Abstract
Objectives: In China, both human urinary kallindinogenase (HUK) and 3-n-butylphthalide (NBP) are recommended for clinical use to improve cerebral blood circulation during an acute ischemic stroke (AIS). The objective was to evaluate the economic value of HUK vs NBP for patients with AIS from a Chinese payer’s perspective.
Methods: An economic evaluation based on data of patients who have been treated with either HUK (n = 488) or NBP (n = 885) from a prospective, phase IV, multi-center, clinical registry study (Chinese Acute Ischemic Stroke Treatment Outcome Registry, CASTOR) was conducted to analyze the cost and effectiveness of HUK vs NBP for AIS in China. Before the analysis, the patients were matched using propensity score. Both a cost-minimization analysis and a cost-effectiveness analysis were conducted to compare the matched pairs. A bootstrapping exercise was conducted for the matched arms to demonstrate the probability of one intervention being cost-effective over another for a given willingness-to-pay for an extra quality-adjusted life-year (QALY).
Results: After propensity score matching, 463 pairs were matched. The overall medical cost in the HUK arm is USD 2,701.20, while the NBP arm is USD 3,436.83, indicating HUK is preferred with cost-minimization analysis. Although the QALY gained in the HUK arm (0.77176) compared with the NBP arm (0.76831) is statistically insignificant (p = .4862), the cost-effectiveness analysis as exploratory analysis found that, compared with NBP, HUK is a cost-saving strategy with the lower costs of USD 735.63 and greater QALYs gained of 0.00345. Among the 5,000 bootstrapping replications, 100% indicates that HUK is cost-effective compared with NBP under a 1-time-GDP threshold; and 97.12% indicates the same under a 3-time-GDP threshold.
Conclusion: This economic evaluation study indicates that administrating HUK is a cost-saving therapy compared with NBP for managing blood flow during AIS in the Chinese setting.
Introduction
Acute ischemic stroke (AIS) is one of the most debilitating conditions to human health by leading to disability and death after the acute attacks. In China, cerebrovascular disease in urban and country areas was reported to be the third and the second leading cause of death in 2015, respectively. The 2015 yearly mortality rates in urban and country areas were 128.23 per 100,000, and 153.63 per 100,000, respectivelyCitation1. A nationally-representative door-to-door survey conducted in 2013 in China reported that the incidence of a diagnosed stroke was estimated to be 345.1 per 100,000, and its prevalence was estimated to be 1,596.0 per 100,000 per year. Ischemic stroke is the most common category among all kinds of stroke, accounting for 69.6% and 77.8% of the incidence and the prevalence, respectivelyCitation2. Inpatient treatment was likely to be needed by patients with an ischemic stroke, sometimes more than once annually, which potentially contributes to a heavy burden on Chinese society. In China, the number of discharged patients with a cerebral infarction in 2015 was 5.71 million, with an average yearly growth rate being 12.16% from 1980 to 2015. In 2015, the total hospitalization expense for cerebral infarction was USD 8.07 billion (converted from CNY using the exchange rate in the end of year 2015), with a 23.47% average annual growth rate since 2004Citation3. With the increased prevalence of cigarette smokers, overweight and obese people, hypertension patients, and dyslipidemia patients, the burden of stroke in China is predicted to rise in the futureCitation4.
In China, human urinary kallindinogenase (HUK) and 3-n-butylphthalide (NBP), as Chinese first-class national new drugs, were recommended by the Chinese guidelines for diagnosis and treatment of acute ischemic stroke to be used for improving cerebral blood circulation during an AISCitation5, with which the clinical need of comparing these two interventions arose. Both HUK and NBP are proven to be able to effectively promote cerebral perfusion and angiogenesis in the ischemic area after a strokeCitation6–9. Especially for HUK, the clinical value in reducing the risk of death or dependency and the improvement of neurological deficit has been demonstrated by a systematic review that included 24 clinical trialsCitation10. Despite the clinical need of comparing HUK and NBP, there are, however, no published studies that examined the cost-effectiveness of HUK and NBP yet. In order to provide further social economic evidence to support rational administration of medications treating AIS, we conducted an economic evaluation based on the 1-year follow-up efficacy and medical-related cost data from a prospective, phase IV, multi-center, clinical registry study (Chinese Acute Ischemic Stroke Treatment Outcome Registry, CASTOR) to evaluate the cost-effectiveness of HUK vs NBP for treating AIS in China.
Methods
Patients included
This study included participants of the CASTOR study, which is an ongoing, naturalistic, prospective, phase IV, multi-center, clinical registry study. The study planned to include 10,000 patients with AIS. The inclusion and exclusion criteria are as follows:
Inclusion criteria:
The patients were 18 years of age or older;
The patients were diagnosed based on the criteria of the guidelines for the diagnosis and treatment of acute ischemic stroke in China (2014)Citation5;
For thrombolysis patients, the time of involvement was within the thrombolysis time window;
For non-thrombolysis patients, the time of involvement was within 1 week from the attack; and
The patient or legal guardian understood and signed the informed consent form.
Exclusion criteria:
Cranial computed tomography or magnetic resonance imaging showed the existence of cerebral hemorrhage;
The patients were expected to survive for less than 3 months due to severe co-morbidities; or
The ability of continuous follow-up was doubted by the physicians.
At the time of analysis, 5,188 patients had been recruited, among which 2,893 patients had follow-up data for more than 1 year. Among these 2,893 patients, there were 1,373 patients who had been treated with either HUK or NBP. Note, the patients who had received both HUK and NBP were excluded, since the main goal of the cost-effectiveness analysis is to compare HUK to NBP directly. With the above criteria, a total of 1,373 patients were included in the cost-effectiveness analysis.
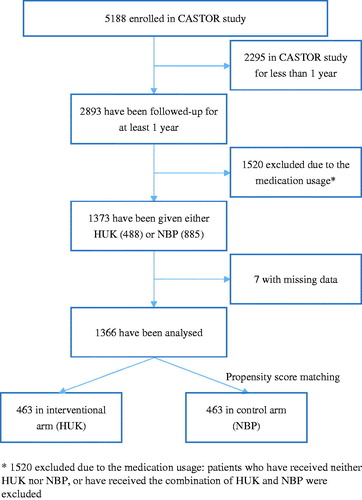
The CASTOR study was designed as an intention-to-treat study, in which patients were not assigned to any controlled interventional group, but were treated based on patients’ needs or real conditions. Therefore, the results represent the real patient behaviors, including real compliances and other information in real-world practice. In order to compare the cost-effectiveness of HUK and NBP, the data of the 1,373 patients were divided into two groups: (A) patients treated with NBP but not HUK (n = 885), and (B) patients treated with HUK but not NBP (n = 488). Finally, propensity score matching analysis was performed on these patients and yielded 463 pairs of patients for the final analysis. The patient flow is depicted in .
Cost data
The direct medical costs were recorded during the CASTOR study, while the direct non-medical costs, i.e. the transportation fees, nutrition fees, and accompany expenses of the family members, were obtained via regular interviews. However, the direct non-medical costs were of relatively poor quality, with 33.5% of the data missing, and could be influenced by multiple factors that were not controlled in this study, such as the interviewee’s memory accuracy. Therefore, the direct non-medical costs were not included in the cost-effectiveness analysis.
The medical service fees, diagnostic costs, treatment fees, rehabilitation costs, medication costs, blood and blood product costs, medical supplies costs, and other medical costs were measured via reviewing patient charts from the Electronic Data Capture (EDC) system. The total inpatient medical costs were calculated for each patient.
All the costs were converted from CNY to USD using the exchange rate at the end date of the data abstracting (1 CNY = 0.145 USD, March 3, 2017).
Effectiveness data
The effectiveness was evaluated with the quality-adjusted life-years (QALYs) gained. A generic three-level EuroQol five-dimensional questionnaire (EQ-5D-3L) was used in the CASTOR study to measure the health-related quality-of-life at four points of time, which were 0 days before medication treatment, hospital discharge time, 90 ± 7 days after medication, and 360 ± 28 days after medication. The patients’ answers to the EQ-5D-3L questionnaire were converted into utility scores using the Chinese time trade-off scoring algorithmCitation11. QALYs were estimated as the area under the curve that linearly interpolated through all points of measurements during the CASTOR study.
Statistical and economic analysis
According to a two-sample Wilcoxon rank-sum (Mann-Whitney) testCitation12,Citation13, the baseline utility values of the patients in these two groups are found to not be evenly distributed (p < .0001). In order to counteract this potentially introduced selection bias, a propensity score matching method was used. After the propensity score matching, a cost-minimization analysis was conducted based on the very similar clinical efficacy between the two comparison groups. To account for the minor and inconsiderable difference in effectiveness between both arms, a cost-effectiveness analysis was conducted as well. The perspective of the economic evaluation is of payers in the Chinese healthcare system. All analyses were conducted with Stata/SE version 12 (Stata Corp LP, College Station, TX).
Propensity score matching
As the first step, propensity scores for each entity were generated using a multivariable logistic regression analysis model based on the following covariates: age, sex, insurance type, whether aspirin was used, stroke history, hypertension history, diabetes history, dyslipidemia history, coronary heart disease history, atrial fibrillation history, carotid artery plaque history, tumor history, baseline NIHSS (national institutes of health stroke scale), baseline GCS (Glasgow coma scale), baseline mRS (modified Rankin scale), and baseline utility value transferred from EQ-5D-3L. Two variables, which are BMI (body mass index) and TOAST (Trial of Org 10172 Acute Stroke Treatment) classification data, were not included because about half of the subjects’ information on these two variables were missing. It is thought that, rather than imputing them with arbitrary assumptions or only using completed data (resulting in losing half of the sample size), excluding these two variables could be the best choice. As the second step, the propensity scores were then employed to create 1:1 matched pairs (patients treated with NBP but not HUK vs patients treated with HUK but not NBP) using a nearest neighbor matching algorithm with a caliper of 0.03 of the standard deviation methodCitation14. In total, 463 pairs of patients were matched and included in this analysis, as shown in . The imbalance of the baseline characteristics between the two arms was then eliminated, which made the matched arms comparable (see Supplementary Appendix).
Cost-minimization analysis
The difference of the QALY gained of the involved patients was assessed with Wilcoxon signed-rank test to confirm whether a cost-minimization analysis is suitable in this case. The total direct medical costs were summarized and compared by the treatment arms over the 1-year follow-up. According to the protocol of the CASTOR study, the direct medical costs consist of the medical service fees, diagnostic costs, treating fees, rehabilitation costs, medication costs, blood and blood product costs, medical supplies costs, and other medical costs.
Cost-effectiveness analysis
The incremental cost-effectiveness ratio (ICER) was calculated by dividing the incremental cost by the incremental QALY gained. The value of 1–3-times the Chinese gross domestic product (GDP) per capita (Chinese GDP per capita = USD 7827) was used as a threshold to determine whether the more effective intervention is worthy of the extra money spentCitation15–17.
In order to assess the sampling uncertainty of the analysis, a bootstrapping exercise was conducted for the matched arms of patients as a probabilistic sensitivity analysis. In total 5,000 bootstrapping replications were generated for each group using the Monte Carlo simulation methodCitation18. The bootstrapping replications were plotted in a cost-effectiveness plane and compared across the groups as the sensitivity analysis. The cost-effectiveness acceptability curves (CEAC) were calculated to demonstrate the probability of one intervention being cost-effective over another for a given value of the ceiling ratio or the willingness-to-pay (WTP) for an extra QALY.
Results
Cost-minimization analysis
The QALYs gained for patients in each arm are summarized in , with HUK group gaining 0.77176 and the NBP group gaining 0.76831. According to a Wilcoxon signed-rank testCitation12,Citation19,Citation20, the hypothesis that the difference of QALYs between the paired arms follows a symmetric distribution around zero cannot be rejected (p = .4862), indicating that the two interventions have an insignificant difference in bringing effectiveness to patients. Meanwhile, the absolute difference of the mean QALY gained of one group over the other in 1 year is ∼0.00345, which can hardly be interpreted as clinically significant, as the threshold of being considered a minimum clinically important difference has been noted to be 0.03 or more by previous studiesCitation21–24. Therefore, the rationale of using a cost-minimization analysis is rightful.
Table 1. The summary of direct medical costs and QALYs gained by arm after matching.
The average medical costs are presented in . The cost minimization analysis indicated that the cost in the HUK arm is USD 2,701.20 (standard error of mean is 53.15), while in the NBP arm it is USD 3,436.83 (standard error of mean is 115.67). This analysis suggested that, compared with the NBP group, administering HUK reduces the overall costs, and the saved amount is ∼ USD 735.63, which is ∼21.3% of the annual disposable income per capita in China.
Cost-effectiveness analysis
The average medical cost in the HUK arm is USD 2,701.20 (standard error of mean is 53.15), while in the NBP arm it is USD 3,436.83 (standard error of mean is 115.67). The average QALY gained in the HUK arm is 0.77176 (standard error of mean is 0.01165), while in the NBP arm it is 0.76831 (standard error of mean is 0.01084). The cost of HUK is less than the of NBP by USD 735.63, while the QALY gained of HUK is more than that of NBP by 0.00345, which indicates that NBP is dominated by HUK in terms of the cost-effectiveness.
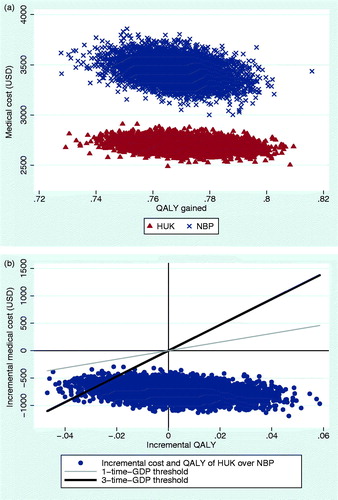
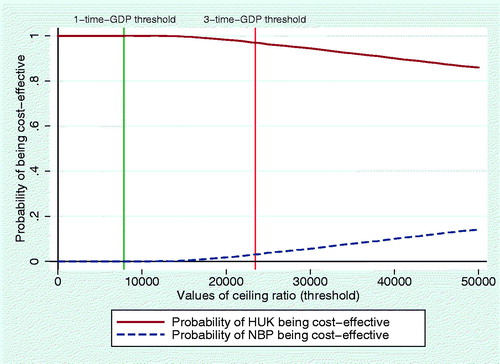
The 5,000 bootstrapping replications for the two matched groups are plotted into one cost-effectiveness plane in . The incremental costs and QALYs of the bootstrapping replications are presented in another cost-effectiveness plane with threshold lines in . Furthermore, the CEAC is drawn in , presenting the probabilities of HUK being cost-effective. In , it can be seen that the curve of HUK is above that of NBP over the whole range from the 1-time-GDP threshold to the 3-time-GDP threshold. There are 100% bootstrapping replications indicating that HUK is cost-effective compared with NBP under a 1-time-GDP threshold; and there are 97.12% replications indicating HUK is cost-effective under a 3-time-GDP threshold.
Discussion
After the propensity score matching, the cost-minimization analysis indicated that HUK has similar efficacy to NBP and lower overall cost compared with NBP. On the cost-effectiveness analysis that accounted for the minor QALY gain difference in the two groups, it was suggested that HUK is a cost-saving strategy with lower cost and greater QALY gained compared with NBP under 1- or 3-times of the GDP per capitaCitation15–17. Probability sensitivity analysis with bootstrapping method indicates that the probability of HUK being cost-effective compared with NBP is 100% under a 1-time-GDP threshold, and the probability of HUK being cost-effective is 97.12% under a 3-time-GDP threshold.
According to the above findings, administrating HUK rather than NBP tends to cost less medical resources, resulting in a slight but not significant enhancement on effectiveness. With the burden of AIS in China being relatively heavy, the usage of HUK rather than NBP could potentially relieve some burden. Furthermore, with pharmacoeconomics information playing an increasingly important role in China’s national or provincial reimbursement drug list decision, this analysis offered real-world cost-effectiveness evidence to support evidence-based decision-making. The decision-makers can rely on these analysis results to include medications with less overall costs, while yielding similar clinical outcomes.
The main strength of this cost-effectiveness analysis is that the data were from a naturalistic clinical registry study that can represent the real-world effectiveness of patients with AIS. Therefore, this study can be considered to be providing more practical information than a RCT in assisting decision-making. Moreover, when the insignificant difference in effectiveness between two arms were found, not only a cost-minimization analysis was conducted, but also the bootstrapping replications were simulated to demonstrate how likely the minor effectiveness difference would impact the decision-making. This was achieved by providing information about the probability of either HUK or NBP being cost-effective under different WTP thresholds.
There are some limitations around the method to impute the missing numbers. The missing numbers were filled in with the mean value of each, which apparently tends to under-estimate the dispersion of the numbers, and, hence, to under-estimate the dispersion of the final outcomesCitation25. However, the missing numbers only account for a very small proportion of the whole sample. Therefore, it can be assumed that these limitations regarding the missing number imputation are not very likely to have an impact on the results.
Additionally, the time horizon of this study was limited to 1-year, as the CASTOR study was designed to follow-up for at most 1 year. Without an appropriate predictive model, the longer-term outcomes of the interventions cannot be captured.
Currently, there is no published literature demonstrating the efficacy or economic superiority of either HUK or NBP. This study provided the first real-world information to support the decision of administrating either HUK or NBP. Further RCT, RCT-based economic evaluation or model-based economic evaluation are needed to examine and add power to the findings.
Conclusion
This economic evaluation study indicates that administerng human urinary kallindinogenase (HUK) is a cost saving therapy compared with 3-n-butylphthalide (NBP) for acute ischemic stroke (AIS) in a Chinese setting. It provides comprehensive economic information to support decision-making in selecting HUK or NBP in the management of AIS.
Transparency
Declaration of funding
This study was funded by Techpool Bio-pharma Co., Ltd.
Declaration of financial/other relationships
No relationships to be declared. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Appendix.docx
Download MS Word (19.7 KB)Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- National Bureau of Statistics of China. China statistical yearbook. 2016. China Statistics Press, China. http://www.stats.gov.cn/tjsj/ndsj/2016/indexeh.htm
- Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China. Circulation 2017;135:759-71
- National Center for Cardiovascular Diseases of China. Report on cardiovascular disease in China (2016). Beijing, China: Encyclopedia of China Publishing House; 2017
- Wang YL, Wu D, Liao X, et al. Burden of stroke in China. Int J Stroke 2007;2:211-13
- Neurology Branch of Chinese Medical Association, Cerebrovascular Disease Group. Guidelines for the diagnosis and treatment of acute ischemic stroke in China (2014). Chin J Neurol 2015;48:246-57
- Lu X, Luo D, Yao X, et al. Dl-3n-butylphthalide promotes angiogenesis via the extracellular signal-regulated kinase 1/2 and phosphatidylinositol 3-kinase/Akt-endothelial nitric oxide synthase signaling pathways. J Cardiovasc Pharmacol 2012;59:352-62
- Liao SJ, Lin JW, Pei Z, et al. Enhanced angiogenesis with dl-3n-butylphthalide treatment after focal cerebral ischemia in RHRSP. Brain Res 2009;1289:69-78
- Han L, Li J, Chen Y, et al. Human urinary kallidinogenase promotes angiogenesis and cerebral perfusion in experimental stroke. PloS One 2015;10:e0134543
- Miao J, Deng F, Zhang Y, et al. Exogenous human urinary kallidinogenase increases cerebral blood flow in patients with acute ischemic stroke. Neurosciences 2016;21:126
- Zhang C, Tao W, Liu M, et al. Efficacy and safety of human urinary kallidinogenase injection for acute ischemic stroke: a systematic review. J EvidBased Med 2012;5:31-9
- Liu GG, Wu H, Li M, et al. Chinese time trade-off values for EQ-5D health states. Value Health 2014;17:597-604
- Wilcoxon F. Individual comparisons by ranking methods. Biometr Bull 1945;1:80-3
- Mann HB, Whitney DR. On a test of whether one of two random variables is stochastically larger than the other. Ann Math Stat 1947;18:50-60
- Guo S, Fraser MW. Propensity score analysis: statistical methods and applications. Sage; Thousand Oaks, CA. 2010
- China Guidelines for Pharmacoeconomic Evaluations. 2011. https://www.ispor.org/PEguidelines/countrydet.asp?c=28&t=4
- Bertram MY, Lauer JA, De Joncheere K, et al. Cost-effectiveness thresholds: pros and cons. Bull WHO 2016;94:925
- Leech AA, Kim DD, Cohen JT, et al. Use and misuse of cost-effectiveness analysis thresholds in low- and middle-income countries: trends in cost-per-DALY studies. Value in Health. Elsevier Inc.; 2018. Available from: http://dx.doi.org/10.1016/j.jval.2017.12.016
- Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med 2000;19:1141-64
- Arbuthnott J. An argument for divine providence, taken from the constant regularity observ'd in the births of both sexes. By Dr. John Arbuthnott, Physitian in Ordinary to Her Majesty, and Fellow of the College of Physitians and the Royal Society. Phil Trans 1710;27:186-90
- Snedecor GW, Cochran WG. Statistical methods. 8th ed. Ames, IA: Iowa State University Press; 1989
- Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med 2001;33:344-9
- Kaplan RM. The minimally clinically important difference in generic utility-based measures. COPD 2005;2:91-7
- Luo N, Johnson JA, Coons SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care 2010;48:365-71
- Feeny D, Spritzer K, Hays RD, et al. Agreement about identifying patients who change over time: cautionary results in cataract and heart failure patients. Med Decis Making 2012;32:273-86
- Briggs A, Clark T, Wolstenholme J, et al. Missing…. presumed at random: cost‐analysis of incomplete data. Health Econ 2003;12:377-92