Abstract
Background and aims
Patients on acute adult and older adult inpatient mental health wards are at an increased risk of accidental injuries and deliberate harm to self and others. A vision-based patient monitoring and management (VBPMM) system was designed by Oxehealth Limited to support ward staff to provide better and more efficient care and to reduce incidents. The VBPMM system uses an infrared-sensitive camera, installed in a patient’s room, that works with cleared medical device software to deliver contact-free vital sign and activity insights to clinical teams. Data from two studies undertaken at an English National Health Service (NHS) mental health trust were used to inform an early economic assessment of VBPMM implementation into acute adult and older adult mental health wards.
Methods
A cost calculator was used to compare the introduction of the VBPMM system as an adjunct to standard care versus standard care alone. Observational data were collected at two English NHS mental health trusts. Both compared data pre- and post-VBPMM implementation using a 12-month baseline period. The model estimated cost per occupied bed day, cost per patient, annual cost per average-sized ward, and total cost to NHS mental health trusts across England. Costs were modeled from an NHS perspective over a 12-month time horizon. Scenario analysis was conducted to test the uncertainty of results using statistical significance of key inputs.
Results and conclusions
This early analysis indicated that the VBPMM system is likely to be cost saving within both settings examined, with an estimated cost saving of £272 per acute adult mental health patient and £4,591 per older adult mental health patient. This translates to £22.3 and £63.3 million, respectively, across NHS mental health trusts in England every year. VBPMM, therefore, has the potential to augment standard care, leading to positive clinical outcomes and monetary savings.
Introduction
Delivering safe, high quality and efficient inpatient care is a challenge for the National Health Service (NHS) in England, particularly when considering stretched funding and resources. During 2020/2021 alone, approximately 2.8 million people in England were in contact with NHS-funded secondary mental health, learning disability, or autism servicesCitation1. During the same year, NHS England spent £2.2 billion on specialized commissioning for mental health services, in addition to the £12.1 billion spent by local Clinical Commissioning Groups (CCGs) on mental health, learning disability, and dementia servicesCitation1.
Acute adult mental health and older adult mental health hospitals for dementia face challenges associated with patient safety, such as falls, assaults, self-harm, and suicide. Providing care for patients in these hospitals is particularly costly as they are at an increased high risk of accidental injuries and deliberate harm to self and others. Staff are required to spend a large majority of their work time keeping them safe and, in many cases, observations are required every 15 minutes, including during the night. Frequent observations are very disruptive, particularly in these vulnerable patient populations. It is important to ensure these hospitals have a strong culture of patient safety, achieved, for example, through adequate staffing and a ward infrastructure that enables proactive patient careCitation2.
Approximately 50% of English NHS mental health trusts have implemented a vision-based patient monitoring and management (VBPMM) system called Oxevision, developed by Oxehealth Limited, to support the delivery of proactive patient careCitation3. The VBPMM system aims to help clinicians deliver safer, higher quality, and more efficient care, when used alongside standard practices. It is contact-free and its hardware (an infrared-sensitive camera) is mounted to the wall of ward bedrooms in a secure housing unit. The system enables remote measurement of a patient’s vital signs (pulse rate and breathing rate) and notifies staff when a patient may need help or assistance via activity- and location-based alerts. For example, when a patient is spending a prolonged period of time by a doorway or in the bathroom, which may indicate self-harming behavior, or when a patient is getting out of bed, which may indicate a fall risk. Information from the system is made available to clinicians through portable tablets and a monitor in the nurses’ station.
A series of staff surveys, focus groups, and interviews were undertaken on 22 inpatient mental health wards in eight NHS mental health trusts to evaluate the outcomes of VBPMM implementation. Analysis of the data revealed improvements in patient and staff safety, care quality, the management of patient risk, the identification of potential incidents, and in the enhancement of patients’ perceived sense of privacy and dignity due to observations by staff being less intrusive, particularly at nightCitation4.
An analysis of working time in mental health hospital personnel demonstrated that psychiatric intensive care units (PICUs) and older adult wards were the two most resource-intensive settings, particularly when nursing staff time was consideredCitation5. An economic analysis of the VBPMM system as an adjunct to standard care for adult patients within one PICU has recently been published and demonstrated the potential for cost savingsCitation6. The current economic evaluation builds on this previous work and aims to assess the costs and outcomes associated with introducing VBPMM in a wider range of inpatient mental health services. Specifically, two settings were examined: an acute adult mental health inpatient hospital and an older adult mental health inpatient hospital for dementia.
Methods
Data collection
Data underpinning the analysis were obtained from published and unpublished observational studies conducted at Coventry and Warwickshire Partnership NHS Trust (CWPT). For the purposes of this study, observational data were collected before and after VBPMM implementation.
In the acute adult mental health hospital, the VBPMM system was implemented on one 22-bedroom female ward and one 20-bedroom male ward, and the VBPMM system was used over a 12-month study period and compared to a 12-month pre-VBPMM period. The results of this pilot study have not yet been published. The study did not collect patient numbers, given the focus was specifically on beds within a ward. However, assuming a length of stay equivalent to 48 days (see ), this would be approximately 300 patients both before and after the introduction of VBPMM.
Table 1. Scaling inputs for application of model results.
In the older adult mental health hospital for dementia, the VBPMM system was implemented on one 12-bedroom female ward and one 12-bedroom male ward. The system was used in half of the bedrooms over a 22-month study period and compared to a 12-month pre-VBPMM periodCitation10. The study for the older adult population also did not collect patient numbers. However, assuming a length of stay equivalent to 82 days, this would be approximately 90 patients before and 170 patients after the introduction of VBPMM.
The number of beds, occupancy rates, and number of wards in the study population are presented in .
The clinical outcomes recorded before and after the introduction of VBPMM in each of the studies were: number of night-time observations, night-time observation time per patient, number of one-to-one observation hours, number of night-time falls (older adult population only), and number of self-harm incidents (acute adult population only). No power analysis was conducted in either study due to the early nature of the analysis. All functions of the VBPMM previously detailed were included when using the technology, such as infrared-sensitive camera, vital signs monitoring, and alert systems.
Model structure
The analysis was conducted in line with the National Institute of Health and Care Excellence (NICE) reference caseCitation13. The focus of the analysis was on costs and reduction in clinical events, in line with the NICE approach to evaluating medical technologiesCitation13. In the base case, costs were modeled from the perspective of the NHS in England and Personal Social Services (PSS) over a 12-month time horizon and no discount rate was applied. Discounting was not applied because the analysis considers a time horizon of 1 year, meaning costs do not need to be converted to a net present value, as per the NICE reference caseCitation13. This time horizon was used for the analysis to adequately reflect both the benefits of VBPMM and its costs, which is based on an annual subscription model. Quality-of-life was not captured within the economic model, which is reflected by the NICE reference case for evaluating medical devicesCitation13. Scenario analyses conducted from alternative perspectives of CCGs and mental health trusts are provided in the Supplementary Material. At the time of analysis, CCGs were still in place within the NHS; these groups were statutory bodies that led the planning of healthcare services in local areas, which would have separate healthcare budgets to the specific mental health trust. The impact of introducing VBPMM is likely to be similar for integrated care systems (ICSs), which replaced CCGs in July 2022Citation14.
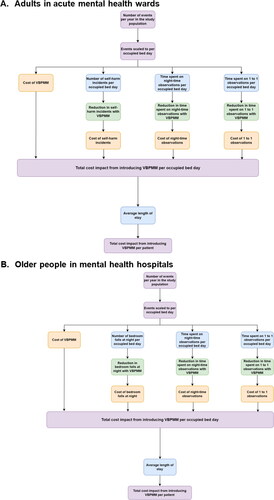
The overall model structure has been described previouslyCitation6. Briefly, the model was a cost calculator comparing the VBPMM system plus standard care versus standard care alone and built in Microsoft Excel (Microsoft Corporation). Outcomes for the two populations are presented separately.
The outcomes of interest were scaled to “per occupied bed day” to provide a common modeling time frame that can be easily converted to per-patient outcome by using average length of stay. The model results can also be presented per ward (based on available ward size and bed occupancy data) or for NHS mental health trusts across England as a whole. The model captured the costs of night-time observations and one-to-one observations for both groups. Other data captured were night-time bedroom falls in older adult mental health inpatients only, and self-harm incidents for the acute adult mental health inpatients only (). The costs associated with length of hospital stay were not included in the analysis due to paucity of data; that is, no difference could be observed in the study data between treatment arms. For both populations, serious incidents, such as severe assaults or severe falls, were also excluded due to insufficient numbers for statistical analysis.
Model inputs
Model inputs were informed by two observational studies on the clinical effectiveness of the VBPMM system undertaken at CWPT, one publishedCitation10 and one unpublished, and by literature searches to inform specific parameters. Costing was based on standard UK sources from the NHS Reference Costs and Personal Social Services Research Unit (PSSRU)Citation15,Citation16.
Clinical inputs
The number of clinical outcomes occurring with standard care, as well as the impact of the VBPMM system on the incidence of these events, were derived from the two CWPT observational studies described aboveCitation10,Citation11,Citation17. Outcomes from the studies were scaled to per occupied bed day, enabling model results to be presented per patient, per average sized ward, and for NHS mental health trusts across England as a whole, using the scaling inputs shown in .
Inputs related to clinical events captured in the model and to the reduction in their incidence after introduction of the VBPMM system are presented in . The effectiveness of the VBPMM system was assumed not to vary with ward size. Staff time needed to manage self-harm events in the acute adult population and night-time bedroom falls in the older adult population was sourced from a series of interviews with mental health hospital staff, details of which are provided in the Supplementary Material.
Table 2. Clinical inputs.
Several assumptions were made in relation to clinical data included in the model. First, the cost of all self-harm incidents and falls resulting in accidents and emergency (A&E) visits were, for simplification, assumed to be equivalent to minor fractures, potentially underestimating the associated costs. Second, the clinical data informing the model were generated at a single NHS Trust, and it was assumed that the outcomes are directly transferable to other similar settings. Finally, some events were considered “not applicable” to each population. This is because the VBPMM system is configured to support managing the main risk factors on the wards, which differs by population; therefore, not all events were captured for each population. For example, bedroom falls were considered a major risk for older adult mental health inpatients but not for adults in acute mental health wards. Therefore, alerts related to getting out of bed were not switched on for adults in acute mental health wards
Cost inputs
Cost inputs for an average ward (16 beds) are presented in . NHS Reference Costs 2018/19 were used for proceduresCitation15 and the 2020 PSSRU data were used for staff costsCitation16, except for the costs for a Healthcare Assistant, which were inflated from PSSRU 2017Citation19 using the NHS cost inflation pay and prices inflation indices, as the relevant data are not available in more recent iterations of the PSSRU publication.
Table 3. Costs inputs.
The upfront costs of implementing the VBPMM were annuitized over the 10-year lifespan of the intervention and 1 year of the annuitized cost was considered within the model, in line with the time horizon used for the analysis.
Outcomes generated by the model
The model estimated cost per occupied bed day, cost per patient, cost per average-sized (16-bed) ward per year, and total cost to NHS mental health trusts across England. Costs were calculated for each model arm (standard care and VBPMM plus standard care) as well as incrementally.
Scenario analyses
A threshold analysis was performed to evaluate the potential breakeven point from introducing VBPMM when only one-to-one observations were considered. These events may require additional staff (for example from a staffing agency) beyond the core ward personnel, so part of the cost of one-to-one observations is expected to be cash releasing, while the remainder represents only an opportunity cost as the core staff time becomes available for other tasks. Cash releasing and overall savings were considered separately in this scenario analysis. If VBPMM potentially reduces one-to-one observations, then it can reduce both cash releasing costs and opportunity costs.
An additional scenario analysis was performed only for the acute adult mental health inpatient population, for which the confidence interval or reduction in one-to-one observations with VBPMM in the unpublished study was wide and crossed zeroCitation8, suggesting a high level of uncertainty surrounding the relevant effectiveness estimate. In this scenario analysis, one-to-one observation hours were not considered in the model, while night-time observations and self-harm incidents were retained. In the older adult mental health inpatient population, all clinical events of interest to the model were significantly reduced with the use of VBPMMCitation10,Citation11,Citation17, so an analogous scenario analysis was not performed in this population. The confidence intervals for the scenario analysis in the acute adult mental health inpatient population are presented in , which are calculated from the relevant clinical study.
Table 4. Confidence intervals for the population of adults on acute mental health wards.
Results
Base case results
Acute adult mental health inpatient population
The introduction of VBPMM in an average-sized acute adult mental health inpatient ward was estimated to result in annual cost savings of £29,827 per ward per year, translating to a saving of £272 per patient. When scaled to NHS mental health trusts across England as a whole, the cost savings in this population were estimated to reach over £22 million per year (). The cost breakdown highlights that the key driver of cost savings is the reduction in one-to-one observations, which are estimated to reduce by around 15 hours per patient per year with the introduction of VBPMM ().
Table 5. Base case results.
Table 6. Clinical events per patient per year.
Older adult mental health inpatient population
The introduction of VBPMM in an average-sized older adult mental health inpatient ward was estimated to lead to cost savings of £294,501 per ward per year, or £4,591 per patient. The savings scaled across NHS mental health trusts in England were estimated at over £63 million per year (). The cost breakdown highlights that the key driver of cost savings is the reduction in one-to-one observations, as well as a 48% reduction (1.14 falls per patient with standard care and 0.59 per patient with VBPMM) in bedroom falls at night per patient which can be costly to manage ().
Scenario analysis results
Threshold analysis was conducted to assess the effect of introducing VBPMM on the costs of one-to-one observations. In the acute adult mental health inpatient population, a 33% reduction in one-to-one observations was needed to break even in-year when only the cash releasing savings were considered. This is higher than the 20% reduction in one-to-one observations incorporated in the model base case. When all potential cost savings were considered (including opportunity costs), a 7% reduction in one-to-one observations was estimated to be sufficient to break even. In the older adult mental health inpatient population, a 52% reduction in one-to-one observations was estimated to be sufficient to break even when considering cash releasing savings alone, and a 2% reduction when considering all cost savings. Both of these figures were substantially lower than the base case reduction in one-to-one observations in this population (71%).
In the second scenario analysis performed for the acute adult mental health inpatient population, one-to-one observations were no longer considered in the model, as the reduction in these events after VBPMM introduction did not reach statistical significance in the source study. This analysis resulted in VBPMM no longer providing cost savings (). This scenario was not conducted for the older adult mental health inpatient population, given all events were statistically significant.
Table 7. Scenario analysis for adults on acute wards excluding one-to-one observations.
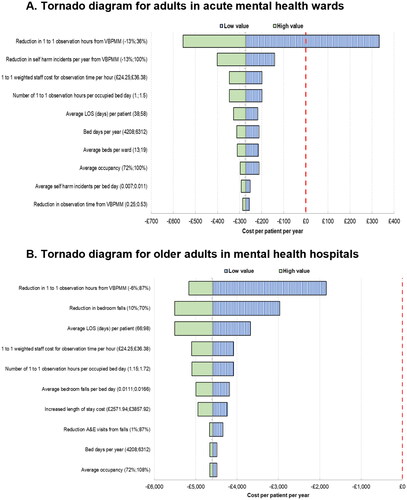
Deterministic sensitivity analysis was conducted to further explore the key drivers of the model results with respect to VBPMM. The results of this analysis are presented in .
As shown in the tornado diagram, the key drivers of the results are the effectiveness of VBPMM in reducing one-to-one observations and other events in the respective populations, such as bedroom falls in the older adult mental health inpatient population, average length of stay per patient, as well as the baseline number of one-to-one observation hours.
Discussion
The introduction of VBPMM to supplement standard care was shown to save costs when evaluated in acute adult wards and in older adult wards in mental health hospitals. Cost savings were estimated in both populations and were substantially higher in the latter: £272 per acute adult patient vs £4,591 per older adult patient, which translates to approximately £63.3 million and £22.3 million, respectively, across NHS mental health trusts in England.
In terms of cost breakdown, the largest driver of cost savings was a reduction in one-to-one observation time in both populations, and a reduction in night-time falls in the older adult population. The potential reduction in one-to-one observation time warrants particular attention as a proportion of these hours often requires additional agency and bank staff, whose employment is costly and its reduction represents a cash releasing opportunity for the NHS. Indeed, threshold analysis demonstrated that a 33% reduction in one-to-one observations for acute adult mental health inpatient wards and a 52% reduction for the older adult mental health inpatient wards were sufficient to generate cash releasing savings for an average sized ward. It is important to note that the proportion of one-to-one observation hours that are potentially cash releasing was based on data from a single NHS Trust, and in those settings where reliance on external staff is higher, the cash releasing break-even point for VBPMM introduction is likely to be lower.
The COVID-19 pandemic caused a surge of interest in remote patient monitoring in general. For example, a recent systematic review described three studies and six ongoing clinical trials that predominantly utilized commercially available wearable devices to monitor physical activity, sleep, heart rate, and ambient light exposure in patients with depressionCitation21. Unlike commercially available wearable devices, the VBPMM system is contact-free and cannot be readily removed by the patient; in addition, it provides alerts to potentially high-risk activities, such as getting out of bed, and also enables remote measurement of vital signs that staff can use as part of clinical practice to improve safety and care planning. In the initial assessments of VBPMM implementation versus standard of care, staff using the system perceived an improvement in care quality and in patient risk management when routine care was augmented with VBPMMCitation4,Citation8,Citation11,Citation17, while patients reported feeling safer, experiencing better quality of sleep, and having a greater sense of privacy and dignity with less physical presence of staff in their roomCitation22. Potential ethical concerns about privacy are important when considering the practical aspects of implementing this intervention. There is no video feed continuously displayed with the VBPMM system and video feed can only be viewed when taking vital sign measurement or when responding to an alert for up to 15 s. When responding to an alert, only anonymized blurred video is available. Patients are informed about the use of the system and can request for it to be turned offCitation10.
Finally, there is approximately a 17% nursing vacancy rate in mental health inpatient hospitalsCitation23 and some wards struggle to meet their minimum safe staffing levels with substantive staff. Due to this intervention, wards may be able to better manage staffing strain while maintaining safety and care for patients.
A previous early analysis has already suggested that cost savings can be achieved by implementing the VBPMM system in PICUs alongside routine careCitation6. The results from our current analysis suggest the same in two other patient populations. The technology therefore has the potential to augment standard care, bringing in both positive clinical outcomes and monetary savings, including cash releasing savings from reduction in agency or bank staff hours and the opportunity for cost savings as core staff can use their time in other ways.
This model aimed to assess the potential cost savings over a 1-year period of implementing the VBPMM system as an adjunct to routine care. However, some of the long-term benefits of the technology were not captured due to insufficient data being available. Consequently, the model estimates are likely to be conservative. An example of the events not captured by the model include the downstream health risks of fractures in the older adult mental health inpatient population, such as rehabilitation, repeat fractures, and venous thromboembolism. For the acute adult mental health inpatient population, self-harm incidents were assumed to result in minor injuries only and, therefore, the model did not capture more serious and long-term health issues. Further, the costs of litigation due to self-harm incidents or falls were not captured, but these cases are likely to be rare. Data from Surrey and Borders Partnership NHS Foundation TrustCitation24 indicate that, if serious incidents are represented by a proxy of suicides, only approximately 0.7% of self-harm incidents would be classed as serious and potentially lead to a litigation. Finally, the model takes an approach of a simple cost calculator. A full cost-utility analysis could formally capture patient-reported outcomes, providing a more comprehensive picture of the benefits associated with VBPMM introduction.
Other limitations of the model relate to its underlying assumptions. The data collected in a single NHS trust were assumed to be generalizable across other similar settings without taking into consideration the differences in staffing or patient mix, which could affect the baseline event rate and, therefore, the cost savings produced by the VBPMM system. The use of average length of stay to obtain patient-level data in the model is associated with a similar limitation as the length of stay will differ between trusts, resulting in variability of actual per-patient benefits.
Effectiveness inputs for the current analysis were derived from early pilot studies with limited sample size. Since the reduction in one-to-one observations was not statistically significant in the pilot study conducted in the acute adult mental health setting, a sensitivity analysis excluding this outcome was performed, in which VBPMM no longer provided cost savings. This result indicates the need for continued collection of real-world data that could reduce the uncertainty associated with the outcomes of implementing the technology and help to identify those wards and hospitals which are most likely to benefit from it.
Conclusions
The results of the current early analysis suggest that augmenting standard care with VBPMM produces cost savings for NHS England when treating older adults in mental health hospitals, and adults on acute mental health wards. Larger-scale real-world studies of VBPMM will aim to more robustly evaluate the potential benefits of this intervention.
Transparency
Declaration of funding
York Health Economics Consortium (YHEC) was funded by Oxehealth to develop the economic model and manuscript.
Declaration of financial/other relationships
RM, JS, and AS are employed by YHEC.
Author contributions
FN and KW were the chief and principal investigators, respectively, in the clinical study of Oxevision. RM and JS were involved in the conceptualization and design of the economic model. The analyses were undertaken by RM and JS. RM drafted the manuscript with critical revision from JS, AS, FN, and KW. All authors approved the final version.
Supplemental Material
Download MS Word (33.8 KB)Acknowledgements
Medical writing and editorial assistance with the preparation of this manuscript was provided by Karolina Badora.
Michelle Green was previously involved in the conceptualization of the economic model to evaluate the cost savings of the vision-based patient monitoring and management system in PICUs
Daniel Bayley helped to provide insight into the technology, the clinical evidence, and how the technology is used in clinical practice. He also provided feedback on the draft manuscript.
Data availability statement
To request the original data regarding Oxevision please contact [email protected]
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Baker C. House of Commons Library. Mental Health Statistics (England) 13 December. 2021; cited 18 June 2022]. Available from https://researchbriefings.files.parliament.uk/documents/SN06988/SN06988.pdf.
- Alshowkan A, Gamal A. Nurses’ perceptions of patient safety in psychiatric wards. IOSR-JNHS. 2019;8(1):1–8.
- Lloyd-Jukes H, Gibson OJ, Wrench T, et al. Vision-based patient monitoring and management in mental health settings. J Clin Eng. 2021;46(1):36–43.
- Oxehealth. Staff experience with Oxevision; [cited 2022 June 19]. Available from: https://assets-global.website-files.com/5f567869171c90518f161723/62569a353b4937643a0ac093_SER_UK_D_8.1.pdf.
- Wolff J, McCrone P, Berger M, et al. A work time study analysing differences in resource use between psychiatric inpatients. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1309–1315.
- Malcolm R, Shore J, Stainthorpe A, et al. Economic evaluation of a vision-based patient monitoring and management system for working-age people in psychiatric intensive care units in England. J Med Econ. 2022;25(1):1101–1109.
- Hospital Episodes Statistics. Hospital Admitted Patient Care Activity 2019–20. 2020; [cited 2021 February 08]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2019-20.
- Coventry and Warwickshire Partnership NHS Trust How technology can change services; [cited 2022 June 19]. Available from https://assets-global.website-files.com/5f567869171c90518f161723/5f7e0bad1a06a32e1da2a3ab_qnpicu–-webinar-presentation-flyer–17-july-2020.pdf.
- The Strategy Unit NHS. Exploring Mental Health Inpatient Capacity across Sustainability and Transformation Partnerships in England. 2019. Available from: https://www.strategyunitwm.nhs.uk/sites/default/files/2019-11/Exploring%20Mental%20Health%20Inpatient%20Capacity%20accross%20Sustainability%20and%20Transformation%20Partnerships%20in%20England%20-%20191030_1.pdf.
- Wright K, Singh S. Reducing falls in dementia inpatients using vision-based technology. J Patient Saf. 2022;18(3):177–181.
- Coventry and Warwickshire Partnership NHS Trust Safer dementia care in Mental Health hospitals; [cited 2022 June 19]. Available from https://assets-global.website-files.com/5f567869171c90518f161723/5f7dd0a836242101825e6c2b_safer_dementia_care.pdf.
- James K, Stewart D, Wright S, et al. Self harm in adult inpatient psychiatric care: a national study of incident reports in the UK. Int J Nurs Stud. 2012;49(10):1212–1219.
- National Institute for Health and Care Excellence. Process and methods [PMG36]. NICE health technology evaluations: the manual. 2022; [cited 2022 August 1]. Available from https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation.
- Charles A, Wenzel L, Kershaw M, et al. A year of integrated care systems. Reviewing the journey so far, 2018. Available from https://www.kingsfund.org.uk/sites/default/files/2018-09/Year-of-integrated-care-systems-reviewing-journey-so-far-full-report.pdf.
- NHS England. National Schedule of NHS costs 2018/19. Available from: https://www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/.
- Curtis L, Burns A. Unit Costs of Health & Social Care 2020. Personal Social Services Research Unit, University of Kent, Canterbury. 2020. Available from https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2020/.
- Coventry and Warwickshire Partnership NHS Trust. Reducing falls in mental health hospitals 2020; [cited 19 June 2022]. Available from https://assets-global.website-files.com/5f567869171c90518f161723/5f7dd15445648b998ebf3715_CWPT_48-falls-reduction.pdf.
- NHS Improvement. The incidence and costs of inpatient falls in hospitals 2017; [cited 2021 February 08]. Available from: https://improvement.nhs.uk/documents/1471/Falls_report_July2017.v2.pdf.
- Curtis L, Burns A. Unit Costs of Health & Social Care 2017. Personal Social Services Research Unit, University of Kent, Canterbury; 2017.
- NHS Improvement. 2019/20 National Tariff Payment System. 2020. Available from: https://improvement.nhs.uk/resources/national-tariff/.
- Sakamaki T, Furusawa Y, Hayashi A, et al. Remote patient monitoring for neuropsychiatric disorders: a scoping review of current trends and future perspectives from recent publications and upcoming clinical trials. Telemedicine and e-Health. 2022.
- Oxehealth. Patient experience with Oxevision; [cited 2022 June 20]. Available from: https://assets-global.website-files.com/5f567869171c90518f161723/624af4d6379d9a1d18fdbf85_PER_UK_D_8.1.pdf.
- NHS Vacancy Statistics. Experimental Statistics. May 2022. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey/april-2015–-march-2022-experimental-statistics#.
- Surrey and Borders Partnership NHS Foundation Trust. Freedom of information act: Absconding, Self-Harm and Suicide over the Last 5 Financial Years. 2018; [cited 2021 February 08]. Available from https://www.sabp.nhs.uk/application/files/6215/2906/6016/5475_Absconding_Self-Harm_and_Suicide_over_the_Last_5_Financial_Years.pdf.