Abstract
Introduction
Transfemoral access (TFA) is the primary access approach for neurointerventional procedures. Transradial access (TRA) is established in cardiology due to its lower complications, yet, it is at its early stages in neuroprocedures. This study performs an early exploration of the economic impact associated with the introduction of TRA in diagnostic and therapeutic neuroprocedures from the Spanish NHS perspective.
Methods
An economic model was developed to estimate the cost and clinical implications of using TRA compared to TFA. Costs considered access-related, complications and recovery time costs obtained from local databases and experts’ inputs. Clinical inputs were sourced from the literature. A panel of eight experts from different Spanish hospitals, validated or adjusted the values based on local experience. Hypothetical cohorts of 10,000 and 1000 patients were considered for diagnostic and therapeutic neuroprocedures respectively. Deterministic sensitivity analysis was performed.
Results
TRA in diagnostic procedures was associated with lower costs with savings ranging between €486 and €157 depending on the TFA recovery time considered. TRA is estimated to lead to 158 fewer access-site complications. In therapeutic procedures, TRA resulted in 76.4 fewer complications and was estimated to be cost-neutral with an incremental cost of €21.56 per patient despite recovery times were not included for this group. Variation of the parameters in the sensitivity analysis did not change the direction of the results.
Limitations
Clinical data was obtained from literature validated by experts therefore results generalizability is limited. In therapeutic neuroprocedures, there is an experience imbalance between approaches and recovery times were not included hence the total impact is not fully captured.
Conclusions
The early economic model suggests that implementing TRA is associated with reduced costs and complications in diagnostic procedures. In therapeutic procedures, TRA lead to fewer complications and it is estimated to be cost-neutral, however its full potential still needs to be quantified.
Introduction
In the field of neurointerventional procedures, transfemoral access (TFA) has been historically the primary approach, mainly due to its larger calibre and ease of accessCitation1,Citation2. However, TFA can present several access site-related complications including bleeding, retroperitoneal hematomas, pseudoaneurysms, and death among othersCitation3,Citation4.
Transradial access (TRA) is an alternative approach where the catheter is inserted via the radial artery rather than the femoral one. The TRA approach has been widely shown to be associated with fewer access site complications, shorter hospital stays, higher patient preference and reduced cost in interventional cardiology, as compared to TFACitation5–17. Currently, the American Heart Association (AHA) guidelines recommend TRA as the first strategy for patients with acute coronary syndromesCitation18.
Fewer studies have investigated the benefits and limits of TRA for neurovascular procedures such as cerebral angiographies and endovascular embolization of intracranial aneurysms with coils and/or flow diverters. A recent study described TRA as highly safe and efficient for performing diagnostic and interventional proceduresCitation19. Other studies have compared TRA to TFA and supported the evidence of radial access benefits over femoral access in terms of lower complication rate (both overall and access-site related) and higher patient preferenceCitation20–22. The radial puncture is associated with fewer complications due to its location, as it excludes the possibility of severe complications such as retroperitoneal bleeding. Moreover, possible hemorrhages or hematomas can be detected easily as it is a superficial artery, allowing to anticipate the treatment of complications as compared to TFA. In addition, as the hand circulation is double (radial and ulnar artery), possible occlusions of one of the arteries have little clinical impact, while occlusions of the femoral artery could have more serious consequencesCitation23.
Given the complications associated with TFA and the aforementioned promising benefits of TRA neurointerventionalists have increasingly begun to incorporate TRA in their practiceCitation3.
With the aim to better understand the economic impact of incorporating TRA into routine practice, an economic model was developed to explore the cost implications associated with the implementation of radial access compared with femoral access in diagnosis or therapeutic neuroprocedures, over a maximum one-year time horizon, from the perspective of the Spanish National Health System (NHS).
Methods
Model structure
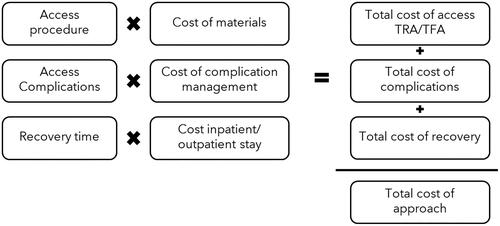
An early economic model was built to estimate the economic impact of using TRA compared to TFA in neuroprocedures. The model estimated the cost differential between the two approaches over a 1-year time horizon to capture all related access complications, as well as incremental clinical benefits (number of catheterizations without crossover, recovery time, and complications) (). Two hypothetical cohorts were entered into the model: 10,000 patients that undergo TRA or TFA for a diagnostic procedure and 1000 patients that undergo TRA or TFA in the context of a therapeutic endovascular procedure. The diagnostic hypothetical cohort considers a larger number of patients for three main reasons. Firstly, there is a higher overall procedure volume. Secondly, TRA is more frequently used due to the simpler nature of the diagnostic procedure. Thirdly, there is better device availability and compatibility compared to the therapeutic procedure group. The proposed modelling approach considered the costs of the procedure (access-related only), complications and recovery time to calculate the total cost of TRA or TFA. Other cost drivers were excluded from the analysis, as the focus was on aspects strictly associated with the access step of the main procedure (from a puncture to access to the target vessel) rather than the whole main technique performed. Indirect costs were also excluded from the analysis as the perspective of the Spanish NHS was considered.
Model parametrization
In order to populate the model, a literature review was performed. Considering the limited evidence on TRA in neuro-procedures, the inputs from the literature were presented to a panel of experts, which validated the model parameters using a virtual nominal group technique. The panel was composed of experts from 8 Spanish hospitals, which are early adopters of TRA, located in 5 out of 17 autonomous communities in the north, central, and south regions, including the islands. These hospitals are centers with a high and moderate volume of neuroprocedures which altogether perform a total of 1940 therapeutic procedures (1264 mechanical thrombectomies; 676 endovascular aneurysm treatment) and 1807 diagnostic procedures (such as cerebral angiograms) per year. The panel of experts could confirm the values obtained from the literature or substitute the values with a consensus on the rates observed in their practice. Regardless of whether the inputs were validated or overridden by the panel of experts, an average of the values provided by the 8 hospitals was used, while the minimum and maximum values were used as lower and upper values for the sensitivity analysis.
Diagnostic procedure model clinical inputs
Procedure success rate
The procedure was defined as successful when it does not require any crossover to reach the endpoint. A crossover was defined as the need to gain access to the neurovasculature by switching to a second access site due to any failure of the initial one (e.g. due to a failed puncture or catheterization of the target vessel). A prospective study on diagnostic cerebral angiography reported that the procedure success rate for radial and femoral access is 96.8% and 98.7%, respectivelyCitation22 (). Data used based on experts’ consensus are aligned with literature results and indicated an average value of 95.8% for TRA and 99.2% for TFA (). The maximum and minimum values reported by experts were used for the sensitivity analysis.
Table 1. Diagnostic procedure success rate, times and contrast volume, and complications.
Procedure time and contrast volume
The procedure time was defined as in-room time, including in-room time before the attempted access start and after the placement of the closure device. A recent paper investigated the differences in procedure time and contrast volume used in patients undergoing TRA or TFA and found no statistically significant difference between the two groups for both parametersCitation22 (). This finding was confirmed by clinical experts, especially after passing the learning curve of TRA. As the resulting cost difference would be minimal, procedure time and contrast volume were not considered in any of the models (diagnostic and therapeutic).
Complications
Literature data for the complication rates were sourced – when possible – from comparative papers, and successively validated by experts to define the data used in the model ().
Intracranial haemorrhage was not considered a potential complication in a diagnostic procedure as there is no catheterization of the intracranial vessels, therefore it was not included in the model.
Regarding occlusive arteries in TRA, experts agreed that generally, the incidence can vary between 5% and 10%, however, in most cases is asymptomatic and combined with the fact that often there is no control afterwards to verify the presence of the occlusion, generally it goes unnoticed. While an occlusive artery in TFA can shortly lead to an ischemic event. The value used for the TRA reflects mainly symptomatic occlusive arteries according to the local experience.
Recovery time
Recovery time was defined as the time elapsed between the end of the procedure and patient discharge. For both approaches, we found heterogeneity among the protocols reported from the centers, therefore multiple scenarios were simulated. For the base case, the most common protocol was considered. For radial access, the base case considers a recovery time equal to 120 min. For the alternative scenario analysis, the shortest recovery time was 60 min (15 min of compression followed by ultrasound before the discharge). For the femoral approach, the protocol differences were determined by the use of a closure device. Without a closure device, the patient was admitted to the hospital for at least 24 h. This time of recovery was used for the base case. However, if a closure device is used, then the patient would be discharged at 6 or 8 h, therefore those times were considered for the alternative scenarios.
Therapeutic procedure model clinical input
For the therapeutic procedure model, the main focus was on access via TRA or TFA for elective procedures (such as the treatment of unruptured aneurysms with flow diversion and coiling), therefore the costs of the devices for aneurysm treatment were not considered in the model.
Procedure success rate
Literature data showed that the procedure success rate for radial and femoral access is very similar with rates of 98.5% and 98.7%, respectivelyCitation20 (). Data used and validated by experts is in line with those from the literature, however, a slight difference was observed in the local experience with an average value of 97.6% for TRA and 98.6% for TFA ().
Table 2. Therapeutic procedure success rate, times and contrast volume, and complications.
Complications
Complication rates were obtained from comparative papers (). Likewise, for the diagnostic procedures, data was reviewed and validated by the experts considering the local experience. However, due to limited literature, in some cases, rates were based on the same sources used for the diagnostic procedure model (e.g. access site pain).
Recovery time
The recovery time parameter was not included in the base case of the therapeutic model, since the current protocols for patients treated with endovascular neuroprocedures consider that patients remain admitted at the hospital for at least 1–2 d after the procedure regardless of the access approach TRA or TFA. Nonetheless, early evidence suggests that TRA may lead to a reduction in the length of stay in neurointervention procedures, therefore an alternative scenario has been simulated. Alternative scenario 1 assumes two days of hospital stay with TFA versus one day with TRA.
Costs
The study considered the Spanish NHS perspective, therefore only direct medical costs were included in the analysis. The costs of access materials for the procedure, recovery, and complications management are summarized in . Costs of medications, procedures and access materials have been taken from Spanish cost databases and market prices which have been validated by a panel of experts.
Table 3. Costs.
According to the panel of experts, the management of vessel perforations in TRA is often conservative, which can be done manually by the operator, with a compression system or in some cases with a small suture and therefore it rarely requires a complex procedure or admission. As the cost of a vessel perforation in the Spanish cost database does not allow differentiation depending on the vessel location (upper or lower limb) or size, a weight has been applied to estimate the cost of a radial vessel perforation that reflects the local experience. Additionally, a €1 cost has been considered for the management of the occlusive artery in TRA, which in most cases is asymptomatic but when detected the management is mainly through medication (e.g. heparin) as indicated by the experts. All costs are presented in Euros and reflect price levels in the year 2022. Due to the time horizon used, no discount rate was considered for costs.
Model outcomes
The primary outcome of this study was to define the cost differences associated with the introduction of TRA when compared with TFA in patients undergoing diagnostic or therapeutic procedures, over a one-year time horizon.
The study also investigated the difference in clinical outcomes (as crossover need, complications and recovery time) in the two TRA and TFA populations, for both the diagnostic and therapeutic scenarios.
Sensitivity analysis
To account for uncertainty around the data used in the model, a univariate deterministic sensitivity analysis (DSA) was undertaken in the form of a tornado diagram for both TRA and TFA populations. The DSA involved altering the value used for individual parameters, within realistic ranges, to assess the impact on the model results. All parameters were variated ±15%, although in some cases one side of the variation was at a lower rate because the maximum possible value was reached.
To further test the model results, an additional DSA was performed using the minimum and maximum values observed in the local practice.
Results
Diagnostic procedure
In the base case scenario, the overall cost per patient having a diagnostic procedure through radial access is €429 less costly than via femoral access over a 1-year time horizon (). For a hypothetical cohort of 10,000 patients, the savings would be equal to €4.29 million. This cost difference is mainly associated with a shorter hospital stay, being the main driver of the cost savings (). Overall, it is estimated that performing diagnostics procedures through TRA could save 220,000 h (). Despite the small difference in costs for complications, TRA can avoid access 158 complications.
Table 4. Model results: Diagnostic procedures.
In all alternative scenarios, TRA appears to be less expensive than TFA (€486, €214 and €157 for alternative scenarios 1, 2 and 3 respectively).
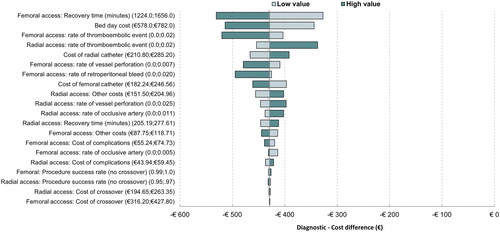
Based on the DSA results, the parameters that generate the most uncertainty are recovery time for femoral access and bed day cost (). In both cases, a variation of ±15% for these inputs generates changes in the cost difference by almost 20%. For lower estimates of recovery time for TFA or bed day costs in the alternative scenarios, the cost differential decreases, and other costs such as material costs become the parameters that would generate the most uncertainty, however, the overall benefits remain in favour of TRA.
Figure 2. Results diagnostic deterministic sensitivity analysis (Tornado diagram, base case, ±15% variation).
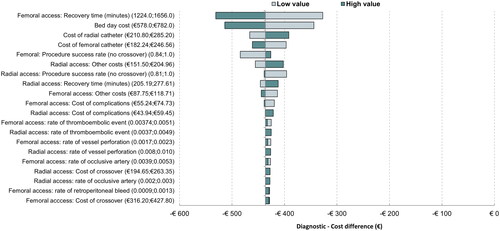
In the base case DSA, other parameters that have an impact on the incremental cost are the cost of radial and femoral catheters, the cost of complications for radial and femoral access, the rate of vessel perforation for radial access, and the radial and femoral access success rate. The remaining parameters do not generate an important variability of the results (<1%).
When using minimum and maximum values reported by the panel of experts, recovery time for femoral access and bed day cost remain the variables generating the most uncertainty and despite other variables related to rates of a complication becoming more predominant, none of them generate an impact that would change the direction of the results ().
Therapeutic procedure
In the base case, the model estimates that TRA is relatively cost neutral, with an incremental cost of €21.56 per patient (). Complication costs are lower in TRA than in TFA generating savings of €153.73, however, the costs of the access materials are projected to be higher with TRA (incremental of €175.3) mainly due to the higher cost of the catheter, the introducer kit and the use of ultrasound. Other potential savings like recovery time have not been considered and therefore this value does not consider all the potential cost implications. It is estimated that 76.4 complication events would be avoided in a cohort of 1,000 patients.
Table 5. Model results: Therapeutic procedures.
The alternative scenario estimates a cost-saving of €658 per patient, mainly due to the savings from shorter lengths of stay, suggesting that the potential benefits of TRA can outweigh the higher costs when all main cost categories are included in the analysis.
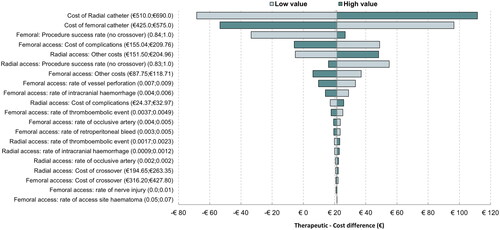
The sensitivity analysis suggests the parameters of the key drivers of uncertainty leading to a higher impact on the model results are the costs of the catheters (TRA and TFA), crossover rates (TRA and TFA) and the cost of complication in TFA ().
Discussion
Our economic model showed that the TRA approach, as compared to TFA, offers a clear advantage in terms of total costs and clinical benefits for patients undergoing diagnostic neuroprocedures. Considering a hypothetical cohort of 10,000 patients, the TRA approach lead to savings in all the scenarios modelled even when shorter hospital stays were considered for TFA (range €486–€157 per patient), representing a possible savings of up to €4.29 million in direct costs for this patient cohort. From the clinical perspective, patients undergoing TRA are projected to present fewer complications compared to TFA (687 vs 845). However, the model showed that patients undergoing radial access are more likely to switch to the femoral approach than vice versa; nonetheless, the additional costs of crossover from TRA to TFA did not change the direction of the results. The cost saving was driven mainly by the reduction in hospital stays as the use of TRA in diagnostic procedures allows patients to return to their homes in a period as short as one hour after the procedure. A recent study comparing supply and equipment costs between both approaches for diagnostic cerebral angiography in the United States, showed that TRA had significantly lower material costs compared to TRA, however is unclear if this study considered the same category of materials and any length of stayCitation24.
In the context of therapeutic neurointerventional procedures, TRA was found relatively cost neutral, leading to a slightly higher total overall cost compared to TFA, with an incremental difference of €21.6 (leading to a difference of €21,561 considering a hypothetical population of 1000 patients). The incremental cost is explained by the exclusion of the recovery cost variable from the therapeutic procedures model (base case), due to the lack of a sufficient amount of data to provide a reliable time estimate. In the alternative scenario, savings of €658 per patient are projected in the hypothetical case that a day of difference is observed between TRA and TFA. Hence, the observed cost difference in the base case largely depends on the higher access material costs of TRA compared to TFA (€783.7 vs €608.4). A study investigating the hospital cost of all elective neuroprocedures performed in a single center showed that TRA access is associated with lower overall costs compared to TFA, where the driver of the lower cost was the reduction of hospital stay for patients in the TRA groupCitation25. In addition, TRA showed lower complications cost than TFA, leading to an incremental cost of – €153.7, mainly driven by the fewer complications that patients treated with TRA could present compared to TFA (28.2 vs 104.5). Analogous results were found in therapeutic neuro-procedures with TRA leading to a lower number of catheterisations without crossover. However, the crossover rates were considered to be lower in this group than in the diagnostic one. Multiple factors could be contributing to this scenario, the most likely one being the selection bias. Patients undergoing therapeutic procedures are carefully selected to avoid complications, then most likely a radial diagnostic procedure has been already performed, and therefore it is known upfront if the patient’s anatomical features are appropriate to ensure the success of the arterial access. In a diagnostic procedure, the anatomy is unknown plus more vessels are being catheterized, which can also contribute to higher cross-over rates. Nonetheless, the values used in the model, are aligned with the literature. Two recent studies investigated the TRA success rate for diagnostic and interventional neuroprocedures and found that its value ranges from 88.8% to 98.9%, with the transition from radial to femoral route occurring in 2.2–6.5% of the casesCitation19,Citation26. The margin of the procedure failure – although low – might explain the need to occasionally crossover to an alternative catheterisation method.
These results have been tested in the DSA, where all variations of the parameters did not change the cost-saving profile of TRA, even using a wider range of minimum and maximum values.
Our economic model is the first performed in Spain providing an early estimate of the cost implications associated with the implementation of radial access in neuro-procedures compared with femoral access (diagnostic and therapeutic). This study supports results obtained by other investigators in the cardio-interventional and neurointerventional field, reinforcing the benefits of TRA for neuro-procedures, more predominantly in diagnostic proceduresCitation10,Citation12,Citation24,Citation25.
Several other TRA-associated advantages described in the literature further endorse the hypothesis that TRA is a valid alternative in neuro-procedures. TRA has been shown to be particularly beneficial in certain sub-populations of patients. Some studies demonstrated reduced cumulative rates of bleeding complications, access-site injury and non-access-site complications with TRA compared to TFA (2.0% vs 7.5%) in extremely obese patientsCitation27. Pregnant patients undergoing TRA can perform arterial access sites away from the uterus, decreasing the radiation exposure to the fetus. Subjects on anticoagulants may also benefit from TRA due to better bleeding control. Finally, elderly patients (>75 years) also have been found to have a lower rate of major complications following TRACitation28. Another important feature is the patient preference for TRA compared to TFA, especially considering that undergoing TFA causes pain and great discomfortCitation3,Citation29,Citation30. This higher preference for TRA has been expressed not only for diagnostic but also for therapeutic procedures that involve hospital overnight stays for observationCitation30.
The transradial access technique also presents some limitations, mostly related to its recent adoption in neurointerventional procedures, especially in therapeutic ones currently dominated by TFACitation3. Performing therapeutic neurointerventions via radial approach can be challenging having limited access catheters and sheaths designed and approved for this purpose, or using guide systems designed for TFA.
On the other hand, the lack of robust comparative data about TRA efficacy and complications compared to TFA, particularly in therapeutic neuroprocedures is another reason that might slow TRA’s adoption. Anatomical variations in the arm or subclavian tortuosity can also lead to a few challenges for physicians: the lusoria artery highly increases the technical difficulty of performing TRA, and could require crossover to complete the procedureCitation27. In addition, radial artery variants (e.g. radial loops) can make difficult catheter advancementCitation31. The small calibre of the radial artery could occasionally cause vasospasms in response to catheterization, difficulting the completion of the procedure and/or leading to a crossover. However, literature may be influenced by the selection of each cohort of TRA and whether a minimum radial diameter was a determining factor.
This study has limitations. First, there is an imbalance in the number of patients treated using TRA in therapeutic neuroprocedures, therefore, data and estimates around TFA are more robust due to the greater experience. Secondly, not all key variables have been included in the therapeutic model (e.g. recovery times,) and therefore the economic impact of using TRA is not fully captured. Third, using a panel of experts may be subject to the presence of bias. In addition, given the study’s scope and data limitations, a probabilistic sensitivity analysis was not conducted. Further procedure experience and research quantifying the total hospital costs are required to confirm the results of this early economic analysis. Analysis of high-risk patient groups is also suggested as the economic benefit from TRA could be greater. Moreover, this study does not consider indirect costs (informal care and productivity loss) associated with each approach, therefore it does not capture the potential economic burden for patients.
Our findings, together with literature data, suggest that TRA appears to have a reasonable safety profile - together with the aforementioned promising findings – could further encourage neurointerventionalists to consider TRA as a valid alternative to gain access to the neurovasculature, which involves a paradigm shift and finding the optimal balance between the available approaches. Dominating both TFA and TRA can only maximize their benefits, ultimately, the final objective is to treat every single patient with the best approach and help overcome any issue for which no other alternative exists.
Conclusion
This early economic model suggests that the total direct costs and the number of complications associated with the implementation of TRA in diagnostics neuroprocedures are lower than those associated with TFA. In therapeutic procedures, TRA is associated with fewer complications and is suggested to be cost-neutral, although key variables such as shorter recovery times and intensity of care have not been included in the base case scenario. Our results are in line with other published findings; however, further studies are needed to better characterize the full potential of TRA in the neurointerventional field.
Transparency
Declaration of funding
This study was sponsored by Medtronic Europe.
Declaration of financial/other relationships
Dr Carlos Rodríguez Paz is a proctor and consultant for Medtronic. The other authors report no conflict.
Valeska Seguel Ravest and Rosa Paolillo are Medtronic employees.
Author contributions
ALG, CRP, YAT, EF, MJG, ALFLJ, PTM, RBP: contributed to the design, data validation, review and revision of the manuscript. VSR: contributed to literature review analysis, interpretation, drafting, review, and revision of the manuscript. RP: drafting, and review of the manuscript.
Reviewer disclosures
Peer reviewers on this manuscript have received an honorarium from JME for their review work but have no other relevant financial relationships to disclose.
Acknowledgements
None stated.
Data availability statement
The manuscript and supplement included all relevant data.
References
- Kaki A, Blank N, Alraies MC, et al. Access and closure management of large bore femoral arterial access. J Interv Cardiol. 2018;31(6):969–977. doi: 10.1111/joic.12571.
- Patel P, Haussen DC, Nogueira RG, et al. The neuro radialist. Interv Cardiol Clin. 2020;9(1):75–86. doi: 10.1016/j.iccl.2019.08.008.
- Snelling BM, Sur S, Shah SS, et al. Transradial access: lessons learned from cardiology. J Neurointerv Surg. 2018;10(5):487–492. doi: 10.1136/neurintsurg-2017-013295.
- Pierot L, Moret J, Barreau X, et al. Aneurysm treatment with WEB in the cumulative population of two prospective, multicenter series: 3-year follow-up. J Neurointerv Surg. 2020;87(2):357–367.
- Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16(1):3–7. doi: 10.1002/ccd.1810160103.
- Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv. 2009;2(11):1047–1054. doi: 10.1016/j.jcin.2009.07.016.
- Brunet M-C, Chen SH, Peterson EC, et al. Transradial access for neurointerventions: management of access challenges and complications. J Neurointerv Surg. 2020;12(1):82–86. doi: 10.1136/neurintsurg-2019-015145.
- Caputo RP, Tremmel JA, Rao S, et al. Transradial arterial access for coronary and peripheral procedures: executive summary by the transradial committee of the SCAI. Catheter Cardiovasc Interv. 2011;78(6):823–839. doi: 10.1002/ccd.23052.
- Kolkailah AA, Alreshq RS, Muhammed AM, et al. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Cochrane Database Syst Rev. 2018;4(4):CD012318.
- Mamas MA, et al. Health economic analysis of access site practice in England during changes in practice: insights from the British cardiovascular interventional society. Circ Cardiovasc Qual Outcomes. 2018;11(5):e004482.
- Mann JT, et al. Right radial access for PTCA: a prospective study demonstrates reduced complications and hospital charges. J Invasive Cardiol. 1996;8(Suppl D):40D–44D.
- Mitchell MD, Hong JA, Lee BY, et al. Systematic review and cost-benefit analysis of radial artery access for coronary angiography and intervention. Circ Cardiovasc Qual Outcomes. 2012;5(4):454–462. doi: 10.1161/CIRCOUTCOMES.112.965269.
- Valgimigli M, Gagnor A, Calabró P, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. 2015;385(9986):2465–2476. doi: 10.1016/S0140-6736(15)60292-6.
- Wang YB, et al. Randomized comparison of radial versus femoral approach for patients with STEMI undergoing early PCI following intravenous thrombolysis. J Invasive Cardiol. 2012;24(8):412–416.
- Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377(9775):1409–1420. doi: 10.1016/S0140-6736(11)60404-2.
- Roule V, Lemaitre A, Sabatier R, et al. Transradial versus transfemoral approach for percutaneous coronary intervention in cardiogenic shock: a radial-first centre experience and meta-analysis of published studies. Arch Cardiovasc Dis. 2015;108(11):563–575. doi: 10.1016/j.acvd.2015.06.005.
- Bhat FA, Changal KH, Raina H, et al. Transradial versus transfemoral approach for coronary angiography and angioplasty – A prospective, randomized comparison. BMC Cardiovasc Disord. 2017;17(1):23. doi: 10.1186/s12872-016-0457-2.
- Mason PJ, Shah B, Tamis-Holland JE, et al. An update on radial artery access and best practices for transradial coronary angiography and intervention in acute coronary syndrome: a scientific statement from the American Heart Association. Circ Cardiovasc Interv. 2018;11(9):e000035.
- Sattur GM, Almallouhi E, Lena JR, Spiotta AM. Illustrated guide to the transradial approach for neuroendovascular surgery: a step-by-Step description gleaned from over 500 cases at an early adopter single center. Op Neuros. 2020;19(2):181–189.
- Catapano JS, Fredrickson VL, Fujii T, et al. Complications of femoral versus radial access in neuroendovascular procedures with propensity adjustment. J Neurointerv Surg. 2020;12(6):611–615. doi: 10.1136/neurintsurg-2019-015569.
- Weinberg JH, Sweid A, Hammoud B, et al. A comparative study of transradial versus transfemoral approach for flow diversion. Neuroradiology. 2021;63(8):1335–1343. doi: 10.1007/s00234-021-02672-4.
- Stone JG, Zussman BM, Tonetti DA, et al. Transradial versus transfemoral approaches for diagnostic cerebral angiography: a prospective, single-center, non-inferiority comparative effectiveness study. J Neurointerv Surg. 2020;12(10):993–998. doi: 10.1136/neurintsurg-2019-015642.
- Ruzsa Z, Csavajda Á, Nemes B, et al. Distal radial artery access for superficial femoral artery interventions. J Endovasc Ther. 2021;28(2):255–261. doi: 10.1177/1526602820963022.
- Dodd W, Small CN, Goutnik M, et al. Cost comparison: evaluating transfemoral and transradial access for diagnostic cerebral angiography. Stroke. 2023;3(1):e000428.
- Catapano JS, Ducruet AF, Koester SW, et al. Propensity-adjusted cost analysis of radial versus femoral access for neuroendovascular procedures. J Neurointerv Surg. 2021;13(8):752–754. doi: 10.1136/neurintsurg-2020-016728.
- Pons RB, Caamaño IR, Chirife OS, et al. Transradial access for diagnostic angiography and interventional neuroradiology procedures: a four-year single-center experience. Interv Neuroradiol. 2020;26(4):506–513. doi: 10.1177/1591019920925711.
- Zalocar LAD, Doroszuk G, Goland J, et al. Transradial approach and its variations for neurointerventional procedures: literature review. Surg Neurol Int. 2020;11(248):248. doi: 10.25259/SNI_366_2020.
- Achenbach S, Ropers D, Kallert L, et al. Achenbach S, ropers D, transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008;72(5):629–635. doi: 10.1002/ccd.21696.
- Khanna O, Sweid A, Mouchtouris N, et al. Radial artery catheterization for neuroendovascular procedures. Stroke. 2019;50(9):2587–2590. doi: 10.1161/STROKEAHA.119.025811.
- Satti SR, Vance AZ, Golwala SN, et al. Patient preference for transradial access over transfemoral access for cerebrovascular procedures. Journal of Vascular and Interventional Neurology. 2017;9(4):1–5.
- Gao B-L, Xu G-Q, Wang Z-L, et al. Transradial stenting for carotid stenosis in patients with bovine type and type III aortic arch: experience in 28 patients. World Neurosurg. 2018;111:e661–e667. doi: 10.1016/j.wneu.2017.12.138.
- Oneissi M, Sweid A, Tjoumakaris S, et al. Access-site complications in transfemoral neuroendovascular procedures: a systematic review of incidence rates and management strategies. Oper Neurosurg. 2020;19(4):353–363. doi: 10.1093/ons/opaa096.