Abstract
Background and aims
Treating patients in psychiatric intensive care units (PICUs) is costly for the English National Health Service (NHS), requiring significant staff time. Oxevision, a non-contact system, providing vision-based patient monitoring and management (VBPMM) has been introduced in some NHS mental health trusts which aims to help clinicians to deliver safer and more efficient care. The objective of this early economic evaluation was to explore the impact of introducing VBPMM with standard care, versus standard care alone on health and economic outcomes in PICUs across England.
Methods
The model uses a cost calculator approach to evaluate the potential benefits of introducing VBPMM, capturing differences in observation hours and critical events such as assaults. Effectiveness data were primarily based on a 24-month observational before and after study undertaken in an NHS mental health trust using VBPMM. Outcomes reported in this study are incremental costs and reduction in clinical events presented as per occupied bed days, per patient, per average ward, and for the English NHS overall. Scenario analysis was conducted to test the uncertainty of results using statistical significance of key inputs.
Results and conclusions
The analysis indicates that introducing VBPMM may be cost saving compared with standard care alone. The biggest driver of estimated cost savings was from the potential reduction in one to one observation hours, which may have significant impact in PICUs. Limitations of the analysis include the single center data underpinning the analysis and assumptions made about transferability of clinical data to different sized wards. Scenario analysis was conducted, and the results were robust to statistically significant changes in input parameters. This study suggests that introducing VBPMM on PICUs has the potential to reduce costs and improve efficiency of resource allocation, but results should be confirmed with additional clinical study evidence.
Introduction
Treating patients in mental health hospitals is costly for the English National Health Service (NHS). The appropriate level of care for patients requires substantial staff time and can involve nursing patients on continuous one to one observation for temporary and extended periods of timeCitation1. Additionally, incidents such as assaults or rapid tranquillization events may occur within these settings resulting in further costs to the mental health trust providing care and to wider NHS services such as accident & emergency (A&E)Citation2,Citation3.
Recently, some psychiatric intensive care units (PICUs) within the NHS have used Oxevision, a system providing vision-based patient monitoring and management (VBPMM), which has the potential to help the NHS to reduce the cost of mental health careCitation2. VBPMM is designed to help healthcare professionals respond to patient needs more quickly and efficiently than is possible with current standard of care alone. The technology is intended to complement existing best practice and not replace clinical judgment or personal interaction with patients. It is a wall mounted system which is contact free and is placed in every single occupancy room on a ward. VBPMM enables the physiological measuring of pulse rate and breathing rate and, with its ability to provide activity and location-based alerts, also enables the physical monitoring of movement and position within the bedroom. Nurses will regularly interact with the system through a monitor in the nurses’ station and portable tablet devices. VBPMM works continuously, and clinical staff are able to access medical grade pulse rate and breathing rate measurements without having to enter the patient’s room. The introduction of VBPMM has the potential to help staff reduce the rate of adverse events, such as assaults and rapid tranquillization events and reduce the number of avoidable one to one observations and night-time observational hours, in adults in PICUs or mental health hospitals with VBPMMCitation2. Furthermore, VBPMM also has the potential to improve patient and staff experience.
Previous research was undertaken at a regional mental health NHS trust in England in 2019 to investigate the impact of adopting VBPMM on safety and quality of careCitation4. This research demonstrated potential benefits to the health system including improved patient safety and the ability to reduce healthcare resource use.
A health-economic model was developed to assess the potential cost savings of using VBPMM alongside standard care, compared with standard care alone, for adults who are admitted to PICUs. Results are presented from an NHS and Personal Social Services (PSS) perspective. Additional analysis from the perspective of individual mental health trusts and clinical commissioning groups (CCGs) is included in the supplementary material. At the time of the analysis, CCGs were still in place within the NHS. The impact of introducing VBPMM is likely to be similar for integrated care systems (ICSs), which are expected to replace CCGsCitation5.
Methods
Data collection
Data underpinning this analysis, such as the baseline events without VBPMM and the effect of its introduction, was from an unpublished observational study on Oxevision conducted in a PICU wardCitation4. The VBPMM was implemented in a PICU in January 2019, and the 12-month period (to December 2019) was compared with the same time period in the previous year. The number of beds, occupancy rates and number of wards in the study are presented in . The study population was defined as adults over 18, with an average age of 36 for those included in the study. All patients included in the study suffered from various diagnosed mental health conditions, with 35% suffering from schizophrenia, 24% suffering from mood affective disorders and 15% from substance misuse. Other conditions suffered by patients in the study included personality disorders, as well as neurosis and stress related disorders.
Table 1. Clinical inputs used to scale populations.
As part of the study, patients, or carers where appropriate, were informed about the system on admission to the wards by the clinicians, through leaflets and one to one talks with their doctor. Patients and carers were engaged through interviews and surveys to receive their feedback. Clinicians received in person training and education material, who were then also engaged through interviews for feedback in using the system.
The following key events were captured in the clinical data to be used in the analysis
Assaults;
Rapid tranquillizations;
Night-time observation time (number of hours that staff take to check patients during the night, excluding one to one observations);
One to one observation time (number of hours that staff are on continuous observations with a patient who is assessed as high risk).
The number of events 12 months before and 12 months after the introduction of VBPMM was recorded, with the difference between the two representing the efficacy of the device in reducing these types of events, i.e. the benefits of VBPMM. Importantly, rapid tranquillization events were recorded separately to assaults, meaning there was no overlap or potential for double counting the effects of VBPMM within the model.
Model structure
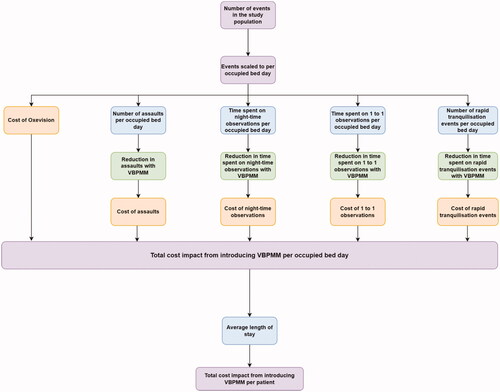
The model was developed in Microsoft Excel (Microsoft Corporation, Redmond, WA) and structured as a cost calculator, comparing the VBPMM system plus standard care versus standard care alone. Standard care alone is defined as usual patient care and medical supervision (i.e. clinical observation) without the VBPMM system. A cost-calculator approach was considered appropriate as it is in line with the National Institute of Health and Care Excellence (NICE) methods for evaluating medical technologiesCitation8. Previous surveys and observational data indicate that introduction of VBPMM may improve patient safety and care when delivered alongside standard of care, through qualitative synthesis of the resultsCitation9. The analysis was therefore focused on comparing the number of clinical events, observations (night time or one to one) and associated costs following the introduction of the VBPMM versus those occurring with standard care alone. The population of the model was adults who were admitted to PICUs in the English NHS. The outcomes collected from the clinical study were specific to the mental health trust in which the study was conductedCitation4. Data from the study were available on the number of clinical events occurring before and after the introduction of the VBPMM over a 24 month timeframe, 12 months before VBPMM and 12 months after. These outcomes were scaled in the model to a common metric, “per occupied bed days”, to convert them to a common time frame for modeling and to provide more generalizable outcomes. Using “per occupied bed days” as a metric has the advantage of allowing events to be scaled to a per patient outcome by using an average length of stay, which is a common reporting metric for economic evaluations in healthcare. The model results can also be reported per ward (providing the number of beds and occupancy rate is available), as well as for the NHS as a whole (by using data on total occupied bed days per year).
All outcomes from the clinical study were scaled to “per occupied bed day” by dividing the outcomes reported in the study, such as number of assaults or tranquillization events, by the total number of occupied bed days relevant to the study population and period over which the study was conducted. A diagram of the model structure is shown in .
Efficacy of VBPMM was derived from the percentage reduction in events reported from the clinical observational data from the use of VBPMM in a PICU wardCitation4.
A 12-month time horizon was used for the analysis as this was considered sufficiently long to capture the full impact of the VBPMM on a single patient cohort, since patient stay in the PICU is short term and all events captured in the model are expected to be short term. A 12-month time horizon also aligns with the annual license fee model for the device.
Length of stay was assumed not to be impacted by the introduction of VBPMM due to the paucity of data. Additionally, the potential for differences in the costs associated with internal and external investigations of serious incidents were excluded from this analysis due to insufficient data. However, there may be anecdotal evidence of this finding, which is expected to be analyzed in future research. Potential time savings associated with staff sickness (e.g. as a result of an assault) and efficiency in multi-disciplinary team meetings and handovers were also excluded from this analysis.
The analysis was conducted in line with the NICE reference case, modeling costs from a UK National Health Service perspectiveCitation10. No discount rate was applied as the cost model uses a 1-year time horizon. Quality of life was not captured within the model. Other perspectives such as those of CCGs and mental health trusts were conducted as scenario analyses, with more detail on these provided in the supplementary information.
Model inputs
Data used to populate the model were informed by several sources. Predominantly, inputs relating to VBPMM and its impact on clinical effectiveness were taken from an unpublished observational study on Oxevision conducted in a PICU wardCitation4. Inputs were supplemented by targeted searching to inform different parameters and publicly available sources such as NHS reference costs and Personal Social Services Research Unit (PSSRU) were used where possible for the costingCitation11–13.
Clinical data
The impact of VBPMM and the baseline number of events occurring with standard care were elicited from an observational study on the impact of VBPMM on clinical effectivenessCitation4. Study data were collected over a 24-month period, 12 months prior to VBPMM and 12 months after VBPMM was introduced. In order to model the events over a common time frame and generalize the results of the model to different population sizes beyond the clinical study, a common metric was used (occupied bed days). This common metric could then be used to transform the results of the model into costs per patient, per average sized ward and the NHS as a whole. details the sources and calculations used to convert occupied bed days to each of these metrics.
presents the data relating to clinical events captured in the model, including the baseline number of events, and the impact associated with the introduction of VBPMM. The resulting assumption here is that the marginal efficacy of VBPMM will remain the same regardless of the ward size. Supplementary material contains a wider description of how staff hours were calculated for each activity. In summary, this was elicited by interviews with clinicians at various grades, from nurses to consultant psychiatrists to clinical management.
Table 2. Clinical inputs used in the model.
There is more detail on how the inputs relate to other perspectives provided within Supplementary Appendix 1. Furthermore, where appropriate for the economic evaluation, the analysis looks to consider the nature of the cost savings, whether they are cash releasing or an opportunity cost saving. Cash releasing cost savings relate to if the cost would see an in-year monetary return without changing safe staffing levels. Opportunity costs are the costs associated with resources being released within safe staffing levels, which can be used for other clinical activities. This is particularly relevant for one to one observation time, given this represents a significant resource constraint for PICUs.
Cost data
All costs used in the analysis were in UK pounds sterling (2018/19 cost year). The values used in the analysis are shown in .
Table 3. Costs associated with PICU events and VBPMM.
Further details on the methodology for the costings are provided in Supplementary Appendix 2, which outlines the method for how resource use was estimated for assaults and rapid tranquillization events. Staff costs were taken from the PSSRUCitation11. Costs for a Healthcare Assistant (HCA) were inflated from the 2017 version using the NHS cost inflation pay and prices inflation indices because PSSRU no longer provides a breakdown of band 3 costsCitation12.
Upfront costs of implementing VBPMM were annuitized over the lifespan of the intervention (10 years). Therefore, only one year of this annuitized cost is considered within the 1-year time horizon of the model. It is expected that the results of the analysis could be extrapolated over future years, with similar cost savings seen each year following implementation of VBPMM. The cost of implementing VBPMM is expected to differ depending on ward size and number of beds, as well as staff numbers.
Assumptions around the severity of injury associated with an assault or complications related to rapid tranquillization were made when costing these events in the model due to a paucity of data. We assumed these were equal to minor fracture codes for assaults, or angina codes for complications from NHS reference costsCitation13. This is because major injuries and complications are assumed to be less frequent; hence, this is considered a conservative assumption. However, this may underestimate the costs of these types of events within the model.
Economic analysis
The following primary outcomes were generated from the model, both for standard care and VBPMM, as well as the incremental differences between the two treatment arms: cost per occupied bed day, cost per patient, cost per average ward per year and cost to the NHS per year. Cost breakdowns on a per patient basis are provided, which highlights where costs are incurred as well as key areas where adopting VBPMM may generate cost savings. The proportion of the cost savings which are cash releasing or opportunity cost saving per event are provided.
Two scenarios were considered in order to account for uncertainty surrounding the data used for input parameter values. These were looking at the confidence intervals of the results, as well as thresholds for break-even points for one to one observation. The results of the scenario analyses are reported using the same primary outcomes of the model as in the base case.
The confidence intervals underpinning the event data are wide for some events, as shown in . This indicates there is a higher level of uncertainty around the estimated efficacy values of the impact of VBPMM on clinical practice used in the model. The model results and conclusion will be more uncertain as a result. Therefore, a scenario was conducted that included the estimated values only for those events where a statistically significant reduction was reported (night-time observation time and rapid tranquillization events), such that the results in the data are not likely to occur by chance alone (p<.05). Events that were not significantly reduced in the study were excluded in this scenario. shows the reduction in events with VBPMM and the associated confidence intervals which were used to determine which variables to include in the scenario analysis.
Table 4. Confidence intervals.
Only the values for reduction in night-time observation time and reduction in rapid tranquillization events were included in this scenario based on the confidence intervals presented in .
Threshold analysis was conducted to assess the potential breakeven point from introducing VBPMM in addition to standard care from both a cash releasing perspective and an overall perspective (cash releasing and opportunity costs). The only cash releasing event is one to one observation hours, given typically many of the staff are taken from agencies or bank staffing, rather than the core PICU staffing establishmentCitation20. As a result, this has potential policy implications for PICUs in terms of resource use.
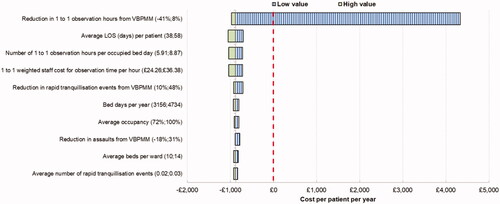
Finally, univariate deterministic sensitivity analysis was conducted in order to explore uncertainty around key parameters inputs and identify key drivers of the analysis. Ranges used for the deterministic sensitivity analysis were based around confidence intervals where available or 20% either side of the base case value where unavailable.
Results
Base case results
Compared with standard care alone, use of VBPMM is estimated to lead to cost savings of £72,286 per ward per year, or £880 per patient per year. The cost saving to the NHS per year is estimated to be around £5.5 million. These results are detailed in .
Table 5. Summary results.
The breakdown of costs highlights that the key driver of cost savings is 36 h of staff time saved per patient per year, primarily driven by one to one observation hours which is a labor-intensive activity. A proportion of one to one observation hours is also expected to be cash releasing, given additional staff (i.e. beyond the safe staffing establishment) will not be required for the ward.
Other events are also expected to be reduced by the introduction of VBPMM, with 0.64 fewer (35.3%) rapid tranquilization events or assaults per patient per year, which can be potentially time-intensive and negatively impact both staff and patients, relative to the severity of the incident.
Further breakdowns of the data are presented in the Supplementary Appendices 3 and 4. These include alternative perspectives for the analysis (mental health trust, CCG), with cost breakdown results presented for an average sized ward for both.
Scenario analysis results
The first scenario conducted considered only those outcomes where a statistically significant benefit was shown in the study. Reduction in time spent on night-time observational hours and rapid tranquillization events as a result of implementing VBPMM were statistically significant, such that the results in the study are not likely to have occurred by chance alone (p<.05). Removing events that were not statistically significant from the analysis still results in a marginal cost saving with the introduction of VBPMM. These results are detailed in .
Table 6. Scenario with only significant events.
The second scenario analysis was conducted to investigate the potential effect that including VBPMM can have just relating to one to one observation hours. From the analysis, a 4% reduction in one to one observation hours is expected to be needed to break even in-year if considering only the cash releasing aspect of one to one observation hours (with all other inputs as per the base case scenario), compared to 7% as estimated in the base case. If considering all potential cost savings, including opportunity costs, it is estimated that cost savings from a reduction in other events would be sufficient to break even without any reduction in one to one observation hours.
Sensitivity analysis results
The results of the deterministic sensitivity analysis are presented in .
The key independent drivers of the results are the efficacy of VBPMM in reducing one to one observation hours, the number of baseline one to one observation hours and the cost of one to one observation time per hour. Only the reduction of one to one observation hours with the VBPMM changes the direction of the results of the analysis to cost incurring. This is likely due to the wide confidence interval around this parameter, demonstrating the value of collecting further data around the impact on observation hours following introduction of the VBPMM.
Discussion
This analysis demonstrates that VBPMM alongside standard care is potentially a cost saving intervention versus standard care alone when implemented for adults who are admitted to PICUs based on the results of a single center observational before and after study. The results of this analysis indicate that adopting VBPMM can lead to cost savings of £880 per patient, £72,286 per average sized ward per year or a total cost saving to the NHS of £5,541,924.
A significant proportion of these benefits relate to a potential reduction in one to one observation hours, of which a proportion is also expected to be in-year cash releasing for the NHS. Reducing one to one observation hours is expected to save £806 per patient per year, with £629 of this expected to be in-year cash releasing savings. This is higher than the cost of implementing VBPMM per patient, highlighting that introducing this system may potentially free up resources within safe staffing establishments, whilst also saving the NHS money for additional staffing requirements (i.e. agency/bank spend). Furthermore, the introduction of VBPMM is estimated to reduce around 3,000 staff hours across an average ward per year by reducing night-time observation hours, one to one observation hours, assaults and rapid tranquillization events. Given the pressures already facing the NHS, this may have policy implications for managing resource use on PICUs, as resources can potentially be more efficiently used on more therapeutically beneficial activities from introducing VBPMM. As shown in the scenario analysis, even if the reduction in one to one observation hours from implementing VBPMM was lower than the base case, a 4% or greater reduction would still generate a cash releasing cost saving for an average sized ward.
Running the model with only those events where the use of VBPMM results in a statistically significant difference had a large impact on the model results. This highlights the uncertainty in the efficacy data. Deterministic sensitivity analysis also highlighted that uncertainty around reduction in observation hours has the potential to change the direction of the results of the analysis when varied alone. Therefore, additional data, particularly around reduction in one to one observation hours, should be incorporated into the economic model when available to improve the robustness of the findings. Further studies are being conducted to evaluate the impact of VBPMM on clinical practice and can provide greater certainty on the expected effects. The results of the analysis are specific to adults admitted to PICU and therefore cannot be generalized to other populations. However, other subgroups of people are currently being explored where VBPMM may also be effective.
While the model aims to capture the operational and monetary value of the benefits associated with introducing VBPMM, there may be further benefits which are not captured within the analysis. For instance, there is qualitative evidence that implementing the system may have benefits to both staff and patient experience, which may lead to improvements in patient care and quality of lifeCitation2. This is particularly important in relation to patient safety, given the reduction in incidents such as assaults and rapid tranquillization events is likely to make both patients and their families feel safer. Other benefits included better sleep and reported improvements in wellbeingCitation9. There is also potential that this could have positive repercussions for staff retention and/or staff sickness, due to the improvements that including VBPMM for assisting staff may have on their experience. Further to this, due to the potential savings in staff time, there could be potential for PICUs to change their staffing mix to best meet individualized patient needs, potentially increasing the capacity of highly trained practitioners available within the NHS. These benefits are unlikely to be quantifiable for an economic evaluation and are generally captured using qualitative data such as surveys. Nonetheless they are important to consider when assessing the potential benefits of introducing VBPMM.
A potential reduction in serious incidents could be a further benefit of VBPMM which has not been captured in the analysis due to both a paucity of data from the initial study on how VBPMM would affect these events, as well as the inherent challenge in costing these heterogeneous events. Serious incidents stem from particularly severe assaults or rapid tranquillization events. These serious incidents could require a lengthy internal review, as well as the potential for legal costs which could be over £30k per event based on other types of NHS litigationCitation21. These types of events would be particularly expensive; however, they are likely to be rare occurrences. For instance, previous literature has indicated only 0.2% of assaults lead to prosecution being pursuedCitation20.
Limitations
A number of assumptions were made when comparing the inclusion of VBPMM to standard care alone. First, it was assumed that the data collected from the observational study on the specific trust are transferable and can be scaled to different populations and settings. This is an important assumption as, in order to evaluate the effects of the intervention from the clinical study and generalize the results, a common metric had to be used (per occupied bed day). This means that for the purposes of the model, the marginal effect of adopting VBPMM remains constant as it is scaled to alternative populations. For instance, it does not consider makeup and staffing of wards, or other factors such as patient case mix which could alter the effectiveness of the intervention and will likely have an impact on the baseline rate of events. Therefore, if the events at baseline are higher than in another ward, this may understate the benefits of using VBPMM, given there may be a greater capacity to benefit from the service. Similarly, if another ward had a lower baseline of events, the model may overstate the potential benefits of using VBPMM.
Second, in order to report the results on a per patient basis, it is assumed that an average length of stay from Hospital Episode Statistics can be used in order to elicit a per patient cost based on mental health trusts as a wholeCitation6. However, it is likely that this length of stay will differ across various trusts as well as patient groups. Furthermore, this value is not specific to adults in PICUs meaning the per patient cost may not be entirely reflective of the average cost per patient. If the average length of stay of patients is longer in another ward, the model is likely to understate the benefits per patient, which means potential for a greater benefit from introducing VBPMM on a per patient basis, even if the cost per occupied bed day is unchanged.
Finally, for the purposes of this model, only costs are considered, not the health benefits associated with using VBPMM. This modeling approach is only appropriate if the VBPMM is equivalent to or better than standard of care in terms of patient outcomes. Further research could look to assess the impact of introducing the VBPMM on patient outcomes and produce a full cost–utility analysis of introducing VBPMM in PICUs, capturing the health impacts alongside the costs associated with the various events. It is likely that there would be a positive impact on patient quality of life as a result of introducing VBPMM due to the reduction in adverse events outlined in this study alone. Further research may be warranted to understand the magnitude of the impacts on quality of life of a reduction in adverse events as well as to identify other areas where patient quality of life is affected by the introduction of VBPMM.
Conclusions
Early economic analysis suggests that implementing VBPMM with standard care is likely to represent a cost saving intervention compared with standard care alone from a UK perspective, for adult patients admitted to PICUs. This is likely to impact a wide range of NHS stakeholders, such as individual NHS trusts providing the services and CCGs, by reducing costly events and resource use. However, this is based on a single center observational before and after study. Further data are currently being collected on the impact of introducing VBPMM with standard care versus standard care alone, which will aid in reaffirming the results and conclusions outlined within this paper.
Transparency
Declaration of funding
RM, JS and AS are employed by York Health Economics Consortium (YHEC). YHEC was funded by Oxehealth to develop the economic model and manuscript.
Declaration of financial/other relationships
YHEC was funded by Oxehealth to develop the economic model and manuscript. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
FN and KW were the chief and principal investigators respectively in the clinical study of Oxevision. RM and JS were involved in the conceptualization and design of the economic model. The analyses were undertaken by RM and JS. RM drafted the manuscript with critical revision from JS, AS, FN and KW. All authors approved the final version. Michelle Green was previously involved in the conceptualization of the economic model to evaluate the cost savings of the vision-based patient monitoring and management system in PICUs. Daniel Bayley helped to provide insight into the technology, the clinical evidence, and how the technology is used in clinical practice. He also provided feedback on the draft manuscript.
Supplemental Material
Download MS Word (28.9 KB)Acknowledgements
None reported.
Data availability statement
To request the original data regarding Oxevision please contact [email protected]
References
- Wolff J, McCrone P, Berger M, et al. A work time study analysing differences in resource use between psychiatric inpatients. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1309–1315.
- Coventry and Warwickshire Partnership NHS Trust. Improving safety in acute mental health hospitals; 2020 [cited 2021 Mar]. Available from: https://assets-global.website-files.com/5f567869171c90518f161723/5f7dd2be9a62bc2d11ed5c79_Patient_CWPT_Early_Insights_Case_Study.pdf
- Crowhurst N, Bowers L. Philosophy, care and treatment on the psychiatric intensive care unit: themes, trends and future practice. J Psychiatr Ment Health Nurs. 2002;9(6):689–695.
- Coventry and Warwickshire Partnership NHS Trust. How technology can change services; 2020 [cited 2021 Mar]. Available from: https://assets-global.website-files.com/5f567869171c90518f161723/5f7e0bad1a06a32e1da2a3ab_qnpicu–-webinar-presentation-flyer–17-july-2020.pdf
- The King’s Fund. A year of integrated care systems: reviewing the journey so far. London: The King’s Fund; 2018 [cited 2021 Mar]. Available from: https://www.kingsfund.org.uk/sites/default/files/2018-09/Year-of-integrated-care-systems-reviewing-journey-so-far-full-report.pdf
- Hospital Episodes Statistics. Hospital admitted patient care activity 2019-20; 2020 [cited 2021 Feb 8]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2019-20
- The Strategy Unit NHS. Exploring mental health inpatient capacity across sustainability and transformation partnerships in England; 2019 [cited 2021 Mar]. Available from: https://www.strategyunitwm.nhs.uk/sites/default/files/2019-11/Exploring%20Mental%20Health%20Inpatient%20Capacity%20accross%20Sustainability%20and%20Transformation%20Partnerships%20in%20England%20-%20191030_1.pdf
- National Institute of Health and Care Excellence. NICE health technology evaluations: the manual. Process and methods [PMG36]; 2022. Available from: https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation
- Oxehealth. Patient experience with Oxevision; 2022 [cited 2022 Jun]. Available from: https://assets-global.website-files.com/5f567869171c90518f161723/624af4d6379d9a1d18fdbf85_PER_UK_D_8.1.pdf
- National Institute of Health and Care Excellence. Guide to the methods of technology appraisal 2013: the reference case; 2013 [cited 2021 Mar]. Available from: https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781
- Personal Social Services Research Unit (PSSRU). Unit Costs of Health & Social Care 2020. Canterbury: University of Kent; 2020 [cited 2021 Mar]. Available from: https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2020/
- Personal Social Services Research Unit (PSSRU). Unit Costs of Health & Social Care 2017. Canterbury: University of Kent; 2017 [cited 2021 Mar]. Available from: https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2017/
- NHS Improvement. 2019/20 National Tariff Payment System; 2020.
- Pilowsky LS, Ring H, Shine PJ, et al. Rapid tranquillisation: a survey of emergency prescribing in a general psychiatric hospital. Br J Psychiatry. 1992;160(6):831-835.
- NHS England. National Schedule of NHS costs 2018/19; 2020 [cited 2021 Mar]. Available from: https://www.england.nhs.uk/national-cost-collection/#ncc1819
- British National Formulary. Haloperidol: BNF; 2021 [cited 2021 Mar]. Available from: https://bnf.nice.org.uk/medicinal-forms/haloperidol-decanoate.html
- British National Formulary. Promethazine hydrochloride: BNF; 2021 [cited 2021 Mar]. Available from: https://bnf.nice.org.uk/medicinal-forms/promethazine-hydrochloride.html
- NHS Sussex Partnership. The Rapid Tranquillisation Policy (including the use of oral PRN medication); 2019 [cited 2021 Mar]. Available from: https://www.sussexpartnership.nhs.uk/sites/default/files/documents/rt_-_rapid_tranquilization_-_jan_2019_ratified_final_circulated.pdf
- Higgins JP, Li T, Deeks JJ. Choosing effect measures and computing estimates of effect; 2021 [cited 2021]. Available from: https://training.cochrane.org/handbook/current/chapter-06
- Pereira SM, Sarsam M, Bhui K, et al. The London Survey of Psychiatric Intensive Care Units: service provision and operational characteristics of National Health Service Units. J Psychiatr Intensive Care. 2005;1(1):7–15.
- NHS Improvement. The incidence and costs of inpatient falls in hospitals; 2017 [cited 2021 Feb 8]. Available from: https://web.archive.org/web/20201229074130/https://improvement.nhs.uk/documents/1471/Falls_report_July2017.v2.pdf