Abstract
Objective: To provide an estimate of the annual number of super-refractory status epilepticus (SRSE) cases in the US and to evaluate utilization of hospital resources by these patients.
Methods: The Premier Hospital Database was utilized to estimate the number of SRSE cases based on hospital discharges during 2012. Discharges were classified as SRSE cases based on an algorithm using seizure-related International Classification of Diseases-9 (ICD-9) codes, Intensive Care Unit (ICU) length of stay (LOS), and treatment protocols (e.g. benzodiazepines, anti-epileptic drugs (AEDs), and ventilator use). Secondary analyses were conducted using more restrictive algorithms for SRSE.
Results: A total of 6,325 hospital discharges were classified as SRSE cases from a total of 5,300,000 hospital discharges. Applying a weighting based on hospital characteristics and 2012 US demographics, this projected to an estimated 41,156 cases of SRSE in the US during 2012, an estimated incidence rate of ∼13/100,000 annually for SRSE in the US. Secondary analyses using stricter SRSE algorithms resulted in estimated incidence rates of ∼11/100,000 and 8/100,000 annually. The mean LOS for SRSE hospitalizations was 16.5 days (median =11; interquartile range [IQR] = 6–20), and the mean ICU LOS was 9.3 days (median =6; IQR =3–12). The mean cost of an SRSE hospitalization was $51,247 (median = $33,294; 95% CI = $49,634–$52,861).
Limitations: The analysis uses ICD-9 diagnostic codes and claims information, and there are inherent limitations in any methodology based on treatment protocol, which created challenges in distinguishing with complete accuracy between SRSE, RSE, and SE on the basis of care patterns in the database.
Conclusion: SRSE is associated with high mortality and morbidity, which place a high burden on healthcare resources. Projections based upon the findings of this study suggest an estimated 25,821–41,959 cases of SRSE may occur in the US each year, but more in-depth studies are required.
Introduction
Status epilepticus (SE) is an acute neurological medical emergency associated, in its more severe forms, with significant mortality and morbidity. SE is defined as a seizure lasting more than 5 min or recurrent seizure activity without recovery (returning to baseline) between seizuresCitation1–4. Primarily treated in the Intensive Care Unit (ICU), refractory SE (RSE) is defined as seizures that continue despite the administration of an initial benzodiazepine, followed by a second-line intravenous (IV) anti-epileptic drug (AED), such as phenytoin, fosphenytoin, levetiracetam, or valproateCitation4,Citation5. SE that persists for 24 h or more following onset of therapy with third-line agents (e.g. propofol, high-dose midazolam, barbiturates) or after the reduction or withdrawal of third-line agents is defined as super-refractory SE (SRSE)Citation6.
The patient population is highly heterogeneous. SRSE may develop de novo, as a result of medication non-compliance, tumors, substance abuse/overdose, or following severe brain insult, such as infection, trauma, stroke, or autoimmune-mediated inflammationCitation6–10.
While there are guidelines for the evaluation and management of SECitation4, the lack of randomized or controlled clinical trials has hindered the development of definitive guidelines for the treatment of SRSECitation11,Citation12. In addition to anesthetics and AEDs, there is a wide range of adjunctive treatments used to manage SRSE in the ICU. These include ketamine, mild hypothermia, ketogenic diet, pyridoxine infusions (pediatrics), magnesium sulfate infusions, immunotherapy (including steroids), and stiripentolCitation6,Citation7,Citation12–16.
Previous reports estimate that SE affects from 12.5–61 people per 100,000 per year in the US, suggesting that the annual number of SE cases in the US could be between 40,345–132,322Citation1,Citation3,Citation17–21. Few studies have examined the incidence for RSE and SRSE, and most of the studies that exist have been focused on small populations in countries outside the USCitation9,Citation10,Citation22–25. Two US studies showed that 31–44% of patients with SE progressed to RSECitation25,Citation26. Shorvon and Ferlisi.Citation12 estimated that ∼10–15% of SE cases become SRSE cases. Several recent attempts have been made to study the incidence of SRSE, with estimations ranging from 5–17% of SE cases becoming SRSE cases in small patient populations outside the USCitation9,Citation10,Citation22. There is still a need for more comprehensive analysis of the incidence of SE, RSE, and SRSE in the US population. There is also little data regarding the healthcare resource utilization of SRSE patients or the economic burden of SRSE hospitalizations. The objectives of this study were to estimate the annual incidence of SRSE cases in the US during 2012 and to assess associated costs and resource utilization for SRSE patients.
Subjects/materials and methods
Study design
This was a cross-sectional study to identify and characterize hospital discharges of SRSE patients during 2012.
Data source
This study used the Premier Hospital Database (referred to as Premier Database). The Premier Database (Premier Healthcare Alliance, Charlotte, NC) is a large US hospital, service-level, all-payer, comparative database that represents real-world US hospitalization patternsCitation27. The Premier Database contains information on ∼6 million annual hospital discharges (representing ∼20% of all US hospitalizations), primarily from non-profit, non-governmental, community, and teaching hospitals, and health systems. In 2012, the inpatient database included a sample of ∼5.3 million discharges across 492 US hospitals. In addition to the service-level data recorded in most standard hospital discharge files, the data source also contains a daily log of all billed items at the individual patient level, including procedures, medications, and laboratory tests, as well as diagnostic and therapeutic services. In addition to standard ICD9-CM procedures and diagnosis codes, this study also leveraged Premier Database chargemaster codes referencing ‘EEG’ services and mechanical ventilation.
Population
SRSE does not have a specific International Classification of Diseases-9 (ICD-9) code, and SE codes are used inconsistently. Therefore, the following algorithm was used to classify a discharge as SRSE (): each discharge was required to have a seizure-related ICD-9 code (); an ICU stay of at least 2 days; treatment with benzodiazepines or AEDs; continuous treatment with both IV AEDs (defined as IV anesthetics, IV barbiturates, and IV midazolam; ) and mechanical ventilation; and either or both treatment with AEDs and benzodiazepines together or a definite SE ICD-9 diagnosis code (). Since patients were required to have stayed at the ICU for at least 2 days, patients who died within the first 48 hours were excluded from the cohort. Patients under 18 years old were classified as pediatric patients.
Figure 1. Primary SRSE hospital discharge inclusion criteria. AED, anti-epilepsy drug; ICD-9, International Classification of Diseases-9; ICU, Intensive Care Unit; IV, intravenous; LOS, length of stay; SE, status epilepticus; SRSE, super-refractory status epilepticus.
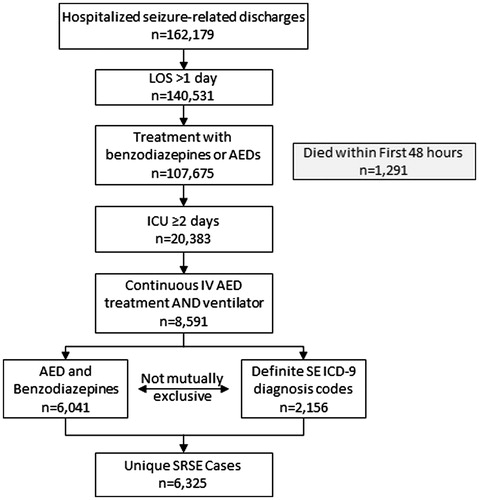
Table 1. Classification of convulsion diagnosis codes to identify initial SE discharge segments.
Table 2. Epilepsy drugs for inclusion.
Outcomes
The primary outcome for the study was the estimated number of annual SRSE cases based on discharges in the Premier Database during 2012. Patients were characterized by healthcare resource utilization, comorbidity, and demographics. The healthcare resource utilization outcomes were reported for overall hospital length of stay (LOS), ICU LOS, epilepsy and non-epilepsy medications, services during hospitalization, discharge status, and total cost of each hospitalization. LOS, services/treatments, and total cost of each hospitalization were abstracted from the dataset directly as supplied by the hospital. ICU LOS was defined as the number of days that ICU room and board charge codes were present during the hospitalization. Medication use was identified based on pharmacy charges. Epilepsy medications included AEDs, benzodiazepines, IV anesthetics, IV barbiturates, and IV benzodiazepines (). Non-epilepsy-specific medications included anti-depressants, anti-infectives, anti-psychotics, bronchodilators, muscle relaxants, narcotics, and vasopressors. Services evaluated were electroencephalogram (EEG), mechanical ventilator use, and tracheotomy. Discharge status indicated whether the patient died in the hospital or was discharged alive. The data did not show whether a patient was discharged home or to another hospital, to long-term care, or to a similar facility. Overall costs were defined as the total cost for hospital treatment and included overhead and direct costs. Costs were calculated based upon cost-to-charge ratios and charges. Reimbursed costs were not available from this dataset. Co-morbid conditions, as defined by ICD-9 codes, were assessed to further characterize the patients.
Analysis
Results were reported for the overall, adult, and pediatric populations. Descriptive statistics were calculated for outcomes, demographic and clinical characteristics, and therapies used. Projection weighting was carried out to estimate the total number of annual hospitalizations of patients classified as SRSE cases, as defined by our algorithm, in the US. The projection was performed at the hospital level. Each discharge was weighted to reflect region, ownership, teaching status, size, and urban designation of hospitals in the Premier Hospital Network, based on national American Hospital Association data. For healthcare resource utilization measures, means and medians were calculated for total hospital LOS and ICU LOS. The proportion of patients utilizing services, epilepsy medications, and other medications were reported. Secondary analyses were conducted to estimate the impact of using more restrictive SRSE algorithms. The first sensitivity analysis evaluated the requirement of an ICU stay of ≥3 days rather than ≥2 days; the other evaluated the requirement of EEG codes during the hospitalization.
Results
Descriptive statistics
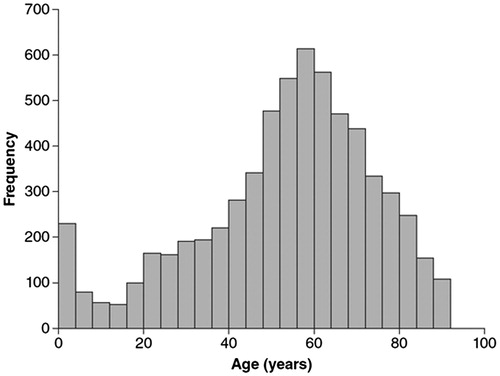
A total of 162,179 seizure-related discharges were identified in the Premier Database, of which 6,325 were classified as SRSE cases based on the primary algorithm (). Adult patients and pediatric patients accounted for 5,863 and 462, respectively, of such discharges. The cases classified as SRSE represented 4% of all ICD-9 codes for seizures in this database. Of all seizure hospitalizations with a hospital LOS of ≤2 days, 1,291 of the patients died during the hospitalization (). Overall, 18% of the patients classified as SRSE cases using the algorithm died during hospitalization; adult mortality was 19%, and pediatric mortality was 5% (). The mean ages of the adult and pediatric patients classified as having SRSE were 56.5 and 5.6 years, respectively (). Seventy per cent of these patients classified as SRSE cases were treated in hospitals with >300 beds. The most common co-morbid conditions were typical for ICU patients, such as acute respiratory failure (74%), essential hypertension (36%), and hypokalemia (32%).
Table 3. Descriptive statistics by age.
National projection
Based on the 6,325 discharges in the Premier Database classified in our study as SRSE cases using the algorithm, it was projected through weighting of these cases based on hospital region, ownership, teaching status, size, and urban designation, and extrapolation using US demographics from 2012, that an estimated 41,156 cases of SRSE occurred in the US during 2012. Of these 41,156 cases, a projected 38,717 (94%) were adults, and 2,439 (6%) were pediatric patients. Based on these results, we further estimated that the total upper limit of the SRSE incidence may be ∼13/100,000 per year in the US.
The second analysis, in which we modified the SRSE definition by requiring an EEG or more days in the ICU, reduced the estimated number of SRSE cases. Using a definition of ≥3 days in the ICU, rather than ≥2 days, reduced the total number of discharges classified as SRSE cases in the database using the algorithm to 5,370. Using the weighting and US demographics, this projected to an estimated 35,150 SRSE cases nationally for 2012, or an incidence rate of 11/100,000 per year in the US. When the SRSE definition in the algorithm included an EEG charge code, a total of 3,998 discharges were classified as SRSE. Including EEG charge codes in the algorithm reduced the extrapolated SRSE projection to 25,915 cases in 2012, or an incidence of 8/100,000 per year in the US.
Healthcare resource utilization
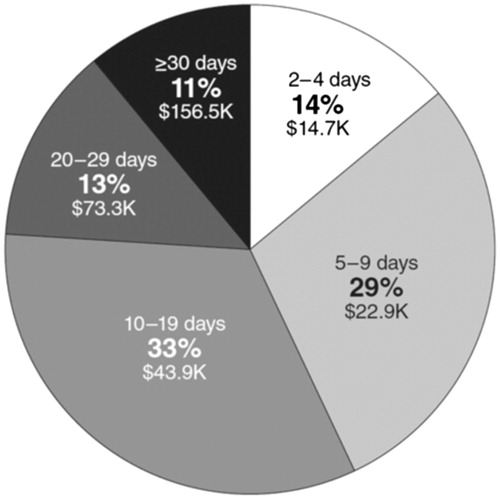
The mean LOS for all patients classified as having SRSE in this sample using the primary methodology was 16.5 days (median = 11; interquartile range [IQR] = 6–20), with a mean of 9.3 days (median = 6; IQR = 3–12) spent in an ICU (). The mean LOS was greater for pediatric patients compared with adults: 20.0 days (median =12; IQR =5–26) vs 16.3 days (median = 11; IQR = 6–19; ). The mean ICU LOS was also longer for pediatric patients compared with adults: 12.7 days (median = 8; IQR = 3–16) vs 9.0 days (median = 6; IQR = 3–11; ). The most common LOS (32%) was 10–19 days ().
Table 4. Costs for LOS, LOS in ICU for adult, pediatric, and overall populations.
The patients classified as SRSE received an average of five different epilepsy medications, with many patients administered multiple medications within each class (). The use of AEDs, benzodiazepines and IV benzodiazepines, and IV midazolam was high in both the adult and pediatric populations (). The use of IV anesthetics was slightly lower in the pediatric population (57%) compared with the adult population (85%), while the use of IV barbiturates was higher in the pediatric population (41%) compared with the adult population (9%: ).
Table 5. Projected services, treatments, and medicines used in treating patients with SRSE.
Costs
The overall mean cost of hospitalization for a patient classified as having SRSE using the primary methodology was $51,247 (95% CI = $49,634–$52,861; ). The mean costs for pediatric and adult patients were $73,230 (95% CI = $64,100–$82,359) and $49,515 (95% CI = $47,938–$51,092), respectively (). The mean cost per day was $3,400 for treating adult patients, compared with $3,860 for treating pediatric patients (). Among adults, Medicare was the most frequent payer, accounting for 52% of discharges (). Medicaid was the most common payer for children (65%). Overall, commercial insurance paid for 18% of discharges ().
Discussion
This is the largest study to date to examine the epidemiology of SRSE using hospital discharge records from chargemaster data and, as far as the authors are aware, the first study to examine the economic impact of hospitalization in SRSE cases. This study suggests that SRSE is associated with significant morbidity, mortality, and healthcare costs. The overall mean cost of treating a patient classified as having SRSE using the primary methodology was $51,247 (95% CI = $49,634–$52,861), with a cost per day of $3,434. SRSE cases had a mean LOS of 16.5 days (median = 11; IQR = 6–20) and a mean ICU LOS of 9.3 days (median = 6; IQR = 3–12). Projections based upon the findings of this study suggest that between 25,915 and 41,156 cases of SRSE may occur in the US each year.
Previous research has shown that the incidence of SE has a bimodal age distribution, with the highest rates occurring in children under 10 years old and adults over 50 years oldCitation3. Jayalakshmi et al.Citation9 observed a similar pattern among SRSE patients. The current study also suggests that SRSE has a bimodal age distribution (). Although age has not been found to be a significant risk factor for SRSE development or mortalityCitation9, the common SRSE etiologies observed in young children and adults (febrile SE/central nervous system infection, and cerebrovascular and immune-mediated disease, respectively)Citation7–9,Citation28–30 may explain the observed distribution.
Figure 3. Age distribution of population. Mean ages: pediatric = 5.6; adult = 56.5; overall 52.7 years. Median ages: pediatric = 4; adult = 57; overall = 56 years; n = 6,325.
The primary aim of this paper is to provide an overall estimation of the annual number of cases of SRSE in the US population and to evaluate the hospital resources used in caring for patients of all age ranges. Variations in the therapies used between the adult and pediatric populations are likely to be due to protocol differences. For example, propofol is less frequently used in children because of the risk of propofol infusion syndromeCitation12.
The mean daily hospitalization costs for adult and pediatric patients classified as having SRSE based on the primary methodology were similar, at $3,400 and $3,860, respectively. However, the mean cost per hospitalization for pediatric patients was $73,230 (95% CI = $69,100–$82,359) compared with $49,515 (95% CI = $47,938–$51,092) for adults. This difference in hospitalization cost appears to be related to the increased LOS in children (20 days) compared with adults (16.3 days). The impact that LOS had upon costs was also seen in the overall population, with shorter stays being associated with lower costs (). Twenty-four per cent of all patients spent ≥20 days in the hospital. The mean cost of treating those with a LOS of 20–29 days was $73,300, while the mean cost of treating those with a LOS of ≥30 days was $156,500 ().
There are more than 6,500 hospitals in the US, over 1,000 of which are tertiary hospitalsCitation31. Most patients classified in the study as having SRSE based on the primary methodology (70%) were treated in hospitals with >300 beds. Hospitals of this size are typically tertiary centers, suggesting that SRSE is usually managed in specialist care facilities.
Data on the prevalence of SE, RSE, and SRSE continue to evolve. There are a range of estimates in the literature, but a lack of comprehensive studies of large patient populations. Prevalence may vary country-to-country based on differences in the rate of occurrence of the underlying conditions and differences in accurate diagnosis rates and reporting. Previous reports estimate that SE affects from 12.5–61 people per 100,000 per year in the US. Globally, investigators have estimated that 5–17% of SE cases become SRSE cases, suggesting that SRSE may occur in up to 10 people per 100,000 per year in the USCitation9,Citation10,Citation12,Citation22. Using the primary methodology, the current study estimates the annual incidence of SRSE in the US to be 13/100,000 per year with a projected figure of 41,156 cases of annual US SRSE. These variations in estimates of incidence may be explained by limitations of the methodology. For instance, as a consequence of our algorithm, some patients with RSE may inadvertently have been included in the SRSE groupCitation32. In fact, employing more stringent SRSE definition criteria reduced the SRSE estimates. For example, when ≥3 ICU days were required in applying the algorithm, the estimated annual SRSE discharges in the US was reduced by ∼15% to 35,150.
One of the major limitations of this study is the restricted accuracy of the database’s EEG codes. In cases of SE, RSE, and SRSE, continuous EEG should be initiated within 1 h of SE onset if ongoing seizures are suspectedCitation4. In this database, 63% of discharges classified SRSE cases based on the algorithm had EEG charge codes. Reasons for this may be that some of the smaller hospitals may not have EEG capability or that EEG codes were not recorded by the chargemaster data. When an EEG code was used as part of the SRSE definition, the patient population classified as SRSE cases was decreased by ∼45%, which projected to 25,915 SRSE patients in 2012, or an estimated incidence rate in the US of 8/100,000 per year. This figure more closely aligns with literature-based estimations that 5–17% of SE cases, which have been estimated to occur in 12.5–61 cases/100,000 per year in the US, will develop into SRSE casesCitation9,Citation10,Citation12,Citation22.
In this and previous studies, the validity of EEG charge codes might be limited, since an EEG is a comparatively inexpensive procedure and a more general code, or the code that maximizes reimbursement may have been used in preference to the most accurate codeCitation33. Furthermore, while it has been demonstrated that providers in neurology care often undercodeCitation33,Citation34, adding EEG charges could also lead to over-estimations. For example, patients admitted with subarachnoid hemorrhage are monitored with continuous EEG for up to 10 days for surveillance of focal slowing, as a marker of the early development of focal cerebral injury following aneurysmal subarachnoid hemorrhageCitation35–37. These patients are more often mechanically ventilated and administered anesthetics, as well as prophylactic anti-epileptic medications. They would only be excluded in our algorithm because of the absence of an ICD-9 code for seizures.
Standardization to guide health-services researchers in their case definitions would be ideal. For instance, some authors have tried to standardize, or provide guidance to, claims-based studies in epilepsyCitation38–40. However, their case definitions do not specify SRSE. Once validated algorithms become available, researchers could explore and compare additional differences, such as particularities of databases, demographics, and care characteristics. For SE patients, step-wise, separate algorithms to identify SE, RSE, and SRSE cases would be idealCitation41. In addition, validation against patient charts would enhance the validity of our findings and provide the platform for subsequent studies.
SRSE has a high mortality rate, and patients who survive are frequently left with some level of neurologic deficit after the episode: only ∼30% of patients achieve satisfactory cognitive outcomesCitation12,Citation42,Citation43. Such levels of mortality and morbidity place significant burdens upon healthcare resources and demonstrate that SRSE remains an area of high unmet need. The mortality rate of 18% observed in this study was lower than the mortality rates of 35–62% reported by other studiesCitation12,Citation42,Citation43. However, the present study estimated the mortality rate within a single hospitalization, whereas previous reports for SRSE mortality have been for a given period of time, such as 1 yearCitation42. Because the present study evaluated only SRSE hospitalizations, any deaths that occurred after discharge were not captured. Additionally, because our definition of SRSE required patients to be in the ICU for at least 2 days, anyone who died within the first day or who died before hospitalization was excluded from this study.
Similarly, the mean LOS for patients in this inpatient hospital database classified as SRSE cases based on the algorithm was overall shorter than what is expected and published for patients with SRSE. However, the duration of stay might be influenced by many factors, including comorbidities, etiology, and discharge status. As outlined above, we were not able to capture discharge status, and this may have led to an important decrease in the mean LOS in our sample. In other words, we were not able to differentiate between patients who were sent home vs patients who were transferred.
Second, the observed LOS using claims data might be significantly different from the observed LOS in smaller cohort studies at academic centersCitation7–9,Citation14. The recent literature suggests that LOS have significant within-hospital and between-hospital variance. This may be partially explained by the various financial and political incentives that hospitals have to discharge patients. As a result, we further believe that the mean LOS for SRSE hospitalizations may have been under-estimated, and that the true mean may have changed over time, and should be stratified by discharge status.
Other studies have examined the economic burden associated with SECitation16,Citation32,Citation44. Using data from 1993–1994, Penberthy et al.Citation32 estimated the annual reimbursed cost in the US for SE inpatient admissions at $4.0B, which is $6.2B after adjusting for inflation. Based on the current study, if we assume that there were 6,325 SRSE hospitalizations with an average cost of $51,250, the total annual cost of SRSE hospitalizations in 2012 would have been ∼$324 million. However, the overall financial impact of caring for patients with SRSE is likely to be much higher than our estimate, since our results do not include non-hospital care, such as community nursing, social care, ambulances, and rehabilitation.
This study had several limitations, including that the data source is based upon claims/chargemaster information (surrogate measures), which does not include definitive chart level patient information. Although a robust data source, this claims information is imperfect and difficult to validate. Other limitations were the lack of specific diagnostic ICD-9 codes for RSE and SRSE and that management of these patients varies between hospitals, units, and clinicians, thus making it difficult to distinguish between SRSE, RSE, and SE on the basis of care patterns. The definition of SRSE was based upon a combination of ICU, LOS, medications, and other available data. Information about when patients were initiated and weaned from various epilepsy medications, along with the reasons for medication changes, would have allowed us to more accurately classify SRSE patients; however, this information was not available in the data source. While a chart audit would have provided this treatment information, it would not have included cost data and would by necessity have been a much smaller and, therefore, less representative, sample.
Another limitation of this study was that, while all patients had seizures, the data did not indicate the reason for the hospitalization. Defining SRSE patients as those who were seen by a neurologist would have provided a more accurate population estimate. However, complete data regarding physician type was unavailable. Benzodiazepine administration was not seen in 4% of patients. This may be due to emergency or pre-hospitalization treatment with benzodiazepines in an ambulance, which may not have been captured in the inpatient database ().
Yet another limitation of the data set was the lack of even more granular data, such as specific anesthetics doses used and whether the patients received anesthetics for sedation during mechanical ventilation and/or for treatment of SRSE. Doses for sedation may vary according to multiple clinical factors, such as weight, age, and other medications, as well as unmeasured factors, such as prescriber experience. As described by WalkerCitation41, when working with claims database algorithms, the information resides in data patterns, rather than data elements, which requires a fresh view of research. The author makes the case that temporal sequence is crucial and that any true indication is represented by a specific sequence orderCitation41. Following this logic, we have with our case-definition tried to follow a stepwise temporal sequence to accurately identify cases of SRSE, starting with the basic case definitions of SE, and adding temporal components to differentiate RSE and SRSECitation17,Citation39,Citation45–51.
Previous studies have demonstrated varying degrees of sensitivity, particularly those which independently surveyed epilepsy prevalence via provider or a separate random sample of chart reviewCitation17,Citation33,Citation39,Citation45–51. In fact, there are no specific ICD-9 codes for SRSE. We used seizure-related ICD-9 codes in addition to other criteria to try to enhance the accuracy of our case definitionCitation17,Citation39,Citation45–51. In epilepsy, validation studies of medical claims databases suggest that accuracy may depend on a variety of factors. A study of Medicaid using ICD codes found that incidence of epilepsy could not be determined before 3 years of enrollment due to claims trendsCitation46. In addition, a comparison of ILAE disease classification and ICD determined that there were significant variations between these systems and versions, resulting in varying ICD validity over timeCitation33. The sensitivity of combined algorithms (ICD-9 + EEG + Medications) may be expected to be high, due to payment incentives for codingCitation52.
Patients who died or recovered during the first 48 h of hospitalization were excluded from the analysis, which may have impacted cost assessments. Based on time/treatment selection criteria, these patients could not be identified as having SRSE according to our definition. We would expect these cases to be associated with comparatively low costs and, thus, had they been incorporated into the dataset, the overall mean cost might have been reduced.
Mortality rate in addition to incidence rate would be a valuable measure to compare our findings with previous studies using different observational datasets. However, our mortality rate of 19% was derived after we excluded patients who died during the first 48 h of admission. While these patients could not be identified as having SRSE, most of these patients would have met the criteria for RSE which would fall within the published mortality rate range of 7–46%Citation7,Citation12,Citation53.
Conclusion
This study suggests that SRSE is associated with high mortality and morbidity, and significant use of healthcare resources. The mean cost of hospital care for a patient classified as having SRSE using the primary methodology was $51,247. Projections based on the number of cases classified as SRSE using the algorithm suggest that US hospitals may treat between 25,915–41,156 cases of SRSE annually. However, more in-depth studies are needed to accurately determine the prevalence of SRSE. Improved prevention and early detection methods are needed for SRSE; these may improve outcomes and decrease healthcare resource utilization. Further research into effective therapies specifically aimed at treating SRSE could also help to reduce the societal and economic impact of this condition.
Transparency
Declaration of funding
This study was supported by Sage Therapeutics, Inc.
Declaration of financial/other relationships
JB, TA, and SK are employees and shareholders of Sage Therapeutics. KF, DF, TF, and SS are employees of Trinity Partners and have received consulting fees from Sage Therapeutics. LM is a former employee of Trinity Partners and has received consulting fees from Sage Therapeutics. Lidia Moura is an epileptologist at Massachusetts General Hospital.
Acknowledgments
We thank Trinity Partners. We thank Bexon Clinical Consulting LLC, Mr Matthew Reid, and Alice Bexon for medical writing services, which were funded by Sage Therapeutics.
References
- DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology 1996;46:1029-35
- DeLorenzo RJ, Kirmani B, Deshpande LS, et al. Comparisons of the mortality and clinical presentations of status epilepticus in private practice community and university hospital settings in Richmond, Virginia. Seizure 2009;18:405-11
- Dham BS, Hunter K, Rincon F. The epidemiology of status epilepticus in the United States. Neurocrit Care 2014;20:476-83. http://www.ncbi.nlm.nih.gov/pubmed/24519080. Accessed March 31, 2016
- Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 2012;17:3-23
- Shorvon S. Super-refractory status epilepticus: An approach to therapy in this difficult clinical situation. Epilepsia 2011;52(Suppl 8):53-6
- Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: A critical review of available therapies and a clinical treatment protocol. Brain 2011;134:2802-18
- Hocker S, Tatum WO, LaRoche S, et al. Refractory and super-refractory status epilepticus - An update. Curr Neurol Neurosci Rep 2014;14: 452
- Li Y, Tian L, Zeng T, et al. Clinical features and outcome of super-refractory status epilepticus: A retrospective analysis in West China. Seizure 2014;23:722-7
- Jayalakshmi S, Ruikar D, Sudhindra Vooturi, et al. Determinants and predictors of outcome in super refractory status epilepticus—A developing country perspective. Epilepsy Res 2014;108:1609-17
- Tian L, Li Y, Xue X, et al. Super-refractory status epilepticus in West China. Acta Neurol Scand 2015;132:1-6
- Trinka E, Shorvon S. Status epilepticus—Where are we in 2013? Epilepsia 2013;54(Suppl 6):1-2
- Shorvon S, Ferlisi M. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain 2012;135:2314-28
- Zeiler FA. Early Use of the NMDA Receptor Antagonist Ketamine in Refractory and Superrefractory Status Epilepticus. Critical Care Research and Practice 2015;2015:5
- Zhumadilov A, Gilman CP and Viderman D. Management of super-refractory status epilepticus with isoflurane and hypothermia. Front. Neurol. 2015;5:286
- Thakur KT, Probasco JC, Hocker SE, et al. Ketogenic diet for adults in super-refractory status epilepticus. Neurology 2014;82:665-70
- Strzelczyk A, Knake S, Oertel WH, et al. Inpatient treatment costs of status epilepticus in adults in Germany. Seizure 2013;22:882-5
- Betjemann JP, Josephson SA, Lowenstein DH, et al. Trends in status epilepticus-related hospitalizations and mortality: Redefined in US practice over time. JAMA Neurol 2015;72:650-5. http://www.ncbi.nlm.nih.gov/pubmed/25915004. Accessed February 1, 2016
- Hesdorffer DC, Logroscino G, Cascino G, et al. Incidence of status epilepticus in Rochester, Minnesota, 1965–1984. Neurology 1998;50:735-41
- Logroscino G, Hesdorffer DC, Cascino G, et al. Time trends in incidence, mortality, and case-fatality after first episode of status epilepticus. Epilepsia 2001;42:1031-5
- Monthly population estimates for the United States: April 1, 2010 to December 1, 2016. US Census Bureau, Population Division. 2015. http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed June 19, 2016
- Neligan A, Shorvon SD. Frequency and prognosis of convulsive status epilepticus of different causes: a systematic review. Arch Neurol 2010;67:931-40
- Kantanen A-M, Reinikainen M, Parviainen I, et al. Incidence and mortality of super-refractory status epilepticus in adults. Epilepsy Behav 2015;49:131-4
- Giovannini G, Monti G, Polisi MM, et al. A one-year prospective study of refractory status epilepticus in Modena, Italy. Epilepsy Behav 2015;49:141-5
- Novy J, Logroscino G, Rossetti AO. Refractory status epilepticus: A prospective observational study. Epilepsia 2010;51:251-6
- Mayer SA, Claassen J, Lokin J, et al. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol 2002;59:205-10
- Rossetti AO, Logroscino G, Bromfield EB. Refractory status epilepticus. Arch Neurol 2005;62:1698-702
- Premier Research Services. https://www.premierinc.com/transforming-healthcare/healthcare-performance-improvement/premier-research-services/. Accessed June 30, 2016
- Holtkamp M, Othman J, Buchheim K, et al. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry 2005;76:534-9
- Gizerian SS. Neurosteroids in cortical development and the etiology of schizophrenia. In Neuroactive Steroids in Brain Function, Behavior and Neuropsychiatric Disorders: Novel Strategies for Research and Treatment. 2008. p. 299 -324
- Schreiber JM, Gaillard WD. Treatment of refractory status epilepticus in childhood. Curr Neurol Neurosci Rep 2011;11:195-204
- Health care institutions-Types of hospitals. Library Index. 2016. http://www.libraryindex.com/pages/1831/Health-Care-Institutions-TYPES-HOSPITALS.html. Accessed June 6, 2016
- Penberthy LT, Towne A, Garnett LK, et al. Estimating the economic burden of status epilepticus to the health care system. Seizure 2005;14:46-51
- Jette N, Beghi E, Hesdorffer D, et al. ICD coding for epilepsy: past, present, and future—a report by the International League Against Epilepsy Task Force on ICD codes in epilepsy. Epilepsia 2015;56:348-55
- Fillit H, Geldmacher DS, Welter RT, et al. Optimizing coding and reimbursement to improve management of Alzheimer’s disease and related dementias. J Am Geriatr Soc 2002;50:1871-8
- Labar DR, Fisch BJ, Pedley TA, et al. Quantitative EEG monitoring for patients with subarachnoid hemorrhage. Electroencephalogr Clin Neurophysiol 1991;78:325-32
- Claassen J, Hirsch LJ, Kreiter KT, et al. Quantitative continuous EEG for detecting delayed cerebral ischemia in patients with poor-grade subarachnoid hemorrhage. Clin Neurophysiol 2004;115:2699-710
- Friedman D, Claassen J, Hirsch LJ. Continuous electroencephalogram monitoring in the intensive care unit. Anesth Analg 2009;109:506-23
- Thurman DJ, Beghi E, Begley CE, et al. Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia 2011;52(Suppl 7):2-26
- Reid AY, St. Germaine-Smith C, Liu M, et al. Development and validation of a case definition for epilepsy for use with administrative health data. Epilepsy Res 2012;102:173-9
- St. Germaine-Smith C, Metcalfe A, Pringsheim T, et al. Recommendations for optimal ICD codes to study neurologic conditions: a systematic review. Neurology 2012;79:1049-55
- Walker AM. Pattern recognition in health insurance claims databases. Pharmacoepidemiol Drug Saf 10:393-7. http://www.ncbi.nlm.nih.gov/pubmed/11802583. Accessed June 6, 2016
- Pugin D, Foreman B, De Marchis GM, et al. Is pentobarbital safe and efficacious in the treatment of super-refractory status epilepticus: a cohort study. Crit Care 2014;18:R103
- Cooper AD, Britton JW, Rabinstein AA. Functional and cognitive outcome in prolonged refractory status epilepticus. Arch Neurol 2009;66:1505-9
- Kortland LM, Knake S, Rosenow F, et al. Cost of status epilepticus: A systematic review. Seizure 2015;24:17-20
- Franchi C, Giussani G, Messina P, et al. Validation of healthcare administrative data for the diagnosis of epilepsy. J Epidemiol Community Health 2013;67:1019-24
- Bakaki PM, Koroukian SM, Jackson LW, et al. Defining incident cases of epilepsy in administrative data. Epilepsy Res 2013;106:273-9
- Christensen J, Vestergaard M, Olsen J, et al. Validation of epilepsy diagnoses in the Danish National Hospital Register. Epilepsy Res 2007;75:162-70
- Christensen J, Vestergaard M, Pedersen MG, et al. Incidence and prevalence of epilepsy in Denmark. Epilepsy Res 2007;76:60-5
- Tu K, Wang M, Jaakkimainen RL, et al. Assessing the validity of using administrative data to identify patients with epilepsy. Epilepsia 2014;55:335-43
- Faught E, Richman J, Martin R, et al. Incidence and prevalence of epilepsy among older US Medicare beneficiaries. Neurology 2012;78:448-53
- Tan M, Wilson I, Braganza V, et al. Development and validation of an epidemiologic case definition of epilepsy for use with routinely collected Australian health data. Epilepsy Behav 2015;51:65-72
- McWilliams JM, Landon BE, Chernew ME. Changes in health care spending and quality for Medicare beneficiaries associated with a commercial ACO contract. JAMA 2013;310:829-836. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3860102&tool=pmcentrez&rendertype=abstract. Accessed May 20, 2016
- Logroscino G, Hesdorffer DC, Cascino G, et al. Mortality after a first episode of status epilepticus in the United States and Europe. Epilepsia 2005;46(Suppl. 11):46-8