Abstract
Background
Influenza is a common cause of acute respiratory infection that leads to exacerbation of underlying chronic obstructive pulmonary disease (COPD). To elucidate the short- and long-term effects of influenza in patients with COPD, we examined health care resource utilization (HRU) and costs up to 13 months following influenza infection.
Methods
We conducted a retrospective cohort study using U.S. insurance claims data from MarketScan. Patients with an influenza diagnosis during the 2012–2014 influenza seasons and continuous enrollment in a health plan from 12 months before to 13 months after the index influenza diagnosis were identified and propensity score–matched 1:5 to controls without evidence of influenza. COPD- and pneumonia-related outcomes were assessed over 13 months following influenza diagnosis.
Results
COPD-associated outcomes after diagnosis were significantly worse in patients with influenza (n = 7,087) vs. controls (n = 35,435) during the first month (exacerbation: 16.1 vs. 3.4%; outpatient visits: 57.1 vs. 35.2%; emergency department (ED) visits: 10.5 vs. 1.8%; and inpatient visits: 5.6 vs. 0.7%) and months 2–13 (exacerbation: 25.1 vs. 21.1%; outpatient visits: 86.1 vs. 85.8%; ED visits: 20.0 vs. 15.7%; and inpatient visits: 6.5 vs. 5.3%). COPD- and pneumonia-associated costs for months 1 and 2–13 were higher in patients with influenza.
Limitations
The study was subject to a residual imbalance between cohorts despite propensity score matching. The use of diagnostic codes to select patients and identify complications could introduce inaccuracies in estimating events.
Conclusions
HRU and costs were higher in COPD patients with influenza during the first month and over the entire year following infection. This suggests influenza has an impact on respiratory health in patients with COPD that lasts beyond the acute infection.
Introduction
Influenza is a significant contributor to morbidity, mortality, and health care expenditures in the United States. Although the acute infection is generally self-limited, the preliminary burden of illness estimates for the 2019–2020 influenza season from the Centers for Disease Control and Prevention (CDC) show that influenza was responsible for 16.1 million excess outpatient visits, 380,209 excess hospitalizations, and 20,342 deathsCitation1. Among adults hospitalized for influenza, >90% have an underlying medical condition that increases the risk for complications, and 30% of these patients have chronic lung diseaseCitation2.
As reported in the Global Burden of Disease Study, chronic obstructive pulmonary disease (COPD) affected 24 million people in the United States and was the third leading cause of morbidity and mortality between 1990 and 2016Citation3. Patients with COPD, even those whose symptoms are stable, may experience exacerbations that manifest as episodes of worsening symptoms due to airflow obstruction resulting from airway inflammation, mucus hypersecretion, mucosal swelling, and bronchospasm. Exacerbations lead to accelerated loss of lung function and are associated with increased mortality and hospitalization, lower quality of life, and higher health care costsCitation4–9.
Respiratory viruses are a key driver for infections that trigger COPD exacerbations, increasing the clinical morbidity and burden for patients. The influenza virus is one of the three most common respiratory viruses detected in patients with COPD who present with an exacerbation, with a frequency of 7–31%Citation10–12. Influenza triggers progressive inflammation in the airways with the production of proinflammatory cytokines and tissue injury that can lead to decreasing pulmonary function and further deterioration of patients’ clinical statusCitation13,Citation14. Disruption of the integrity of the barrier function of the respiratory epithelium by influenza virus predisposes patients to bacterial superinfection, with secondary bacterial pneumonia being a complication and a predominant cause of morbidity and mortalityCitation15–17.
Much of the inference of poorer outcomes in patients with COPD and influenza has been derived from studies that evaluated the efficacy of influenza vaccination or from studies of elderly individuals with chronic lung diseaseCitation18–20. There are scant data on the longer-term consequences of influenza in the COPD population, in particular on how the disease may be destabilized over time or how morbidity may be aggravated. In this study, we used real-world US claims data from three influenza seasons in the U.S. (2012, 2013, and 2014) to assess COPD exacerbations, influenza-related complications, and health care resource utilization (HRU) up to one year following influenza diagnosis in patients with COPD.
Methods
Study design
In this retrospective observational cohort study, we extracted data from the MarketScan Commercial Claims and Encounters Database and the MarketScan Medicare Supplemental and Coordination of Benefits Database (IBM Watson Health, Cambridge, MA, USA) (). Databases included information on health insurance claims for employees, dependents, and retirees covered by employer-sponsored commercial and Medicare insurance. The claims files captured inpatient and outpatient care, use of health care facilities and services, prescription fills, and payment information. Each medical claim had up to 15 diagnosis codes (ICD-9-CM [International Classification of Diseases, 9th Revision, Clinical Modification], ICD-10) and 15 procedure codes (ICD PCS [Procedure Coding System], CPT [Current Procedural Terminology], and HCPCS [Healthcare Common Procedure Coding System]) documented for billing purposes.
The study used deidentified data and was exempt from Institutional Review Board review. The research was compliant with the Health Insurance Portability and Accountability Act.
Study population
For each influenza season, patients with COPD were identified over a 2-year time frame that included the influenza season and the preceding 1-year period. Patients were included if they were ≥40 years old (to limit potential overlap with asthma), if they had ≥1 inpatient admission with a primary diagnosis of COPD, or if they had ≥2 outpatient visits for COPD dated at least 30 days apart and at least 2 inhaled steroid COPD prescription fills in the 12 months preceding the index date. The ICD-9 or ICD-10 diagnosis codes for identifying COPD patients were chronic bronchitis (491, J41, J42), emphysema (492, J43, J98), chronic airway obstruction (496), or COPD (J44.xx)Citation21. Prescription medications used to qualify COPD cases for inclusion included inhaled bronchodilators, steroids, and phosphodiesterase (PDE)/PDE4 inhibitors.
For each influenza season, we first selected the patients with COPD. From these patients, we identified those who were diagnosed with influenza. Cases of influenza were identified for three influenza seasons: 2012 season (1 October 2012 to 30 September 2013), 2013 season (1 October 2013 to 30 September 2014), and 2014 season (1 October 2014 to 30 September 2015). Patients with a claim associated with a diagnosis suggesting influenza (ICD-9 codes 487.xx or 488.xx; ICD-10 codes J09.xx, J10.xx, or J11.xx) were included. The index date was defined as the date of the first influenza event in the season. Patients without influenza were randomly assigned a pseudo-index date, with the index month based on the distribution of months in each season that influenza was diagnosed among the cases. Patients had to be continuously enrolled in a health plan for at least 12 months before and 13 months after the index date.
For each season, patients with COPD with influenza were propensity score–matched at a 1:5 ratio to COPD patients without influenza. Propensity scores were calculated based on the following demographic variables: age categories, sex, geographic region, type of health plan, month of index event, region, plan type, and Charlson Comorbidity Index (CCI). Additionally, the following COPD severity measures were included in the matching algorithm: ratio of controller (maintenance) medications to total COPD medications (CTR) (an independent risk measure for COPD severityCitation22), number of baseline COPD-related outpatient visits, and number of baseline COPD-related inpatient visits.
Outcomes
We assessed outcomes during the first month after influenza diagnosis/index infection and over a full year following the initial 1-month period (months 2–13 combined after the index date). Outcomes for the 1-year period following the first month were also broken down and assessed as 4 quarters (each quarter was a 3-month period) in addition to the full year period.
The percentage of patients with exacerbation of COPD or any COPD- or pneumonia-related outcomes, including HRU and associated costs, was determined based on relevant ICD-9 or ICD-10 codes. COPD exacerbation was defined as an inpatient visit for COPD or receipt of an oral steroid prescription within 2 weeks of a COPD-related outpatient visit. Pneumonia was identified with the following codes: viral/bacterial/unspecified pneumonia (codes 480–486, 487.0, J12–J18); influenza due to certain identified influenza viruses with pneumonia (488.01, 488.11, 488.81), influenza due to identified novel influenza A virus with pneumonia (J09.X1), influenza due to other identified influenza virus with pneumonia (J10.0), and influenza due to unidentified influenza virus with pneumonia (J11.0).
COPD- or pneumonia-related HRU and costs were also assessed. These included the number of and total cost of inpatient, emergency department (ED), and outpatient visits. Costs were adjusted to 2017 dollars using the medical component of the Consumer Price Index.
Statistical analysis
Outcomes of COPD patients with influenza and those without influenza were compared for each time period (month 1 after diagnosis, quarter 1 [Q1; months 2–4], Q2 [months 5–7], Q3 [months 8–10], Q4 [months 11–13], and months 2–13 combined) with the chi-squared test for categorical measures and Wilcoxon signed-rank test for counts and costs. Analyses were conducted using SAS v9.4 software (SAS Institute Inc., Cary, NC, USA).
Results
Study population
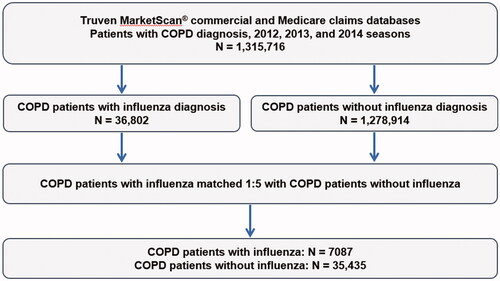
Over 2012, 2013, and 2014 influenza seasons, a total of 36,802 COPD patients with a diagnosis of influenza were identified. Following propensity score matching at a 1:5 ratio, the study population consisted of 7,087 COPD patients with influenza and 35,435 control COPD patients without influenza ().
Patients with COPD with or without influenza were well-matched overall and by season for the listed variables (). In the study population overall, 54.9% of patients were older than 65 years, 31.5% were older than 75 years, and 58.5% were female. The CCI was ≥3 in 35.8% of the population and ≥2 in 44.5% of patients. A CCI of 0 was reported in 5.0% of patients; this was possible because the CCI was determined in the 1-year baseline period preceding the index date, and some patients may not have had COPD-related visits if they were well-managed. The CTR was >0.8 in 49.8% of patients. From the time of diagnosis, 31.3% of patients had ≥6 COPD-related outpatient visits and 9.0% had been hospitalized for COPD.
Table 1. Baseline demographic and clinical characteristics of COPD patients with influenza and matched cohorts during 2012, 2013, and 2014 influenza seasons.
COPD-related outcomes
Exacerbations were significantly more frequent in COPD patients with influenza than in those without influenza in the first month after infection (16.1 vs. 3.4%; p < .0001) and over the next full year (months 2–13) (25.1 vs. 21.1%; p < .0001) (). Previous influenza infection was found to have an impact on COPD exacerbations during each of the individual 4 quarters after the first month ().
Figure 2. COPD-related outcomes over 13 months in patients with or without influenza during 2012, 2013, and 2014 influenza seasons (A) Month 1 and Year 1 (B) Quarterly over 1 year. *p < .0001 (for patients with influenza vs. patients without influenza). Abbreviations. COPD, chronic obstructive pulmonary disease; ED, emergency department.
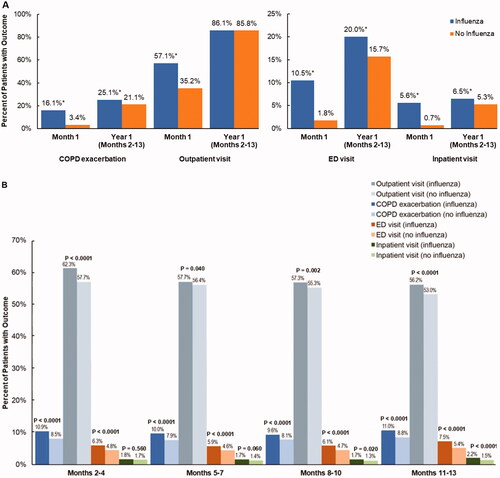
COPD patients with a diagnosis of influenza used significantly more health care resources at all future time periods examined. COPD-related inpatient visits, ED visits, and outpatient visits were higher in the first month and over a full year in COPD patients post influenza than in control patients (p < .0001 for all comparisons except p = .46 for outpatient visits over year 1) (). Health care resource utilization was also significantly higher for patients with influenza over each quarter (p < .0001 to p < .05) except for inpatient visits during Q1 (months 2–4) and Q2 (months 5–7) ().
The duration of inpatient stay was significantly longer and the number of inpatient visits, ED visits, and outpatient visits for COPD-related complications in the first month and the next full year were significantly higher in patients post influenza than in those who had not contracted influenza (p < .0001 for all comparisons) (). The findings were similar for all four quarters, except that the duration of inpatient stays in Q1 (months 2–4) and the number of inpatient stays in Q1 (months 2–4) and Q2 (months 5–7) did not differ significantly between post influenza and control groups.
Table 2. COPD-related health care resource utilization in patients with or without influenza during 2012, 2013, and 2014 influenza seasons.
Pneumonia-related outcomes
A significantly higher percentage of patients with COPD had a pneumonia-related outpatient, ED, or inpatient visit during the first month and over the next full year (months 2–13) after an influenza episode compared with control patients (). During month 1 in particular, pneumonia-related outpatient visits, ED visits, and inpatient visits occurred in a significantly greater proportion of patients with influenza than in those without influenza (outpatient visits: 23.7 vs. 2.6%, p < .0001; ED visits: 4.3 vs. 0.5%, p < .0001; inpatient visits: 6.2 vs. 0.3%, p < .0001, respectively). The higher frequency of HRU for pneumonia-related outcomes in patients with influenza persisted over the entire year following month 1, although the differences were not as marked as during month 1. When analyzed by quarters, outpatient visits, ED visits, and inpatient visits were higher among patients with influenza than among those without influenza ().
Figure 3. Pneumonia-related outcomes over 13 months in patients with or without influenza during 2012, 2013, and 2014 influenza seasons (A) Month 1 and Year 1 (B) Quarterly over 1 year. *p < .0001 (for patients with influenza vs. patients without influenza). Abbreviations. COPD, chronic obstructive pulmonary disease; ED, emergency department.
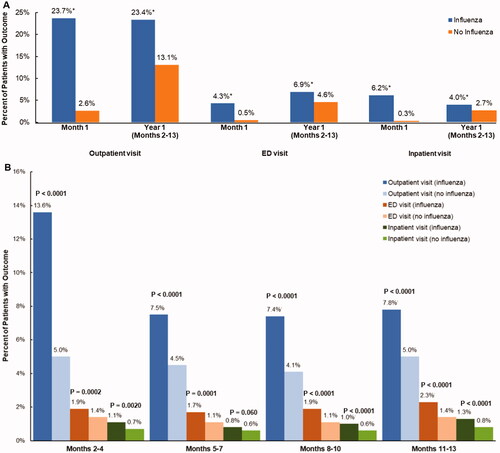
As with COPD-related complications, the duration of hospitalization was significantly longer and the number of inpatient, ED, and outpatient visits for pneumonia-related complications in the first month and the next full year were significantly higher in patients with influenza than in those without influenza (p ≤ .0001 for all comparisons) (). Significant differences in these outcomes between patients with and without influenza were observed over all 4 quarters examined (p < .01) other than the number of inpatient visits during Q2 (months 5–7) (p ≥ .05).
Table 3. Pneumonia-related health care resource utilization in patients with or without influenza during 2012, 2013, and 2014 influenza seasons.
COPD and pneumonia-related health care costs
The costs of inpatient, outpatient, and ED visits related to either COPD or pneumonia in the first month and year (months 2–13) were significantly higher in patients with COPD who had influenza than in patients without influenza (p ≤ .0001 for all comparisons) (). In month 1, patients with influenza had significantly higher COPD-related inpatient ($870.49 vs. $112.92, p < .0001), outpatient ($416.86 vs. $156.23, p < .0001), and ED ($360.59 vs. $71.82, p < .0001) costs than patients without influenza. Similarly, patients with influenza had significantly higher COPD-related inpatient ($1238.51 vs. $48.62, p < .0001), outpatient ($293.44 vs. $18.90, p < .0001), and ED ($162.90 vs. $30.65, p < .0001) costs than those without influenza.
Table 4. COPD- and pneumonia-related costs in patients with or without influenza during 2012, 2013, and 2014 influenza seasons.
Patients with influenza continued to incur significantly higher costs for both COPD- and pneumonia-related complications over the following 12 months. Other than COPD-related inpatient costs during Q1, both COPD-related and pneumonia-related costs were higher for patients with influenza during all 4 quarters ().
Discussion
This study used real-world claims data from three influenza seasons in the United States to document both the immediate and long-term impact of influenza on the frequency of COPD exacerbations and pneumonia as well as on COPD- and pneumonia-related HRU and costs. We found that compared with a matched influenza-free cohort, COPD patients with influenza infection not only required intensified medical care directly related to the event but continued to experience a small but significant increase in COPD exacerbations and pneumonia up to a full year after the index influenza episode. Our findings suggest that influenza is associated with long-term sustained deterioration of respiratory-related health in patients with underlying COPD disease.
Chronic obstructive pulmonary disease leads to progressive respiratory impairment, with well-documented health and economic impacts on both individuals and societyCitation23. In parallel, seasonal influenza is associated with a high annual rate of pulmonary infections and may thus add to the already high burden of disease in patients with COPDCitation24. While COPD exacerbations are known to accelerate disease progressionCitation25,Citation26, the influence of the immune response to the influenza virus on the progression of COPD is not well understood. Our study showed that an episode of influenza significantly increased the risk of a COPD exacerbation in the month following the index case; the frequency of an exacerbation was 16.1% in COPD patients post influenza compared with 3.4% in those without an infection. Notably, the effect of an episode of influenza on the likelihood of exacerbations was sustained over 13 months post-infection. In addition to an increased risk of COPD exacerbation, these patients also experienced a higher frequency of inpatient and ED visits as well as an increase in related costs during both the first month post-infection and over each subsequent quarter. The sustained increase in HRU up to 13 months after diagnosis suggests that influenza induces longer-term deleterious effects in COPD patients that continue even after the acute phase has resolved. Experimental evidence suggests that influenza A virus RNA can persist in pulmonary parenchyma and can aggravate chronic lung diseaseCitation27.
Patients with COPD are at heightened risk for developing pneumonia compared with those without COPDCitation28,Citation29. In healthy lungs, innate immune surveillance protects the lower respiratory tract from infection, but pathologic changes in the airways of patients with COPD are conducive to bacterial colonization and infectionCitation30. The influenza virus itself can cause pneumonia, by direct airway damage or by damage from the immune response, but influenza also predisposes to a secondary bacterial infection because of an altered lung immune environmentCitation31. In the current study, we found that patients with COPD who had influenza experienced a higher burden of pneumonia-related HRU, including outpatient visits, inpatient stays, and ED visits, together with higher associated costs, compared with those who did not have influenza. Intensified pneumonia-related HRU and costs were observed not only in the early period after infection but also continued to a smaller but statistically significant extent over the entire year after infection.
These results highlight the serious burden of influenza and underscore the importance of preventing influenza in patients with COPD in particular. Influenza vaccination can significantly reduce the number of exacerbationsCitation32 and influenza-related hospitalizations in COPD patientsCitation20. Annual immunization against influenza is recommended for individuals with COPD to reduce influenza-triggered exacerbations and acute respiratory infections and thus reduce related costsCitation33–35. Despite guideline recommendations, as many as 34% of hospitalized patients with COPD were reported to be unvaccinated against influenzaCitation20. Additionally, the use of antiviral treatment could potentially benefit individuals with COPD. Previous studies have documented a reduction in hospitalization and influenza-related complications in at-risk populations following early antiviral treatmentCitation36,Citation37. Furthermore, in a real-world analysis of patients with COPD and influenza, we documented a reduction in HRU and costs among patients who received antiviral treatment for influenzaCitation38. Rates of antiviral prescribing, however, remain low among patients with acute respiratory illness in both hospital and outpatient settingsCitation20,Citation39, and strategies that limit the impact of influenza in vulnerable groups, such as patients with COPD, therefore, need to be investigated further.
This study provides novel evidence of the impact of influenza on COPD patients’ long-term health using a large commercial claims database, which allowed for a large real-world substantial patient sample to be analyzed. Also, by using propensity score matching for variables that could influence outcomes, we were able to ensure the comparability of the cohorts with or without influenza. Further, we used the CTR (a measure of the severity of COPD), the CCI, and inpatient and outpatient visits in the preceding year to control for differences in baseline morbidity and severity of COPD. However, there are limitations because of the data used and study design. The database includes enrollees in commercial health plans and some supplemental Medicare plans and may therefore not be representative of the entire US population. Additionally, because influenza and pneumococcal vaccinations are not consistently reported in claims databasesCitation40,Citation41, vaccination status was not controlled for in matching and could have impacted results if vaccination was not evenly distributed between the cohorts. Despite the use of propensity score matching to reduce the risk of selection bias, the possibility of residual bias could not be discounted. Because only exacerbations that resulted in a health care encounter were identified from the database, mild exacerbations not requiring medical attention that may affect routine functioning may have been missed. Additionally, the influenza cases included in the study were identified by clinical diagnosis and were not necessarily confirmed by laboratory-based influenza testing; this study may therefore have included cases with other viral illnesses identified as influenza. This study examined only HRU and costs related to exacerbations and pneumonia in COPD patients with influenza. However, other comorbidities, such as cardiovascular disease may also worsen due to COPD exacerbations and require additional resources, but these may not be coded with a COPD diagnosis code. COPD exacerbations and pneumonia were identified based on diagnosis codes in the claims databases and were not verified by review of medical records; this could introduce errors due to missing information or inclusion of unconfirmed events. However, the use of claims data allowed a larger, more diverse group of patients to be evaluated over a longer period.
Conclusions
The results of our study demonstrate that one influenza episode in patients with COPD can be associated with poor COPD outcomes and increased HRU not only over the first month after the influenza diagnosis but also over the full year following the acute infection. Furthermore, COPD-related inpatient, outpatient, and ED visits and costs were higher in patients who had influenza than in matched controls. A similar pattern was also noted for increases in short-term and long-term pneumonia-related HRU in COPD patients with influenza. Our findings underline the need to implement strategies that could lower the risk of influenza in patients with COPD and influenza, which may lead to clinical benefits and reduction of economic costs.
Transparency
Declaration of funding
The study was sponsored and funded by Genentech, Inc., South San Francisco, CA, USA.
Declaration of financial/other relationships
CW, TMT, SK, HM, and DW are current employees of Genentech/Roche, Inc., and hold Roche stock.
Author contributions
All authors were involved with all aspects of the manuscript–data collection and analysis and manuscript review and approval.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Previous presentations
This study was presented in poster format at the 6th International Society for Influenza and Other Respiratory Viruses conference, Rockville, MD, 13–15 November 2018.
Acknowledgements
Meher M. Dustoor, and Esther Tazartes, of Global Outcomes Group, provided editorial assistance; these services were funded by Genentech, Inc.
Data availability statement
The data that support the findings of this study are available from IBM MarketScan Research Databases, but these data are not publicly available. All relevant data are provided within the manuscript and supporting files.
References
- Centers for Disease Control and Prevention. Estimated flu-related illnesses, medical visits, hospsitalizations, and deaths in the United States–2019–2020 influenza season; 2021 [cited 2021 Nov 13]. Available from: https://www.cdc.gov/flu/about/burden/2019-2020.html
- Garten R, Blanton L, Elal AIA, et al. Update: Influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. Morb Mortal Wkly Rep. 2018;67(22):634–642.
- Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472.
- Yu AP, Yang H, Wu EQ, et al. Incremental third-party costs associated with COPD exacerbations: a retrospective claims analysis. J Med Econ. 2011;14(3):315–323.
- Dalal AA, Patel J, D'Souza A, et al. Impact of COPD exacerbation frequency on costs for a managed care population. J Manag Care Spec Pharm. 2015;21(7):575–583.
- Patel JG, Coutinho AD, Lunacsek OE, et al. COPD affects worker productivity and health care costs. Int J Chron Obstruct Pulmon Dis. 2018;13:2301–2311.
- Guarascio AJ, Ray SM, Finch CK, et al. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–245.
- Pasquale MK, Sun SX, Song F, et al. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764.
- Hurst JR, Skolnik N, Hansen GJ, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1–6.
- Mohan A, Chandra S, Agarwal D, et al. Prevalence of viral infection detected by PCR and RT-PCR in patients with acute exacerbation of COPD: a systematic review. Respirology. 2010;15(3):536–542.
- Zwaans WA, Mallia P, van Winden ME, et al. The relevance of respiratory viral infections in the exacerbations of chronic obstructive pulmonary disease–a systematic review. J Clin Virol. 2014;61(2):181–188.
- Biancardi E, Fennell M, Rawlinson W, et al. Viruses are frequently present as the infecting agent in acute exacerbations of chronic obstructive pulmonary disease in patients presenting to hospital. Intern Med J. 2016;46(10):1160–1165.
- Herold S, Becker C, Ridge KM, et al. Influenza virus-induced lung injury: pathogenesis and implications for treatment. Eur Respir J. 2015;45(5):1463–1478.
- Betakova T, Kostrabova A, Lachova V, et al. Cytokines induced during influenza virus infection. Curr Pharm Des. 2017;23(18):2616–2622.
- MacIntyre CR, Chughtai AA, Barnes M, et al. The role of pneumonia and secondary bacterial infection in fatal and serious outcomes of pandemic influenza a(H1N1)pdm09. BMC Infect Dis. 2018;18(1):637.
- Rice TW, Rubinson L, Uyeki TM, et al. Critical illness from 2009 pandemic influenza a virus and bacterial coinfection in the United States. Crit Care Med. 2012;40(5):1487–1498.
- Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198(7):962–970.
- Bekkat-Berkani R, Wilkinson T, Buchy P, et al. Seasonal influenza vaccination in patients with COPD: a systematic literature review. BMC Pulm Med. 2017;17(1):79.
- Mallia P, Johnston SL. Influenza infection and COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(1):55–64.
- Mulpuru S, Li L, Ye L, et al. Effectiveness of influenza vaccination on hospitalizations and risk factors for severe outcomes in hospitalized patients with COPD. Chest. 2019;155(1):69–78.
- COPD Foundation. COPD and other respiratory conditions. ICD-9-CM and ICD-10-CM Reference Guide; 2021 [cited 2021 Nov 13]. Available from: https://www.copdfoundation.org/pdfs/ICD%20Reference%20Codes.pdf
- Stanford RH, Nag A, Mapel DW, et al. Validation of a new risk measure for chronic obstructive pulmonary disease exacerbation using health insurance claims data. Ann Am Thorac Soc. 2016;13(7):1067–1075.
- National Center for Health Statistics. Chronic obstructive pulmponary disease (COPD) FastStats; 2021 [cited 2021 Nov 13]. Available from: https://www.cdc.gov/nchs/fastats/copd.htm
- Troeger CE, Blacker BF, Khalil IA, et al. Morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: an analysis for the global burden of disease study 2017. Lancet Respir Med. 2019;7(1):69–89.
- Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852.
- Wedzicha JA, Donaldson GC. Natural history of successive COPD exacerbations. Thorax. 2012;67(11):935–936.
- Keeler SP, Agapov EV, Hinojosa ME, et al. Influenza a virus infection causes chronic lung disease linked to sites of active viral RNA remnants. J Immunol. 2018;201(8):2354–2368.
- Mullerova H, Chigbo C, Hagan GW, et al. The natural history of community-acquired pneumonia in COPD patients: a population database analysis. Respir Med. 2012;106(8):1124–1133.
- Soriano JB, Visick GT, Muellerova H, et al. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–2107.
- Sethi S. Infection as a comorbidity of COPD. Eur Respir J. 2010;35(6):1209–1215.
- Kalil AC, Thomas PG. Influenza virus-related critical illness: pathophysiology and epidemiology. Crit Care. 2019;23(1):258.
- Kopsaftis Z, Wood-Baker R, Poole P. Influenza vaccine for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2018;6:CD002733.
- Centers for Disease Control and Prevention. People at higher risk of flu complications; 2021 [cited 2021 Nov 13]. Available from: https://www.cdc.gov/flu/about/disease/high_risk.htm
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Arch Bronconeumol. 2017;53(3):128–149.
- O'Donnell DE, Hernandez P, Kaplan A, et al. Canadian thoracic society recommendations for management of chronic obstructive pulmonary disease – 2008 update – highlights for primary care. Can Respir J. 2008;15 (Suppl A):1A–8A.
- Muthuri SG, Venkatesan S, Myles PR, et al. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza a H1N1pdm09 virus infection: a meta-analysis of individual participant data. Lancet Respir Med. 2014;2(5):395–404.
- Venkatesan S, Myles PR, Leonardi-Bee J, et al. Impact of outpatient neuraminidase inhibitor treatment in patients infected with influenza A(H1N1)pdm09 at high risk of hospitalization: an individual participant data metaanalysis. Clin Infect Dis. 2017;64(10):1328–1334.
- Wallick C, Wu N, To T, et al. Treating influenza with antivirals is associated with a decreased burden of complicatons and health resource utilization in high risk patients. Presented at the Options X for the Control of Influenza Conference; 2019 August 28–September 1; Singapore; 2019. Abstract 11161, p. 35. Available from: https://isirvorg/site/images/conferences/Optionsx/Options%20X_Abstracts%20_Oral%20and%20Posterpdf
- Havers F, Flannery B, Clippard JR, et al. Use of influenza antiviral medications among outpatients at high risk for influenza-associated complications during the 2013–2014 influenza season. Clin Infect Dis. 2015;60(11):1677–1680.
- Lochner KA, Wynne MA, Wheatcroft GH, et al. Medicare claims versus beneficiary self-report for influenza vaccination surveillance. Am J Prev Med. 2015;48(4):384–391.
- Schwartz KL, Jembere N, Campitelli MA, et al. Using physician billing claims from the Ontario health insurance plan to determine individual influenza vaccination status: an updated validation study. CMAJ Open. 2016;4(3):E463–E470.