Abstract
Background
Minimally invasive surgical therapies, such as water vapor thermal therapy (WVTT) and prostatic urethral lift (PUL), are typically second-line options for patients in whom medical management (MM) failed but who are unwilling or unsuitable to undergo invasive transurethral resection of the prostate (TURP). However, the incremental cost-effectiveness of WVTT or PUL as first- or second-line therapy is unknown. We evaluated the incremental cost-effectiveness of alternative first- and second-line treatments for patients with moderate-to-severe benign prostatic hyperplasia (BPH) in Singapore to help policymakers make subsidy decisions based on value for money.
Methods
We considered six stepped-up treatment strategies, beginning with MM, WVTT, PUL or TURP. In each strategy, patients requiring retreatment advance to a more invasive treatment until TURP, which may be undergone twice. A Markov cohort model was used to simulate transitions between BPH severity states and retreatment, accruing costs and quality-adjusted life-years (QALYs) over a lifetime horizon.
Results
In moderate patients, strategies beginning with MM had similar cost and effectiveness, and first-line WVTT was incrementally cost-effective to first-line MM (33,307 SGD/QALY). First-line TURP was not incrementally cost-effective to first-line WVTT (159,361 SGD/QALY). For severe patients, WVTT was incrementally cost-effective to MM as a first-line treatment (30,133 SGD/QALY) and to TURP as a second-line treatment following MM (6877 SGD/QALY). TURP was incrementally cost-effective to WVTT as a first-line treatment (48,209 SGD/QALY) in severe patients only. All pathways involving PUL were dominated (higher costs and lower QALYs).
Conclusion
Based on the common willingness-to-pay threshold of SGD 50,000/QALY, this study demonstrates the cost-effectiveness of WVTT over MM as first-line treatment for patients with moderate or severe BPH, suggesting it represents good value for money and should be considered for subsidy. PUL is not cost-effective as a first- nor second-line treatment. For patients with severe BPH, TURP as first-line is also cost-effective.
PLAIN LANGUAGE SUMMARY
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate, common among older men. Its symptoms include difficulties with starting and completing urination, incontinence, frequent and urgent need to urinate. Minimally invasive procedures, such as water vapor thermal therapy (WVTT) and prostatic urethral lift (PUL), are typically offered as second-line options to patients for whom medication has failed but who are unwilling or unsuitable to undergo invasive surgery (transurethral resection of the prostate, TURP). However, whether offering these procedures as first-line options represents good value for money (i.e. cost-effectiveness) is an open question. To address this question and inform subsidy decisions in Singapore, we investigated six stepped-up treatment strategies which differ in first- and second-line treatments. For each strategy, we simulated healthcare costs and quality of life for a cohort of moderate and severe BPH patients over their lifetime, considering the possibility of treatment-related adverse effects and multiple rounds of retreatment. The incremental cost of a unit improvement in quality of life for a strategy relative to the next most expensive one was compared against a willingness-to-pay threshold to determine cost-effectiveness. We found that WVTT was cost-effective relative to medication as a first-line treatment for patients with moderate or severe BPH, suggesting it represents good value for money and should be considered for subsidy. PUL was not cost-effective as first- nor second-line treatment. TURP is cost-effective as first-line for severe BPH patients only.
Introduction
Benign prostatic hyperplasia (BPH), the non-cancerous enlargement of the prostate gland, is a common ageing-related progressive condition. It affects up to 50% of men aged 50 and olderCitation1 and nearly 80% of men by age 90Citation2. Several BPH treatment options are available, varying in terms of efficacy, invasiveness, and cost. Transurethral resection of the prostate (TURP) is considered the gold standard but, despite its high efficacy, it is the most costly and invasive option, with a higher risk of peri-operative and long-term adverse eventsCitation3,Citation4. For this reason, patients often start treatment with medical management (MM)Citation4. While generally considered safer than surgical options, MM can cause bothersome side effects, such as dizziness, postural hypotension, ejaculatory dysfunction, decreased libido, erectile dysfunctionCitation5 and may not provide sufficient reliefCitation4. Long-term MM is also subject to cumulative costs, and outcomes are affected by patient adherence to therapy, which can be poorCitation6.
In the past decade, minimally invasive surgical therapies (MISTs) have been developed for patients who failed medication therapy but are unwilling or unable to undergo TURP. Among the newest are Prostatic Urethral Lift (PUL) and Water Vapor Thermal Therapy (WVTT)Citation7–9. PUL involves the delivery of permanent implants to retract prostatic tissue, while WVTT uses radiofrequency to create water vapor in the form of steam to achieve targeted necrosis of prostate tissue. These procedures are effective, associated with a low risk of Lower Urinary Tract Symptoms (LUTS)-related adverse events, and may be less expensive than MM in the long runCitation10,Citation11.
As MM is often recommended as first-line in clinical practiceCitation4, the incremental cost-effectiveness of providing MISTs as first-line is an open question. This study aims to evaluate the incremental cost-effectiveness of alternative first- and second-line treatments for patients with moderate or severe BPH over their remaining lifetime. The six strategies considered are: (1) MM-WVTT-TURP-TURP, (2) MM-PUL-TURP-TURP, (3) MM-TURP-TURP, (4) WVTT-TURP-TURP, (5) PUL-TURP-TURP, (6) TURP-TURP. Each strategy represents a plausible treatment pathway that differs primarily by the first- and second-line treatment. Patients who require retreatment receive the next treatment as specified in each strategy. MM represents a generic combination of a-blocker and 5a-reductase inhibitor, as recommended by the American Urological Association for moderate-to-severe LUTS. TURP is the final treatment for all strategies and may be repeated once if required. Taking the Singapore healthcare system perspective, we separately estimated the cost, effectiveness, and incremental cost-effectiveness of these six treatment strategies for patients with moderate and severe BPH at baseline. These results could inform clinical guidelines and subsidy decisions in Singapore and other countries that apply cost-effectiveness analysis in treatment pathways and resource allocation decisionsCitation12.
Methods
A Markov model was developed in TreeAge Pro 2022Citation13 to evaluate the cost and effectiveness of BPH treatment strategies for a cohort of treatment-naïve males with moderate or severe BPH at baseline. Patients were assumed to be 66 years of age, which is the mean age of BPH patients in SingaporeCitation14. The model ran for 20 years using quarterly cycles to match the period over which short-term adverse events typically resolveCitation15. Benefits were measured in terms of quality-adjusted life-years (QALYs). Following guidelines by Singapore’s Agency for Care Effectiveness (ACE)Citation16, costs and benefits were discounted at 3% annually beyond the first year. To determine cost-effectiveness, a willingness-to-pay (WTP) threshold of SGD 50,000/QALY was used, in line with the GBP 30,000/QALY threshold adopted by the National Institute for Health and Clinical Excellence (NICE), as ACE does not publish a specific thresholdCitation17. This manuscript was written in accordance with the Consolidated Health Economic Evaluation Reporting Standards statementCitation18.
Model structure
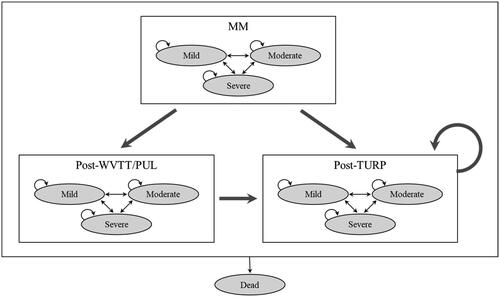
The model consists of 10 health states (). Alive health states are the three treatment states (rectangles): (i) MM, (ii) post-WVTT/PUL, (iii) post-TURP, crossed with the three BPH severity states (ovals): (i) Mild, (ii) Moderate, (iii) Severe, as defined by International Prostate Symptom Score (IPSS). IPSS is a validated eight-question screening tool created by the American Urological Association to diagnose, track and inform the management of BPH. The questionnaire assesses patients based on urinary storage and voiding symptoms such as frequency, urgency and weak urinary stream, and one overall Quality-of-Life item. It is scored from 0 to 35 and stratifies patients into three groups based on symptoms: mild (0–7), moderate (8–19), and severe (20–35) BPH. Mild BPH is typically asymptomatic as there is no significant blockage of the bladder; moderate BPH consists of bladder blockage which may impede the flow of urine; severe BPH consists of a severe blockage in which the patient is unable to empty the bladder completely, resulting in frequent urination in small amountsCitation19. Patients with more severe symptoms are less likely to benefit from conservative medical treatmentsCitation20.
Figure 1. Markov state transition diagram. BPH severity states and the dead state are represented by ovals, while treatment states are represented by rectangles. Small arrows indicate possible transitions between BPH severity states within a certain treatment arm. Large arrows indicate possible retreatment pathways. Abbreviations. MM, medical management; WVTT, water vapor thermal therapy; PUL, prostatic urethral lift; TURP, transurethral resection of the prostate; QALY, quality-adjusted life-years.
The model begins with moderate or severe patients receiving their first-line treatment and transitioning between mild, moderate, or severe health states according to the respective treatment effectiveness derived from Chughtai et al. They conducted a network meta-analysis of multiple trials for MM, PUL, WVTT and TURP treatments to obtain changes in participants’ IPSS following initial treatment for a period of five yearsCitation21. Health state utility values corresponding to a patient’s BPH severity are assigned each quarter. WVTT, PUL and TURP are one-time procedures. Patients who undergo WVTT, PUL or TURP incur a one-time treatment cost associated with the procedure, while patients on MM incur recurring cost of drugs regardless of BPH severity. In the event of retreatment to the next treatment line, patients on MM discontinue their medication and receive the relevant one-off procedures. Patients who undergo TURP receive a one-time decrement in utility due to the invasiveness of the procedure. Patients also incur follow-up costs after treatment: once in the first 3 months and every 9 months thereafter for MM, twice in the first 3 months and every 9 months thereafter for WVTT, PUL and TURP.
In each quarter, patients are subject to the risk of short- and long-term treatment-related adverse events, and the risk of death from all-cause mortality. Short-term adverse events are assumed to resolve within the first three months after treatment and are associated with a utility decrement and additional costs during the treatment quarter. Long-term adverse events are associated with a utility decrement and additional costs that last for as long as the patient remains in the same treatment state or dies. Age-specific death rates were obtained from Singapore Life Tables. Those who die are assigned zero costs and utilities.
Each quarter, a proportion of patients in the severe state progress to the next treatment. Upon retreatment, patients can improve or remain in the severe state according to the effectiveness of the last received treatment and are subject to associated short-term and long-term adverse events. The most invasive and last line of treatment in each arm is TURP.
Costs and utilities
reports the unit costs in 2022 and utility weights used in the model. Unsubsidized treatment and adverse event costs were based on typical bill sizes estimated by clinicians working at the Department of Urology at Singapore General Hospital (SGH), the largest public hospital in Singapore. Costs included are for treatment procedures, medications, follow-up visits, and the probability-weighted costs of common short- and long-term adverse events. The number of follow-up visits associated with each event was obtained from clinicians. These expected costs were calculated as the probability of having an adverse event multiplied by the cost of that adverse event and summing over each adverse event (Supplementary Appendix S1). Expected disutility for short- and long-term adverse events were calculated using a similar approach (Supplementary Appendix S2). Disutility weights were obtained from the literature.
Table 1. Model parameters.
Transition probabilities
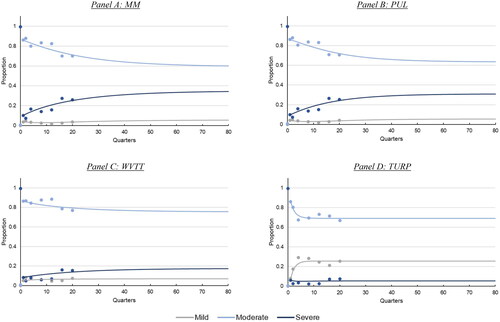
The transition probabilities which describe the short-term and long-term effectiveness of the four BPH treatments under consideration were derived from a network meta-analysis of the IPSS trajectories over 5 yearsCitation21. Assuming that IPSS follows a beta distribution bounded at 0 and 35, we calculated the implied distribution of BPH severity over 5 years. Further assuming a first-order Markov process, we fit a multinomial logistic regression model to changes in the distribution over time to estimate the transition probabilities between BPH severity states. These transition probabilities were then used to simulate BPH severity outcomes over 20 years in the absence of retreatment. Further details of the procedure are described in Supplementary Appendix S6. and show the resulting distribution of BPH severity in the absence of retreatment.
Figure 2. Trajectory of BPH severity over 20 years for patients with moderate BPH at baseline. Points indicate the implied distribution of BPH severity from the network meta-analysis in Chughtai et al.Citation21 Lines indicate the distribution generated from the fitted first-order Markov process. Abbreviations. MM, medical management; WVTT, water vapor thermal therapy; PUL, prostatic urethral lift; TURP, transurethral resection of the prostate.
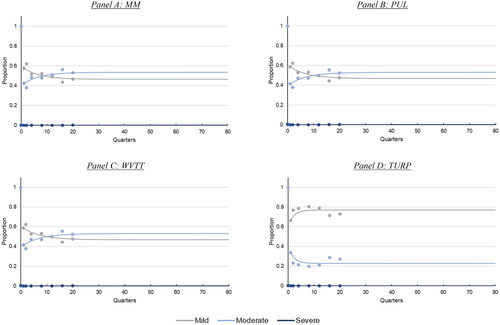
Figure 3. Trajectory of BPH severity over 20 years for patients with severe BPH at baseline. Points indicate the implied distribution of BPH severity from the network meta-analysis in Chughtai et al.Citation21 Lines indicate the distribution generated from the fitted first-order Markov process. Abbreviations. MM, medical management; WVTT, water vapor thermal therapy; PUL, prostatic urethral lift; TURP, transurethral resection of the prostate.
Probabilities of undergoing retreatment are based on published trialsCitation8,Citation9,Citation24,Citation25. Assuming only patients with severe BPH may undergo retreatment, we divided the unconditional retreatment rate reported in trials by the predicted proportion with severe BPH over the same period (details in Supplementary Appendix S4).
Scenario and sensitivity analysis
We conducted one-way deterministic analysis over the range of parameter values specified in to identify the most influential parameters. We also conducted probabilistic sensitivity analysis with 10,000 iterations to evaluate the impact of statistical uncertainty on ICERs. Transition probabilities between health states were drawn from Dirichlet distributions and cost parameters were drawn from gamma distributions. Retreatment probabilities and utility weights were drawn from beta distributions. Results of the probabilistic sensitivity analysis were presented as cost-effectiveness acceptability curves (CEAC) that show each strategy’s probability of being the optimal strategy (i.e. highest net monetary benefit) at different WTP thresholds.
We also investigated the sensitivity of the base case results to different assumptions on retreatment probabilities. To address the potential influence of patient (and physician) preferences on reported retreatment rates, which vary by factors other than BPH severity, we re-estimated ICERs assuming a uniform retreatment probability of 2% per quarter such that patients in the severe state are equally likely to retreat regardless of the previous treatment received. In another scenario, we relaxed the assumption that only patients with severe BPH may undergo retreatment and assumed those in the moderate state could also retreat but at one-third the rate of those in the severe state. Retreatment probabilities for both moderate and severe states were recalculated to ensure overall retreatment rates matched those reported in the trials (details in Supplementary Appendix S5).
Results
reports the incremental cost-effectiveness ratios (ICERs) of six treatment strategies for moderate and severe BPH patients at baseline. For both groups, MM-TURP-TURP was the least costly, followed by MM-WVTT-TURP-TURP, MM-PUL-TURP-TURP, WVTT-TURP-TURP, PUL-TURP-TURP, and TURP-TURP. All strategies involving PUL were dominated, as they incurred higher costs for a lower effectiveness than other strategies. Among moderate BPH patients, MM-WVTT-TURP-TURP and MM-PUL-TURP-TURP were dominated by MM-TURP-TURP however there were negligible differences in cost and QALYs between these three strategies because few moderate BPH patients progressed to the severe state and required retreatment. Compared to MM-TURP-TURP, WVTT-TURP-TURP cost SGD 4071 more and resulted in 0.12 higher QALYs (ICER: SGD 33,307/QALY). On the other hand, the incremental cost of TURP as first-line relative to WVTT as first-line was SGD 8231, but the incremental effectiveness was only 0.05 QALYs (ICER: SGD 159,361/QALY). Based on the WTP threshold of SGD 50,000/QALY, only WVTT-TURP-TURP was incrementally cost-effective to MM-TURP-TURP for moderate BPH patients.
Table 2. Costs, effectiveness, and incremental cost-effectiveness of treatment strategies by baseline BPH severity.
Among severe BPH patients, MM-WVTT-TURP-TURP cost SGD 264 more and had 0.04 more QALYs than MM-TURP-TURP (ICER: SGD 6877/QALY). Furthermore, the incremental cost of performing WVTT as first-line versus second-line was SGD 4172, while the incremental effectiveness was 0.14 QALYs (ICER: 30,113/QALY). Relative to WVVT-TURP-TURP, TURP-TURP was SGD 7958 more costly and resulted in 0.17 higher QALYs (ICER: SGD 48,209/QALY). Based on the WTP threshold, MM-WVTT-TURP-TURP, WVTT-TURP-TURP and TURP-TURP are incrementally cost-effective, with TURP-TURP being the optimal strategy.
Scenario and sensitivity analysis
One-way deterministic sensitivity analysis (see Supplementary Appendix S7 for tornado diagram) showed that baseline ICERs were most influenced by baseline age, utility weights associated with BPH severity, discount rate and treatment costs. Overall, a higher baseline age increased ICERs as older patients had a shorter period to accumulate improved QALYs following treatment. ICERs also increased when there were smaller differences between the utility weights of mild, moderate, and severe BPH, reducing QALYs gained. A higher discount rate also increased ICERs because treatment costs were incurred earlier and subjected to less discounting than QALY improvements.
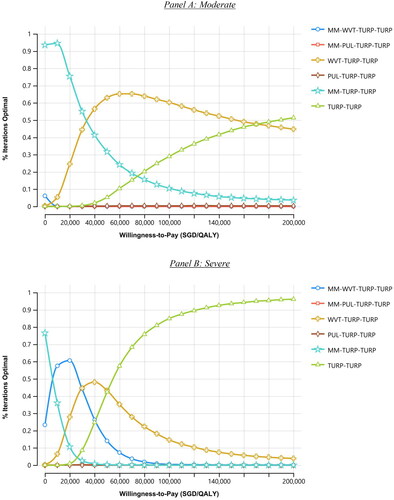
shows the cost-effectiveness acceptability curves from probabilistic sensitivity analysis, which mirrored the main findings from the mean value. At the SGD 50,000/QALY WTP threshold, WVTT-TURP-TURP was optimal (i.e. highest net monetary benefit) 63% of the time, followed by MM-TURP-TURP at 32%, and TURP-TURP at 5% among moderate BPH. For severe BPH, results are split between WVTT-TURP-TURP and TURP-TURP (43% vs 42% optimal).
Figure 4. Cost-effectiveness acceptability curve for moderate and severe BPH at baseline. Abbreviations. MM, medical management; WVTT, water vapor thermal therapy; PUL, prostatic urethral lift; TURP, transurethral resection of the prostate; SGD, Singapore Dollars; QALY, quality-adjusted life-years.
We examined the robustness of estimated ICERs under two different retreatment scenarios (see Supplementary Appendix S8). Assuming a uniform retreatment probability of 2% per quarter across all treatments changed the cost ordering of treatment strategies, but all strategies including PUL remain dominated and the ICERs of WVTT-TURP-TURP and TURP-TURP are similar to baseline results. Assuming patients in the moderate state retreat at one-third the rate of those in the severe state also did not lead to different conclusions.
Discussion
This study assessed the incremental cost-effectiveness of six alternative first- and second-line treatment strategies for patients with moderate or severe BPH over a lifetime horizon. Of the two MISTs being considered, PUL was not cost-effective as either first- or second-line treatment because it was more costly and less effective than pathways utilizing WVTT. In contrast, we found that WVTT as first-line was cost-effective compared to treatment pathways with MM as first-line, although ICERs were highly dependent on the patient’s baseline age. Relative to MM-TURP-TURP, WVTT as second-line had a negligible impact on cost and effectiveness for patients with moderate BPH at baseline. However, for patients who were severe at baseline, WVTT as second-line was highly cost-effective relative to MM-TURP-TURP. At the SGD 50,000/QALY WTP threshold, WVTT-TURP-TURP or TURP-TURP were more likely to be optimal treatment strategies.
Our findings are largely consistent with previous evaluations of MISTs for moderate-to-severe BPH patients from the United States (US) Medicare perspective. Over a two- to five-year horizon, PUL was either dominated by WVTT, or had similar effectiveness but cost substantially more than WVTTCitation21,Citation26. Furthermore, Chughtai et al. found that MM was also dominated by WVTT, and that TURP, despite being more effective than WVTT, was not incrementally cost-effective over a five-year time periodCitation21. However, since BPH is a chronic condition and patients may undergo multiple rounds of retreatment as the disease progresses, the five-year time horizon applied in the study may not capture the full incremental cost and benefits that accrue over the patient’s lifetime. To our knowledge, only one study has investigated the cost-effectiveness of MISTs as initial treatment and accounted for subsequent therapies over the patient’s lifetimeCitation27. Using a microsimulation approach, Sahakyan et al. found that WVTT as first-line dominated treatment pathways starting with either MM or PUL. Our results differ for MM mainly because the cost difference between MM and WVTT is much larger in Singapore than in the US (MM is 1% of WVTT procedure cost in Singapore vs 14% in the U.S.).
Our study has several strengths. First, we performed a comprehensive evaluation of first- and second-line treatment options available to local BPH patients, which included pathways that exclude MISTs or that start with invasive TURP. Second, we utilized a data-driven approach to extrapolate the long-term effectiveness of individual therapies over a lifetime horizon, which is also consistent with the Markov model employed. Third, we stratified our analyses for patients with moderate and severe BPH, showing that TURP as first-line may be cost-effective only for patients with severe symptoms at baseline. Lastly, we showed that age is a key factor for whether WVTT as first-line is cost-effective because treatment costs are upfront while QALY gains are accrued gradually over time.
Our study also has several limitations. First, we assumed a simplified stepped-up care pathway in consultation with local urologists, where patients receive the next most invasive therapy option in the event of treatment failure. Although it is possible for patients who had received MIST to receive a repeat MIST procedure, a different MIST procedure, or even non-invasive MM, such cases are not standard practice in Singapore’s public healthcare setting. Second, our model did not consider potential poor adherence to MM which may lower the effectiveness and cost of pathways involving MMCitation6. Third, our model made simplifying assumptions regarding retreatment due to insufficient information on local practices. Lastly, our analysis assumed that treatment effectiveness does not depend on whether therapies were received as first- or subsequent lines. If treatment is less effective when used as a second- or third-line, this will improve the cost-effectiveness of strategies which prioritize more invasive therapies.
Conclusions
Based on the common willingness-to-pay threshold of SGD 50,000/QALY, this study demonstrates the cost-effectiveness of WVTT over MM as first-line treatment for patients with moderate or severe BPH, suggesting it represents good value for money and should be considered for subsidy. PUL is not cost-effective as first- nor second-line treatment. For patients with severe BPH, TURP as first-line is also cost-effective.
Transparency
Declaration of funding
This study was funded by Boston Scientific.
Declaration of financial/other relationships
CW and GS are full-time employees of Boston Scientific.
Author contributions
CJ contributed to conception and design, data analysis and interpretation, manuscript writing, and statistical analysis. RJS contributed to data analysis and interpretation, manuscript writing and statistical analysis. JYMT, EJA, CWJ, HSSH, CW and GS contributed to data acquisition, critical revision of the manuscript and supervision of the research and writing of this article. EF supervised the research and writing of this article.
Ethics statement
This study was granted exemption from NUS Institutional Review Board (NUS-IRB-2022-264).
Supplemental Material
Download MS Word (136.2 KB)Acknowledgements
No assistance in the preparation of this article is to be declared. Findings of this paper have been presented at the 38th Annual European Association of Urology Congress.
Data availability statement
Data supporting the findings of this study are available within the article and its supplementary materials.
References
- Kapoor A. Benign prostatic hyperplasia (BPH) management in the primary care setting. Can J Urol. 2012;19(Suppl 1):10–17.
- Berry SJ, Coffey DS, Walsh PC, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474–479. doi: 10.1016/s0022-5347(17)49698-4.
- Bortnick E, Brown C, Simma-Chiang V, et al. Modern best practice in the management of benign prostatic hyperplasia in the elderly. Ther Adv Urol. 2020;12:1756287220929486. doi: 10.1177/1756287220929486.
- Lerner LB, McVary KT, Barry MJ, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART I-Initial work-up and medical management. J Urol. 2021;206(4):806–817. doi: 10.1097/JU.0000000000002183.
- Yu ZJ, Yan HL, Xu FH, et al. Efficacy and side effects of drugs commonly used for the treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia. Front Pharmacol. 2020;11:658. doi: 10.3389/fphar.2020.00658.
- Cindolo L, Pirozzi L, Sountoulides P, et al. Patient’s adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy? BMC Urol. 2015;15(1):96. doi: 10.1186/s12894-015-0090-x.
- Leong JY, Patel AS, Ramasamy R. Minimizing sexual dysfunction in BPH surgery. Curr Sex Health Rep. 2019;11(3):190–200. doi: 10.1007/s11930-019-00210-1.
- Roehrborn CG, Barkin J, Gange SN, et al. Five year results of the prospective randomized controlled prostatic urethral L.I.F.T. study. Can J Urol. 2017;24(3):8802–8813.
- McVary KT, Gittelman MC, Goldberg KA, et al. Final 5-year outcomes of the multicenter randomized sham-controlled trial of a water vapor thermal therapy for treatment of moderate to severe lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2021;206(3):715–724. doi: 10.1097/JU.0000000000001778.
- Roehrborn CG, Gange SN, Shore ND, et al. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L.I.F.T. study. J Urol. 2013;190(6):2161–2167. doi: 10.1016/j.juro.2013.05.116.
- McVary KT, Gange SN, Gittelman MC, et al. Minimally invasive prostate convective water vapor energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2016;195(5):1529–1538. doi: 10.1016/j.juro.2015.10.181.
- Agency for Care Effectiveness. Medical technologies evaluation methods and process guide. Singapore: Ministry of Health Singapore; 2022.
- TreeAge Software. TreeAge pro 2021. Williamstown, MA: TreeAge Software; 2021. http://www.treeage.com.
- Loh AH, Ng KK, Ng FC. Presentation and progression of benign prostatic hyperplasia: a Singapore experience profiling ethnic differences in a multiracial study cohort. Ann Acad Med Singap. 2009;38(5):451–456. doi: 10.47102/annals-acadmedsg.V38N5p451.
- Erman A, Masucci L, Krahn MD, et al. Pharmacotherapy vs surgery as initial therapy for patients with moderate-to-severe benign prostate hyperplasia: a cost-effectiveness analysis. BJU Int. 2018;122(5):879–888. doi: 10.1111/bju.14520.
- Agency for Care Effectiveness. Drug evaluation methods and process guide. Singapore: ACE; 2019.
- Pearce F, Lin L, Teo E, et al. Health technology assessment and its use in drug policies: Singapore. Value Health Reg Issues. 2019;18:176–183. doi: 10.1016/j.vhri.2018.03.007.
- Don H, Michael D, Federico A, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25(1):10–31.
- Health Promotion Board. Lower urinary tract symptoms suggestive of enlarged prostate gland. Singapore: Ministry of Health Singapore; 2006.
- Ng M, Baradhi KM. Benign prostatic hyperplasia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Chughtai B, Rojanasarot S, Neeser K, et al. A comprehensive analysis of clinical, quality of life, and cost-effectiveness outcomes of key treatment options for benign prostatic hyperplasia. PLOS One. 2022;17(4):e0266824. doi: 10.1371/journal.pone.0266824.
- Ackerman SJ, Rein AL, Blute M, et al. Cost effectiveness of microwave thermotherapy in patients with benign prostatic hyperplasia: part I-methods. Urology. 2000;56(6):972–980. doi: 10.1016/s0090-4295(00)00828-1.
- Rognoni C, Tarricone R. Healthcare resource consumption for intermittent urinary catheterisation: cost-effectiveness of hydrophilic catheters and budget impact analyses. BMJ Open. 2017;7(1):e012360. doi: 10.1136/bmjopen-2016-012360.
- Teo JS, Lee YM, Ho HSS. An update on transurethral surgery for benign prostatic obstruction. Asian J Urol. 2017;4(3):195–198. doi: 10.1016/j.ajur.2017.06.006.
- Roehrborn CG, Siami P, Barkin J, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57(1):123–131. doi: 10.1016/j.eururo.2009.09.035.
- Ulchaker JC, Martinson MS. Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Clinicoecon Outcomes Res. 2018;10:29–43. doi: 10.2147/CEOR.S148195.
- Sahakyan Y, Erman A, Bhojani N, et al. Pharmacotherapy vs. minimally invasive therapies as initial therapy for moderate-to-severe benign prostatic hyperplasia: a cost-effectiveness study. Prostate Cancer Prostatic Dis. 2023;26(1):113–118. doi: 10.1038/s41391-022-00561-2.
