Abstract
Objective: This study aimed to evaluate the relationship between sexual activity and sexual function using questionnaires distributed to middle-aged Japanese patients with localized prostate cancer.
Methods: A total of 145 patients who underwent radical prostatectomy were enrolled in the survey reported on herein. Sexual activity and sexual function were investigated via the Expanded Prostate Cancer Index Composite (EPIC) and an original self-reported questionnaire.
Results: Of participants, 24.1% and 20.7% had sexual activity within a month period as investigated via the EPIC and original questionnaire, respectively. However, 29.7% of all those who reported sexual activity rate reported “about once every 2 months to a year,” as shown in the original questionnaire. Regarding sexual function as addressed through EPIC, no results within that questionnaire’s measure of sexual function showed significant differences among patients with a rate of actual sexual activity.
Conclusions: The present survey showed that more than quarter of preoperative middle-aged Japanese prostate cancer patients surveyed had actual sexual activity, though not within the preceding 4 weeks. To precisely evaluate sexual function of middle-aged Japanese patients, it is necessary to consider actual sexual activity.
Introduction
Sexual function after radical prostatectomy is one of the primary concerns affecting quality of life (QOL) for men with localized prostate cancer. In the era of robotic-assisted laparoscopic radical prostatectomy, a trifecta outcome (cancer control, urinary continence, and sexual function) has been considered the superior objective [Citation1,Citation2]. Accurate evaluation of preoperative sexual function is needed so that physicians can better determine adaptation to nerve-sparing surgery and follow up on postoperative sexual function. Regarding questionnaires that evaluate sexual function pre- and post-treatment of localized prostate cancer, in many cases general (e.g. International Index of Erectile Function [IIEF] [Citation3], Erection Hardness Score [EHS] [Citation4]), or cause-specific (e.g. Expanded Prostate Cancer Index Composite [EPIC] [Citation5] or University of California at Los Angeles Prostate Cancer Index [UCLA-PCI] [Citation6]) types are used. However, some questionnaires inquire on sexual activity within a certain period of time; whereby no sexual activity during that defined period leads to underestimation of sexual function. Physicians would agree that the choice of validated questionnaire used and the baseline sexual function data are important factors for evaluating postoperative sexual function [Citation7]. To evaluate the relationship between actual sexual activity and sexual function, we surveyed preoperative sexual activity using our original questionnaire, as well as the EPIC questionnaire, on middle-aged Japanese localized prostate cancer patients.
Methods
From December 2012 to December 2015, from among 365 Japanese men with localized prostate cancer who underwent radical prostatectomy at Kansai Medical University Hospital, we enrolled 145 who fully answered our original questionnaire on actual sexual activity (), as well as the EPIC questionnaire, and whose risk factors for erectile dysfunction (ED) could be collected. All patients were informed about the writing of the contents and purpose of the survey.
Table 1. Original questionnaire.
Indication of nerve-sparing prostatectomy is decided mainly based on tumor side/lesions detected from prostate biopsy and magnetic resonance imaging. Nerve sparing is performed not only for sexual function but also for prevention of postoperative urinary incontinence [Citation8,Citation9]. The ratio of erectile function recovery after surgery was informed when the patient chose radical prostatectomy [Citation10].
A validated Japanese version of EPIC [Citation11] was sent by postal mail to patients’ homes ≤2–3 weeks before radical prostatectomy and completed questionnaires were returned in a postage-paid envelope. EPIC consists of four domains (urinary, bowel, sexual, and hormonal), including a question (number 22) on sexual activity during the preceding 4 weeks (Suppl. Table 1). The original questionnaire was conducted through self-reporting, and collected on the same day, when patients were first admitted to our hospital. Associations between sexual activity (as defined per both EPIC and our original questionnaire), risk factors for ED, and sexual function (as defined per EPIC) were analyzed retrospectively.
The survey was approved by the Ethical Committee of the University Hospital (#H120406) and conducted in accordance with the Declaration of Helsinki. Data are presented as mean ± standard deviation. Relations between sexual activity and risk factors for ED were assessed using univariate logistic regression analysis. Differences values were determined using an unpaired Mann–Whitney U-test and chi-square test. p < .05 was considered to be statistically significant.
Results
The mean age of the 145 enrolled patients was 67.7 ± 5.2 (range, 45–76) years. The distribution of the final tumor stage after complete histopathological processing was 3 with stage pT0, 20 with pT2a, 3 with pT2b, 90 with pT2c, 24 with pT3a, and 5 with pT3b. Unilateral nerve sparing was attempted in 66 patients and bilateral nerve sparing in only 1. No patients were taking phosphodiesterase type 5 (PDE5) inhibitors before treatment and only 1 used a PDE5 inhibitor after surgery, on-demand for penile rehabilitation. Sexual activity as reported via EPIC is shown in . 35 (24.1%) patients responded that they had some sexual activity within the preceding 4 weeks. No patients responded “several times a week” or “daily”. From the original questionnaire related to actual sexual activity, 73 of the 145 (50.3%) patients responded that they had some amount of sexual activity (). The ratio of patients who had sexual activity in patients with nerve sparing (52.2%; n = 35/67) and those without (48.7%; n = 38/78), as revealed through our original questionnaire, did not significantly differ (p = .67). Of these, 30 (20.7%) had a sexual activity rate of “at least once a month” and 43 (29.7%) “about once every 2 months to a year”. The effects of ED-related risk factors were determined (). Age was found to be the only significant predictor of sexual activity (p = .0036). In contrast, there was no significant difference in sexual activity rate among those in sexually active groups (). shows comparison between actual sexual activity from EPIC and our original questionnaire. Among the 73 patients who had actual sexual activity, 41 (56.1%) reported no sexual activity during the preceding 4 weeks. Irrespective of actual sexual activity rate, the sexual function measure of EPIC showed no significant differences among patients who had some sexual activity in the preceding 4 weeks (Suppl. Figure 1a). However, sexual function per EPIC was significantly lower among actual sexually active patients who reported no sexual activity within the preceding 4 weeks than among actual sexually active patients who reported some sexual activity in that same time frame (Suppl. Figure 1b).
Figure 1. (a) Sexual activity revealed from Expanded Prostate Cancer Index Composite (n = 145). (b) Actual sexual activity revealed from original questionnaire (n = 145).
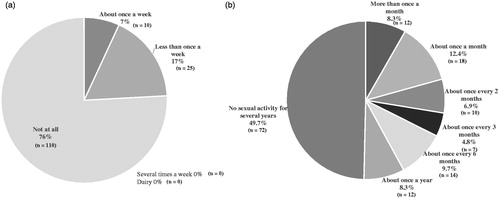
Table 2. (a) Determination of sexual activity by univariate logistic regression analysis.
(b) Determination of sexual activity rate among the patients who have actual sexual activity by univariate logistic regression analysis.
Table 3. Relation of numbers of patients regarding sexual activity comparing Expanded Prostate Cancer Index Composite (EPIC) questionnaire and original questionnaire before radical prostatectomy (total; n = 145).
Discussion
To precisely evaluate erectile function after radical prostatectomy, one of the most important factors is accurate evaluation of preoperative erectile function [Citation7]. Though there is agreement that objective use of a device would be the most precise means of evaluation [Citation12], the associated time and effort of such an approach make it difficult to routinely perform. Therefore, in many cases, erectile function before and after radical prostatectomy is evaluated subjectively via questionnaires, some of which are concerned with the presence/absence of sexual activity within a certain period (e.g. IIEF-15, EPIC).
About half of the middle-aged Japanese patients in the present study reported they were sexually active, but only 20.7% of the entire group reported engaging in sexual activity at least once a month (). From the Cologne Male Survey in Germany, Braun et al. reported 71% of 70–80 year olds actively engaged in sex; 41% on a weekly basis [Citation13]. Compared with findings from studies on Westerners, the ratio of sexual activity among middle-aged Japanese patients in the present study was low. Namiki et al., using the UCLA Prostate Cancer Index, revealed that Japanese men were more likely than American men to report infrequency of erections, and less likely to be bothered by sexual function [Citation14]. Masumori et al. surveyed Japanese and American men aged 49–79 years using a self-reported questionnaire and revealed that, though more Japanese than American men reported ED and decreased libido, there were no noteworthy differences in self-reported sexual satisfaction [Citation15]. These reports indicate that consideration of racial and cultural differences are necessary when evaluating erectile function; different cultures have different concepts of sexual function [Citation16]. They also suggest that the rate of sexual activity does not always reflect actual sexual function. In fact, no results of the EPIC sexual domain showed significant differences among sexually active patients (Suppl. Figure 1(a)). The questionnaires that inquire on sexual activity within a certain period of time are incapable of indicating exact sexual function, at least for middle-aged Japanese prostate cancer patients.
Comparison results related to the presence/absence of sexual activity showed that, in our original questionnaire, age was the only significant indicator for having sexual activity. Age is obviously a risk factor for ED [Citation17], yet among the sexually active patients, there were no significant differences in risk factors for ED between patients who had sexual activity “at least once a month” and “about once every 2 months to a year” (). This result would also seem to indicate that differences in sexual activity rate do not affect sexual function in middle-aged Japanese prostate cancer patients.
Sexual activity of pretreatment prostate cancer patients as per EPIC revealed that 24.1% of all men surveyed had sexual activity within the preceding 4 weeks (). This ratio was nearly the same as that for actual sexual activity assessed in our original questionnaire among those reporting sexual activity at least once a month (20.7%) (). Among sexually active patients, 41 (56.1%) responded they had no sexual activity during the preceding 4 weeks (). This result indicates that more than half of these patients underestimated their erectile function pretreatment.
The present study had several limitations. First, biological measurement was not sufficiently determined. Though the relationship of testosterone levels with sexual activity in middle-aged men is a debated topic [Citation18,Citation19], the value of serum testosterone would affect sexual function. Lunenfeld et al. recommended that patients with co-morbidities (obesity or type 2 diabetes mellitus, hyperprolactinemia, metabolic syndrome, bladder outlet obstruction, peripheral vascular disease, or taking medication) should be concerned with testosterone-deficiency-related erectile dysfunction [Citation20]. Second, the present survey made no inquiry regarding education, working status, or marital status. These demographic differences influence the choice of treatment option for localized prostate cancer, and influence baseline pretreatment sexual function [Citation21,Citation22]. Existence and cooperation of a partner are important factors behind sexual desire and motivation for prostatectomy patients [Citation23]. Third, the present analysis included only 40% of all potentially survey-eligible patients who underwent prostatectomy. In this retrospective study, we only analyzed patients who fully answered our original, EPIC questionnaire, and whose risk factors for ED could be collected. Though there is no commonly accepted standard for an acceptable participate rate, to be useful, the survey needs a high collection rate.
Results from the present survey suggest that evaluators consider the association or discrepancy between actual sexual activity and questionnaire results. There is the possibility of underestimation when evaluating sexual function using questionnaires concerning sexual activity within a certain period of time. At least for middle-aged Japanese prostate cancer patients, determining adaptation to nerve-sparing surgery should be considered not only from results indicating sexual function using a subjective questionnaire but also from sufficient objective assessment of sexual function, direct inquiry, and other factors. Further studies with accurate preoperative and postoperative evaluation of sexual function are needed.
Conclusions
In the present study, though about half of the surveyed middle-aged Japanese men with localized prostate cancer reported sexual activity, more than half reported no sexual activity within the preceding 4 weeks. To extrapolate an exact determination of sexual function pre- and post-treatment for prostate cancer, it is necessary to consider not only questionnaire responses and results, but also actual sexual activity.
Suppl.Table.eps
Download EPS Image (618.9 KB)Suppl._Fig.1.eps
Download EPS Image (651.7 KB)Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Shikanov SA, Zoen KC, Zagaja GP, et al. Trifecta outcomes after robotic-assisted laparoscopic prostatectomy. Urology. 2009;74:619–623.
- Vickers AJ. The trifecta: great concept, lousy statistic. BJU Int. 2012;110:771–772.
- Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326.
- Goldstein I, Lue TF, Padma-Nathan H, et al. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397–1404.
- Wei JT, Dunn RL, Litwin MS, et al. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905.
- Litwin MS, Hays RD, Fink A, et al. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002–1012.
- Mulhall JP. Defining and reporting erectile function outcomes after radical prostatectomy: challenges and misconceptions. J Urol. 2009;181:462–471.
- Reeves F, Preece P, Kapoor J, et al. Preservation of the neurovascular bundles is associated with improved time to continence after radical prostatectomy but not long-term continence rates: results of a systematic review and meta-analysis. Eur Urol. 2015;68:692–704.
- Steineck G, Bjartell A, Hugosson J, LAPPRO steering committee, et al. Degree of preservation of the neurovascular bundles during radical prostatectomy and urinary continence 1 year after surgery. Eur Urol. 2015;67:559–568.
- Capogrosso P, Salonia A, Briganti A, et al. Postprostatectomy erectile dysfunction: a review. World J Mens Health. 2016;34:73–88.
- Kakehi Y, Takegami M, Suzukamo Y, et al. Health related quality of life in Japanese men with localized prostate cancer treated with current multiple modalities assessed by a newly developed Japanese version of the Expanded Prostate Cancer Index Composite. J Urol. 2007;177:1856–1861.
- Taniguchi H, Kawa G, Kinoshita H, et al. Recovery of erectile function after nerve-sparing laparoscopic radical prostatectomy in Japanese patients undergoing both subjective and objective assessments. J Sex Med. 2012;9:1931–1936.
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the 'Cologne Male Survey'. Int J Impot Res. 2000;12:305–311.
- Namiki S, Kwan L, Kagawa-Singer M, et al. Sexual function reported by Japanese and American men. J Urol. 2008;179:245–249.
- Masumori N, Tsukamoto T, Kumamoto Y, et al. Decline of sexual function with age in Japanese men compared with American men-results of two community-based studies. Urology. 1999;54:335–344.
- Namiki S, Arai Y. Health-related quality of life in men with localized prostate cancer. Int J Urol. 2010;17:125–138.
- Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
- O’Connor DB, Lee DM, Corona G, European Male Ageing Study Group, et al. The relationships between sex hormones and sexual function in middle-aged and older European men. J Clin Endocrinol Metab. 2011;96:1577–1587.
- Cunningham GR, Stephens-Shields AJ, Rosen RC, et al. Association of sex hormones with sexual function, vitality, and physical function of symptomatic older men with low testosterone levels at baseline in the testosterone trials. J Clin Endocrinol Metab. 2015;100:1146–1155.
- Lunenfeld B, Mskhalaya G, Zitzmann M, et al. Recommendations on the diagnosis, treatment and monitoring of hypogonadism in men. Aging Male. 2015;18:5–15.
- Pearce SM, Wang CH, Victorson DE, et al. A longitudinal study of predictors of sexual dysfunction in men on active surveillance for prostate cancer. Sex Med. 2015;3:156–164.
- van den Bergh RC, Korfage IJ, Roobol MJ, et al. Sexual function with localized prostate cancer: active surveillance vs radical therapy. BJU Int. 2012;110:1032–1039.
- Sato Y, Tanda H, Nakajima H, et al. Dissociation between patients and their partners in expectations for sexual life after radical prostatectomy. Int J Urol. 2013;20:322–328.
