of settings is explained. E-learning modules for residents are currently under consideration by the Dutch Surgical society, but much more is needed to ensure proper education, and to guarantee safe use of electrosurgery.
Another interesting observation is the statement that residents adjust the approach to the preferences of the daily supervisors. Most supervisors often have a personal working style and may request the resident to follow. Although these professionals have years of experience, their training in medical devices might be outdated. In that sense, the residents may even have more up-to-date knowledge about the proper use of the devices. This also argues for recurrent obligated training programs for supervisors. This is emphasized by the noteworthy number of incidents reported by the residents that may be inflicted by themselves, as well as the supervisor.
One limitation of this study is that only residents from the Netherlands were addressed. Also, the response rate of the different specialties was unbalanced. However, we believe that the way the training programs are offered and organised does not differ extensively from one discipline to the other, and that this is representable for most Western European countries.
In conclusion, surgical residents are not satisfied with their acquired competences in theory and practical skills regarding electrosurgery. They are also not satisfied with the theoretical knowledge of their supervisors. Since complications regarding surgical energy occur frequently, more training for both groups is needed to ensure patient safety.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgements
The authors would like to thank the Dutch resident associations (VAGH, Jonge Urologen, VAGO, JVPC, Juniorkamer NVvT and the VOCA) for their help.
Additional information
Funding
References
- Jones DB, Brunt LM, Feldman LS, et al. Safe energy use in the operating room. Curr Prob Surg. 2015;52:447–468.
- Nduka CC, Super PA, Monson JR, et al. Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg. 1994;179:161–170.
- Hyslop JW, Maull KI. Natural history of the retained surgical sponge. South Med J. 1982;75:657–660.
- Brill AI, Feste JR, Hamilton TL, et al. Patient safety during laparoscopic monopolar electrosurgery–principles and guidelines. Consortium on electrosurgical safety during laparoscopy. JSLS. 1998;2:221–225.
- Feldman LS, Fuchshuber P, Jones DB, et al. Surgeons don't know what they don't know about the safe use of energy in surgery. Surg Endosc. 2012;26:2735–2739.
- Mayooran Z, Pearce S, Tsaltas J, et al. Ignorance of electrosurgery among obstetricians and gynaecologists. BJOG. 2004;111:1413–1418.
- Modaffari P, Panuccio E, Zimmiti G, et al. Are gynecologists sufficiently trained and educated on electro surgery and basic laparoscopic setting? Surg Endosc. 2016;30:3327–3333.
- Watanabe Y, Kurashima Y, Madani A, et al. Surgeons have knowledge gaps in the safe use of energy devices: a multicenter cross-sectional study. Surg Endos. 2016;30:588–592.
- Khan MA, Siddiqui SS, Zubair M. Safe electrosurgery use: knowledge, attitudes and practices of surgical trainees. JPMI. 2015;29: 83–87.
- Assiotis A, Christofi T, Raptis DA, et al. Diathermy training and usage trends among surgical trainees – will we get our fingers burnt? Surg-J R Coll Surg E. 2009;7:132–136.
- Hur HC, Green I, Modest AM, et al. Needs assessment for electrosurgery training of residents and faculty in obstetrics and gynecology. JSLS. 2014;18:e00293.
- ECRI Institute. Executive Brief. Top 10 Health Technology Hazards for 2016. Health Devices. 2015.
- Lee J. Update on electrosurgery. Outpatient Surgery. 2002;3:44–53.
- Feldman LS, Brunt LM, Fuchshuber P, et al. Rationale for the fundamental use of surgical Energy (FUSE) curriculum assessment: focus on safety. Surg Endos. 2013;27:4054–4059.
- Madani A, Jones DB, Fuchshuber P, et al. Fundamental use of surgical energy (FUSE): a curriculum on surgical energy-based devices. Surg Endosc. 2014;28:2509–2512.
- Madani A, Watanabe Y, Vassiliou MC, et al. Impact of a hands-on component on learning in the fundamental use of surgical energy (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc. 2014:28:2772–2782.
- Fuchshuber PR, Robinson TN, Feldman LS, et al. Fundamental use of surgical energy (FUSE) closing a gap in medical education. Ann Surg. 2015;262:20–22.
- IGZ (Dutch Healthcare Inspectorate). State of Health Care. 2008 Medical technological risks underestimated [Staat van de gezondheidszorg 2008. Risico's van medische technologie onderschat]. Den Haag: IGZ.
- Dutch Association of Hospitals (NVZ) and Dutch Association of University Hospitals (NFU). Convenant veilige toepassing van medische technologie in het ziekenhuis. [Convenant safe application of medical technology in hospitals]. Utrecht, Netherlands: Dutch Association of Hospitals; 2011.
- Dutch Healthcare Inspectorate (IGZ). Veilig gebruik van medische technologie krijgt onvoldoende bestuurlijke aandacht in de ziekenhuizen. Utrecht, Netherlands: Dutch Healthcare Inspectorate; 2014.
- Norman G. Likert scales, levels of measurement and the "laws" of statistics. Adv Health Sci Educ. 2010;15:625–632.
- Halsted WS. The training of the surgeon. B Johns Hopkins Hosp. 1904;15:267–275.
- Sexton JB, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. Brit Med J. 2000;320:745–749.