Abstract
Aims
This study aimed to analyze the cost-effectiveness of intradiscal condoliase injection compared to surgical or conservative treatment for patients with lumbar disc herniation (LDH) who are refractory to conservative treatment.
Methods
We performed the following cost-effectiveness analyses: (I) condoliase followed by open surgery (for non-responders to condoliase) vs. open surgery from the beginning, (II) condoliase followed by endoscopic surgery (for non-responders to condoliase) vs. endoscopic surgery from the beginning, and (III) condoliase + conservative treatment vs. conservative treatment. In the first two comparisons with surgical treatments, we assumed that utilities were equal in both groups and estimated the tangible (treatment, adverse events, postoperative follow-up) and intangible (mental and physical burden, and productivity loss) costs based on the existing literature, the medical expense scoring table, and online questionnaire. In the last comparison without surgical treatment, we estimated the incremental cost-effectiveness.
Results
The average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) was 701,643 yen, with a reduction of 663,369 in comparison to that of open surgery from the beginning (1,365,012 yen). The average cost per patient of condoliase followed by endoscopic surgery (for non-responders to condoliase) was 643,909 yen, with a reduction of 514,909 in comparison to that of endoscopic surgery from the beginning (1,158,817 yen). ICER was 1.58 million yen/QALY (ΔQALY = 0.119, 95% confidence interval: 0.059–0.180; Δcost = 188,809 yen at 2 years post-treatment).
Conclusions
Condoliase as a first line treatment option ahead of surgical treatment for LDH is superior, from a cost perspective, to surgical treatment from the beginning. Condoliase is also a cost-effective alternative to non-surgery conservative treatment.
Introduction
Lumbar disc herniation (LDH) is a degenerative spinal disease that can cause symptoms such as low back pain, leg pain, and numbness, which further result in the physical burden on daily life and the associated loss of work opportunities and economic lossCitation1–5. While approximately 90% of LDH cases improve with conservative treatment such as medication and physical therapyCitation6,Citation7, cases refractory to this treatment type are conventionally indicated for surgery.
As an intermediate therapy between conservative and surgical treatments, intradiscal condoliase injection (HernicoreFootnotei, covered by insurance in Japan in 2018) provides a treatment option. Condoliase reduces hernia-induced nerve root compression via local injection into the intervertebral disc to break down chondroitin sulfate that makes up the nucleus pulposus of the disc, thereby reducing the pressure within the discCitation8. Condoliase is minimally invasive and can be administered on an outpatient basis or during an overnight stay. Therefore, condoliase is expected to reduce inpatient medical costs and provide benefits, such as reduced productivity loss, decreased wound size, and decreased treatment-associated pain duration.
Although accumulating evidence on the efficacy and safety of condoliase vs. placebo existsCitation9,Citation10, cost-effectiveness analyses comparing condoliase as a first line treatment option versus surgical or conservative treatment options is lacking. The absence of such health economic information can be a barrier for clinicians to decide on treatment strategies. In this study, we conducted cost-effectiveness analyses to visualize the value of condoliase from a health economic perspective to assist treatment decision-making.
Methods
Study design
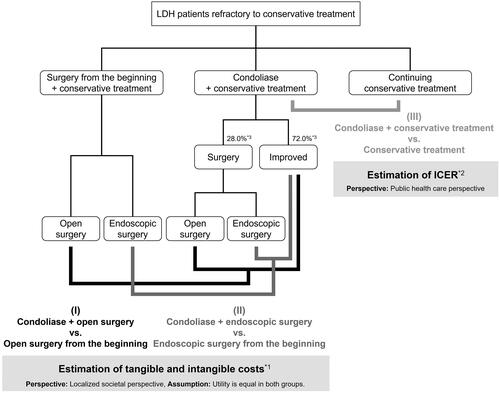
We performed the following three cost-effectiveness analyses for LDH patients, who were refractory to conservative treatment (): (I) condoliase followed by open surgery (for non-responders to condoliase) vs. open surgery from the beginning, (II) condoliase followed by endoscopic surgery (for non-responders to condoliase) vs. endoscopic surgery from the beginning, and (III) condoliase followed by conservative treatment vs. conservative treatment. In the first two analyses with surgical treatments, we assumed that utility was equal in both groups and estimated both tangible and intangible costs from a localized social perspective based on the existing literature, a medical expense scoring table, and the result of an online questionnaire with conjoint cards. Similarly, in the third analysis, we estimated the incremental cost-effectiveness ratio (ICER) from a public health care standpoint. We conducted an online survey prior to the cost-effectiveness analyses to estimate the intangible costs of each treatment and the proportion of inpatient versus outpatient use of condoliase (referred to as the in/out ratio), in which a preference survey with conjoint cards and an additional survey of each treatment-experienced patient were conducted simultaneously for calibration.
Figure 1. Schematic diagram of the study design. *1A cost comparison was performed between surgery for patients with inadequate efficacy at 13 weeks after condliase treatment and surgery from the beginning. If the efficacy is equal in both groups, the cost after the second year of treatment can be considered equivalent. Therefore, the analysis period was set to one year. Since conservative treatment is no longer necessary once patients are completely cured, medical costs for conservative treatment were calculated by setting an upper limit on the number of treatment. *2The time horizon for this analysis was set at 2 years. As a sensitivity analysis, the efficacy at 3 and 4 years after treatment were also calculated. Since QOL data during longer condliase treatment than 1 year were not available, the analysis was performed assuming that the QOL at 1 year in this analysis persisted. It was assumed that conservative treatment in the condliase group remained the same for two years after condliase administration as in the conservative treatment group (conservative conditions unfavorable to condliase). Therefore, medical costs for conservative treatment would be offset in both groups. *3The response rate for condoliase was assumed to be 72.0%, which is the response rate at 13 weeks after treatment with condoliase (95% CI: 62.2–81.7%)Citation9, and the remaining 28.0% were assumed to undergo open surgery at 13 weeks.
Assumptions in the cost analyses in (I) and (II)
In (I), we assume that utility is equal in both groups. Posterior resection (Love method) was considered open surgery, while micro endoscopic discectomy (MED method) was considered endoscopic surgery, currently the most common surgical or endoscopic technique for LDHCitation11,Citation12. We estimated tangible (treatment, adverse events, and postoperative follow-up) and intangible costs (mental and physical burden, and productivity losses) from a localized societal perspective. The response rate for condoliase was assumed to be 72.0%, which is the response rate at 13 weeks after treatment with condoliase (95% CI: 62.2–81.7%)Citation9, and the remaining 28.0% were assumed to undergo open surgery at 13 weeks.
Tangible costs were calculated using a stacking method based on a standard medical process, in consultation with an orthopaedic surgeon. We used the medical expense scoring table of April 2021 for calculations. Since condoliase has both inpatient and outpatient patterns, the medical costs were calculated by weighting the patient ratio based on an online survey. Since adverse events in the condoliase and placebo groups were similarCitation9,Citation10, their medical costs were not included in the tangible costs for condoliase. The frequencies of adverse events were estimated from existing published studiesCitation9–12. Postoperative follow-up costs were the costs of two treatment-related outpatient visits.
Intangible costs were calculated based on an online survey. Productivity loss was calculated as the product of lost workdays and wages. For lost wages, the average wage for all industries, ages, and genders (307,700 yen/month) from the latest Basic Survey on Wage Structure in 2020 was utilized. The employment rate of those aged 18 years and over was assumed to be 100%. For lost workdays, we used the average number of days from the online survey of patients receiving condoliase and open surgery. For sensitivity analysis, productivity loss was also calculated using the results of discharged patients survey in 2019 published by the Ministry of Health, Labour and Welfare [MHLW] to evaluate the impact of the Diagnosis Procedure Combination (DPC) introduction (average length of stay for endoscopic surgery: 10 days, open surgery: 16 days). In this regard, the average length of hospital stay multiplied by 5/7 was the number of lost workdays. Intangible costs other than productivity loss were calculated using a conjoint analysis of a public online survey. The average responses in the questionnaires for patients who received each treatment was used for calibration.
If the efficacy is equal in both groups, the cost after the second year of treatment can be considered equivalent. Therefore, the analysis period was set to one year. Owing to the short analysis period, the discount rate for costs was not considered in this study. The cost analysis in (II) was calculated using the same method as in (I).
Assumptions in the cost-effectiveness analysis in (III)
We compared the cost and effectiveness of condoliase and conservative treatment from the beginning vs. conservative treatment alone from a public health care standpoint. Due to expected improvement in symptoms in the former, its medical costs after condoliase should be lower than those of the latter. However, we conservatively assumed that the medical costs for conservative treatment would be offset in both groups and that the cost difference between the two groups was the medical costs for condoliase and post treatment follow-up (two visits).
Efficacy was calculated by converting the eight subscale decompositions of the 36-Item Short Form Health Survey (SF-36)Citation13 at 13 and 52 weeks after treatment, as reported inCitation9 into quality of life (QOL) as previously describedCitation14. The time horizon for this analysis was set at 2 years since prognostic results during longer term than 52 weeks were only available up to approximately 2 years. The efficacy at 2 years after treatment was calculated by linear interpolation under the assumption that QOL did not change for both after 1 year of treatment. According to prognostic analyses of domestic Phase II/III trials, there was no significant change in disc height between the placebo and condoliase groups in the final treatment evaluation (at 52 weeks after treatment) and the prognostic study evaluation (mean time of 25.7 months). Based on these findings, the aforementioned assumption and analysis periods were established. As a sensitivity analysis, the efficacy at 3 and 4 years after treatment were also calculated with the same assumption as above.
Although adverse-event related medical costs were not included in the cost analysis for the same reasons as in (I), a sensitivity analysis was performed for reference, considering anaphylaxis, neutropenia, lymphadenitis, and allergic reactions, all of which are serious adverse events associated with condoliase. Since the analysis period was short (2 years or up to 4 years for sensitivity analysis) and accurate values after 52 weeks could not be referenced at this time, the discount rate for cost and utility was not considered.
Internet questionnaire survey
Data sources and analysis populations
The online survey was conducted from 5 to 14, January 2022, on a panel (INTAGE Inc.), who had given their survey consent in advance. The following populations were included in the analysis: individuals between 20 and 70 years of age in the general panel who were randomly selected based on the distribution of the entire Japanese population (400 targets, group 1); and patients in the low back pain panel with a history of LDH diagnosis and invasive treatment where condoliase or endoscopic/open surgery was defined as invasive treatment (400 targets, group 2). In group 2, the patients were randomly selected with the condoliase: endoscopic surgery: open surgery ratio of 2:1:1. Medical professionals, advertising agencies, research organization workers, and their families were excluded. Only those who answered all questions were considered respondents, all of whom were included in the analysis. Group 1 also included some patients in the low back pain panel for representation of LDH distribution in the general population. In the Japanese healthcare system, medical fees are revised every two years, most recently in April 2021. For the two years after the revision, the medical cost is the same for the same surgery for the same disease. Therefore, medical costs are calculated as of April 2021. Whereas intangible costs such as productivity loss were calculated as of January 2022, after the start of the study, because they need to be calculated through a questionnaire survey.
Survey methods
The respondents to the online survey were first given a specific and thorough explanation of the medical condition and symptoms of LDH using illustrations. They were asked to envision a situation in which they needed to undergo invasive treatment because conservative treatment showed no improvement. In practice, after explaining the medical condition, we asked them to assume the following situation: “Assume that you have lumbar disc herniation. When you carry something heavy, bend over, cough, or sneeze, you experience severe pain from the low back to the legs. You have been treated for three months with analgesic agents to suppress the pain, but there has been no improvement. When you consulted your doctor, he suggested treatment for the hernia itself, since the pain could not be controlled with analgesic agents.”
Conjoint cards with one-to-one comparisons were then presented to respondents. The attributes and levels of conjoint cards are listed in . The six attributes included wound size, treatment-associated pain duration, treatment-associated pain level, anesthesia method, response rate, and co-payment based on interviews with a medical specialist. We used the six-level Wong-Baker FACES Pain Rating Scale (0–5) for the pain evaluation. The response rate was defined as the percentage of back or leg pain due to hernia that improved by more than half after treatment, which is the same definition as responder rate in ofCitation9.
Table 1. Attributes and levels of conjoint cards.
Table 2. An example of a conjoint card used in the online survey.
While there are 972 level combinations, we limited the combinations presented to each respondent according to orthogonal programming to reduce the survey burden of the respondent. Each respondent was presented with two different cards and asked to choose a preferred card. Twenty sets of conjoint cards were presented for each respondent. An example of a conjoint card is presented in . The utility values were calculated by regression analysis of the respondents’ data, and the monetary value of each attribute level was estimated by comparison with the utility of co-payment. In addition, for each patient in group 2, additional questions were asked after the conjoint card selection about the wound size of the treatment (mm), treatment-associated pain duration (days), treatment-associated pain level (six levels from 0 to 5), and number of lost workdays (days) (all in integer-value response format). Respondents who had experienced condoliase were also asked to indicate whether they were treated in an inpatient or outpatient setting.
Statistical analysis
Intangible costs were calculated by converting each attribute level into monetary terms using a conjoint analysis (conditional logit model) for the general public in the online survey and calibrating it with the results of additional questions for patients in group 2. Because (I) and (II) were cost analyses, the response rate, which is a utility, was excluded. The total of the four items of wound size, level and duration of treatment-associated pain, and anesthesia method was used as the intangible costs. Because this study was a treatment cost analysis and did not aim to align and compare patients’ background factors, no confounding adjustment of the questionnaire results was performed in the calibration.
We also estimated the impact of the change in response rate to condoliase, the revised medical expense from April 2022, the shortening of hospitalization for surgical treatment, and a change to the in/out ratio of condoliase treatment on the study results for sensitivity analyses. SAS ver. 9.4, and Microsoft Excel 2016 were used for the analysis.
Ethical review
We submitted an ethics application and obtained approval before conducting the online survey because of the risk that research subjects, particularly those with hernia, may experience psychological distress from recalling memories of their illness or treatment during the survey, which falls under the category of minor invasion in the “Guidance on Ethical Guidelines for Life Science and Medical Research Involving Human Subjects” (RIHDS Ethics Review Committee, Receipt No. RI2021019). In addition, the UMIN clinical trial registration was also conducted (UMIN study ID: 000046417). To minimize emotional distress to survey respondents, an opt-out option was offered before the survey began. Those who were unwilling to respond did not have to respond or could stop in the middle of their response.
Results
Summary of main results
The average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) was 701,643 yen, with a reduction of 663,369 in comparison to that of open surgery from the beginning (1,365,012 yen). The average cost per patient of condoliase followed by endoscopic surgery (for non-responders to condoliase) was 643,909 yen, with a reduction of 514,909 in comparison to that of endoscopic surgery from the beginning (1,158,817 yen). ICER was 1.58 million yen/QALY (ΔQALY = 0.119, 95% confident interval [CI]: 0.059–0.180, Δcost = 188,809 yen at 2 years post-treatment). The details of the results are as follows.
Questionnaire survey results
Group 1 included 423 respondents (mean age 46.1 years (standard deviation [SD] 13.5), 50.1% female), matching the Japanese population distribution. Group 2 included 433 respondents (mean age 55.6 years (SD 13.6), 25.4% female). The treatment breakdown was as follows: 216 condoliases, 109 endoscopic surgeries, and 108 open surgeries. The male:female ratio for each treatment was approximately 3:1.
A conjoint analysis in group 1 yielded the utility and intangible costs for each attribute level, as shown in and . The level and duration of pain, and response rate tended to be more important than the size of the wound or anesthesia method. Conjoint analysis was also performed for those who experienced invasive treatment as a sensitivity analysis, which showed similar results, except for the statistically insignificant preference for general over local anesthesia.
Figure 2. ΔIntangible cost of each attribute. The results of the conjoint analysis in are visualized on the wound size, pain duration, pain level, and the response rate with linear interpolation between each level.
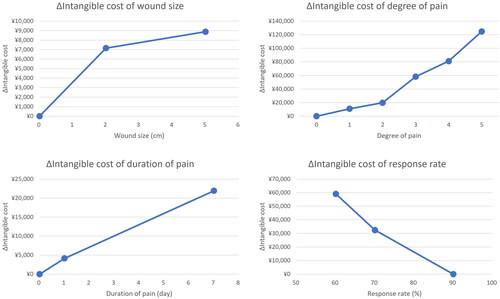
Table 3. Results of the conjoint analysis for group 1.
The aggregate results for each treatment-experienced respondent in group 2 are presented in . Responses that were clearly considered outliers were excluded (treatment-related pain duration of 365 days, n = 1). The in/out ratio of patients treated with condoliase was 63/153 (29.2%/70.8%). The intangible costs for analyses (I) and (II) were calculated as the difference from α (the intangible cost in the case of wound size, 0 mm; treatment-associated pain level, 0; treatment-associated pain duration, 0 days; and anesthesia method, local anesthesia), which can be considered almost 0. Calibration was performed using a linear interpolation of the conjoint analysis results.
Table 4. Results of the questionnaire for group 2.
Cost analysis results in (I) and (II)
The average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) was 701,643 yen, with a reduction of 663,369 in comparison to that of open surgery from the beginning (1,365,012 yen), as shown in . The factors contributing to the cost difference were in the following order of importance: treatment (523,372 yen, of which the difference in surgery cost was 32,655 yen), productivity loss (144,086 yen), adverse events (7,091 yen), follow-up (–3,531 yen), and intangibles (–7,649 yen). The average cost per patient of condoliase followed by endoscopic surgery (for non-responders to condoliase) was 643,909 yen, with a reduction of 514,909 in comparison to that of endoscopic surgery from the beginning (1,158,817 yen), as shown in . The factors contributing to the cost difference were in the following order of importance: treatment (441,047 yen, of which the difference in surgery cost was 82,119 yen), productivity loss (99,777 yen), adverse events (–937 yen), follow-up (–3,531 yen), and intangibles (–21,448 yen).
Table 5. Results of the cost analyses.
The estimated medical costs for condoliase were 142,701 yen for outpatient treatment, 214,001 yen for inpatient treatment, and 25,312 yen for two postoperative follow-ups (detailed summary in Table S1, Supplementary Material). Adverse-event related medical costs were estimated at 2,685 yen for outpatient and 2,336 yen for inpatients (). For each adverse event, we assumed the following: anaphylaxis, two days and one night of inpatient care; neutropenia, one more return visit and five additional outpatient blood tests with follow-up; lymphadenitis, spontaneous resolution within 2 months from onset with three more examination follow-ups; skin symptoms, skin rash appeared the day after treatment and healed after 10 days of anti-allergic medication and ointment (detailed summary in Table S2, Supplementary Material).
Table 6. Frequency of adverse events and medical costs of condoliase.
The estimated medical costs for surgery were 953,985 yen for open surgery, 839,645 yen for endoscopic surgery, and 30,252 yen for two postoperative follow-ups (detailed summary in Table S3, Supplementary Material). Adverse-event related medical costs were estimated at 13,436 yen for open surgery and 2,286 yen for endoscopic surgery (). For each adverse event, we assumed the following: dural injury, no increase in medical costs other than intraoperative material costs for both procedures; caudal disorder, hospital stay increased by 28 days for both procedures; nerve root disorder, hospital stay increased by 7 days for both procedures; postoperative hematoma, hospital stay increased by 10 days for both procedures; deep wound infection, hospital stay increased by 28 days for both procedures; tooth damage, crown fractures that do not require nerve treatment and require two outpatient treatments; misidentification of level for endoscopic surgery, no additional medical costs due to intraoperative correction; articular process fracture for endoscopic surgery, pain persists for 1 month and is followed up with analgesics; conversion to open surgery from endoscopic surgery, no additional medical cost is incurred because the reimbursement score for endoscopy is higher and the higher reimbursement score is adopted (detailed summary in Table S4, Supplementary Material).
Table 7. Frequency of adverse events and medical costs of surgery.
Cost analysis results in (III)
ΔQALY at 2 years post-treatment for the placebo group was 0.119 (95% CI: 0.059–0.180, Δcost = 188,809 yen). The ICER was 1.58 million yen/QALY < 5 million yen/QALY (threshold), indicating that condoliase was cost-effective. ΔCost was calculated as a weighted average of the medical cost of condoliase performed in inpatient and outpatient settings, weighted by the in/out ratio of those who experienced condoliase according to the questionnaire results (details on QOL changes after condoliase treatment in ).
Table 8. QOL changes after condoliase treatment.
Sensitivity analysis
In the cost analysis, when the number of lost workdays was calculated as 5/7 of the average length of hospital stay, the average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) changed from 701,643 to 597,517 yen, the average cost per patient of open surgery from the beginning changed from 1,365,012 to 1,190,942 yen, with a change in the cost difference from 663,369 to 593,425 yen. Similarly, the average cost per patients of condoliase followed by endoscopic surgery (for non-responders to condoliase) changed from 643,909 to 544,706 yen, the average cost per patient of endoscopic surgery from the beginning changed from 1,158,817 to 1,002,230 yen, with a change in the cost difference from 514,909 to 457,624 yen. Also, when the response rate at 13 weeks after treatment with consoliase varied within the 95% confidence interval of 62.2 to 81.7%Citation9, the average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) varied from 569,237 to 835,414 yen. Similarly, the average cost per patients of condoliase followed by endoscopic surgery (for non-responders to condoliase) varied from 531,503 to 757,473 yen.
For the cost-effectiveness analysis in (III), we performed sensitivity analyses by changing the measurement period and considering adverse events. When the time periods were set at 3 and 4 years post-treatment, ΔQALY was 0.188 (95% CI: 0.094–0.282) and 0.257 (95% CI: 0.129–0.385) respectively. The ICER was 1.00 million and 0.74 million yen/QALY respectively. ΔCost was assumed to be unchanged by the extended measurement period because it is derived from costs within one year after treatment. When adverse events were considered, ΔICER increased by 21,662 yen/QALY at 2 years post-treatment, compared to that of groups without adverse-event adjustment.
We then estimated how the revision of medical service expenses starting in April 2022 would affect the results of the analysis. When calculated based on new reimbursement points with the piece-rate payment method, the average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) changed from 701,643 to 701,043 yen, the average cost per patient of open surgery from the beginning changed from 1,365,012 to 1,359,996 yen, with a change in cost difference from 663,369 to 658,953 yen. Similarly, the average cost per patient of condoliase followed by endoscopic surgery changed from 643,909 to 643,224 yen, the average cost for endoscopic surgery (for non-responders to condoliase) from the beginning changed from 1,158,817 to 1,153,499 yen, with a change cost difference from 514,909 to 510,275 yen. The ICER in changed from 1.58 million to 1.59 million yen/QALY.
Since inpatient treatment for condoliase has been newly added to the diagnosis group classification of the Diagnosis Procedure Combination (DPC) since April 2022, we further conducted a cost analysis using the comprehensive payment method. The average cost per patient of condoliase followed by open surgery (for non-responders to condoliase) changed from 701,643 to 657,293 yen, whereas the average cost per patient of open surgery from the beginning changed from 1,365,012 to 1,225,639 yen, resulting in a change of cost difference from 663,369 to 568,345 yen. Similarly, the average cost per patient of condoliase followed by endoscopic surgery (for non-responders to condoliase) changed from 643,909 to 611,343 yen, and the average cost per patient of endoscopic surgery from the beginning changed from 1,158,817 to 1,061,532 yen, resulting in a change in cost difference from 514,909 to 450,189 yen. Medical fees under the DPC system in Japan are divided into a comprehensive evaluation part and a stacking evaluation part. The former includes general hospitalization fee and some additional fees for general hospitalization, and is calculated as the product of number of points per day per diagnosis group, coefficient per medical institution (sum of functional evaluation coefficient I, functional evaluation coefficient II, basic coefficient, and mitigation coefficient for drastic changes), number of days in hospital, and 10 (yen). The latter mainly includes costs such as examinations, rehabilitation, procedures, surgery, and anesthesia. The average number of hospitalization days was set as Day II (national average number of hospitalization days) in the comprehensive evaluation. The medical institution coefficients were calculated using the following assumptions: the function evaluation coefficient I = sum of the additions estimated to be applicable, the function evaluation coefficient II = national average of DPC standard hospital groups, basic coefficient = basic coefficient of DPC standard hospital groups, and mitigation coefficient for drastic changes = 0.
We next examined the impact of shortened hospitalization on surgical treatment. In recent years, the average length of hospital stay has been gradually shortening owing to minimally invasive treatment, early ambulation and rehabilitation, and the influence of the reimbursement system. According to the patient survey conducted by the MHLW in 2017, the length of hospital stay has been reduced by approximately 0.6 days each year over the past decades. Although we used the national average length of hospital stay for surgical treatment of 10 days (endoscopic surgery) and 16 days (open surgery) in 2019 in the cost analysis, we further examined the impact of a shorter hospital stay, given that hospitalization costs generally account for a large proportion of medical costs. Assuming that the length of hospital stay was shortened by one day in each case, the average cost of condoliase and open surgery under the piece-rate payment method would change from 701,643 to 694,525 yen (a 1.0% decrease), and the average cost of open surgery from the beginning would change from 1,365,012 to 1,339,592 yen (a 1.9% decrease), resulting in a change in cost difference from 663,369 to 645,067 yen. Similarly, the average cost of condoliase and endoscopic surgery would change from 643,909 to 634,655 yen (1.4% decrease), whereas the average cost of endoscopic surgery from the beginning would change from 1,158,817 to 1,125,767 yen (2.9% decrease), resulting in a change in cost difference from 514,909 to 491,113 yen.
Finally, we examined the effect of the in/out ratio on condoliase activity. In this study, the in/out ratio of condoliase (the percentage of hospitalizations to the total) was calculated as 29.2% from the results of the survey. To examine the impact of this change in the in/out ratio on the results of the analysis, we performed a cost analysis for each case with an in/out ratio of 0% (all outpatient treatment) and 100% (all inpatient treatment). The average cost of condoliase and open surgery changed from 701,643 to 680,847 and 752,147 yen, respectively, and the cost difference changed from 663,369 to 684,165 and 612,865 yen, respectively. Similarly, the average cost of condoliase and endoscopic surgery increased from 643,909 yen to 623,113 yen and 694,413 yen, respectively, and the cost difference increased from 514,909 yen to 535,705 yen and 464,405 yen, respectively. The ICER in analysis (III) changed from 1.58 million to 1.41 million and 2.01 million yen/QALY, respectively.
Discussion
This is the first report for revealing that treatment with condoliase was less expensive than surgical treatment due to the avoidance of long hospitalization associated with surgical treatment among the 72% of patients whose LDH is expected to resolve after treatment with condoliase. In contrast, analysis (III) showed that condoliase is a cost-effective treatment compared to conservative treatment in cases where surgical treatment is not a prerequisite.
The reasons condoliase was not implemented for patients who were refractory to conservative treatment may include the patient’s psychological resistance to the potential lack of responsiveness to condoliase, the patient’s physical and psychological stress of undergoing further surgery, the physician’s lack of understanding of the treatment, and physicians’ psychological resistance to implementing a treatment that may not be effective. However, this study indicated that even after considering the physical and psychological burden of patients, it is more economical to perform condoliase treatment first, when the patient is to undergo surgical treatment. Even in the absence of surgical treatment, condoliase treatment was cost-effective compared to conservative treatment. Therefore, the value of condoliase may have been underestimated.
In this study, we recorded available standard deviations and confidence intervals for the surveys and known literature data. While the medical costs are point estimates based on medical validity with no clear consensus, the cost differences between therapies were accounted for by treatment costs that are less sensitive to the patients’ background, such as hospitalization charges and other hospitalization and rehabilitation factors. Therefore, a slight change in estimates would not have a sufficiently large impact to overturn the comparative results. In fact, even if the estimated costs were to independently increase or decrease by a range of 25% (i.e. changes in the range 75–125%) in each group, the comparison results in analyses (I) and (II) would remain the same, and the ICER in (III) would still be below the threshold of 5 million yen/QALY. In addition, adverse-event related medical costs can vary greatly, depending on the severity of the event. However, the incidence is so low that even if the treatment differs slightly, the impact on overall costs is expected to be small. Sensitivity analyses were also conducted in terms of productivity loss, hospital stay duration, analysis period, adverse events, response rate to condoliase, revision of medical service expenses, shortened hospitalization, and the in/out ratio of condoliase. However, changes in each condition did not significantly affect the results of the cost analysis.
Regarding the online survey, we need to focus on treatment-associated wound size, and age as a possible confounding factor for lost workdays. The average wound size was 20.4 mm for those who had experienced condoliase, which is very large for an injection scar. Since the patients could not see the treatment site in the back, they might have recognized the size of the wound dressing as the wound size. The intangible cost of wound size is approximately 10,000 yen, even for a 5 cm wound, with an extremely small contribution to the overall cost. The number of lost workdays could be particularly affected by age due to the average difference in the treatment invasiveness among treatment-experienced patients used in the calibration. To verify this possibility, we performed an age-adjusted regression analysis, in which age was used as a reference explanatory variable for the sensitivity analysis. After adjustment, the mean number of lost workdays was 6.5, 22.0, and 29.0 days for the condoliase, endoscopic surgery, and open surgery groups, respectively, with no significant adjustment-dependent impact. Therefore, treatment was not correlated with age.
Study limitations
This study has limited external validity as there was selection bias for the respondents, who were limited to panel members of a research firm.
This study has limited internal validity for the following reasons. First, there may have been a bias due to scenario misspecifications, in which the intended setting of the disease or treatment may not have been communicated well to the respondents. Second, there may have been also a bias due to the implied value cues. For example, respondents may be strongly influenced by out-of-pocket costs or may focus only on certain attributes to reduce response time. Third, there may have been a bias caused by the respondents intentionally presenting false answers. Fourth, there is a recall bias. When being asked about past experiences, respondents may provide different answers than they actually did, depending on their ability to recall the past. However, all these limitations are considered to have little effect on the results in this study, because the findings in (I) and (II) were driven by the avoidance of the surgical procedure, and changes in the in/out ratio in (III) had only a small effect on the results.
Conclusions
From a cost perspective, condoliase as a first line treatment option ahead of surgical treatment for LDH patients who are refractory to conservative treatment is superior to surgical treatment from the beginning. In the same patient group without surgical treatment, condoliase also represents a cost-effective alternative to conservative treatment.
Transparency
Declaration of funding
This study was supported by Kaken Pharmaceutical Co., Ltd.
Declaration of financial/other relationships
MI received consultancy fees from Kaken Pharmaceutical Co., Ltd. ST and HM are employees of Kaken Pharmaceutical Co., Ltd. The authors have no other relevant affiliations or financial involvement with any organization or associations that have a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Author contributions
ST and HM contributed to the study conception. All authors contributed to the study design and interpretation of findings. All authors commented on the previous versions of the manuscript. All authors approved the final version of the manuscript for submission.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Previous presentations
There is no previous presentation.
Supplemental Material
Download MS Excel (58.7 KB)Acknowledgements
We thank Ms. Elizabeth Anne Jackson at Milliman and Dr. Yoshiaki Kita at Medical Professional Relations Inc. for writing and editorial support of this manuscript. We also thank INTAGE Healthcare Inc. for the execution of the online survey and Editage for English language editing.
Notes
i Hernicore is a registered trademark of Seikagaku Corp., Tokyo, Japan.
References
- Deyo RA, Mirza SK. Clinical practice. Herniated lumbar intervertebral disk. N Engl J Med. 2016;374(18):1763–1772.
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367.
- Alonso-García M, Sarría-Santamera A. The economic and social burden of low back pain in Spain: a national assessment of the economic and social impact of low back pain in Spain. Spine. 2020:45(16): e1026–e1032.
- Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96(1 Suppl):34–44.
- Olafsson G, Jonsson E, Fritzell P, et al. Cost of low back pain: results from a national register study in Sweden. Eur Spine J. 2018;27(11):2875–2881.
- Ito T, Takano Y, Yuasa N. Reduction of the number of herniotomies by conservative treatment. Rinsho Seikei Geka. 2001;36:487–490. Japanese.
- Kawabata M. Lumbar disc herniation. Rinsho Seikei Geka. 1989;24:825–831. Japanese.
- Matsuyama Y, Chiba K. Condoliase for treatment of lumbar disc herniation. Drugs Today. 2019;55(1):17–23.
- Chiba K, Matsuyama Y, Seo T, et al. Condoliase for the treatment of lumbar disc herniation: a randomized controlled trial. Spine. 2018;43(15):E869–E876.
- Matsuyama Y, Chiba K, Iwata H, et al. A multicenter, randomized, double-blind, dose-finding study of condoliase in patients with lumbar disc herniation. J Neurosurg Spine. 2018;28(5):499–511.
- Matsumoto M, Hasegawa T, Ito M, et al. Annual Report 2008 of the spinal endoscopic surgery in Japan. J Jpn Orthop Assoc. 2009;83(12):1022–1027. Japanese.
- Imajo Y, Taguchi T, Yone K, et al. Nationwide Survey for spine surgery in Japan 2013. J Spine Res. 2013;4(9):1367–1379. Japanese.
- Fukuhara S, Suzukamo Y. Manual of SF-36v2 Japanese Version. Kyoto: Institute for Health Outcomes and Process Evaluation Research; 2004.
- Ara R, Brazier J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available). Value Health. 2008;11(7):1131–1143.
- Abdullah F, Bai A, Sahil F, et al. Lumbar disc herniation: comparing pain relief after medical and surgical intervention. Cureus. 2021;13(6):e15885.
