Abstract
Objective
This study aimed to assess the comorbidity profile, use of health care resources and medical costs of patients with chronic obstructive pulmonary disease (COPD) treated at the hospital level in Spain.
Methods
Admission records of patients with COPD and at least two admissions registered between January 2016 and December 2020 were obtained from a Spanish hospital discharge database and analyzed in a retrospective multicenter study.
Results
95,140 patients met the inclusion criteria; 69.1% were males with a median age of 75 years. Mean Charlson comorbidity index (CCI) was 1.9 in the index admission, increasing to 2.1 during the follow-up period. An acute exacerbation of COPD was registered in 93.6% of patients in the index admission; other secondary diagnoses included respiratory failure (56.8%), essential hypertension (36.9%), hypercholesterolemia (26.7%) and diabetes (26.3%). The age-adjusted incidence rate of COPD was 22.6 per 10,000 persons over the study period, decreasing significantly in the year 2020. Mortality rate was 4.1% for COPD patients, increasing to 6.6% in the year 2020. The year 2020, 191 patients registered a COVID-19 infection, with a mortality rate of 23.0%. Length of hospital stay, and intensive care unit (ICU) stay increased in the follow-up period versus the index admission, similar to admission costs. Mean admission cost was €3212 in the index admission, with cost increases being associated with age, length of stay, ICU stay and CCI.
Conclusions
Patients’ condition worsened significantly over the follow-up period, in terms of comorbidity and dependence on respirator, with an increased mortality rate and higher admission costs.
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogenous disease, characterized by a persistent airflow obstruction and other symptoms that include chronic cough, chest congestion and tirednessCitation1. Although disease severity is variable, these symptoms can critically affect patients’ quality of life; in this direction, a group of patients surveyed in a European cross-sectional observational study described variable symptoms that had an impact on daily activitiesCitation2. In addition, acute infectious and non-infectious exacerbations of the disease are associated with an accelerated decline in lung function, morbidity and mortalityCitation3.
COPD is the third leading cause of death worldwide and is a major cause of disabilityCitation4. The prevalence of COPD varies regionally and is highly dependent on air pollution and tobacco use; in Spain prevalence of COPD was 9.1% in adults in the year 1997, as estimated in the context of the IBERPOC studyCitation5,Citation6. This data was updated in the context of the EPISCAN study in 2007, which found a prevalence of 14.6%, and the EPISCAN II study, which defined a prevalence of COPD of 11.8% in the population aged 40 years or olderCitation7,Citation8. The same study found a high rate of underdiagnosed COPD cases in the Spanish population, which was the highest (80.6%) in women aged 40 or olderCitation8. Mortality in patients with COPD is frequently attributed to other causes, complicating mortality rate estimations, and great variability has been described between countries; nevertheless, data suggest that mortality rates could increase globally as the global population agesCitation9.
In terms of diagnosis and treatment, specific guidelines are issued by national and international expert groups including recommendations for the diagnosis and management of COPD; the Global Initiative for Chronic Obstructive Lung Disease (GOLD), updated in 2019, included revised evidence for pharmacological treatment recommendations, reflecting a shift towards a more personalized approachCitation10. At the Spanish level, the Spanish COPD Guidelines (GesEPOC), updated in 2021, recommendations include diagnosis, determination of risk level, initial and subsequent inhaled therapy and identification and management of treatable traitsCitation11. In addition, a Spanish clinical practice consensus in internal medicine was elaborated focusing on the treatment of stable COPD and COPD with exacerbation in patients with multimorbidityCitation12. Despite the availability of specific guidelines, data suggest a low adherence to COPD management guidelines in Spain, a situation that could be associated with increased healthcare costsCitation13.
COPD represents a substantial economic burden globally, with total costs that could increase with the aging of the populationCitation14. For this reason, understanding the burden of COPD is essential for an efficient management of the disease.
The objective of this study was to analyze the characteristics, use of health care resources and medical costs associated to a COPD cohort treated in Spanish hospitals with a 5-year follow-up period.
Methods
Study setting and data extraction
Admission records of patients with COPD and admitted in Spanish hospitals between 1 Jan 2016 and 31 Dec 2020 were analyzed in a retrospective cohort study. Records were extracted from a Spanish National discharge database, which covers 90% of hospitals in Spain and includes data from all Spanish regions. All hospital admissions in which COPD was registered as the admission motive were claimed by means of the corresponding International Statistical Classification of Diseases and Related Health Problems, 10th version (ICD-10) codes: J40–J47.9Citation15. Information about prescription drugs was obtained from a primary care registry, using the International Classification of Primary Care, second edition (ICPC-2) code corresponding to COPD: R95Citation16.
Data codification, evaluation and confidentiality are the responsibility of centers. The database is validated internally and subjected to periodic audits, eliminating errors and unreliable data. All identifying parameters were re-coded to keep patient data anonymous as stated in the principles of Good Clinical Practice and the Declaration of Helsinki. This study did not involve any human subjects and there was no identifiable information. Thus, Spanish legislation does not require ethics committee approval or patient consentCitation17.
Study variables
The variables extracted from the hospital discharge database were: patient’s age and sex, region of origin, date of admission, type of admission, ICU admission and time of stay, date of discharge, type of discharge (including death), department, primary diagnosis, up to 20 secondary diagnoses registered during the admission, medical procedures and total admission cost. Data on prescription medication, extracted from a primary care registry, was only available for the years 2017 and 2018.
Data analysis
Individual patients were identified using a re-coded patient identifier, patients with only one admission during the study period were excluded. The first admission per patient registered over the study period was considered the index admission; all subsequent admissions registered during the study period were considered in the follow-up period.
Age-adjusted incidence rate corresponded to the annual number of registered cases of COPD within the total population. Mortality rate was calculated as the number of deaths registered in patients with COPD within all patients treated at the hospital level during the study period.
Direct medical costs of hospital care were obtained from the database, where they are assigned to each admission file according to the standardized average expenses of admissions and medical procedures determined by the Spanish Ministry of Health (including all expenses related to the admission: examination, medication, surgery, diet, costs associated to personnel, medical equipment and resources). Direct medical costs were assigned to an admission depending on the diagnostic-related group assigned to the admission and include information from the billing system. Costs were adjusted for inflation in Spain during the study period.
Normality was assessed with the Kolmogorov–Smirnov test. The mean or median and interquartile range (IQR) were estimated for continuous variables and frequencies and percentages are reported for dichotomous variables. Chi-squared tests were used for the analysis of differences between categorical variables, Mann-Whitney U test or one-way analysis of variance was conducted, where appropriate, and two-sample Z-tests were also conducted to test for differences in sample ratios, with p < .05 being considered statistically significant. The association of secondary conditions to hospital mortality was assessed using the odds ratio (OR) with 95% confidence interval (CI), with the group of patients non-deceased during the hospitalization as the reference group, and the Spearman correlation test was used to test the correlation between age, length of stay, Charlson’s comorbidity index and medical costs. A general linear model was used to adjust the age to calculate age-adjusted incidence rate. Statistical analyses were performed using Microsoft Excel© Professional Plus 2010 (Microsoft Corporation, Redmond, WA, USA) and StataSE 12 for Windows (StataCorp LP. 2011. Stata Statistical Software: Release 12. College Station, TX, USA).
Results
Patient characteristics
Files corresponding to 95,140 individual patients were obtained from the database. Median age was 75 (interquartile range [IQR] = 11) years and 69.1% of the patients were males (). Patients were primarily obtained from centers located in the northwestern or central region of Spain.
Table 1. Patient baseline characteristics.
Patient comorbidity profile was evaluated in the index admission and in the admissions registered in the 5-year follow-up period, summing 311,736 admissions over the study period (). Mean Charlson’s comorbidity index (CCI) was 1.9 in the index admission, increasing to 2.1 during the follow-up period (p < .0001) (). Most of the admissions registered an acute exacerbation of COPD, including infective exacerbation. The most frequent secondary diagnoses registered during the admission were a respiratory failure, essential hypertension, hypercholesterolemia, diabetes mellitus, heart failure and hypertensive heart and kidney disease, all increasing in frequency over the study period except for essential hypertension. Additionally, 20.0% of the patients were smokers and 31.7% had a history of tobacco use on the index admission. The proportion of patients requiring a respirator (ventilator), supplemental oxygen or another enabling device increased significantly over the study period (p < .0001).
Figure 1. Cohort Charlson comorbidity index (a), length of hospital stay (b), mortality rate (c) and mean admission cost (d) in the index and subsequent admissions with 95% confidence interval.
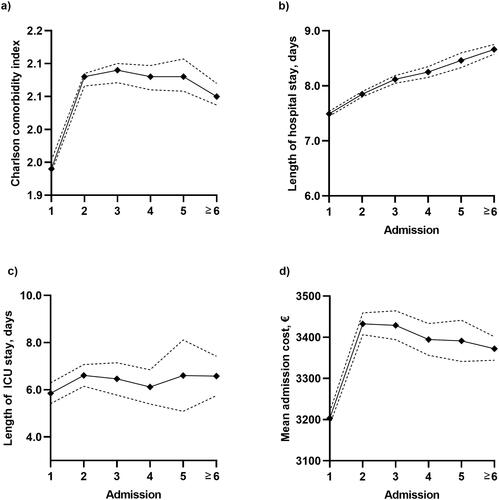
Table 2. Patient comorbidity profile in the index admission vs. the 5-year follow-up period.
In addition, 191 patients registered COVID-19 as a secondary diagnosis of COPD. The mortality rate in this group was 23.0% (Table S1). Spearman correlation coefficients showed that there was no statistically significant correlation between age, length of stay, Charlson’s comorbidity index and medical costs (Table S2).
Incidence and mortality
The age-adjusted incidence rate of COPD measured at the hospital level was 22.6 per 10,000 inhabitants over the study period. The incidence of COPD in Spanish hospitals decreased significantly the year 2020 (p < .0001) ().
Figure 2. Age-adjusted incidence of COPD per 10,000 inhabitants (a) and in-hospital mortality rate (b) between 2016 and 2020 with 95% confidence interval.
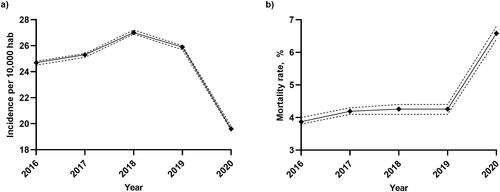
The overall in-hospital mortality rate associated to patients with COPD in the database was 4.1%, increasing significantly in the year 2020, to 6.6% (p < .0001) (). The average mortality rate in this cohort increased significantly in follow-up admissions versus the index admission, increasing from 2.0% to 10.0% (p < .0001). In addition, the mortality rate in patients admitted due to an acute exacerbation of COPD was 11.4%.
Cause of death was not formally disclosed, but heart failure (OR, 95%CI = 2.3282, 2.2373–2.4227), respiratory failure (OR, 95%CI = 3.4092, 3.2462–3.5805), kidney disease (OR, 95%CI = 2.9013, 2.7882–3.0189), malignant neoplasm (OR, 95%CI = 3.3399, 3.1907–3.4960) and pneumonia (OR, 95%CI = 2.2702, 2.1740–2.3706) were associated with in-hospital mortality.
Health care resource utilization and costs
Health care resource utilization was analyzed in the index admission and in the follow-up period (). Mean length of hospital stay was 7.5 days, increasing significantly during the follow-up period (p < .0001) (). Only 2.0% of admissions included a stay in an intensive care unit (ICU), with a mean stay of 5.9 days, increasing too in the follow-up period (p = 0.0232) (). Admissions were predominantly registered in internal medicine and pneumology departments.
Table 3. Health care resource utilization in the index admission vs. the 5-year follow-up period.
The medical procedures registered during the admission included the introduction of anti-infective and other therapeutic substances, the measurement of arterial saturation, assisted ventilation and imaging diagnostic procedures. In addition, prescription drugs were obtained from a primary care database. The most frequently prescribed drugs were antibacterial agents and inhalants for obstructive airway diseases, theophylline was prescribed to 11.7% of patients (). About 40% of patients were prescribed agents acting on the renin-angiotensin system and antithrombotic agents.
Table 4. Prescription medication registered in primary care settings (2017–2018).
Mean admission cost increased significantly in the follow-up period versus the index admission (p < .0001) (). Mean admission cost was €3212 in the index admission, €3415 during the follow-up period (). Age (p < .0001), length of stay (p < .0001), ICU stay (p < .0001) and CCI (p < .0001) were associated with medical costs. In addition, mean admission cost in patients with a COVID-19 infection increased to €4973 (p < .0001).
Table 5. Direct medical costs in the index admission vs. the 5-year follow-up period.
Discussion
This retrospective study found that the age-adjusted incidence rate of COPD was 22.6 per 10,000 persons over the study period, with a mortality rate of 4.1%, increasing to 6.6% in the year 2020. In the year 2020, 191 patients registered a COVID-19 infection, with a mortality rate of 23.0%. Length of hospital stay, and intensive care unit (ICU) stay increased in the follow-up period versus the index admission, similar to admission costs. Mean admission cost was €3212 in the index admission, with cost increases being associated with age, length of stay, ICU stay and CCI.
The study included data from 95,140 patients with COPD admitted in Spanish hospitals over a 5-year period, providing data on patients’ condition and medical costs. Most patients included in the study (59.2%) were aged 65 to 84 years, and 69.1% were males. Numerous comorbid conditions were identified, with a mean CCI of 1.9. A previous cross-sectional study evaluating the clinical characteristics of patients newly diagnosed with COPD in the region of Catalonia described a highly comorbid populationCitation18. In addition, patients’ overall condition worsened significantly in this study during the follow-up period, as reflected in the increased CCI and the frequency of diagnoses.
Age-adjusted incidence of COPD at the hospital level was 22.6 per 10,000 persons over the study period, decreasing significantly in the year 2020. A study analyzing COPD exacerbations via a survey developed in a Spanish hospital during the 2020 lockdown found a strong reduction in COPD exacerbations during that period, presumably due to a protective effect against viral and bacterial infections, and air pollutants, provided by self-protective and general measuresCitation19. On the other hand, the in-hospital mortality rate increased significantly in the year 2020, when considering all patients in the hospital discharge database. Further studies will be required to analyze the reasons behind this increase, which could be related to changes in management protocols due to the COVID-19 pandemic. Risk factors for mortality in the COPD cohort included heart failure, respiratory failure, kidney disease, malignant neoplasm, and pneumonia, as well as an acute exacerbation of COPD. In addition, patients with COVID-19 admitted the year 2020 displayed an increased mortality rate, reaching 23.0%.
The increasing comorbidity found in the follow-up period correlated with lengthier hospital stays. The most frequent medical procedures registered during the admission were the introduction of anti-infective and other therapeutic substances. Assisted ventilation was only registered in 8.0% of follow-up admissions.
Pharmacological interventions for COPD are generally focused on inhaled therapies to reduce exacerbation risk; these include bronchodilator therapy with a long-acting muscarinic antagonist (LAMA) or long-acting β2-agonist (LABA), and inhaled corticosteroidsCitation10,Citation20. Guidelines recommend using combinations of these treatments to patients with persistent symptoms or exacerbationsCitation10. Data obtained from primary care showed a high portion of patients with prescribed antibacterial drugs, as well as adrenergics and other inhalants.
Direct medical costs were evaluated at the hospital level, with a mean admission cost of €3212, increasing in patients’ follow-up period and by the length of hospital stay. Annual direct medical costs per patient in Europe ranked from €1906 ($1889) in Spain to €11,893 ($11,787) in Norway in a systematic review, however, data corresponding to Spain was obtained from a single regionCitation21,Citation22. In another Spanish study, including patients with COPD and concomitant bronchiectasis, hospital admission costs were €3813 for males and €3769 for females between 2012 and 2014Citation23. Data obtained in the present study would suggest a decreasing trend in hospital admission costs in Spain.
In addition, data gathered the year 2020 showed a significant increase in medical costs in patients with a concomitant COVID-19 infection.
A new study analyzed the impact of COVID-19 in the diagnosis and treatment of COPD during the pandemicCitation24. This study assessed the experience of 279 pulmonologists and the results showed that the diagnostic test was reduced by a 68.1%, and there was a lower adherence to treatment. Another important point was that the election of treatment was based on the device ease of use, to increase adherence. In addition, as expected, the number of remote visits increased.
Other interesting publications have assessed the sex differences in COVID-19 hospitalizations and mortality in patients with COPDCitation25. This study found that the in-hospital mortality was higher in women with COPD but has no effects on men with COPD. On the other hand, men with COPD with COVID-19 had a 25% higher risk of dying in the hospital than women.
Regarding costs, a study published in 2017 has assessed the mortality predictive power of BODE (body mass index, obstruction, dyspnea, and exercise performance) by adding total health care cost related to exacerbations or hospitalizations to the BODE indexCitation26. This study yielded two key findings; it showed that adding the number of exacerbations and hospitalizations to the BODE index improves the ability to predict mortality over three years of follow-up and found that this updated BODE index (PRO-BODE) also allows to project the future healthcare costs.
A series of limitations have influenced the results of this study. A possible misclassification bias in the database must be considered. Additionally, the study is centered in patients requiring hospital care, and results are not generalizable to the entire COPD population.
Conclusions
Patients’ overall condition worsened significantly during the follow-up period, which correlated with an increased mortality rate and major direct medical costs. Further research will be required to evaluate the total burden of COPD in Spain, considering indirect and societal costs.
Transparency
Declaration of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of financial/ other relationships
The authors declare that they have no competing interests.
Author contributions
JD contributed to the investigation by analysing and interpreting the burden associated to COPD in Spain and was a major contribution in the intellectual content revision. MA analysed the current situation of COPD in Spain, interpreted the statistical data and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplemental Material
Download MS Word (13.6 KB)Acknowledgements
Not applicable.
Data availability statement
The data that support the findings of this study is available from the Spanish Ministry of Health via the Unit of Health Care Information and Statistics (Spanish Institute of Health Information) for researchers who meet the criteria for access to confidential data at https://www.mscbs.gob.es/estadEstudios/sanidadDatos/home.htm
References
- Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet. 2012; 379(9823):1341–1351.
- Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J. 2011;37(2):264–272.
- Christenson SA, Smith BM, Bafadhel M, et al. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227–2242.
- World Health Organization (WHO). Chronic obstructive pulmonary disease (COPD). WHO; 2022. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). Accessed 20 Jun 2022.
- Miravitlles M, Sobradillo V, Villasante C, et al. Estudio epidemiológico de la EPOC en España (IBERPOC): reclutamiento y trabajo de campo [epidemiological study of chronic obstructive pulmonary disease in Spain (IBERPOC): recruitment and field work]. Arch Bronconeumol. 1999;35(4):152–158.
- Sobradillo V, Miravitlles M, Jiménez CA, et al. Estudio IBERPOC en España: prevalencia de síntomas respiratorios habituales y de limitación crónica al flujo aéreo [epidemiological study of chronic obstructive pulmonary disease in Spain (IBERPOC): prevalence of chronic respiratory symptoms and airflow limitation]. Arch Bronconeumol. 1999;35(4):159–166.
- Soriano JB, Ancochea J, Miravitlles M, et al. Recent trends in COPD prevalence in Spain: a repeated cross-sectional survey 1997–2007. Eur Respir J. 2010;36(4):758–765.
- Soriano JB, Alfageme I, Miravitlles M, et al. Prevalence and determinants of COPD in Spain: EPISCAN II. Arch Bronconeumol (Engl Ed). 2021;57(1):61–69.
- Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773.
- Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164.
- Miravitlles M, Calle M, Molina J, et al. Spanish COPD guidelines (GesEPOC) 2021: updated pharmacological treatment of stable COPD. Arch Bronconeumol. 2022;58(1):69–81.
- Recio Iglesias J, López García F, Almagro P, et al. Spanish clinical practice consensus in internal medicine on chronic obstructive pulmonary disease patients with comorbidities (miEPOC). Curr Med Res Opin. 2020;36(6):1033–1042.
- Miravitlles M, Solé A, Aguilar H, et al. Economic impact of low adherence to COPD management guidelines in Spain. Int J Chron Obstruct Pulmon Dis. 2021;16:3131–3143.
- Gutiérrez Villegas C, Paz-Zulueta M, Herrero-Montes M, et al. Cost analysis of chronic obstructive pulmonary disease (COPD): a systematic review. Health Econ Rev. 2021;11(1):31.
- Centers for Disease Control and Prevention (CDC). International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). CDC; 2022. https://www.cdc.gov/nchs/icd/icd-10-cm.htm. Accessed 10 May 2022.
- World Health Organization (WHO). International classification of primary care., 2nd edition (ICPC-2). WHO; 2022. https://www.who.int/standards/classifications/other-classifications/international-classification-of-primary-care. Accessed 10 May 2022.
- Law 14/2007 3rd July, on biomedical research (Boe, 4 July 2007). Rev Derecho Genoma Hum. 2007; (26):283–325. PMID: 18201045
- Montserrat-Capdevila J, Marsal JR, Ortega M, et al. Clinico-epidemiological characteristics of men and women with a new diagnosis of chronic obstructive pulmonary disease: a database (SIDIAP) study. BMC Pulm Med. 2021;21(1):44.
- González J, Moncusí-Moix A, Benitez ID, et al. Clinical consequences of COVID-19 lockdown in patients with COPD: results of a pre-post study in Spain. Chest. 2021;160(1):135–138.
- Wedzicha JA, Calverley PMA, Albert RK, et al. Prevention of COPD exacerbations: a european respiratory society/American thoracic society guideline. Eur Respir J. 2017;50(3):1602265.
- Rehman AU, Ahmad Hassali MA, Muhammad SA, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in the USA, Europe, and Asia: results from a systematic review of the literature. Expert Rev Pharmacoecon Outcomes Res. 2020;20(6):661–672.
- Merino M, Villoro R, Hidalgo-Vega Á, et al. Social economic costs of COPD in extremadura (Spain): an observational study. Int J Chron Obstruct Pulmon Dis. 2018;13:2501–2514.
- Sánchez-Muñoz G, Lopez-de-Andrés A, Hernández-Barrera V, et al. Bronchiectasis in patients hospitalized with acute exacerbation of COPD in Spain: influence on mortality, hospital stay, and hospital costs (2006–2014) according to gender. PLOS One. 2019;14(1):e0211222.
- Landete P, Prieto Romo JI, Giacomini F. Experience on the management of patients with asthma or chronic obstructive pulmonary disease during the COVID-19 pandemic: the NEUMOBIAL study. Adv Ther. 2022;39(11):5216–5228.
- de Miguel-Diez J, Lopez-de-Andres A, Jimenez-Garcia R, et al. Sex differences in COVID-19 hospitalization and hospital mortality among patients with COPD in Spain: a retrospective cohort study. Viruses. 2022;14(6):1238. Published 2022 Jun 7.
- Dal Negro RW, Celli BR. Patient related outcomes-BODE (PRO-BODE): a composite index incorporating health utilization resources predicts mortality and economic cost of COPD in real life. Respir Med. 2017;131:175–178.
