Abstract
Background: Procedural efficiencies can contribute to cost reductions in transcatheter aortic valve replacement procedures (TAVR). The objective of this study is to determine operating room (OR) variable cost per minute in endovascular TAVR procedures, in a real-world hospital setting.
Methods: Using Premier data from January 2015–June 2016 for patients undergoing a primary endovascular TAVR (primary ICD-9 code of 35.05, ICD-10 code of 02RF37Z, 02RF38Z, 02RF3JZ, or 02RF3KZ) procedure, the OR cost per minute was calculated for each patient by dividing the total hospital OR variable cost by the OR time (minutes).
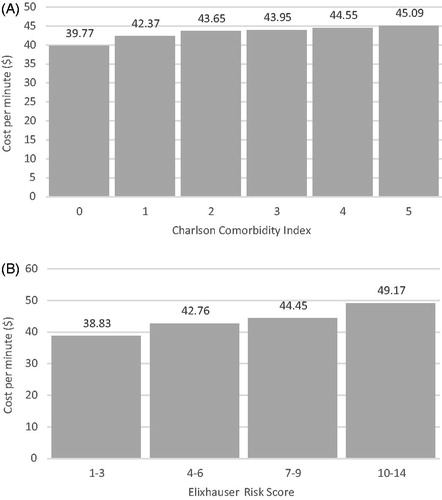
Results: Of the 4,573 patients in the cohort, the average age was 80 years, 77% were admitted electively, and the vast majority were discharged home with (30%) or without (45%) home care. Median OR time for endovascular TAVR procedures was 180 min. The trimmed mean OR cost per minute was $43.59 (SD = $28.68). When stratified by Elixhauser Risk score and Charlson comorbidity index, OR cost per minute increased with higher risk and comorbidity (p < 0.0001 and p < 0.041, respectively).
Conclusions: This contemporary estimate of the real-world variable OR cost per minute provides researchers with a critical parameter to refine economic models of TAVR and aid clinical program directors in resource planning according to a priori risk and comorbidity.
Introduction
Transcatheter aortic valve replacement (TAVR) has increasingly become the standard of care for treating patients with severe symptomatic aortic stenosis who are inoperable or considered intermediate or higher risk for conventional surgical replacement. In a recent US cost-effectiveness analysis of TAVR in intermediate risk patients, the estimated costs associated with index hospitalizations for TAVR procedures ranged from $54,256–$61,433, driven primarily by procedure costs, which are largely due to the cost of the valve itselfCitation1. However, as center experience increases and technologies evolve, procedural efficiencies can be expected to contribute to cost reductions during the index hospitalization; an important consideration in the current healthcare landscape of resource constriction. Herein, we explore the impact of operating room (OR) time and OR costs—two potentially modifiable components of the TAVR procedure—with the objective of determining the OR variable cost per minute for endovascular TAVR procedures in a real-world hospital setting.
Methods
We retrospectively examined Premier data from January 2015–June 2016 for patients undergoing a primary endovascular TAVR (primary ICD-9 code of 35.05, ICD-10 code of 02RF37Z, 02RF38Z, 02RF3JZ, or 02RF3KZ) in the US. The Premier Database (Premier Inc. Charlotte, NC) collects resource utilization during hospitalizations from more than 600 US hospitals, with day-by-day service level detail. The Premier database was ideally suited to the research question because of the availability of robust operating room time and cost data. OR cost per minute was calculated by dividing the total variable hospital OR cost (USD) by the OR time (minutes) during TAVR procedures. Outliers in the recorded data for OR time and cost were handled by trimming the OR cost per minute by 1% at both the upper and lower tails of the distribution. We subsequently stratified the variable OR cost per minute by the Charlson comorbidity indexCitation2 and the Elixhauser Risk scoreCitation3. Analysis of variance was performed to analyze OR cost per minute differences across risk scores. Sample selection and creation of analytic variables were performed using Instant Health Data (IHD) platform (BHE, Boston, MA). Statistical analyses were undertaken with R, version 3.2.1 (R Foundation for Statistical Computing, Vienna, Austria) and Microsoft Excel.
Results
The cohort included 4,573 patients. Baseline patient and facility characteristics are presented in . Nearly half of patients were female, with an average age of 80 years. 76.6% of admissions were elective, 7.0% were emergency, and 16.4% were considered urgent. The average Charlson comorbidity index was 2.73. The majority of patients (58.3%) were treated at a large (500+ beds) hospital, and the vast majority were discharged home (45.5%) or home with home care (30.4%). Other patients were discharged to a skilled nursing facility (15.1%) and inpatient rehabilitation (4.9%). A minority of patients (1.6%) were coded as discharged elsewhere, and 2.6% died in hospital. A little more than half of patients were treated in the South of the US (55.3%) with the balance of cases about equally distributed among the remaining regions (12.1% Midwest, 18.2% Northeast, and 14.5% West).
Table 1. Facility and patient characteristics for patients undergoing primary endovascular TAVR in Premier Database from January 2015 to June 2016.
Median OR time for endovascular TAVR procedures was 180 min (IQR = 150–238). The mean OR cost per minute was $43.59 (SD = $28.68) with a median cost per minute of $39.04 (IQR = $27.29–$51.34). When stratified by patient risk, OR cost per minute increased significantly with both the Elixhauser Risk Score (p < 0.0001) and Charlson Comorbidity Index (p < 0.041; ).
Discussion
Procedural costs are the main determinant of TAVR hospitalization costsCitation1. While most of the procedural costs are driven by the cost of the transcatheter valve, operating room expenses are one of the variable costs that can be potentially controlled through efficiencies and appropriate quality control. As TAVR programs gain experience, procedural efficiencies and improved outcomes may be predicted to reduce OR time or obviate the need for operating room time altogether in appropriately selected patients. The present analysis is significant in that it provides the most contemporary and generalizable detailed estimation of the real-world variable OR cost per minute in the US.
Moreover, we have shown for the first time that the variable OR cost per minute correlates positively with both patient comorbidity and a priori risk as measured by the Charlson Index and Elixhauser Score, suggesting that more complex patients not only contribute more OR time, but also more intensive resource utilization during that time.
The OR cost per minute is a critical parameter for both health economic researchers and hospital administrators allowing for refined predictions of cost-effectiveness and more effective resource planning. It can also be a useful consideration in terms of benchmarking TAVR program performance as the OR costs are likely impacted by both center experience and the quality of patient selection.
Transparency
Declaration of funding
This analysis was funded by Edwards Lifesciences.
Declaration of financial/other relationships
BJP has received research funding from Edwards Lifesciences and honoraria from Abbott and Boston Scientific. CAT is a full-time employee and shareholder of Edwards Lifesciences. The JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
None reported.
References
- Baron SJ, Wang K, House JA, et al. Cost-effectiveness of transcatheter vs. surgical aortic valve replacement in patients with severe aortic stenosis at intermediate risk: results from the PARTNER 2 trial. Circulation. 2018;139(7):877–888.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.