ABSTRACT
This article aims to alert social work researchers and practitioners to the importance of engaging in research and debate about how to approach and understand ADHD among children in general and locked-after children in care in particular. Social work researchers have largely been absent from academic discussions about the ‘ADHD epidemic’ despite the fact that the prevalence of ADHD diagnosis and medication is very high in child welfare populations. The social work profession can make important contributions to understanding a phenomenon that is common among children and adolescent clients, that is often co-morbid with other conditions such as conduct disorder and that is linked to social adversity. We argue that research on ADHD in the child welfare systems should be a top priority in social work, and outline some important questions that need to be addressed by both researchers and social workers.
ABSTRAKT
Trots att förekomsten av ADHD-diagnoser och ADHD-medicin är mycket hög inom den sociala barnavården har forskare inom socialt arbete i stor utsträckning lyst med sin frånvaro i akademiska diskussioner kring ”ADHD-epidemin”. Denna artikel syftar till att uppmuntra forskare och praktiker inom socialt arbete att bidra till forskningen och debatten om hur vi ska förstå ADHD bland barn i allmänhet och samhällsplacerade barn i synnerhet. Socialt arbete som profession kan bidra med viktig förståelse av ett fenomen som är vanligt bland barn och ungdomar som är i kontakt med socialtjänsten, som ofta förekommer tillsammans med andra tillstånd och som är sammanlänkat med social utsatthet. Vi menar att forskning kring ADHD inom den sociala barnavården bör prioriteras högt och pekar på viktiga frågor som behöver adresseras av såväl forskare som praktiker.
KEYWORDS:
NYCKELORD:
Introduction
ADHD (Attention Deficit/Hyperactivity Disorder) is probably the fastest growing psychiatric diagnosis among young people in general and looked after children in particular. The core features of the condition are inattention, impulsiveness and hyperactivity (e.g. Singh, Citation2008). This article discusses the link between ADHD, social work research and social work practice with children and adolescents. When looking for research literature, we were surprised to learn that there are relatively few influential (e.g. highly cited) social work studies on ADHD. Our impression is that ADHD has not really been a major issue of concern for social work researchers. Instead, research is dominated by medicine, which can be seen as part of a process of medicalisation of social problems (Conrad & Bergey, Citation2014).
Our main message is simple: the social work profession should take an active part in discussions and research on how to approach and understand the phenomenon. The prevalence of ADHD is very high in child welfare populations as compared to the general youth population. We believe that this statistical fact is in itself sufficient to alert social work researchers to why they should engage more in this issue. The links between ADHD and other diagnoses such as conduct disorder and oppositional deficiency disorder is another case in point.
To substantiate our claims, we draw primarily on general social science research on ADHD and on social work research on ADHD and certain recent findings from our own research (Karlsson & Lundström, Citation2015; Lundström, Citation2016). There are important lessons to be learnt from research with a social science orientation. For example, ADHD diagnosis and medication are clearly linked to different forms of social adversity. As social work researchers we should not shy away from conducting research on ADHD despite processes of increasing medicalisation (Conrad & Bergey, Citation2014) and pharmaceuticalisation (Abraham, Citation2010) in this and adjacent fields. As we see it, the need for social research is immense precisely because of these processes. Reducing such a complex phenomenon as ADHD to an individual pathology caused by deficits in neurological functioning will hardly help the young clients in child welfare whose situations often are characterised by layers of layers of social adversity.
The article begins with a short presentation of how we have chosen the literature that underlies our claims in the article. Then follows a section where we outline research on the nature, diagnosis and treatment of ADHD. We devote considerable space to the challenges of setting diagnosis, the geographical pattering of the condition as well as social correlates of diagnosis and medication. Our main focus is on social work with children and youth with ADHD, but, as we see it, social work researchers should also view ADHD in its broader context, including rising prevalence rates, individualisation of complex social problems (Conrad, Citation1975) and the strong co-morbidity between ADHD and other conditions. Along the way, we highlight important research opportunities for social work researchers and conclude with some recommendations for further work. Our ambition with this article is to contribute to theoretical and methodological debates on ADHD from a social work and social science perspective, and to call attention to the need of more comparative research in this field.
Method
We searched for research on ADHD in social work and the social sciences, but also more broadly on ADHD in general. The search term ‘ADHD’, unsurprisingly, generated numerous hits on search engines such as Google scholar. As for the background text under the heading ‘Diagnosing ADHD’ and ‘ADHD treatment’ we have used well known, often cited texts on these topics. The same goes for ‘prevalence, trends and variations in ADHD diagnosis and medication’. As for ‘ADHD in the child welfare population’ we have carried out a search on Google Scholar and Social Services Abstracts (search terms: ‘ADHD’, ‘child’, ‘children’, ‘Child protection’, ‘medication’, ‘prevalence’ ‘child welfare’, ‘residential care’ and ‘out of home care’ in different combinations). We also inspected the references on the relatively few hits we found on ADHD in social work in general and in child protection in particular. The analysis of the Swedish situation for ADHD diagnosis and medication among young persons in general and in the child welfare population is built on data from the Swedish pharmaceutical register published by the Swedish National Board of Health and Welfare. The quality of the pharmaceutical register is generally regarded as of very high quality (Socialstyrelsen, Citation2014, Citation2018 see also Karlsson & Lundström, Citation2015; Lundström, Citation2016).
Diagnosing ADHD
Individuals are diagnosed with ADHD based on instruments measuring the different behavioural symptoms that characterise it, with an additional professional judgement. The two main instruments used are the American Psychiatric Association’s DSM (Diagnostic and Statistical Manual of Mental Disorders) and the WHO’s ICD (International Classification of Disorders). In DSM-V ADHD is defined as ‘a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development’ (American Psychiatric Association, Citation2013). ADHD emerged in DSM-II in 1968, but was then called ‘Hyperkinetic Reaction of Childhood’ (Epstein & Loren, Citation2013). DSM-III referred to it as ‘Attention Deficit Disorder (with and without hyperactivity)’ and the term ADHD emerged in the revised version of DSM-III (DSM-III-R). DSM-IV further developed the diagnosis into three subcategories: ‘predominantly Inattentive’, ‘predominantly Hyperactive-Impulsive’, and ‘Combined’. These are also used in DSM V (Epstein & Loren, Citation2013). As Taylor (Citation2009) observes, the emergence of ‘attention deficit’ in DSM terminology illustrates the idea (or ‘hope’ as he refers to it) that ‘the condition, which is behaviourally defined, can be reduced to a deficit in neuropsychological processes of attention’ (p. 129). While this view has received its share of criticism, it is clearly the dominant perspective on ADHD still.
ICD-10 is the most recent version of ICD used in practice, but ICD-11 was published in 2018 (though not in effect yet). ICD-10 refers to ‘hyperkinetic disorders’ instead of ADHD. Its defining features are ‘early onset; a combination of overactive, poorly modulated behaviour with marked inattention and lack of persistent task involvement; and pervasiveness over situations and persistence over time of these behavioural characteristics’ (WHO, Citation1992, p. 206). ICD is stricter in its requirements for setting diagnosis. A hyperkinetic disorder diagnosis is comparable to a severe form of the ‘combined’ subgroup in DSM and prevalence estimates have consequently been found to be higher when the DSM system is used (NICE, Citation2009).
There are no biological markers for ADHD and this inevitably brings an element of uncertainty when setting diagnosis. Symptoms of ADHD often overlap with symptoms of other diagnoses and the diagnostic challenges are exacerbated by the fact that ADHD is often co-morbid with psychiatric and other problems such as substance use disorders, conduct disorders and anxiety disorders (Yoshimasu et al., Citation2012). This co-morbidity can be expected to be particularly strong for child protection populations (cf. Klein, Damiani-Taraba, Koster, Cambpell, & Scholz, Citation2015). Richards (Citation2013) has in a manner that is of great importance for social work discussed the overlap between ADHD and conduct disorder and refers to a study showing that clinicians blind to the diagnostic status of children saw similar levels of psychosocial problems in children with ADHD and conduct disorder. Clinicians who knew the diagnostic status of the children, on the other hand, observed lower levels of these problems in ADHD. As she notes, ‘being told that a child had a diagnosis of ADHD made clinicians less likely to notice psychosocial issues and family factors impacting on that child and even to ask about physical abuse’ (Richards, Citation2013, p. 484; see also Howe, Citation2010; Singh, Citation2008).
We see a risk that social work practitioners, if informed that a child has ADHD, adopt an overly narrow view and thus overlook other adversities affecting his or her situation. Detailed evidence shows that when psychiatrists assess whether a child has ADHD, they filter out information that is not directly relevant for the diagnosis but which may be crucial for understanding the child’s behaviour (e.g. the context of the behaviour) (see Tegtmejer, Hjörne, & Säljö, Citation2017). Symptoms common in child welfare population may in some cases also be attributed to ADHD when in fact they may reflect other conditions (Howe, Citation2010; Klein et al., Citation2015). This issue is surely not only of academic interest; diagnoses with similar symptoms but with different aetiologies may require different treatments (Tegtmejer et al., Citation2017). If other causes for the symptoms are not considered, the symptoms may thus in part remain, even if e.g. ADHD medicine is prescribed (Klein et al., Citation2015). As Klein et al. (Citation2015) point out in a review, the diagnostic guidelines for ADHD are less suitable for children in child welfare whose problems often are multifactorial. Instead, they advocate ‘a more holistic approach to ADHD management’ in this group of children and youth, including a broader assessment of the children’s situation (Klein et al., Citation2015, p. 181).
ICD-10 explicitly acknowledges the diagnostic difficulties in separating ‘hyperkinetic disorder’ (i.e. ADHD) from conduct disorder, and how this should be dealt with: ‘The major problems in diagnosis lie in differentiation from conduct disorder: when its criteria are met, hyperkinetic disorder is diagnosed with priority over conduct disorder. However, milder degrees of overactivity and inattention are common in conduct disorder. When features of both hyperactivity and conduct disorder are present, and the hyperactivity is pervasive and severe, “hyperkinetic conduct disorder" … should be the diagnosis’ (WHO, Citation1992, pp. 207–208). ICD-10 also notes the diagnostic difficulties stemming from the fact that inattention and overactivity can be symptoms of anxiety or depressive disorders. In addition, reported symptoms of ADHD fluctuate on a day-to-day basis, which suggests that clinicians may have to make repeated assessments of an individual’s symptoms to set an accurate diagnosis (Schmid, Stadler, Dirk, Fiege, & Gawrilow, Citation2016). The question also arises as to whether ADHD actually exists as a distinct entity (categorical) or whether it is better understood as lying on a continuum (dimensional). Most studies suggest that it is best understood as dimensional (see Marcus, Norris, & Coccaro, Citation2012), but the diagnostic systems by design construct it as categorical: either people are diagnosed or not. However, where to set the cut-off point is surely not self-evident (Taylor, Citation2009).
We are not going to immerse ourselves in this discussion, but only remind readers of the fact that research has still not come up with instruments that can identify ADHD as a clear-cut (neuro) biological entity in individuals (Rose & Abi-Rached, Citation2013). Thus, diagnosis relies heavily on professional discretion and it is obvious that there is no clear-cut border between those with ADHD and those without. As illustrated below, such an ambiguous diagnosis is sensitive to system-related differences and to different professional cultures. This seems to be the case whether effects of differing school systems, healthcare or professional practice are considered.
Adhd treatment
Treatment options for ADHD consist of pharmacological (in particular methylphenidate) and psychosocial interventions. There is a general research consensus that methylphenidate has positive short-term effects on ADHD symptoms (e.g. SBU, Citation2013). That said, the long-term effects are more or less unknown (Craig, Davies, Schibuk, Weiss, & Hechtman, Citation2015). However, the quality of the available evidence regarding short-term effects has also been called into question. Storebø et al. (Citation2015) recently published a controversial Cochrane Review of 185 RCTs (covering about 12,000 individuals) in which they stressed that the primary studies included were of low quality: Storebø et al. criticised prior systematic reviews of methylphenidate for not following the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) or the Cochrane Handbook for Systematic Reviews of Interventions, both of which were developed to facilitate the transparency and quality of systematic reviews. The review evoked strong reactions. Banaschewski et al. (Citation2016) provide severe criticism regarding how studies were selected, how the clinical relevance of the findings was interpreted, and how risk of bias was assessed in the Storebø et al. review.
These controversies among researchers are of course of importance for professionals within the healthcare system, but also for social workers who meet clients during the diagnostic phase as well as during treatment. Moreover, and more importantly, it has been suggested that the diagnostic systems and treatments that are currently used may not be suitable for children in child protection whose symptoms may also be reflective of maltreatment (Klein et al., Citation2015). Some ‘ADHD-like symptoms’ may be consequences of maltreatment, so relying solely on ADHD treatment options may then be an overly narrow approach to complex problems (Klein et al., Citation2015).
The effects of different kinds of psychosocial interventions, on their own or in combination with medical treatment, are not as well researched as pharmacological treatment, but studies tend to show a lack of evidence (SBU, Citation2013). However, some researchers have a lot of confidence in the combination of different forms of treatment, especially taking into consideration the fact that ADHD often appear in combination with other problems or diagnoses (see Howe, Citation2010) Our aim in this article is not to discuss the evidence of treatment effects; however, it may be worth noting that in some respect research on psychosocial interventions can be described as ‘absence of evidence’ rather than ‘evidence of absence’ – especially when comparing with the abundance of research on pharmacological treatment. There is, however, some evidence to suggest that social workers prefer psychosocial interventions to medication for the treatment of children with ADHD (Pentecost & Wood, Citation2002).
Social work researchers have an important role to play in determining how to tailor the interventions to the needs of children and adolescents with ADHD in child protection where ADHD often is only one of many difficulties facing these individuals. As Adams, Matto, and LeCroy (Citation2009) discusses in an article on evidence-based practice and social work, the individualistic focus characteristic of medical practice may not be particularly appropriate in practical social work with disadvantaged groups. They take ADHD as an example, where the social workers’ role is much broader than that of treating the condition as such. While social work typically views social problems as embedded in different systems (families, etc) the social worker also has to consider, for example, parenting practices and resources in the family (Adams et al., Citation2009; Howe, Citation2010). Disconnecting the ADHD diagnosed child from the influence on such systems and focusing solely on providing medication would be an overly simplistic solution to this complex phenomenon (cf. Richards, Citation2013; Howe, Citation2010).
Prevalence, trends and variations in ADHD diagnosis and medication
A dramatic increase in ADHD diagnosis and medication has been noted worldwide, but there are considerable variations both within and between countries. Generally, epidemiologists do not attribute this variability to actual differences across countries. It is instead seen as being due to factors such as the use of different types of diagnostic instruments and to different ways of defining the same kind of psychiatric problem (Polanczyk, Willcutt, Salum, Kieling, & Rohde, Citation2014).
The United States is often mentioned as a country with high rates of diagnosed children and adolescents. Estimates suggest that 11 per cent in the 4–17 age group have been diagnosed with ADHD, and in some states the figures are close to 15 per cent (Visser et al., Citation2014). A recent meta-analysis on the prevalence of ADHD in children (18 or under) used 7.2 per cent as a sort of benchmark; higher numbers allegedly indicate over-diagnosis whereas lower suggest under-diagnosis (Thomas, Sanders, Doust, Beller, & Glasziou, Citation2015).
The prevalence rates of ADHD medication are lower than the prevalence rates of diagnosis. For instance, in the US, roughly 6 per cent of adolescents aged 10–17 are on medication (Visser et al., Citation2014) and the corresponding figure in Sweden is around 4 per cent (Socialstyrelsen, Citation2018). However, there is a clear upward trend also for the prevalence of ADHD medicine use in Sweden. presents temporal trends regarding the use of ADHD medicine in Swedish boys and girls (aged 10–19) between 2006 and 2015. These figures are based on official aggregated data from the Swedish pharmaceutical register. As increases in ADHD medicine use might reflect overall increases in psychotropic use, we have also included the temporal trends for the use of antidepressants for comparative purposes.
Figure 1. Trends in the use of ADHD medicine and antidepressants in Swedish boys and girls (aged 10–19) between 2006 and 2015. Source: Socialstyrelsens statistikdatabas (http://www.socialstyrelsen.se/statistik/statistikdatabas, accessed 24-08-2017).
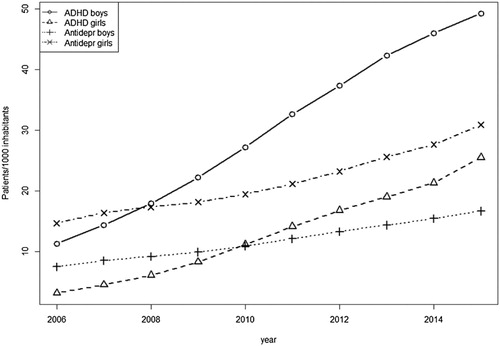
The figures are worth commenting. At the start of the period covered, the highest prevalence rates relatively speaking were found in the use of antidepressants in females, followed by ADHD medicine in males. The lowest figure pertains to ADHD medicine in girls. While the prevalence rates of ADHD medicine are substantially lower in females compared to males throughout the period, the percentage change from 2006 to 2015 is greatest in female ADHD medicine use. For both genders, the percentage increase in ADHD medicine is much greater than the increase in antidepressants. The relative changes over the years covered are 335 per cent for male ADHD medicine, 633 per cent for female ADHD medicine, and 121 and 110 per cent for male and female antidepressant use respectively. This rather steep increase in ADHD medicine use is in no way unique for Sweden. For example, the UK witnessed a more than 30-fold increase in ADHD medicine prescriptions for children between 1995 and 2013, and an 8-fold increase in incidence, although the trends plateaued after 2008 (Beau-Lejdstrom, Douglas, Evans, & Smeeth, Citation2016).
The prevalence of ADHD diagnosis and medicine does not only vary over time and across population groups but also across geographical areas. In a recent study, we found evidence of a clear spatial patterning regarding prescription rates for methylphenidate in Swedish youth in Swedish municipalities, and the municipalities’ regional affiliation were a strong predictor of prescription rates (Karlsson & Lundström, Citation2015).
A number of factors have been proposed to account for regional and local variations in the prevalence of ADHD diagnosis and numbers on medication. American researchers have pointed at different state-level incentives directed at the school system as a possible explanation for between-state differences (Hinshaw & Scheffler, Citation2014). Danish, Norwegian and Swedish researchers have pointed at large regional differences and have attributed this in part to variations in ‘diagnostic practice’ within the healthcare system (Surén et al., Citation2013). However, not only professional practices may drive such spatial differences. Socio-demographics probably also play a role in accounting for regional and local variations regarding ADHD. Research has continuously shown that those who are in a more disadvantaged situation are more likely to be diagnosed or to receive medicine. Social adversity, measured, for example, as being on social welfare, is clearly linked to ADHD in young people (Björkenstam, Björkenstam, Jablonska, & Kosidou, Citation2018; Hjern, Weitoft, & Lindblad, Citation2010).
The research community should pay considerable attention to delineating the potential reasons for the patterning of ADHD diagnosis and medication within and between countries. Given the focus of this paper, such research would be particularly salient when it comes to child welfare populations. Children with ADHD are more likely to be removed from their home environment compared to children with other types of psychiatric diagnoses (Foreman, Foreman, & Minty, Citation2005), and individuals with ADHD are more likely to have been abused or maltreated (Briscoe-Smith & Hinshaw, Citation2006; Fuller-Thomson, Mehta, & Valeo, Citation2014; Ouyang, Fang, Mercy, Perou, & Grosse, Citation2008). Drawing on Canadian data, Fuller-Thomson et al. (Citation2014) report that individuals, who as adults have reported that they were abused during childhood, had a seven-fold higher odds of reporting having ADHD or ADD in models adjusting for several control variables.
When trying to make sense of such patterns, researchers need, on the one hand, to distinguish between explanations that focus on why ADHD is more common in certain social groups than in others (e.g. in lower SES groups and in child welfare populations) and, on the other, why there also seem to be variations in prevalence rates in child welfare populations across national, regional and local contexts. A systematic review of ADHD among looked after children (Willis, Dhakras, & Cortese, Citation2017) suggests a quite dramatic difference in the prevalence estimates across countries. France stands out as a country with comparably low rates of ADHD diagnoses in looked after children, with an estimated 3.8 per cent prevalence of ADHD diagnosis. According to Willis et al. (Citation2017), the low prevalence rates in France could thus be due to the traditionally strong influence of psychodynamic views in the child psychiatry profession compared to countries with other dominant views.
Are these spatial, professional and system related variations in diagnostics and medication of any importance for social workers? We think they are. Social workers in high-level regions are probably more often in contact with children with a diagnosis and/or on medication. Furthermore, social workers are also active in, for example, schools, healthcare and child protection services that stand out as strongly associated with system-related differences. What kind of research and practice-oriented questions this raises is discussed further below.
Adhd in the child welfare population
Data on ADHD in child welfare populations is scarce. Yet, as might be expected, the data available demonstrate a huge over-representation compared to the general population. Studies from the United States and Canada report prescription rates exceeding 50 per cent for ADHD and other types of psychoactive drugs for children in residential care (Breland-Noble et al., Citation2004; Brenner, Southerland, Burns, Wagner, & Farmer, Citation2014; Klein et al., Citation2015; Leslie et al., Citation2011; Rubin et al., Citation2012). However, the prevalence rates of ADHD diagnosis and medication in looked after children vary appreciably across studies, and it should be noted that most data are from the United States (Willis et al., Citation2017).
presents prevalence rates of ADHD diagnosis and medication for Swedish children between the ages of 13 and 17 who have been placed in residential or foster care, including also the general population in the same age group. It is obvious that there is a huge overrepresentation of children in out of home care both when it comes to diagnosis and medication when compared to Swedish children in general. For example, if comparing ‘Swedish children’ with ‘children in foster care’, there are 5.5 times more common for boys and 6.1 more common for girls in foster care to be on ADHD medication. For children in secure units where young people with serious behavioural problems (i.e. conduct disorder), including drugs and crime, are placed, close to 50 per cent have been diagnosed and about one third are on medication. This includes both boys and girls.
Table 1. Medication (methylphenidate) and ADHD diagnosis in Swedish children, children in foster care and residential care (age: 13–17). Per cent. Source: Socialstyrelsen (Citation2014).
These data show that there is a strong correlation between living in foster care or in residential care and ADHD diagnosis/medication. Unfortunately, we have no information about the temporal order between type of placement and ADHD diagnosis and medication, which prevents any causal inferences to be made. In all likelihood, individuals with ADHD (particularly given its co-morbidity with typical child welfare problems such as conduct disorder) are more likely to be selected into, for example, placement, but it is also conceivable that a fair number of these adolescents were diagnosed once placed in care.
To understand the high prevalence of ADHD diagnosis and medicine among children in residential care, social work research should also look at the potential of ADHD symptoms being ‘transmitted’ between young people. For example, a well-established finding is that ‘troubled youth’ placed together learn problematic behaviours from each other, a phenomenon usually referred to as ‘deviancy training’ or ‘peer influence’ (Dodge, Dishion, & Lansford, Citation2006) and which might be conceivable also when it comes to ADHD-symptoms. ADHD-symptoms – or an intensification in these – may potentially also emerge as a negative reaction towards the care environment among children placed in e.g. residential care (cf. the idea that ADHD-like symptoms may be a reaction to one’s situation).
Based on the Swedish data available, we are not able to count the number of children/adolescents with an ADHD diagnosis or the numbers on medication who are included in different types of open care programmes or the ones under investigation for child protection issues. A fair guess is that those with an ADHD diagnosis are over-represented compared to the general population, but not as much as the ones in out of home care. This suggestion is reinforced by the fact that children in single-parent families and children from families on social welfare are over-represented when it comes to ADHD diagnosis (Hjern et al., Citation2010).
Singh (Citation2008) with reference to Jensen et al. (Citation2001) estimates that only 31% of those with ADHD have this disorder alone. Much more common are combinations with especially oppositional defiant disorder, conduct disorder and anxiety disorder. A fair guess is that it is even more uncommon with ADHD alone in the child welfare population and that combinations with especially oppositional disorders and conduct disorder are much more common in this population (reminding that the definitions of these disorders are far from clear-cut). In any case, based on the large numbers of children with a diagnosis in out of home care, we can conclude that ADHD is an issue for social work research and practice, especially in the area of child protection.
Conclusions and future orientations
ADHD diagnosis and the use of medication for ADHD has grown very fast worldwide. As we have shown, the relative growth in methylphenidate use in Sweden was over 300 per cent for boys and more than 600 per cent for girls from 2006 to 2015. Similar developments have been observed for other countries. Besides this large upward trend, the prevalence rates of ADHD diagnosis and use of medication are highly elevated in child welfare populations. Being in care may be one of the strongest correlates of ADHD; children in foster care and residential care are extremely over-represented for ADHD when compared to the general population. This inevitably leads to questions on how we handle the borders of normality in relation to sickness but also on the demarcation between different psychiatric diagnoses prevalent in child welfare populations (e.g. ADHD vs. conduct disorder). Should we be concerned when 10 per cent of the boys in some municipalities or 30–50 per cent in certain residential care settings are on ADHD medication?
As we have shown, variations in diagnosis seem to be linked to system-related and socio-economic factors as well differing professional logics. This leads us to the conclusion that there is an urgent need for empirical as well as theory-driven social science research in this particular field. In addition, the fact that young people in out of home care are heavily overrepresented as regards both diagnosis and medication for ADHD leads us to the conclusion that research on ADHD in the child welfare system should be a top priority in social work. This includes, but is not limited to:
Studies on the prevalence of children with ADHD diagnosis within child protection as a whole (not only in out of home care). These studies should preferably also address geographical patterns in ADHD diagnosis and medicine in child protection within and between countries.
Longitudinal studies tracking temporal trends in ADHD in child protection over time. Such studies could assess potential spill over effects from overall trends in ADHD in the general population to trends in child protection.
Research on the way issues regarding ADHD are handled in different care settings (child welfare agencies and residential care units). This may also include international comparative studies.
Studies on what medical treatment entails for the care situation. How is medication handled in day-to-day care? What impact does medication and diagnosis have on peer relationships in residential care, where some adolescents are on medication and others not?
What role do social workers play when it comes to initiating diagnosis and medication? How do they collaborate with other professions in this respect? How does the interaction between healthcare, schools and child protection but also parents and client organisations work in the setting of a diagnosis? In-depth case studies should be able to address these issues.
In what way is it possible to use an ADHD diagnosis in parents and/or children in decisions on coercive measures within the child protection system?
Willis et al. (Citation2017, p. 83) suggest that ‘rather than assessing if ADHD is over or under diagnosed and treated in LAC [Looking after Children], future research should aim to understand to which extent ADHD is appropriately diagnosed and treated in LAC’. We would like to widen this question to include comparative research on the mechanisms driving differences between and within nations regarding ADHD diagnosis for child protection. To what extent are these differences related to, for example, variations in the child protection population and differences in the child protection itself and related systems? This includes the importance of differences in professional ideology and practice.
ADHD also poses significant questions for social workers, whether they work in schools, healthcare or child protection. Questions include ethical concerns, for example, how to take into account and weigh the different interests of actors involved (adolescents, parents, schools, foster families and residential care staff)? Howe (Citation2010) argues convincingly about the importance of understanding ADHD in its context, not only as a medical condition. As for treatment, he ends up with the conclusion that psychosocially based interventions are still of great importance for social workers when working with clients diagnosed with ADHD. However, as emphasised in this article, there are no clear-cut borders for ADHD diagnosis and its conceptualisations differ widely. This will probably make this a field of controversies for a long time to come (Conrad & Bergey, Citation2014; Singh, Citation2008).
Social workers in child protection should be updated on research and research debate in this area. This includes issues regarding diagnostic criteria, the partly contradictory evidence base regarding both short and long-term treatment effects of pharmacological and other treatments, the debates on how to explain the phenomenon and the fact that numbers of diagnosed vary by different system related factors. To put it simple, social workers needs knowledge enough to question individual diagnosis as well as the numbers of diagnosed, but also knowledge on effects of different treatment options.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Patrik Karlsson
Patrik Karlsson, associate professor, works as a senior lecturer at the Department of Social Work, Stockholm University. His main research area is alcohol and illicit drug use in youth. Another research interest concerns evidence-based practice.
Tommy Lundström
Tommy Lundström is a professor of Social Work at Stockholm University. His research areas are social work with children and youth, and the organisation of social services in social work. He has also been doing research on the voluntary sector and voluntary social work.
References
- Abraham, J. (2010). Pharmaceuticalization of society in context: Theoretical, empirical and health dimensions. Sociology, 44(4), 603–622. doi: https://doi.org/10.1177/0038038510369368
- Adams, K. B., Matto, H. C., & LeCroy, C. W. (2009). Limitations of evidence-based practice for social work education: Unpacking the complexity. Journal of Social Work Education, 45(2), 165–186. doi: https://doi.org/10.5175/JSWE.2009.200700105
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
- Banaschewski, T., Buitelaar, J., Chui, C. S., Coghill, D., Cortese, S., Simonoff, E., & Wong, I. C. (2016). Methylphenidate for ADHD in children and adolescents: Throwing the baby out with the bathwater. Evidence-Based Mental Health, 19(4), 97–99. doi: https://doi.org/10.1136/eb-2016-102461
- Beau-Lejdstrom, R., Douglas, I., Evans, S. J., & Smeeth, L. (2016). Latest trends in ADHD drug prescribing patterns in children in the UK: Prevalence, incidence and persistence. BMJ Open, 6(6), e010508. doi: https://doi.org/10.1136/bmjopen-2015-010508
- Björkenstam, E., Björkenstam, C., Jablonska, B., & Kosidou, K. (2018). Cumulative exposure to childhood adversity, and treated attention deficit/hyperactivity disorder: A cohort study of 543 650 adolescents and young adults in Sweden. Psychological Medicine, 48(3), 498–507. doi: https://doi.org/10.1017/S0033291717001933
- Breland-Noble, A. M., Elbogen, E. B., Farmer, E. M., Dubs, M. S., Wagner, H. R., & Burns, B. J. (2004). Use of psychotropic medications by youths in therapeutic foster care and group homes. Psychiatric Services, 55(6), 706–708. doi: https://doi.org/10.1176/appi.ps.55.6.706
- Brenner, S. L., Southerland, D. G., Burns, B. J., Wagner, H. R., & Farmer, E. M. (2014). Use of psychotropic medications among youth in treatment foster care. Journal of Child and Family Studies, 23(4), 666–674. doi: https://doi.org/10.1007/s10826-013-9882-3
- Briscoe-Smith, A. M., & Hinshaw, S. P. (2006). Linkages between child abuse and attention-deficit/hyperactivity disorder in girls: Behavioral and social correlates. Child Abuse & Neglect, 30(11), 1239–1255. doi: https://doi.org/10.1016/j.chiabu.2006.04.008
- Conrad, P. (1975). The discovery of hyperkinesis: Notes on the medicalization of deviant behavior. Social Problems, 23(1), 12–21. doi: https://doi.org/10.2307/799624
- Conrad, P., & Bergey, M. (2014). The impending globalization of ADHD: Notes on the expansion and growth of a medicalized disorder. Social Science & Medicine, 122, 31–43. doi: https://doi.org/10.1016/j.socscimed.2014.10.019
- Craig, S. G., Davies, G., Schibuk, L., Weiss, M. D., & Hechtman, L. (2015). Long-term effects of stimulant treatment for ADHD: What can we tell our patients? Current Developmental Disorders Reports, 2(1), 1–9. doi: https://doi.org/10.1007/s40474-015-0039-5
- Dodge, K. A., Dishion, T. J., & Lansford, J. E. (Eds). Deviant peer influences in programs for youth: Problems and solutions. New York: Guilford Press.
- Epstein, J. N., & Loren, R. E. (2013). Changes in the definition of ADHD in DSM-5: Subtle but important. Neuropsychiatry, 3(5), 455–458. doi: https://doi.org/10.2217/npy.13.59
- Foreman, D. M., Foreman, D., & Minty, E. B. (2005). The association between hyperkinesis and breakdown of parenting in clinic populations. Archives of Disease in Childhood, 90, 245–248. doi: https://doi.org/10.1136/adc.2003.039826
- Fuller-Thomson, E., Mehta, R., & Valeo, A. (2014). Establishing a link between attention deficit disorder/attention deficit hyperactivity disorder and childhood physical abuse. Journal of Aggression, Maltreatment & Trauma, 23(2), 188–198. doi: https://doi.org/10.1080/10926771.2014.873510
- Hinshaw, S. P., & Scheffler, R. M. (2014). The ADHD Explosion: Myths, medication, money, and today's push for performance. New York: Oxford University Press.
- Hjern, A., Weitoft, G. R., & Lindblad, F. (2010). Social adversity predicts ADHD-medication in school children–a national cohort study. Acta Paediatrica, 99(6), 920–924. doi: https://doi.org/10.1111/j.1651-2227.2009.01638.x
- Howe, D. (2010). Adhd and its comorbidity: An example of gene–environment interaction and its implications for child and family social work. Child & Family Social Work, 15(3), 265–275. doi: https://doi.org/10.1111/j.1365-2206.2009.00666.x
- Jensen, P. S., Hinshaw, S. P., Swanson, J. M., Greenhill, L. L., Keith Conners, C., Eugene Arnold, L., … Wigal, T. (2001). Findings from the NIMH multimodal treatment study (MTA): Implications and applications for primary care providers. Journal of Developmental and Behavioral Pediatrics, 22, 60–73.
- Karlsson, P., & Lundström, T. (2015). Adhd på kartan: om geografiska skillnader i medicinering till barn och unga. Socialmedicinsk Tidskrift, 92(5), 553–565.
- Klein, B., Damiani-Taraba, G., Koster, A., Cambpell, J., & Scholz, C. (2015). Diagnosing attention-deficit hyperactivity disorder (ADHD) in children involved with child protection services: Are current diagnostic guidelines acceptable for vulnerable populations? Child Care, Health Development, 41(2), 178–85. doi: https://doi.org/10.1111/cch.12168
- Leslie, L. K., Raghavan, R., Hurley, M., Zhang, J., Landsverk, J., & Aarons, G. (2011). Investigating geographic variation in use of psychotropic medications among youth in child welfare. Child Abuse & Neglect, 35(5), 333–342. doi: https://doi.org/10.1016/j.chiabu.2011.01.012
- Lundström, T. (2016). Adhd; Om förekomst, ökning och konsekvenserna för social barnavård. Socionomens forskningssupplement. Socionomen, 1, 18–31.
- Marcus, D. K., Norris, A. L., & Coccaro, E. F. (2012). The latent structure of attention deficit/hyperactivity disorder in an adult sample. Journal of Psychiatric Research, 46(6), 782–789. doi: https://doi.org/10.1016/j.jpsychires.2012.03.010
- NICE. (2009). Attention deficit hyperactivity disorder. Diagnosis and management of ADHD in children, young people and adults.
- Ouyang, L., Fang, X., Mercy, J., Perou, R., & Grosse, S. D. (2008). Attention-deficit/hyperactivity disorder symptoms and child maltreatment: A population-based study. The Journal of Pediatrics, 153(6), 851–856. doi: https://doi.org/10.1016/j.jpeds.2008.06.002
- Pentecost, D., & Wood, N. (2002). Knowledge and perceptions of child-care social workers about ADHD. The British Journal of Social Work, 32(7), 931–943. doi: https://doi.org/10.1093/bjsw/32.7.931
- Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., & Rohde, L. A. (2014). Adhd prevalence estimates across three decades: An updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43(2), 434–442. doi: https://doi.org/10.1093/ije/dyt261
- Richards, L. M. E. (2013). It is time for a more integrated bio-psycho-social approach to ADHD. Clinical Child Psychology and Psychiatry, 18(4), 483–503. doi: https://doi.org/10.1177/1359104512458228
- Rose, N. S., & Abi-Rached, J. M. (2013). Neuro: The new brain sciences and the management of the mind. Princeton: Princeton University Press.
- Rubin, D., Matone, M., Huang, Y., DosReis, S., Feudtner, C., & Localio, R. (2012). Interstate variation in trends of psychotropic medication use among Medicaid-enrolled children in foster care. Children and Youth Services Review, 34, 1492–1499. doi: https://doi.org/10.1016/j.childyouth.2012.04.006
- SBU. (2013). Adhd Diagnostik och behandling, vårdens organisation och patientens delaktighet En systematisk litteraturöversikt. [ADHD: Diagnosis and treatment, the organising of care and patient particiaption. A systematic overview]. Stockholm: SBU.
- Schmid, J., Stadler, G., Dirk, J., Fiege, C., & Gawrilow, C. (2016). Adhd Symptoms in adolescents’ Everyday Life: Fluctuations and Symptom Structure within and between individuals. Journal of Attention Disorders. doi: https://doi.org/10.1177/1087054716629214
- Singh, I. (2008). Beyond polemics: Science and ethics of ADHD. Nature Reviews Neuroscience, 9(12), 957–964. doi: https://doi.org/10.1038/nrn2514
- Socialstyrelsen. (2014). Förskrivning av psykofarmaka till placerade barn och ungdomar [Prescipition of psychotropic drugs to children in care]. Stockholm: Socialstyrelsen.
- Socialstyrelsen. (2018). Fortsatt ökad användning av adhd-läkemedel 2017. Stockholm: Socialstyrelsen.
- Storebø, O. J., Ramstad, E., Krogh, H. B., Nilausen, T. D., Skoog, M., Holmskov, M., … Gillies, D. (2015). Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). Cochrane Database of Systematic Reviews, 11.
- Surén, P., Bakken, I. J., Lie, K. K., Schjølberg, S., Aase, H., Reichborn-Kjennerud, T., … Stoltenberg, C. (2013). Differences across counties in the registered prevalence of autism, ADHD, epilepsy and cerebral palsy in Norway. Tidsskrift for Den Norske Legeforening, 133, 1929–1934. doi: https://doi.org/10.4045/tidsskr.13.0050
- Taylor, E. (2009). Developing Adhd. Journal of Child Psychology and Psychiatry, 50(1-2), 126–132. doi: https://doi.org/10.1111/j.1469-7610.2008.01999.x
- Tegtmejer, T., Hjörne, E., & Säljö, R. (2017). Diagnosing ADHD in Danish primary school children: A case study of the institutional categorization om emotional and behavioural difficulties. Emotional and Behavioural Difficulties, 23(2), 127–140.
- Thomas, R., Sanders, S., Doust, J., Beller, E., & Glasziou, P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994–e1001. doi: https://doi.org/10.1542/peds.2014-3482
- Visser, S. N., Danielson, M. L., Bitsko, R. H., Holbrook, J. R., Kogan, M. D., Ghandour, R. M., … Blumberg, S. J. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry, 53 (1), 34–46. doi: https://doi.org/10.1016/j.jaac.2013.09.001
- WHO. (1992). The ICD-10. Classification of mental and behavioural disorders. Geneva: World Health Organization.
- Willis, R., Dhakras, S., & Cortese, S. (2017). - Attention-deficit/hyperactivity disorder in looked-after children: A systematic review of the literature. Current Developmental Disorders Reports, 4(3), 78–84. doi: https://doi.org/10.1007/s40474-017-0116-z
- Yoshimasu, K., Barbaresi, W. J., Colligan, R. C., Voigt, R. G., Killian, J. M., Weaver, A. L., & Katusic, S. K. (2012). Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: A population-based birth cohort study. Journal of Child Psychology and Psychiatry, 53(10), 1036–1043. doi: https://doi.org/10.1111/j.1469-7610.2012.02567.x
