Abstract
A 65-year-old gentleman, with no past medical problems and not on any anticoagulation was seen in the urology clinic with persistent hematospermia for the last few years. A thorough history and examination including a digital examination of the prostate was unremarkable. Bleeding from his female partner was also ruled out. Investigations such as prostate specific antigen (PSA) blood test, urine culture, semen culture, and flexible cystoscopy were performed, and these investigations were also within normal limits. Due to his persistent hematospermia even after masturbation, a magnetic resonance imaging (MRI) of his pelvis was performed to rule out any sinister intrapelvic pathology. His MRI pelvis revealed a right seminal vesicle haemorrhage which was the cause of his hematospermia. He was treated conservatively with the advice to abstain from ejaculation for a few months. More importantly, we have also reassured the patient.
Case report
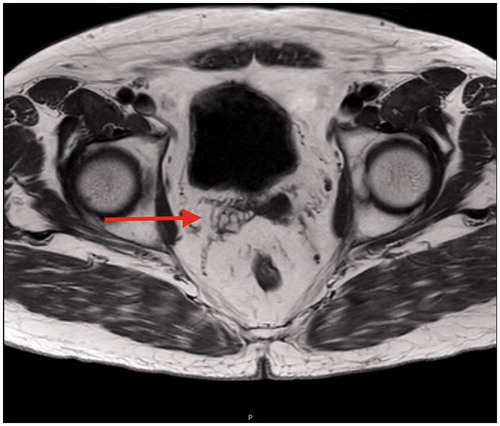
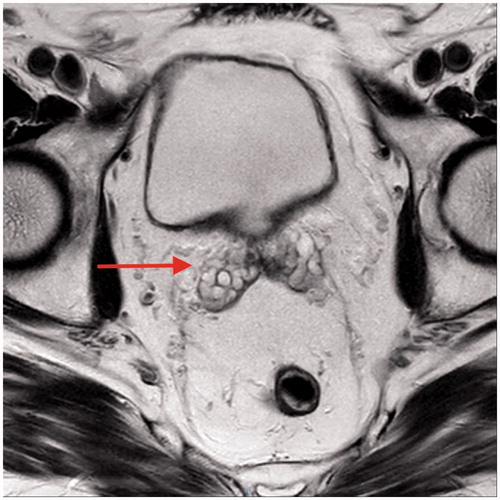
A 65-year-old gentleman, with no past medical problems and not on any anticoagulation was seen in the urology clinic with persistent hematospermia for the last few years. A thorough history and examination including a digital examination of the prostate was unremarkable. Bleeding from his female partner was also ruled out. Investigations such as prostate specific antigen (PSA) blood test, urine culture, semen culture, and flexible cystoscopy were performed, and these investigations were also within normal limits. Due to his persistent hematospermia even after masturbation, a magnetic resonance imaging (MRI) of his pelvis was performed to rule out any sinister intrapelvic pathology. His MRI pelvis revealed a right seminal vesicle haemorrhage which was the cause of his hematospermia ( and ). He was treated conservatively with the advice to abstain from ejaculation for a few months. More importantly, we have also reassured the patient.
Discussion
Hematospermia can be distressing and alarming for many sexually active male patients and their partners. It is reported that hematospermia make up about 1% of all urological symptoms [Citation1]. The two commonest causes of hematospermia are trauma – which could be secondary to prostate biopsy, cystoscopy, brachytherapy, and pelvic injury – and infections [Citation2,Citation3]. Other causes include malignancy of the male genitourinary system and seminal vesicle stones while other rare causes include severe arterial hypertension, bleeding diathesis, and liver cirrhosis. More often than not, no exact cause of hematospermia can be found. Therefore, it is pertinent to allay patients’ anxiety and reassure them [Citation3].
In Zhao et al. [Citation4] study of 270 patients who presented with haematospermia, eight patients (3.0%) were found to have urological malignancy, i.e. five prostate cancers, two seminal vesicle cancers, and one bladder cancer and these eight patients were more than 40 years old. Although hematospermia is a rare presentation for urological malignancy, it is an important diagnosis to rule out especially when prostate cancer is a very common urological malignancy among elderly men [Citation5]. One of the interesting findings in Zhao et al. study is they have found prostatic calcifications in 106 patients and seminal vesicle calcifications in 19 patients on transrectal ultrasound. Similarly, from an analysis of 298 specimens from radical prostatectomies or cystoprostatectomies, Suh et al. [Citation6] have found that calcifications in the prostate and ejaculatory system were also common features too. In their study, they found calcifications in 264 prostates (88.6%), 173 seminal vesicles (58.1%), and 51 ejaculatory ducts (17.1%). Although calcifications can occur in the areas of prostatic adenocarcinoma, they are often more associated with benign prostatic hyperplasia rather than malignancy.
Men under the age of 40 years old with a single episode of hematospermia are usually benign and self-limiting. A course of quinolone such as ciprofloxacin, or doxycycline, or in combination can be considered if a clinician suspects an infection even in the absence of a clear urine culture. However, in men who are above the age of 40 years old and have persistent hematospermia, a more aggressive investigation strategy is warranted to rule out any malignancy in the male genitourinary system. This includes a digital rectal examination, which is shown to be well-tolerated and accepted examination [Citation7], an urgent flexible cystoscopy, and an urgent MRI pelvis scan which is an excellent imaging modality to investigate persistent hematospermia [Citation8,Citation9].
In the context of our patient, his digital examination of prostate, PSA test, and flexible cystoscopy were normal. His MRI pelvis revealed a right seminal vesicle bleed. He was treated conservatively. Several months later after abstaining from ejaculation, his symptoms were resolved.
Learning point
Persistent hematospermia should warrant investigations.
MRI pelvis is an excellent imaging modality to investigate persistent hematospermia.
In sexually active patients, female partners as source of bleeding should always be ruled out.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Polito M, Giannubilo W, d’Anzeo G, et al. Hematospermia: diagnosis and treatment. Arch Ital Urol Androl. 2006;78:82–85.
- Mathers MJ, Degener S, Sperling H, et al. Hematospermia – a symptom with many possible causes. Deutsches Ärzteblatt Int. 2017;114:186–191.
- Kumar P, Kapoor S, Nargund V. Haematospermia – a systematic review. Ann R Coll Surg Engl. 2006;88:339–342.
- Zhao H, Luo J, Wang D, et al. The value of transrectal ultrasound in the diagnosis of hematospermia in a large cohort of patients. J Androl. 2012;33:897–903.
- Cepeda O, Gammack J. Cancer in older men: a gender-based review. Aging Male. 2006;9:149–158.
- Suh JH, Gardner JM, Kee KH, et al. Calcifications in prostate and ejaculatory system: a study on 298 consecutive whole mount sections of prostate from radical prostatectomy or cystoprostatectomy specimens. Ann Diagn Pathol. 2008;12:165–170.
- Naccarato AM, Reis LO, Matheus WE, et al. Barriers to prostate cancer screening: psychological aspects and descriptive variables – is there a correlation? Aging Male. 2011;14:66–71.
- Li BJ, Zhang C, Li K, et al. Clinical analysis of the characterization of magnetic resonance imaging in 102 cases of refractory haematospermia. Andrology 2013;1:948–956.
- Mittal PK, Camacho JC, Sahani DV, et al. Hematospermia evaluation at MR imaging. Radiographics. 2016;36:1373–1389.