Abstract
Objectives: This study evaluated the frequency of hospital readmissions for venous thromboembolism (VTE) and the associated costs and length of stay (LOS) among acute medically ill patients in the US using a real-world claims database analysis.
Methods: Patients (≥40 years of age) at risk of VTE due to hospitalization for acute medical illnesses, based on primary hospital discharge diagnosis codes, were identified from the MarketScan databases between July 1, 2011 and March 31, 2015. Patients were required to have continuous insurance enrollment in the 6 months prior to initial (index) hospitalizations (baseline period) and in the 6 months after hospital discharge (follow-up period). The proportions of patients with VTE-related (diagnosis at any position) and VTE as primary diagnosis hospital readmissions during the follow-up period were evaluated. The associated costs and LOS for such readmissions were also determined, as well as time to VTE-related readmissions.
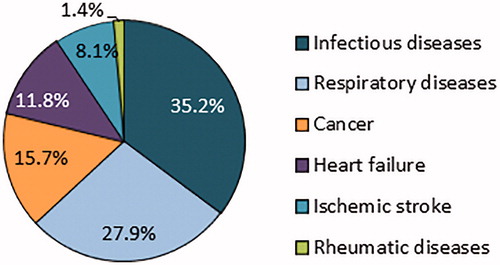
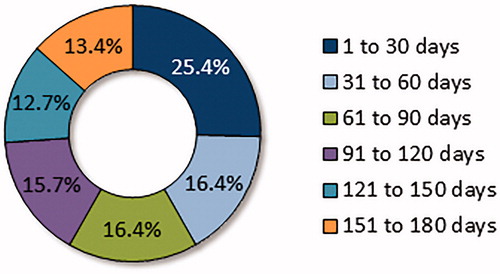
Results: Of the study population (n = 12,785; mean age = 68.3 years), most were hospitalized primarily for infectious diseases (35.2%), followed by respiratory diseases (27.9%), cancer (15.7%), heart failure (11.8%), ischemic stroke (8.1%), and rheumatic diseases (1.4%). Of the overall study population, 2.1% (n = 268) had a VTE-related hospital readmission in the 6 months following discharge of their index hospitalization, of which 36.6% (n = 98) were for a primary diagnosis of VTE. Approximately 25.4% of the VTE-related hospital readmissions occurred within the first 30 days of discharge and 58.2% within 90 days. The mean cost for a hospital readmission with a primary diagnosis of VTE was $18,681 (mean LOS = 5.0 days); for readmissions with a primary diagnosis of DVT and PE, mean costs were $14,719 and $23,305, respectively.
Conclusions: Among this study population of patients hospitalized for acute medical illnesses, some experienced a VTE event requiring re-hospitalization, with 25% occurring within the first 30 days after hospital discharge.
Introduction
Patients hospitalized for acute medical illnesses are at risk for venous thromboembolism (VTE), a leading cause of preventable morbidity and mortality among hospitalized patients in the USCitation1. Based on the American College of Chest Physicians (ACCP) 2012 criteria, greater than 7 million hospitalized patients with acute medical illnesses were at risk for VTE in the US in 2014Citation2,Citation3. Using data from the Rochester Epidemiology Project, Heit et al.Citation4 estimated ∼ 500,000 VTE events occur in the US annually; and 52% are related to recent hospitalization. Such a large clinical burden is reflected in the high healthcare costs of VTE, which in the US in 2014 USD were estimated to range between $13.5 and $27.2 billion for total hospital-acquired costsCitation5.
It is essential to understand the clinical and economic burden of VTE-related hospital readmissions among hospitalized acute medically ill patients, an area which is poorly explored and, thus, not well acknowledged. Furthermore, hospital readmissions are a significant concern in the US, with active programs (e.g. Centers for Medicare & Medicaid Services Readmissions Reduction Program) requiring reporting and instituting financial penalties, especially in the case of readmissions occurring within 30 days of hospitalization. Therefore, we evaluated the frequency of hospital readmissions for VTE, as well as the associated costs and lengths of stay and times to readmissions among patients recently hospitalized for acute medical illnesses in the US using a real-world claims database analysis.
Patients and methods
Study design
This study was a retrospective claims database analysis using the Truven Health MarketScan Commercial and Medicare Supplemental healthcare claims databases. These claims databases encompass > 130 million employees, spouses, and dependents located in all 10 US census regions. The claims data includes inpatient and outpatient information, reflecting real-world treatment patterns and costs. In compliance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA)Citation6, the databases consist of fully de-identified data sets, with synthetic identifiers applied to patient-level and provider-level data to protect the identities of both the patients and data contributors. This study was exempt from internal review board oversight in accordance with the Department of Health and Human Services Policy for Protection of Human Research Subjects (45 CFR §46.101(b)(4))Citation7.
Study population
Patients (≥ 40 years of age) at risk of VTE due to hospitalization for acute medical illnesses of cancer, heart failure, infectious diseases, ischemic stroke, respiratory diseases, and rheumatic diseasesCitation3, as the primary hospital discharge diagnosis, were identified from the Truven Health MarketScan Commercial and Medicare Supplemental healthcare claims databases between July 1, 2011 and March 31, 2015. Medical illnesses were identified by International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) codes. The acute medical illnesses evaluated were based on ACCP guidelinesCitation3 and other patient types in VTE clinical trialsCitation8,Citation9.
Index hospitalization was defined as the earliest hospitalization for acute medical illnesses to occur during the index identification period. Patients were required to have 6 months of continuous medical and prescription insurance coverage prior to the index hospitalization (baseline period). Patients were additionally required to have 6 months of continuous insurance coverage after the index admission discharge date (follow-up period). Patients were excluded if they had a pregnancy diagnosis during the baseline period or at the index hospitalization, death during the index hospitalization, or hip or knee replacement surgery during the index hospitalization.
Demographics and patient clinical characteristics
Patient demographics and clinical characteristics, including age, gender, US geographic region, health plan type, Charlson Comorbidity Index (CCI) score, and index hospital length of stay (LOS), were evaluated during the 6-month baseline period and index hospitalization for the overall study population.
VTE-related and VTE (primary diagnosis) hospital readmissions
The proportions of patients with VTE-related hospital readmissions (i.e. discharge ICD-9 code indicating VTE at any diagnosis position) and readmissions with VTE as the primary diagnosis were evaluated. The associated costs and LOSs for VTE-related and VTE (primary diagnosis) readmissions were also determined and are reported for any VTE, deep vein thrombosis (DVT), and pulmonary embolism (PE). The cost data evaluated in this analysis were obtained from claims within the MarketScan databases and reflect the final reimbursed amount of the healthcare claims (i.e. payment made by both the insurance companies and patients). Times to VTE-related readmission were additionally determined.
Statistical analyses
Descriptive statistics were utilized to summarize demographics, clinical characteristics, proportions of patients with VTE-related and VTE readmissions, costs and LOSs of readmissions, and times to readmissions. Potential predictors of any VTE readmissions (VTE-related and VTE − primary diagnosis) were evaluated in a generalized linear model (GLM). The covariates used in the GLM included acute medical illness type, age group, gender, geographical region, CCI score group, health plan type, index hospitalization VTE status, and index hospital LOS. All statistical analyses were carried out using SAS 9.4.
Results
Study population
shows the baseline demographics and clinical characteristics of the hospitalized population stratified by acute medical illness type. Among the overall study population (n = 12,785), most were hospitalized with a primary diagnosis for infectious diseases (35.2%, n = 4,500), followed by respiratory diseases (27.9%, n = 3,571), cancer (15.7%, n = 2,002), heart failure (11.8%, n = 1,507), ischemic stroke (8.1%, n = 1,030), and rheumatic diseases (1.4%, n = 175) (). The mean age of patients within the overall study population was 68.3 years, 44.3% were < 65 years of age, 51.6% were female, and the mean CCI score was 3.1 prior to the index hospitalization. For the overall population, the mean index hospitalization LOS was 5.2 days (standard deviation [SD] = 6.0 days).
Table 1. Demographics and clinical characteristics of hospitalized population: all and stratified by type of acute medical illness.
VTE-related and VTE (primary diagnosis) hospital readmissions
Of the overall study population, 2.1% (n = 268) had a VTE-related hospital readmission in the 6 months following discharge of their index hospitalization, of which 36.6% (n = 98) were for a primary diagnosis of VTE (). Patients initially hospitalized for cancer had the highest rate of VTE-related hospital readmission at 3.9% (n = 78), of which 51.3% were for a primary diagnosis of VTE (). Among patients initially hospitalized for infectious diseases, the rate of VTE-related hospital readmission was 2.0% (n = 88); for those hospitalized for heart failure it was 1.9% (n = 29); for those hospitalized for rheumatic diseases it was 1.7% (n = 3), for those hospitalized for respiratory diseases it was 1.6% (n = 56); and for those hospitalized for ischemic stroke it was 1.4% (n = 14) ().
Figure 2. Proportions of patients with VTE-related and VTE (primary diagnosis [Dx]) readmissions during the 6-month follow-up stratified by type of acute medical illness. Each full-length horizontal bar indicates the proportion of patients with VTE-related hospital readmissions; the green part of each bar depicts the proportion of readmissions that were associated with a primary Dx for VTE.
![Figure 2. Proportions of patients with VTE-related and VTE (primary diagnosis [Dx]) readmissions during the 6-month follow-up stratified by type of acute medical illness. Each full-length horizontal bar indicates the proportion of patients with VTE-related hospital readmissions; the green part of each bar depicts the proportion of readmissions that were associated with a primary Dx for VTE.](/cms/asset/e321ea05-8e1e-46cf-af4f-0b36adbb6530/ijme_a_1618862_f0002_c.jpg)
Costs and LOSs for VTE-related and VTE (primary diagnosis) hospital readmissions
For any VTE-related (VTE at any diagnosis position) hospital readmissions, the mean cost was $42,158 and mean LOS was 9.4 days per patient; for readmissions with a diagnosis of DVT at any diagnosis position, the mean cost was $40,994 and mean LOS was 10.4 days; for readmissions with a diagnosis of PE at any diagnosis position the mean cost was $49,877 and mean LOS was 8.0 days per patient ().
Table 2. Associated cost and LOS of VTE-related and VTE (primary diagnosis) hospital readmissions.
For readmissions with a primary diagnosis of any VTE, the mean cost for a hospital readmission was $18,681, and mean LOS was 5.0 days per patient; for readmissions with a primary diagnosis of DVT, the mean cost was $14,719 and mean LOS was 4.7 days; for readmission with a primary diagnosis of PE, the mean cost was $23,305 and mean LOS was 5.4 days per patient ().
Time to VTE-related hospital readmissions
shows the time to VTE-related hospital readmissions. Approximately 25.4% of the VTE-related hospital readmissions of the overall population occurred within the first 30 days of discharge and 58.2% within 90 days. The proportion of VTE-related readmissions that occurred within 30 days among patients initially hospitalized for cancer was 28.2%; for those hospitalized with infectious diseases it was 26.1%; for those hospitalized for heart failure it was 20.7%; for those hospitalized for rheumatic diseases it was 33.3%; for those hospitalized for respiratory diseases it was 19.6%; and for those hospitalized for ischemic stroke it was 35.7%.
Potential predictors of VTE-related and VTE (primary diagnosis) readmission
Patients who had a VTE during their index hospitalization had a nearly 5-fold increased risk of having any VTE readmission during the 6-month follow-up period compared to patients who did not have an index hospitalization VTE (odds ratio = 4.65, p < 0.001, ). Other potential predictors of any VTE readmission were an index hospitalization for rheumatic disease vs infectious disease, greater comorbidity and having a longer index hospitalization LOS ().
Table 3. Potential predictors of VTE-related and VTE (primary diagnosis) readmissions.
Discussion
In this nationally representative claims database analysis that included nearly 13,000 patients hospitalized for acute medical illnesses, 2.1% had a VTE-related hospital readmission within 6 months of initial hospitalization, of which 25% occurred within the first 30 days of discharge. Among the patients hospitalized for acute medical illnesses, the frequency of hospital readmission for VTE ranged from 1.4–3.9%; the highest rate was among patients hospitalized for cancer. Although the mean ages of study populations differed and acute medical illness distribution was somewhat different, the overall rate of VTE-related readmissions was relatively similar to the rate in our previous study of hospitalized acute medically ill patients (mean age = 58.4 years), which was 2.8%Citation10. The VTE event rate in our current study is also consistent with the earlier database claims analysis of 141,628 patients hospitalized for acute illnesses between 2005 and 2009 by Mahan et al.Citation11, in which the VTE event rate was 1.9% within 90 days post-discharge of index hospitalizations.
In this study, the average cost for hospital readmissions of patients with VTE as their primary diagnosis was $18,681. This cost is comparable to that in the study of Cohoon et al.Citation12, who reported that, compared to hospitalized control cases, medical costs within the first 3 months of hospitalization were increased by ∼ $17,000 (2011 USD) for patients who had a VTE event during or after a recent hospitalization. The hospitalization costs for VTE reported here are also consistent with the findings of Grosse et al.Citation13, who, after an analysis of several different studies, reported incremental direct medical costs ranging between $12,000–$15,000 (2014 USD) for treatment of acute VTE. These cost studies highlight the high inpatient costs associated with the treatment of VTE, and our most recent data suggest the inpatient costs for treating VTE may still be increasing.
Another recently conducted study points out the significant cost burden associated with readmission after discharge from an acute VTE hospitalization, especially among patients with serious comorbiditiesCitation14. Using data from the Nationwide Readmission Database, Secemsky et al.Citation14 identified 1,176,335 hospitalizations for acute VTE between January 1, 2010 and December 31, 2014; of the patients hospitalized for acute VTE, 6.2% died during hospitalization; of those who survived, 17.5% had another hospitalization (for any cause) within 30 days; of those with a readmission, 8.1% died. The median hospitalization cost for readmissions (all-cause) was $10,000. Hospital readmissions represent a significant area of focus for several regional and national organizations in the US, the national cost of which is noted in a study published in July 2017 by Strom et al.Citation15. In this study, which also used data from the Nationwide Readmission Database, between January 1, 2013 and November 31, 2013, 12,533,551 all-cause hospitalizations were identified, of which 14.5% were associated with readmission within 30 days, at a total cost of nearly 51 billion USD (Medicare 29.6 billion; non-Medicare: 21 billion)Citation15.
The substantial clinical and economic burden of VTE readmissions among patients hospitalized for acute medical illnesses reported in this study may help to increase the awareness of the need for improvement in VTE prophylaxis among this patient group, as well as highlight the need for better management practices of patients in the outpatient continuum of care. Such improvements may help reduce the burden of VTE readmissions. In our recent study of VTE prophylaxis patterns of 17,895 patients hospitalized for acute medical illnesses in the US, the findings were that nearly 60% did not receive any pharmacologic VTE prophylaxis, and only 7% received both inpatient and outpatient prophylaxisCitation10. Although not all hospitalized acutely medically ill patients may be at high risk for VTE based on the ACCP criteriaCitation3, the potential under treatment of such a patient population and the accompanying irresolution regarding who is at high risk for VTE requires attention. Towards these goals, there has been a proposal of new paradigms that involve an individualized and more patient-centered approach for the assessment of both VTE and bleeding riskCitation16. As of January 1, 2017, the Center for Medicare & Medicaid Services has mandated the use of standardized VTE Validated Risk Assessment Models (RAMs) during hospital admission to aid in the identification of acutely ill hospitalized patients who are at increased risk for VTE and would benefit most from VTE prophylaxisCitation16. As hospital stays in the US are decreasing in duration for patients hospitalized for acute medical illnesses, and there is a risk for readmission for VTE among this patient population, it has become increasingly critical to more fully implement timely individualized assessment of VTE risk during hospitalization, and also to provide a provider level assisted transition of care for patients to the outpatient setting.
Clinical evidence is still limited regarding extended VTE prophylaxis, but new treatment options are becoming available to specifically treat VTE among patients hospitalized for acute medical illnesses. In June 2017, the Food and Drug Administration approved betrixaban with extended duration prophylaxis for VTE prophylaxis in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications due to moderate or severe restricted mobility and other risk factors for VTE based on the results of the phase III multinational APEX trial (Acute Medically Ill VTE Prevention With Extended Duration Betrixaban Study)Citation8. The APEX trial showed that admission-to-home, extended-duration prophylaxis with betrixaban (up to 35–42 days) reduced VTE events among acutely ill hospitalized patients, without increasing the risk for major bleeding, compared with standard-duration (6–14 days) enoxaparinCitation8. As betrixaban is new to the US market, further study is needed to examine its efficacy and safety for VTE risk reduction among patients hospitalized for acute medical illness in the real-world setting. Updated clinical practice guidelines regarding extended VTE prophylaxis are needed, and, thus, more evidence is required.
Limitations
While many patients with VTE are increasingly being treated in the outpatient setting, this study focused on VTE hospitalizations and readmissions, since such events incur much higher healthcare costs and are of national concern. With this focus of the study, the overall healthcare cost burden associated with VTE recurrence is likely under-estimated, and future studies examining the increase of VTE treatment in the outpatient setting and the associated costs are warranted. The costs evaluated herein reflect the final payment amounts made by the insurance companies and patients for the healthcare services. Such paid amounts may not be entirely reflective of the actual costs incurred to hospitals or the hospital charged amount. However, since the paid amounts reflect the final transactions for the healthcare services, they are generally considered as the actual cost burden of the hospital medical services.
Retrospective claims database analyses have certain limitations. First, claims in the MarketScan databases are subject to coding errors, coding for the purpose of rule-out rather than actual disease, and under coding, either by the healthcare provider or due to limitations imposed by the database. Furthermore, ICD-9 codes may not always be indicative of actual VTE eventsCitation17, and, therefore, the VTE event rate reported in this study could have been over-estimated, as well as the costs for VTE. It has been observed in previous studies that most VTE events among patient populations similar as in this study occur within the first few months after hospital dischargeCitation10,Citation11. For this study, we used an extended follow-up of 6 months to capture as many VTE events as possible among the hospitalized study population. A follow-up period beyond this duration might be compromised by greater patient attrition due to the loss of patients without continuous insurance coverage and the data coverage in the database. We do acknowledge though that some patients have VTE events 1–2 years later after hospitalization, and further study of this patient group is warranted in future follow-up studies. The MarketScan databases may not be representative of the US population as a whole; for example, this study used claims data from MarketScan commercial and Medicare supplemental databases, which may not generalize to patients insured by Medicaid. Also, the majority of claims in the MarketScan databases are from patients located in the South Census region and, thus, may not account for regional differences in patient care. Despite the potential limitations, the MarketScan databases are robust in data, which likely represent real-world patterns associated with clinical practice.
Conclusion
Among this study population of patients hospitalized for acute medical illnesses, some (2.1%) of them experienced a VTE event requiring re-hospitalization, with 25% of the readmissions occurring within the first 30 days after hospital discharge.
Transparency
Declaration of funding
Sponsorship for this study and development of this manuscript were funded by Portola Pharmaceuticals.
Declaration of financial/other interests
AA is a research consultant and/or speaker for Novosys Health, Portola, Boehringer Ingelheim, Bristol-Myers Squibb, and Pfizer. AA did not receive funding for the development of this manuscript. SD is a consultant for Novosys Health. IB is an employee of Portola Pharmaceuticals. WRN was an employee of Portola Pharmaceuticals at the time of this study. JL, MLS, and BM are employees of Novosys Health, which has received research funds from Portola Pharmaceuticals in connection with conducting this study and development of this manuscript. A peer reviewer on this manuscript has disclosed being an advisory board member for Janssen Pharmaceuticals. The peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Acknowledgements
None reported.
References
- Cardoso L, Krokoscz D, Paiva E, et al. Results of a venous thromboembolism prophylaxis program for hospitalized patients. Vasc Health Risk Manag. 2016;12:491–496.
- Huang W, Cohen A, Zayaruzny M, et al. Impact of evolving ACCP guidelines on estimates of venous thromboembolism risk in US hospitals. International Society on Thrombosis and Haemostatsis (ISTH). July 8–13, 2017. Berlin Germany. Res Pract Thromb Haemost Suppl. 2017;S1:1–1451.
- Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e195S–e226S.
- Heit JA, Crusan DJ, Ashrani AA, et al. Effect of a near-universal hospitalization-based prophylaxis regimen on annual number of venous thromboembolism events in the US. Blood. 2017;130:109–114.
- Mahan CE, Borrego ME, Woersching AL, et al. Venous thromboembolism: annualised United States models for total, hospital-acquired and preventable costs utilising long-term attack rates. Thromb Haemost. 2012;108:291–302.
- US Department of Health & Human Services. The HIPAA privacy rule; December 28, 2000 [cited 2019, April 26]. Available from: https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
- US Department of Health & Human Services. 45 CFR 46; 1991 [cited 2019, April 26]. Available from: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html#subparta
- Cohen AT, Harrington RA, Goldhaber SZ, APEX Investigators, et al. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med. 2016;375:534–544.
- Cohen AT, Spiro TE, Buller HR, The MAGELLAN Investigators, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368:513–523.
- Amin A, Neuman WR, Lingohr-Smith M, et al. Venous thromboembolism prophylaxis and risk in the inpatient and outpatient continuum of care among hospitalized acutely ill patients in the US. Adv Ther. 2019;36:59–71.
- Mahan CE, Fisher MD, Mills RM, et al. Thromboprophylaxis patterns, risk factors, and outcomes of care in the medically ill patient population. Thromb Res. 2013;132:520–526.
- Cohoon KP, Leibson CL, Ransom JE, et al. Costs of venous thromboembolism associated with hospitalization for medical illness. Am J Manag Care. 2015;21:e255–e263.
- Grosse SD, Nelson RE, Nyarko KA, et al. The economic burden of incident venous thromboembolism in the United States: a review of estimated attributable healthcare costs. Thromb Res. 2016;137:3–10.
- Secemsky EA, Rosenfield K, Kennedy KF, et al. High burden of 30-day readmissions after acute venous thromboembolism in the United States. J Am Heart Assoc. 2018;7:e009047.
- Strom JB, Kramer DB, Wang W, et al. Short-term rehospitalization across the spectrum of age and insurance types in the United States. PLoS One. 2017;12:e0180767.
- Spyropoulos AC, Raskob GE. New paradigms in venous thromboprophylaxis of medically ill patients. Thromb Haemost. 2017;117:1662–1670.
- Lau BD, Haut ER, Hobson DB, et al. ICD-9 code-based venous thromboembolism performance targets fails to measure up. Am J Med Qual. 2016;31:448–453.