Abstract
Aims
There is wide variation in opioid prescribing patterns after common surgical procedures. This study examines outcomes for beneficiaries undergoing hospital outpatient department (HOPD) procedures using liposomal bupivacaine (LB) for control of post-surgical pain. As a non-opioid surgical analgesic, LB may afford beneficial outcomes for reducing subsequent opioid use and improving post-surgical service use outcomes.
Methods
This retrospective cohort comparison study analyzed 100% Medicare claims data from 2014–2019. HOPD claims were matched to approximately 100 of the most common surgical procedures where LB was utilized. Within these procedures, a one-to-many, with replacement propensity score matching model was used to control for possible selection bias. By procedure, those claims which were identified as using LB for control of post-surgical pain were matched to those not receiving LB. Outcomes were the probability of a subsequent Part D opioid prescription fill, emergency department (ED) visit, and short-term acute care hospital admission.
Results
Higher provider use rates of LB are significantly correlated with a decrease in post-HOPD opioid use and a reduction in post-operative ED visits. For each 10% increase in LB use rate by a given provider, Part D opioid events by Day 30 decreased by 2.6 percentage points and by 2.1 percentage points by day 90 (p < .01). Similarly, for each 10% increase in provider LB use rate, there is a 0.4 percentage point reduction in post-operative ED use by day 30 (p < .01) and a 0.3 percentage point reduction by day 90 (p < .05).
Limitations
Part D data only indicate that a prescription was filled, not whether the drug was taken.
Conclusions
Increased provider use of LB is correlated with improved patient outcomes in real-world provider experience with the Medicare population for many outpatient procedures. Policies that support increased provider use of LB should reduce reliance on opioid drugs for post-surgical pain management.
Introduction
Opioids have been shown to be extremely addictive, and since the mid-1990s, opioid abuse has been a national public health crisis in the United States. This crisis has intensified under the COVID-19 public health emergency (PHE)Citation1. Statistics underscore the severity of the current epidemic, with the National Institute on Drug Abuse reporting that, in 2018, more than 2 million Americans abused opioids. Opioids were involved in 46,802 overdose deaths that year, or 69.5% of all drug overdose deathsCitation2.
Currently, there is substantial variation in opioid prescribing patterns after common surgical proceduresCitation3. Prolonged opioid use (defined as continuing to fill an opioid prescription 90-180 days after outpatient surgery) affects anywhere from 3 percent to 10 percent of post-surgical patients depending upon the procedure, and it comprises a continuing, if not increasing, public health concernCitation4,Citation5. Although there have been declines in morbidity and mortality following most surgical procedures over the last decade, some researchers maintain that prolonged use of opioids following surgery might be seen as an under-recognized surgical complicationCitation6. For many patients who subsequently develop an opioid use disorder (OUD), outpatient surgery may have first introduced them to opioids, and they may have continued using these drugs long after their surgeriesCitation7.
One way to combat this growing crisis in the prolonged use of opioids following surgery could be to increase the utilization of non-opioid treatments for post-surgical pain management. In 2011, the Food and Drug Administration (FDA) approved the use of liposomal bupivacaine (LB; [bupivacaine liposome injectable suspension], Pacira BioSciences, Inc., Parsippany, NJ) to provide post-surgical analgesia. LB is a non-opioid nerve blocker and is administered at the surgical site to produce postsurgical analgesia.Footnotei Prior randomized, controlled studies have shown that LB can both reduce the use of opioids in post-surgical pain managementCitation8 and provide beneficial post-surgical service outcomes, including reduced postsurgical pain, reduced opioid consumption, and increased numbers of patients with an opioid-free recoveryCitation9,Citation10. In recognition of these results and to support the continued use of non-opioid alternatives, starting in 2019, the Centers for Medicare and Medicaid Services (CMS) authorized separate Medicare payments for LB when used in ambulatory service centers (ASCs). In contrast, Medicare payment for LB when used in the hospital outpatient department (HOPD) is packaged within the ambulatory payment classification (APC) bundle and is not paid separatelyCitationii.
This retrospective cohort comparison study of Medicare claims data sought to better understand the real-world impact of LB use and provider experience with LB on outcomes of postsurgical events associated with common outpatient surgical procedures performed in the HOPD setting. The Medicare claims data provide a very large sample from which inferences can be drawn on the effectiveness of LB to reduce post-surgical opioid use. The claims data also provide a comprehensive universe of providers and their usage of LB, especially in the Medicare population. Small sample size (e.g. public availability of only 5% of total Medicare physician claims heretofore and clinical trials with smaller study groups) has been a limitation in some prior studies of the effects of LB on post-surgical outcomes.
Methods
Data: Data for this study were extracted from the 100% Research Identifiable File Medicare Fee for Service (FFS) claims data and beneficiary summary files under CMS Data Use Agreement (DUA) 54757. Cases were identified as those Medicare claims for procedures occurring in the HOPD from 2014 through 2019, and where at least one revenue center line procedure code matched to a list of the 102 HOPD surgical procedures in which LB is most frequently administered (by claim volume). This requirement enabled the capture of most HOPD claims reporting LB (about 75% of all HOPD LB claims), as well as the universe of Medicare HOPD claims for the selected procedures in which LB was not used. The 102 most common procedures utilizing LB were obtained from a tabulation of the procedures within the HOPD claims data from 2017 to determine those most frequent procedures (listed in Appendix). Because total knee arthroplasty (TKA) was the most frequent procedure in our data in 2018 and 2019, we created a TKA subgroup of cases in which a TKA procedure was performed (Current Procedural Terminology code 27447).
Cases were included in the main study group if 1) there was a claim for an included HOPD procedure from 2014 through 2019, 2) the beneficiary was enrolled in Medicare Fee for Service (FFS) (and not Medicare Advantage) for their risk and outcome measurement period pre- and post-HOPD surgery, and 3) they did not have a previous HOPD surgery in the 90 days preceding (if a beneficiary had multiple qualifying surgeries, only the first qualifying surgery was used). The Medicare FFS beneficiary summary and claims data allow for the construction of a variety of measures to indicate enrollment, entitlement, demographic characteristics, and patient complexity. These measures were used to compare similar surgical patients and procedures which did and did not utilize LB for post-surgical pain control.
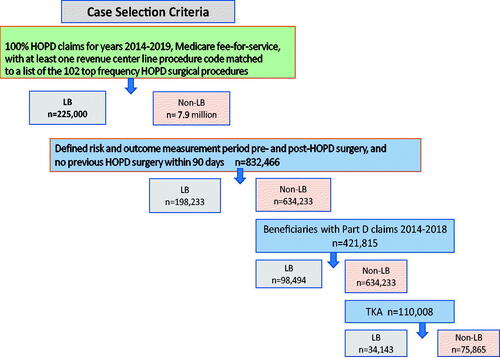
To measure post-surgical opioid prescription use, Medicare Part D data were analyzed. These data were available for claims paid by Medicare from 2014 through 2018 for roughly 75% of the Medicare beneficiary population who were enrolled in Part D. These specific analyses were limited to Part D enrollees such that sufficient enrollment time was available to measure risk and use both before and following an HOPD surgery. Only those beneficiaries with a 90-day pre-period enrollment in Part D and a 180-day post-period enrollment in Part D (or until time of death) for related measures were included. See which shows the case selection criteria.
To identify if a beneficiary had or developed an opioid use disorder (OUD), Chronic Condition Warehouse (CCW) data were utilized. The CCW contains flags which capture the initial instance of a diagnosis indicating OUD, hospitalization for an OUD event, or a prescription for Medication-Assisted Treatment of OUD. These OUD algorithms were developed by the Centers for Medicare and Medicaid Services (CMS) CCW using administrative claims data. This algorithm is included in the Appendix.
Addressing potential selection bias
To address potential selection bias, a sample of cases with and without LB was extracted and matched using propensity score matching techniques. Potential matching covariates related to patient and HOPD surgery characteristics were extracted from the Medicare FFS data (see below). These characteristics are: 1) beneficiary age at the time of surgery, 2) whether they had an inpatient hospital discharge in the 30 days prior to HOPD surgical event, 3) whether they resided in a rural area, 4) beneficiary count of chronic conditions, 5) gender, 6) enrolled with end-stage renal disease (ESRD), 7) dually Medicare and Medicaid enrolled, 8) disabled, 9) White, 10) Black, 11) Asian, 12) Other (Hispanic was the omitted reference category), 13) history of Alzheimer’s and/or dementia, 14) depression, 15) the total claim expenditures of the HOPD surgical event, 16) whether fentanyl was used during the HOPD event, and 17) the provider LB use rate (regardless of whether LB was used in the case). These characteristics following cleaning procedures and a 4-to-1 matching approach described further below are presented in in the Results section.
Table 2. Pre-cleaning, pre-match study database characteristics for TKA and all cases, in total, with LB, and without LB.
The use of LB as a component of the surgical recovery is determined in part by the provider’s assessment of the clinical severity of the case. To account for this case selection, we measured 1) the count of chronic conditions, 2) the HOPD surgical event Medicare Part A and B claim expenditures, and a variable showing whether there was a short-term acute care hospital (STACH) stay within the thirty days before the procedure. It may be that increases in these three variables might indicate that a given case could present as more severe to a provider and thus may influence the type of post-surgical pain management selected by the provider. Provider use rate was constructed as a proxy for hospital experience with LB. This was accomplished by dividing the total number of cases for which an outpatient department provider prescribed LB for post-surgical pain control by the provider’s HOPD surgical patient caseload or panel (then multiplying by 100).
To determine which, if any, of these covariates should be retained, a stepwise logit model was estimated. Only those variables which obtained a coefficient estimate significantly different from zero at the twenty percent level were retained for inclusion in the matching model. The logit estimation results indicated that all variables were predictors of LB utilization and thus all of these variables were used in matching the two cohorts.
To severity-match cases receiving LB to those which did not, a propensity score one-to-many optimal matching model, with replacement, was employed. Each case receiving LB could be matched with up to four non-LB comparison cases. On average, there were 3.2 non-treated comparison cases matched to each case for which LB was utilized. Overall, the two-sample groups were balanced in terms of the predictor variables, with the two exceptions being initial event spending and provider use rate. Only for these two variables did the matching model fail to reduce the absolute value of the standardized mean difference to a value of less than 0.10. The adoption of both replacement and use of multiple matching cases allows for a richer and more consistent sample upon which the subsequent analytical analyses would be conducted (regression, stage 1).
Constructing provider LB use rate
Usage of LB for post-surgical pain control varies significantly across providers. Nearly 75% of providers utilize LB minimally (i.e. had fewer than 11 LB claims in the six years). Even among those providers who use a non-negligible amount of LB, the use rate can vary substantially. shows the distribution of LB usage for all providers and for providers for whom at least eleven claims (due to HIPAA compliance) indicate the utilization of LB.
Table 1. Distribution of provider LB use rate among providers in study.
Outcome measures
Outcome measures were constructed using claims data for included cases in the 30, 90, and 180 days following hospital outpatient department (HOPD) surgery. The three outcome measures included are 1) likelihood of a Part D Opioid Event (beneficiary claim for a Part D opioid prescription fill), 2) likelihood of emergency department (ED) use, and 3) likelihood of a short-term acute care hospital (STACH) admission.
Analysis
Once the “balanced” (matched) sample was extracted, a logit regression model, with results being displayed as marginal effects was adopted for dependent variables (i.e. Part D opioid prescription fills, ED visits, and short-term acute care hospital (STACH) admissions at 30-, 90-, and 180-days following HOPD discharge). The interpretation of the derived coefficient estimates is as follows: the coefficient estimate represents the change in the dependent variable (outcome) as the predictor variable increases by one unit. These marginal or incremental effects represent the change in the probability, in percentage point terms, of observing the outcome variable as the predictor variable changes by one percentage point (often displayed as 10 percentage points for ease of interpretation).
Results
Pre-cleaning, pre-match patient database characteristics follow in . Patients with TKA (overall, with LB use and without LB use during HOPD surgical event) are shown in the left columns with the full set of cases shown right. LB was used in about 22% of cases with TKA but only about 3% of cases with any of the 102 included procedures (including TKA).
shows post-cleaning, post-match database characteristics for the remaining cases. As described above, cleaning procedures removed cases with insufficient enrollment or eligibility to conduct risk and outcome measurements of interest or if they had multiple qualifying HOPD surgical events with overlapping measurement periods (if so, the first case was kept). The 4-to-1 matching procedure also removed cases, particularly in the all cases-no LB (comparison) group.
Table 3. Post-match study database characteristics for TKA and all cases, in total, with LB, and without LB.
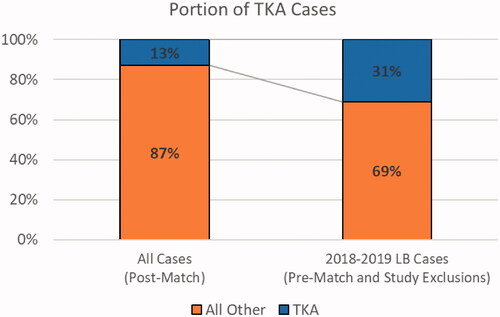
Total Knee Arthroplasty (TKA) became fully eligible for Medicare payment in the HOPD setting in 2018 and has since become the single most frequent procedure for LB use in this setting among Medicare beneficiaries. The Medicare claims data used in this analysis run from 2014 through 2019, and only include Part D opioid prescription data through 2018 due to data lag. Given that TKA was not fully eligible for Medicare payment before 2018, it is underrepresented in the main group findings relative to current practice. Overall, TKA represents 13% of HOPD cases in the dataset (2014 to 2019), but 31% of cases with an LB use in 2018 and 2019 (see ). Due to the increasing importance of LB as a non-opioid analgesic and the impact of opioid addiction on future policy, we first focus on those claims arising from a TKA.
In , the first column presents the outcome predicted by the model: post-HOPD Part D opioid prescription fill, ED use, and STACH admission. The next column (2) indicates the average frequency of each outcome within the TKA subgroup (e.g. 85% of included TKA cases had a Part D opioid event by day 30). The average marginal effects are presented in columns 3 and 4 in lieu of the coefficient estimate for these measures. Coefficient estimates represent the change in the log odds ratio associated with changes in the independent variable and not changes in the actual probabilities of observing these events. Marginal effects, instead of an odds ratio, are provided as they can provide a more meaningful assessment of a characteristic’s impact on an outcome. Marginal effects are the actual percentage point change associated with possessing a characteristic, ceteris paribus.
Table 4. Select multivariate estimates for case-level LB and provider LB use rate on outcomes for patients with a TKA.
All matching covariates and year dummy variables were applied in the regression analysis to control for effects not addressed by the matching process. The matching process estimates the probability of receiving LB based upon the totality of a vector of characteristics, even if differences remain between the two groups in the values of specific covariates. Thus, it is imperative to nevertheless control for these unique effects possessed by the individual covariates in the subsequent estimation models following initial matching procedures.
Examining first the likelihood of a patient having a post-surgical opioid prescription fill by Day 30, a highly significant estimated marginal effect is shown for the provider LB use rate in column (3). For those patients whose surgery occurred with a provider having an LB use rate 10 percentage points higher than the average use rate, a 2.6 percentage point reduction in the likelihood of filling an opioid prescription (Part D event) in the 30 days post-HOPD event is predicted and is statistically significant at the 0.01 level. Statistically significant reductions in post-HOPD opioid events are also observed at 90 and 180 days for providers with increased rates of LB use (–2.1% and −1.9%, both at p < .01). Consistent reductions are also seen in the 30 and 90 days post-HOPD ED visits (p < .01 and p < .05, respectively).
Here, case-level use of LB (dichotomous variable) for post-surgical pain control does not hold significant predictive power. Nonsignificant results were obtained for the likelihood of a patient receiving an opioid prescription 30, 90, and 180 d subsequent to the TKA procedure. The marginal effects estimated for the change in the probability of observing a post-surgical ED use 30, 90, and 180 d after a TKA procedure when a patient is prescribed LB is also nonsignificant, and largely not different from zero (column 4). In the case of observing a STACH admission 90 and 180 d after the surgery, it appears that prescribing LB results in a statistically significant reduction in post-HOPD acute admission (p < .05).
Given the above-noted variation in LB utilization by providers, some additional context is needed. indicates that the level of effect we typically see from provider LB use rate occurs at a discernible effect size in the fourth quartile of LB use (75th percentile and above). For instance, at the 95th percentile in , which shows a provider LB use rate of 21.0%, we would expect a 5.5 percentage point reduction in patients’ Part D opioid events at post-surgical Day 30 (i.e. 21% use rate multiplied by 2.6 percentage points per 10 points of difference (21*2.6/10 = 5.5)).
shows outcome measures and their average values in the left two columns. The remaining columns show the percentage point change expected if the case received LB (dichotomous variable = 1) and the provider LB use varied by a reasonable degree (see ).
Table 5. Linear interpolation of LB use and provider use rate, TKA cases.
This table directly demonstrates the relationship between LB use (a dichotomous variable) marginal effects and provider LB use rate (a continuous variable). Applying this within a marginal effects framework allows the reader to see changes to these variables (while holding all others constant) in order to isolate the effects of interest.
For example, the first row of below indicates that, on average, 85% of the TKA cases with sufficient Part D coverage in the dataset had a Part D opioid prescription fill by Day 30 following the HOPD surgical event (column 2). When LB was applied by a provider not experienced with its use (provider LB use rate was negligible, column 3), one could expect no change in the likelihood of a Part D opioid fill by Day 30 (i.e. average value, column 3 is 0.0). If instead, the case received LB and the provider had an average LB use rate (6.7%, column 4), one would predict a 1.7 percentage point decrease in the average value of a Part D opioid fill by Day 30 (row 1, column 4), reducing the estimated likelihood of a Part D opioid fill from 85% to 83.3%. Similarly, a highly experienced provider with a high LB use rate (95th percentile, column 6), accrues large improvements in patient outcomes and would be predicted to have a 5.3 percentage point decrease in the estimated likelihood of a Part D opioid fill by Day 30 (a reduction from 85% to 79.7%).
These findings hold in the general study population as well (subsequent table not shown), noting that effects of LB are more often significant and negative, or of a small magnitude. Non-significant case-level LB use findings are generally counteracted by statistically significant positive findings of a higher magnitude with increased provider LB use rate.
As was shown in , below presents the predicted outcome in the first column for all included patients for the top 102 LB procedures, not only TKA patients. The second column presents the average value observed for the outcome. The third column presents the estimated average marginal effects obtained from the logistic regression estimation. These marginal effects represent the change in the likelihood of observing the outcome in column 1 for a ten-point increase in the provider LB use rate, holding all other characteristics constant. For patient post-surgical LB use, see column 4, where the estimated marginal effects are reported. As was the case with the TKA analyses, all seventeen matching covariates, dummy variables for a surgical year, and dummy variables for procedure codes were included as control variables.
Table 6. Select multivariate estimates for case-level LB and provider LB use rates on select outcomes for all included patients.
LB utilization at the case level observed across providers with highly variable LB experience over six years () is associated with a slightly higher likelihood of a Part D opioid fill, ED use, and STACH use. This effect is counteracted by increases in the provider LB use rate. In other words, with a greater provider LB use rate, one expects better outcomes for all patients.
Once again, a greater provider LB use rate is shown to be correlated with improved patient outcomes. Using the full range of provider LB use rates, a linear interpolation of the sometimes countering, sometimes additive effects of case-level LB utilization in and provider LB use rate are shown. Interpolation findings for the main group are broadly consistent with the TKA subgroup shown in .
For example, among patients with an included case, on average, 75.9% are expected to have a Part D opioid fill in the 30 d following the HOPD event. If one patient from 2014 through 2019 received LB for post-surgical pain control, it is generally expected that they would have a 0.6 percentage point increase in the likelihood of having a Part D opioid fill in the same period. However, if the patient was treated at a provider that had an overall LB use rate of 10% (at about the 75th percentile, ), one would expect a 1.0 percentage point reduction in the likelihood of a Part D opioid fill by Day 30, resulting in a lower net average value of 75.5% (sum of columns 2, 3, and 4).
Also examined were OUD incidence and mortality, but these events were relatively rare following HOPD surgery and did not yield significant results.
Discussion
The effects of increasing provider LB use rates indicate that LB is an important tool for providers committed to using non-opioid pain management options for improving postsurgical patient outcomes. Greater provider LB use rate is strongly associated with a reduction in undesired outcomes in both the TKA group and the main procedure group. Although case-level LB use is associated with unfavorable outcome impacts in the main procedures group, this association was offset and reversed by increasing provider LB use rate, which yields net cross-cohort reductions in undesired outcomes.
Current utilization trends suggest that a 9% LB use rate (the 75th percentile of provider LB use) is the inflection point in the all-procedure models, where any minimal disadvantage that appeared with a case-level use of LB is overcome by the provider LB use effect. (See above). Given that the 75th percentile of provider LB use rate remains modest at approximately 9% of eligible procedures (See above), there remains a significant opportunity to increase provider use rates of LB to accrue substantial favorable patient outcomes, such as reduced opioid use, reduced ED visits, and reduced STACH admissions.
Consistent with prospective clinical investigations that found the use of LB resulted in clinically meaningful improvements in patient outcomes and opioid avoidanceCitation10, the findings of this methodologically distinct, retrospective claims-based cohort comparison of Medicare patients found that higher rates of LB use are correlated with a meaningful reduction in adverse outcomes – most notably reduction of post-operative Part D opioid events.
It is important to recognize that patients who receive LB have potentially significant real-world differences from their non-LB counterparts, many of which were addressed in the matching procedures. Regardless, patient access to LB as a safe, effective, and clinically meaningful opioid alternative is ultimately determined by provider choice, access, and experience.
Access to LB is not distributed equally among providers. Many life-altering chronic conditions and indicators of potentially poor access to care result in disproportionally lower access to LB as shown in . For example, dual Medicare-Medicaid enrollees (14.1% LB vs. 19.5% not), persons with disabilities (13.9% LB vs. 18.5% not), and persons with greater burden of chronic conditions, recent hospital discharge or prior opioid use disorder were all less likely to receive LB and therefore less likely to achieve the improved health outcomes discussed above. This may be due to a combination of economic barriers to access, such as for beneficiaries served by safety-net hospitals, as well as potentially risk-based patient selection by providersCitation11,Citation12.
Higher LB use rates may be indicative of adherence to Enhanced Recovery Pathways, which emphasize the use of opioid alternatives and have been shown to yield positive results for multiple surgical typesCitation13,Citation14. Postoperative Enhanced Recovery Pathway adherence has been shown to be lower than pre- and intraoperative periods when components are administered passivelyCitation15–17. This may support further advantage to a long-acting local analgesic that is administered during surgery and can provide prolonged coverage in the postoperative period when adherence to multimodal analgesics may be less reliable.
Overall, we generally found positive outcomes among LB beneficiaries in descriptive statistics that yielded a more nuanced finding in regression-adjusted effects. Given higher provider, LB use rates are correlated with improved outcomes, a policy of increasing provider access to LB relatively rapidly through providing separate payment for LB may accelerate accrual of patient benefits and be more equitable than a slower expansion from retaining LB in the bundled APC payment, as is current Medicare policy. Increased LB use could effectively address access equity issues that may be detrimental to achieving high-quality postsurgical outcomes and reduce long-term systemic costs associated with opioid useCitation18.
Additional research is needed to further explore both the effect of LB on specific procedure subgroups within the Medicare HOPD surgery population and to further analyze the impact of LB use on Medicare expenditures and long-term cost offsets. This study examined additional Medicare beneficiary subgroups (i.e. opioid naïve patients) and found that LB may be useful in maintaining opioid naivete after outpatient surgery as well as other outcomes, however, inter-procedure differences explained much of the observed variance. Finally, future research could examine the characteristics of prescribers who use LB at a higher-than-average level.
Limitations
The use of LB as a component of surgical recovery is largely a decision made by the provider and influenced by payors’ coverage and payment rules, including those of the Medicare program. Provider experience with LB, as well as available supply purchased by the hospital, are also determinants of LB use.
This study used administrative claims data to identify cases as well as to assess patient risk and service use outcomes. Inherently, these data limited the observable outcomes (e.g. precluding patient quality of recovery and pain). As outcomes were measured through observed interactions of the patient and the healthcare system, this also limits our inferences. For example, Part D opioid events are prescriptions filled by the beneficiary; we cannot know if the full script was taken as directed, taken at all, or otherwise diverted. However, administrative claims did enable a very robust sample size and have led to an analysis of LB as practically applied in the Medicare population.
Conclusions
From this retrospective cohort comparison study of Medicare claims data, we conclude that increased provider use of LB is correlated with improved patient outcomes. Patient outcomes from LB use itself are sometimes directionally opposite to the outcome effects among patients of providers with high use rates of LB (meaning that patients receiving LB from providers with low LB utilization rates did not realize improved outcomes). However, desirable patient outcomes are strongly correlated with increasing provider LB use rate and result in aggregate positive outcomes for all patients.
This finding suggests that LB is an important tool for providers committed to improving patient outcomes and that providers with low LB use rates are not realizing the full potential of improved patient outcomes that increased use of LB confers. Because increased provider use of LB is associated with more positive patient outcomes, policies that support increased provider use rates of LB by facilitating provider access to and experience with LB consequentially reducing reliance on opioid drugs and should be encouraged.
Transparency
Declaration of funding
This study was funded by Pacira BioSciences, Inc. Pacira BioSciences, Inc. and contractors participated in the study conception, design, analysis and interpretation, as well as review of the manuscript. Authors alone were responsible for the review and final approval of the submission to the journal.
Declaration of financial interests
No potential conflict of interest was reported by the author.
Peer reviewers on this manuscript have received an honorarium from JME for their review work but have no other relevant financial relationships to disclose.
Author contributions
All co-authors made significant contributions to the conception, study design, execution, acquisition of data, analysis and interpretation. All authors worked on drafting and/or writing the manuscript, substantially revised and/or critically reviewed the article and have agreed on the journal to which the article will be submitted. All authors have reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage, and agree to take responsibility and be accountable for the contents of the article. Finally, all authors share the responsibility to resolve any questions raised about the accuracy or integrity of the published work.
Supplemental Material: Appendix 1
Download PDF (132.6 KB)Supplemental Material: Appendix 2
Download PDF (127.4 KB)Acknowledgements
The authors wish to acknowledge the work of Sung Kim for extensive claims programing and Stephanie Demian for research support work on this project.
Notes
i LB is indicated: 1) In patients aged 6 years and older for single-dose infiltration to produce postsurgical local analgesia, and 2) In adults as an interscalene brachial plexus nerve block to produce postsurgical regional analgesia. Local Analgesia via Infiltration Dosing in Adults: The recommended dose of LB for local infiltration in adults is up to a maximum dose of 266 mg (20 mL), and it is based on the following factors: 1) Size of the surgical site, 2) Volume required to cover the area, and 3) individual patient factors that may impact the safety of an amide local anesthetic. No overall differences in safety or effectiveness were observed between patients aged 65 and over and younger patients. Clinical experience with LB has not identified. differences in efficacy or safety between elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/022496s035lbl.pdf
ii See 83 Fed. Reg. 37051 (“For CY 2019, in response to the recommendations from the President’s Commission on Combating Drug Addiction and the Opioid Crisis, we are proposing to change the packaging policy for certain drugs when administered in the ASC setting and provide separate payment for non-opioid pain management drugs that function as a supply when used in a surgical procedure when the procedure is performed in an ASC.”); 83 Fed. Reg. 58854-58857.
References
- Slavova S, Rock P, Bush HM, et al. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176.
- Opioid Overdoses: Drug Overdose Deaths. 2020.. In Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/drugoverdose/data/statedeaths.html
- Hill MV, McMahon ML, Stucke RS, et al. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–714.
- Brummett CM, Waljee J, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504.
- Clark H, Soneji N, Ko DT, et al. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251.
- Wright EA, Katz JN, Abrams S, et al. Trends in prescription of opioids from 2003–2009 in persons with knee osteoarthritis. Arthritis Care Res. 2014;66(10):1489–1495.
- Brummett CM, England C, Evans-Shields J, et al. Health care burden associated with outpatient opioid use following inpatient or outpatient surgery. JMCP. 2019;25(9):973–983.
- Asche CV, Dagenais A, Kang A, et al. Impact of liposomal bupivacaine on opioid use, hospital length of stay, discharge status, and hospitalization costs in patients undergoing total hip arthroplasty. J Med Econ. 2019;22(12):1253–1260.
- Asche CV, Dagenais A, Kang A, et al. Impact of treatment with liposomal bupivacaine on hospital costs, length of stay, and discharge status in patients undergoing total knee arthroplasty at high-use institutions. J Med Econ. 2019;22(1):85–94.
- Mont MA, Beaver WB, Dysart SH, et al. Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: results of a randomized controlled trial. J Arthroplasty. 2018;33(1):90–96.
- Suskind AM, Zhang Y, Dunn RL, et al. Understanding the diffusion of ambulatory surgery centers. Surg Innov. 2015;22(3):257–265.
- 2019 National Healthcare Quality and Disparities Report. (2021). In Agency for Healthcare Research and Quality. Available from: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html
- ERAS Compliance Group. The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg. 2015;261:1153–1159.
- Messenger DE, Curtis NJ, Jones A, et al. Factors predicting outcome from enhanced recovery programmes in laparoscopic colorectal surgery: a systematic review. Surg Endosc. 2017;31(5):2050–2071.
- Ahmed J, Khan S, Lim M, et al. Enhanced recovery after surgery protocols – compliance and variations in practice during routine colorectal surgery. Colorectal Dis. 2012;14(9):1045–1051.
- Feroci F, Lenzi E, Baraghini M, et al. Fast-track surgery in real life: how patient factors influence outcomes and compliance with an enhanced recovery clinical pathway after colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2013;23(3):259–265.
- Thorn CC, White I, Burch J, et al. Active and passive compliance in an enhanced recovery programme. Int J Colorectal Dis. 2016;31(7):1329–1339.
- McNeil BJ. Shattuck lecture-hidden barriers to improvement in the quality of care. N Engl J Med. 2001;345(22):1612–1620.