Abstract
Objectives
To characterize people who died by suicide after having previous contacts with public health system using the data available in a primary care setting.
Method
A retrospective, population-based case-control study identified through autopsy reports subjects who died from suicide between 2010 and 2015 in Barcelona province. Those who had previous interaction with primary healthcare services were selected, and 20 controls per case with similar age, sex and residence area were randomly sampled from a primary healthcare medical database; the available medical data derived from routine primary care records were anonymised and retrieved for analysis in all subjects.
Results
Of 2109 people deceased by suicide, 971 had previous primary healthcare interactions; 33.8% aged over 65 and 74% men. Of those with previous contact, 33% died during the week after and 58.5% within one month. A multivariable analysis identified several significant risk factors in the database, including previous suicide attempts, psychiatric diagnosis, number of primary healthcare visits, referrals to mental health, number of drugs prescribed, recent psychoactive drug prescriptions, and being on sick leave due to mental conditions in the previous year.
Conclusions
Nearly half of suicide subjects contacted primary healthcare before dying but remained either undetected or not effectively managed for prevention. In cases who interacted, available data on risk factors included high frequentation and being on sick leave due to mental health disorders, in addition to other well-known factors. Routine electronic medical records represent an opportunity to provide clinical-decision support tools that could be implemented through automatized risk calculation.
Most of suicide patients had a recent interaction with the healthcare system
Well known risk factors were available in the routine electronic medical records
Additional alerting tools could be implemented through automatized risk calculation
HIGHLIGHTS
INTRODUCTION
Suicide happens in all regions of the world and throughout all stages of life. There were approximately 800,000 suicide deaths worldwide in 2016, which indicates a rate of 10.5 per 100,000 population globally (World Health Organization, Citation2018). Its incidence is high, so it has been said that every 40 seconds a suicide occurs somewhere in the world. In addition, for every suicide there are more than 20 suicide attempts (World Health Organization, Citation2014). It is remarkable that, in the young population between 15 and 29 years, suicide is the second cause of death worldwide (World Health Organization, Citation2014). Thus, suicide constitutes one of the most important problems of world public health, and preventive strategies are needed (World Health Organization, Citation2013). Detection of subjects at high risk is one of the key elements to implement preventive strategies.
Many risk factors have already been repeatedly described and reported as associated with an increased risk of death by suicide in many settings, such as a history of previous suicide attempts or deliberate self-harm behavior, previous psychiatric disorders, either previously diagnosed or ascertained through psychiatric autopsies, substance misuse, family history of suicide, physical diseases and recent hospital admission, chronic pain, job or financial loss, or exposure to suicide, amongst others. Gender and older age are also related to suicidal behavior, so that women have more suicide ideation and suicide attempts, but men have higher rates of suicide deaths. The risk of suicide increases proportionally to the number of concurrent risk factors, although some have a greater specific weight than others, and may vary in different societies and cultures (Cavanagh, Carson, Sharpe, & Lawrie, Citation2003; Turecki & Brent, Citation2016).
Up to 80% of subjects contact primary care services during the last year prior to suicide, and from 45% to 66% do so in the month prior, so that placing suicide prevention strategies and interventions within the primary health care setting is important (Andersen, Andersen, Rosholm, & Gram, Citation2000; Stene-Larsen & Reneflot, Citation2019; Turecki & Brent, Citation2016; World Health Organization, Citation2013, Citation2014). A pilot study showed that less than 40% of healthcare professionals assess suicide risk in these last contacts and all of them fail to detect this risk despite the assessment (Draper, Snowdon, & Wyder, Citation2008). One of the WHO proposed actions to improve global mental health considers to integrate mental health into the routine health information system in order to improve prevention strategies (World Health Organization, Citation2013). Many of the already known risk factors (Cavanagh et al., Citation2003; Stene-Larsen & Reneflot, Citation2019; Turecki & Brent, Citation2016; World Health Organization, Citation2013, Citation2014, Citation2018) may be already available in the patient’s primary care routine medical records; also, other characteristics of patient’s interactions with the healthcare system may be able to detect subjects at risk (Stene-Larsen & Reneflot, Citation2019), and may be retrieved using data readily available in primary healthcare.
Aims of the Study
Our aim was to describe known and potential risk factors of death by suicide using a data available in electronic medical routine records of primary care, applying a case-control approach, and to identify items that might be used to improve detection of high risk patients in primary care.
MATERIALS AND METHODS
Study Design and Participants
A retrospective, population-based, case-control study was carried out. Cases were identified from the registry of the Institut de Medicina Legal i Ciències Forenses (IMLCF, Institute of Legal Medicine and Forensic Sciences) of Catalonia of deceased subjects in the province of Barcelona during the period from 2010 to 2015. IMLCF is the official organization responsible of doing and registering all the legally required autopsies in Catalonia. Subjects whose death certificate got any of the ICD 10 codes “Intentional self-harm” codes (Supplementary Table 1) as cause of death were selected, and their autopsy records were manually checked for confirmation of the cause of death.
Sistema d’Informació per al Desenvolupament de la Investigació en Atenció Primària (SIDIAP, Information System for the Development of Research in Primary Care) is a database that includes the medical history electronic registries from Institut Català de Salut (ICS, Catalan Health Institute). This database contains longitudinal information since 2006 from the e-CAP program, a computerized medical record system used at ICS in primary care. Information is gathered from 287 primary healthcare centers, with an assigned population of 5.605.293 inhabitants (76.3% of the Catalan population); in the Barcelona province, the assigned population is 4.189.554 inhabitants (76.4% of the Barcelona population) (SIDIAP, Citationn.d.).
In the Catalan Health System, insured subjects are assigned a unique code, the Personal Identification Code (PIC), an alphanumeric sequence built using 4 letters of surnames, gender, date of birth and some additional items (Generalitat de Catalunya, Citation2015). The PIC univocally identifies a subject in many healthcare databases of Catalonia, allowing provision of services and linking of information from a number of sources, including SIDIAP. However, the PIC is not used by IMLCF. Since the two databases did not share an identifier, the final selection of cases was carried out in a three-phase process: Firstly, a PIC identifier in mortality database was created based on surnames, gender and date of birth (or age if DOB wasn't available) as present in the autopsy records, or a proxy was built using best possible approach if data were missing. The mortality PIC was then searched in SIDIAP by means of probabilistic models. For each case in the mortality database, none, one or more than one possible candidates were obtained. Secondly, a manual review was done blindly by a third person, an administrative who did not know the purpose of the study, in order to select the most probable candidate/s matching the code.
Cases who did not have any activity or records in the SIDIAP during the period of the study, or who had clinical data recorded many days after the decease date, were excluded (see supplementary materials). Also, 20 controls per case that were alive on the index date were randomly sampled from SIDIAP database to obtain similar distribution of sex, age (±2 years) and residence area than the cases. Data on demographics (age, sex, BMI, socioeconomic status according to area of residence, employment status, use of social services), clinical data (structured data on BMI, use of toxics, co-morbidities (Charlson, Szatrowski, Peterson, & Gold, Citation1994), and ICD10 codes for previous and current health problems), type and number of health care interactions, and drug dispensation data for public financed treatments (Supplementary Table 2) were obtained from the SIDIAP database. All personal identification was permanently removed from the data before release to the research team. The data extraction and anonymization was done by personnel who were not part of the research team, so that no personal information on cases or controls was available to the investigative team at any time.
No formal sample size calculation was done, because the number of cases was determined by availability of reliable data since 2010 and mortality due to suicide. The number of 20 controls per case was chosen to enhance the chance of observing exposures to risk factors of low prevalence in the control group.
Statistical Methods
Qualitative variables were described by the number of valid values and the frequency and percentage of each category. Quantitative variables were described by measures of central tendency and dispersion and were categorized applying commonly used criteria (age, BMI, Chalson index, polimedication) or by applying clinical criteria (number of previous visits in last year). Where required, a category including missing values was used in the analysis; no missing data imputation was done. Odds ratios and their confident intervals were calculated by comparing cases versus controls in each of the different categories using the mid-p method (Rothman, Greenland, & Associate, Citation2008). In polytomous variables, ratios are shown with respect to an assigned reference level.
A multivariable analysis was performed to identify the potential risk factors of suicide. For feature selection, we used a random forest algorithm to previously select up to 15 variables that classify better between cases and controls based on their Gini index (Breiman, Citation2001). Then, with this set of variables, a logistic regression model was fitted choosing the final model by AIC in a stepwise algorithm. The goodness-of-fit of the final model was evaluated by means of ROC curves.
All analyses were performed using the R statistical package (R. D. C. Team, Citation2011) with a significance level of 0.05.
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Independent Ethics Committee of IDIAP Jordi Gol (approval number P16/010), and was communicated to the Agencia Española de Medicamentos y Productos Sanitarios (Spanish Agency of Medicines and Medical Devices) in compliance with local regulations. Because population-based medical records were used for epidemiological purposes and only anonymised data were used, a waiver for informed consent was issued by the Ethics Committee.
RESULTS
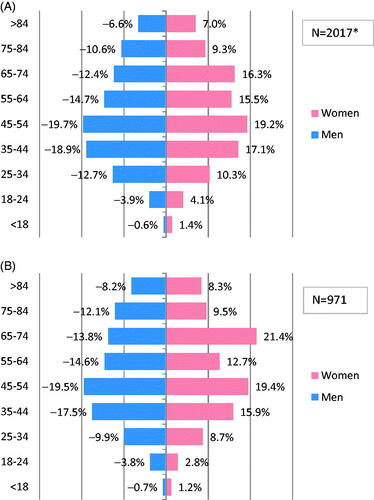
During the study period (2010–2015), a total of 2,109 deaths were registered as due to suicide in the province of Barcelona. Using the total number of people living in Barcelona (Instituto Nacional de Estadística, Citation2016) as denominator, we may extrapolate that an average of 6.36 deaths by suicide per 100,000 people in the province of Barcelona have happened during the study period (9.70 for men and 3.14 for women). These data are roughly consistent with previously published estimations (Supplementary Figure 2) (Generalitat de Catalunya, Citation2018). After excluding unidentifiable subjects, duplicate records, subjects not affiliated to healthcare in Barcelona and subjects lacking medical records in the public health system, 1,281 subjects (60.7%) were searched in SIDIAP, of which 971 (75.8%) had clinical data available in the database resulting from affiliation to ICS in Barcelona and previous healthcare interactions (Supplementary Figure 1). The age distribution of all deceased subjects and of those with previous primary healthcare interactions are shown in , respectively; those with previous primary care interactions were slightly older than the full set of cases, and the proportion of women aged 65–74 years was 21.4% as compared with 16.3% in the full set of cases.
FIGURE 1. Age and sex of cases. (A) All identified cases of death by suicide. (B) Cases of death by suicide with previous primary care interactions. *Total number of cases 2109, missing values for age in 92 cases.
The main characteristics of the identified cases and of those with previous healthcare interactions in primary care were similar, and have been summarized in Supplementary Table 3. The most frequent mechanisms of suicide included hanging/suffocating, jumping from height and self-poisoning, with differences between men and women (Supplementary Table 4) and similar for subjects with previous interactions with primary healthcare and in the full set (Supplementary Table 3).
The proportion of subjects who had healthcare interactions at any time before death was 46%; overall, 36% contacted within three months before suicide, 27% did it within one month and 15% during the week before suicide ().
TABLE 1. Period of time since the last contact to primary care on suicide patients.
A total of 19,420 controls with previous healthcare interactions in primary care were selected with similar age, sex and residence area, resulting in a database with a total of 20,391 subjects (Supplementary Figure 1). summarizes the main characteristics of the case and control cohorts. Overall, 74% of subjects were male, and the mean age was 56.37 (18.9) years [57.27 (18.75) years for women and 56.02 (18.94) years for men]. Most subjects lived in urban areas. There were no differences in BMI between cases and controls; most of the subjects had overweight or were obese (63.2%). The antecedent of “having smoked” (obtained from a specific clinical record and also ICD-10 codes) was affirmative in 54% of cases and 39% of controls.
TABLE 2. Description of characteristics of cases and controls (univariate model).
Cases and controls significantly differed in the proportion of subjects with previous history of autolytic attempt (5.66% of cases and 0.1% of controls), and in the proportion of subjects with at least one record of sick leave in the year before suicide and who were on sick leave at the index date; sick leave related to mental health disorders was also more frequent amongst cases (). Cases also used more frequently the primary care health services and the public social services than controls. The prevalence of exposure to any drug was higher among cases, specifically the exposure to at least one psychoactive drug. Significantly more cases had a Charlson Index of high comorbidity, as compared to controls, and psychiatric disorders were more prevalent in cases ().
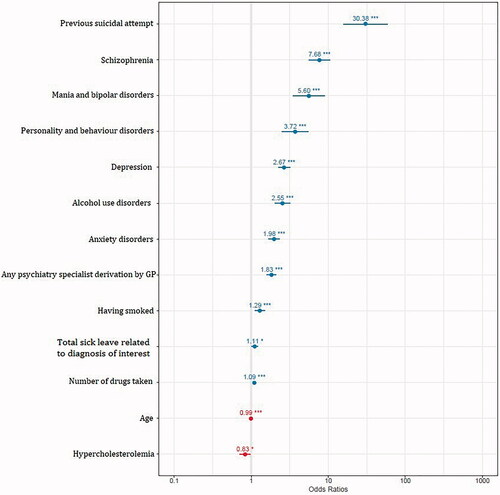
The most prevalent psychiatric lifetime diagnoses recorded in the database for cases were substance use disorders, anxiety disorders and mood (affective) disorders (40.5, 36.3, and 32.8%, respectively) (). The multivariable analysis model identified a number of significant risk factors ( and Supplementary Table 5). Those with stronger associations included a previous suicide attempt, and several psychiatric disorders (schizophrenia, mania and bipolar disorders, personality and behavior disorders, depression, alcohol use disorders and anxiety disorders) already available in the medical records. Also, in univariate models we observed significant associations for increased risk of suicide for some non-psychiatric conditions, in descending order for fibromyalgia, epilepsy, vestibular disorders, migraine and osteoarthritis. While vestibular disorders, osteoarthritis and migraine had Gini scores above 7 and were included in the multivariable model, these variables did not remain significant in final adjusted analysis. Any mental health specialist derivation by GP, having smoked, being or having been on sick leave due to diagnoses related to mental health, and the number of drugs taken were also identified as risk factors.
TABLE 3. Psychiatric and non-psychiatric comorbidity (univariate model).
DISCUSSION
In our setting, roughly half of subjects who died by suicide had previous interactions in primary care. We summarized their main risk factors, as retrieved from already available information in the routine electronic primary care medical records. The comparison with controls allowed to confirm that well known factors, as well as some other characteristics related to the use of medical and social services, were associated to increased risk, so that high risk was associated to previous suicide attempts, a previous lifetime diagnosis of several mental disorders, increased number of medications and use of psychoactive medications, previous derivation to mental health specialists, frequent use of primary care health services and being on sick leave on the year before.
Previous studies reporting risk factors either focused on suicidal behavior in specific conditions or in given populations, or used clinical coding from medical or administrative databases to identify cases, which have previously been questioned as unreliable due to under or over reporting (Morgan et al., Citation2018). We have been able to exhaustively identify confirmed cases through coroners’ reports because a single institution, IMLCF, does all autopsies for our province.
The population studied was chosen based on availability of exhaustive data from judicial autopsies done in the Barcelona province for the study period. Judicial autopsies are mandatory for a number of circumstances where medical care does not allow to clearly establish the cause of death, or whenever self-harm, violent or criminal causes cannot be excluded (Boletín Oficial del Estado, Citation1882). Whether the sample is exhaustive cannot be ensured, since the thoroughness of the data collected in the Mortality Registry on deaths due to external causes may be suboptimal (Gotsens et al., Citation2011), and an underreporting may occur. We cannot discard that, some coded deaths attributed to accidental or natural causes such as traumatic injuries not specified (X59) or unspecified obstruction of breathing (W48) respectively, can be actually due to undetected suicide (Puigdefàbregas et al., Citation2013). We decided to include only data from unequivocal cases of suicide; however, other alternative approaches that also include potential cases of suicide are also a consistent approach. We have checked how many subjects could have been included in our study if we had considered codes Y10-Y34, and according to the national statistics the maximum number of additional subjects, assuming all of them were actually deaths due to suicide, would have been 36 (Instituto Nacional de Estadística, Citation2016).
Only 46% of the cases had previous interactions with primary care, which can be considered lower than the average reported in a recent systematic review (Stene-Larsen & Reneflot, Citation2019), although similar to that reported in some countries such as Canada (37%) (Vasiliadis, Ngamini-Ngui, & Lesage, Citation2015) or Scotland (46.4%) (Stark, Vaughan, Huc, & O’Neill, Citation2012) which have similar statistics on suicidality to those of Spain (Instituto Nacional de Estadística, Citation2016; World Health Organization, Citation2014). Considering that the rates of suicide derived from our case identification are consistent with the expected number of cases in Spain (Supplementary Figure 2), this low percentage may be interpreted in a number of ways; it may mean either that the access to primary medical care is more difficult in our setting, that seeking of medical help in our setting is culturally different, or that, the effectivity of detection and management of cases in our primary care system is associated to a lower lethality rate (the Spanish rate of death by suicide is in the low boundary of those reported globally) (Instituto Nacional de Estadística, Citation2016; World Health Organization, Citation2014, Citation2018). In any case, in our cohort the system for detection and prevention failed for 46% of subjects.
Regarding the timing of healthcare contacts, data in the literature reports that the percentage of patients that contacted healthcare within 3 months was in average 41% (range 17–50%), within 1 month it was 44% (range 17–73%), and one week prior to suicide the rate was 16% (range 12–21%) (Stene-Larsen & Reneflot, Citation2019). Our data shows consistent percentages of interactions with healthcare, although in the lower bound of those reported, with 15% of all suicidal subjects contacting primary care in the week before, 27% in the month before and 36% within 3 months of death. While in absolute terms this represents 757 subjects for whom an intervention could had been tried if detected, low rates of healthcare interaction by subjects at high risk may be regarded as an area for improvement in our setting.
The 971 cases known to the system as compared to the full set of identified cases by autopsy showed a higher proportion of women aged 65–74 amongst those with previous interactions as compared to those without contacts. Contrarily, younger age groups were slightly more represented in the complete set of cases. This is consistent with previous reports (Stene-Larsen & Reneflot, Citation2019) and may reflect a general trend in the use of healthcare systems (Wang, Hunt, Nazareth, Freemantle, & Petersen, Citation2013).
Regarding suicidal methods, in our sample we observed a higher proportion of subjects who died by suicide by jumping on a moving object, jumping from height or by self-poisoning, with lower rates of suicide by hanging, firearms or drowning as compared with methods referred for the Spanish population (Instituto Nacional de Estadística, Citation2016). Differences may be explained by the proportion of population living in rural areas (20.3% in Spain (Goerlich Gisbert & Cantarino Martí, Citation2015) and 13.8% in our cohort, respectively). The availability of train and underground in urban areas may be a strong influence; contrarily, access to firearms, mainly weapons used for hunting, might be higher in rural areas of Spain. Access to firearms is a known influence on methods of suicide; our sample shows a similar profile to other European countries where weapons are tightly controlled, and different from United States, where easier access is accompanied by use of firearms in up to 50% of suicides (Mann & Michel, Citation2016).
There were no substantial differences in the general characteristics (age, sex, year of decease and the main method of suicide) of those subjects with and without previous contact with primary care, although an inherent limitation of the study is the scarcity of information on subjects that were unknown to the healthcare system at the time of decease, which precludes to compare the full characteristics of these subjects to those with previous medical records.
Strengths of using routine electronic medical records for retrospective assessment of risk include the fact that the variables used are already existing records, and as such are not subject to recall bias. However, only those variables present in administrative and clinical structured records are available for adjustment, and thus may be incomplete to reflect other clinically relevant risk factors. In particular, our data lacked detailed information on hospitalization and use of specialized mental health care, which in Catalonia is offered by a number of different health services providers and yet cannot be directly linked to primary care databases. Also, when considering drug exposure, we used invoicing information, but we cannot ensure that all dispensed medication had actually been taken. Despite these limitations, we consider that our approach to the study of risks factors for suicide based on clinical and administrative information is appropriate, since the use of databases has been able to capture information on enough number of relevant risk factors.
Most of our results confirmed previous reports from the literature regarding increased risks associated to previous suicide attempt, a diagnosis of schizophrenia, mania and bipolar disorders, personality and behavior disorders, depression, alcohol use disorder, anxiety disorders and having smoked. Similar to other series, our cohort of people who died by suicide included mainly senior male (Cavanagh et al., Citation2003; Morgan et al., Citation2018; Turecki & Brent, Citation2016).
We have been able to retrieve relevant medical and administrative information available at the primary care level that allows to obtain information on well described risk factors, as well as to identify other readily available information associated to increased risk in our sample. We observed that the number of psychiatry referrals, the number of drugs taken and being on sick leave related to psychiatric conditions were all associated to higher risk. Also, the number of interactions with healthcare in the year previous to suicide was higher in cases, and in particular the interactions in the primary care setting. The fact that people dying by suicide were more likely to have been followed by a primary care provider has been previously described in our setting (Parra Uribe et al., Citation2013). Our observations confirms once again that often suicide patients contact the healthcare system, but remain either undetected for high risk of suicide, or not effectively managed for prevention (Turecki & Brent, Citation2016). In this prospect, the availability through the electronic medical records of data on many risk factors may represent an opportunity for intervention (Bright et al., Citation2012; Horrocks, Michail, Aubeeluck, Wright, & Morriss, Citation2018). The use of available information on risk factors may allow producing clinical decision support systems assisting healthcare professionals, I ex: by prompting specific diagnostic tools in subjects with several high-risk factors. Because a unique identification public healthcare code is available for all subjects in Catalonia (Generalitat de Catalunya, Citation2015), currently missing information on relevant risk factors, such as data on previous hospitalization and mental healthcare interactions of subjects, may be retrieved if interoperability of data is prioritized at the healthcare system level.
In conclusion, nearly half of suicide subjects contacted primary healthcare before dying and one third of those contacting died during the week after; thus they remained either undetected or not effectively managed for prevention. It is noteworthy that, for cases that interacted with primary care, well known risk factors were available in the routine electronic medical records. This circumstance represents an opportunity to provide additional alerting tools that could be implemented through automatized risk calculation.
AUTHOR NOTES
Marc Fradera, PhD, Researcher, Department of Pharmacology, Therapeutics and Toxicology, Unitat Docent Parc Taulí, Facultat de Medicina, Universitat Autònoma de Barcelona, Sabadell, Spain. Parc Taulí Hospital Universitari, Institut d’Investigació iInnovació Parc Taulí I3PT, Universitat Autònoma de Barcelona, Sabadell, Spain.
Dan Ouchi, Researcher, Unitat d’Estudi del Medicament. Institut Universitari d'Investigació en Atenció Primària Jordi Gol, Barcelona, Spain.
Oriol Prat, Researcher, Unitat d’Estudi del Medicament. Institut Universitari d'Investigació en Atenció Primària Jordi Gol, Barcelona, Spain.
Rosa Morros, MD PhD, Coordinator, Unitat d’Estudi del Medicament. Institut Universitari d'Investigació en Atenció Primària Jordi Gol, Barcelona, Spain; Medical Associate Professor, Department of Pharmacology, Therapeutics and Toxicology, Unitat Docent Sant Pau, Facultat de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain.
Carles Martin-Fumadó, MD PhD, Deputy director. Institut de Medicina Legal i Ciències Forenses de Catalunya, Barcelona, Spain.
Diego Palao, MD PhD, Director, Department of Mental Health, University Hospital Parc Taulí, Institut d'Investigació i Innovació Parc Taulí. CIBERSAM, Sabadell, Spain; Professor, Department of Psychiatry and Forensic Medicine, Unitat Docent Parc Taulí, Facultat de Medicina. Universitat Autònoma de Barcelona, Sabadell, Spain.
Narcís Cardoner, MD PhD. Senior consultant, Department of Mental Health, University Hospital Parc Taulí. Institut d'Investigació i Innovació Parc Taulí. CIBERSAM, Sabadell, Spain; Medical Associate Professor, Department of Psychiatry and Forensic Medicine, Unitat Docent Parc Taulí, Facultat de Medicina, Universitat Autònoma de Barcelona, Sabadell, Spain.
Maria Teresa Campillo, MSc. Researcher, Institut de Neuropsiquiatria i Addiccions, Hospital del Mar, Institut Municipal d’Investigació Mèdica, CIBERSAM, Barcelona, Spain; Department of Psychiatry and Forensic Medicine, Unitat Docent Parc Salut Mar, Universitat Autonoma de Barcelona, Barcelona, Spain.
Víctor Pérez-Solà, MD PhD. Director, Institut de Neuropsiquiatria i Addiccions, Hospital del Mar, Institut Municipal d’Investigació Mèdica, CIBERSAM, Barcelona, Spain; Department of Psychiatry and Forensic Medicine, Unitat Docent Parc Salut Mar, Universitat Autonoma de Barcelona, Barcelona, Spain.
Caridad Pontes, MD, PhD, Associate Professor, Department of Pharmacology, Therapeutics and Toxicology, Unitat Docent Parc Taulí, Facultat de Medicina, Universitat Autònoma de Barcelona, Sabadell, Spain; Manager of Pharmacotherapeutic Harmonization Program, Medicines Area, Catalan Health Service, Barcelona, Spain.
AUTHOR CONTRIBUTIONS
MF, RM, VP, CM-F, CP, and all the authors contributed to the study concept and design. MF, CM-F, RM, VP, MC and CP collected or supervised the data collection. DO, OP and MF did the data analysis and wrote the findings in the initial manuscript. RM, CP and all the authors provided a careful statistical and methodological revision of the manuscript and contributed to the final draft. MF, RM, VP, DP, NC and CP contributed to the interpretation of the results. All authors had full access to all data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Supplemental Material
Download MS Word (166.3 KB)ACKNOWLEDGEMENTS
The study is part of the PhD project of Marc Fradera at the Department of Pharmacology, Therapeutics and Toxicology of the Universitat Autònoma de Barcelona.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
DATA AVAILABILITY STATEMENT
The terms of access to the data agreed by Institut Català de la Salut and Institut de Medicina Legal i Ciències Forenses indicate that the database can be used only for the purpose of the authorized study and cannot be transferred to third parties.
Additional information
Funding
REFERENCES
- Andersen, U. A., Andersen, M., Rosholm, J. U., & Gram, L. F. (2000). Contacts to the health care system prior to suicide: A comprehensive analysis using registers for general and psychiatric hospital admissions, contacts to general practitioners and practising specialists and drug prescriptions. Acta Psychiatrica Scandinavica, 102(2), 126–134. doi:10.1034/j.1600-0447.2000.102002126.x
- Boletín Oficial del Estado. (1882). Real Decreto de 14 de septiembre de 1882 por el que se aprueba la Ley de Enjuiciamiento Criminal. BOE 260; 17/09/19882 updated by BOE 296; 11/12/2015. Retrieved August 4, 2019, from https://www.boe.es/eli/es/rd/1882/09/14/(1)/con.
- Breiman, L. (2001). Random forests. Machine Learning, 45(1), 5–32. doi:10.1023/A:1010933404324
- Bright, T. J., Wong, A., Dhurjati, R., Bristow, E., Bastian, L., Coeytaux, R. R., … Lobach, D. (2012). Effect of clinical decision-support systems: A systematic review. Annals of Internal Medicine, 157(1), 29–43. doi:10.7326/0003-4819-157-1-201207030-00450
- Cavanagh, J. T., Carson, A. J., Sharpe, M., & Lawrie, S. M. (2003). Psychological autopsy studies of suicide: A systematic review. Psychological Medicine, 33(3), 395–405. http://www.ncbi.nlm.nih.gov/pubmed/12701661.
- Charlson, M., Szatrowski, T. P., Peterson, J., & Gold, J. (1994). Validation of a combined comorbidity index. Journal of Clinical Epidemiology, 47(11), 1245–1251. doi:10.1016/0895-4356(94)90129-5
- Draper, B., Snowdon, J., & Wyder, M. (2008). A pilot study of the suicide victim’s last contact with a health professional. Crisis, 29(2), 96–101. doi:10.1027/0227-5910.29.2.96
- Generalitat de Catalunya. (2015). ORDRE SLT/330/2015, de 20 d’octubre, per la qual es regulen el contingut i el model de la targeta sanitària individual a Catalunya. Retrieved from https://portaljuridic.gencat.cat/ca/pjur_ocults/pjur_resultats_fitxa/?action=fitxa&mode=single&documentId=706589&versionId=1452634&language=ca_ES.
- Generalitat de Catalunya. (2018). Observatori del Sistema de Salut de Catalunya. Mortalitat. Retrieved February 20, 2019, from http://salutweb.gencat.cat/ca/el_departament/estadistiques_sanitaries/dades_de_salut_i_serveis_sanitaris/mortalitat/.
- Goerlich Gisbert, F. J., & Cantarino Martí, I. (2015). Estimaciones de la población rural y urbana a nivel municipal. Estadística Española, 57(186), 5–28.
- Gotsens, M., Marí-Dell'Olmo, M., Rodríguez-Sanz, M., Martos, D., Espelt, A., Pérez, G., … Borrell, C. (2011). Validation of the underlying cause of death in medicolegal deaths. Revista Espanola de Salud Publica, 85(2), 163–174. doi:10.1590/S1135-57272011000200005
- Horrocks, M., Michail, M., Aubeeluck, A., Wright, N., & Morriss, R. (2018). An electronic clinical decision support system for the assessment and management of suicidality in primary care: Protocol for a Mixed-Methods Study. JMIR Research Protocols, 7(12), e11135. doi:10.2196/11135
- Instituto Nacional de Estadística. (2016). Instituto Nacional de Estadística (España). INEbase. Retrieved March 6, 2019, from http://www.ine.es/inebmenu/indice.htm.
- Mann, J. J., & Michel, C. A. (2016). Prevention of firearm suicide in the United States: What works and what is possible. American Journal of Psychiatry, 173(10), 969–979. https://doi.org/10.1176/appi.ajp.2016.16010069.
- Morgan, C., Webb, R. T., Carr, M. J., Kontopantelis, E., Chew-Graham, C. A., Kapur, N., & Ashcroft, D. M. (2018). Self-harm in a primary care cohort of older people: Incidence, clinical management, and risk of suicide and other causes of death. The Lancet Psychiatry, 5(11), 905–912. doi:10.1016/S2215-0366(18)30348-1
- Parra Uribe, I., Blasco-Fontecilla, H., García-Parés, G., Giró Batalla, M., Llorens Capdevila, M., Cebrià Meca, A., … Palao Vidal, D.J. (2013). Attempted and completed suicide: Not what we expected? Journal of Affective Disorders, 150(3), 840–846. doi:10.1016/j.jad.2013.03.013
- Puigdefàbregas, A., Freitas, A., Gibert, A., Zaragoza, S., Ribas, G., & Domènech, J. (2013). Estadístiques de mortalitat a Catalunya i lʼEstat espanyol. Impacte del canvi de documents i circuits per comunicar les defuncions. Butlletí Epidemiològic de Catalunya, 24, 1–13. http://hdl.handle.net/11351/2199.
- R. D. C. Team. (2011). R: A language and environment for statistical computing (Vol. 2). Vienna, Austria: R Foundation for Statistical Computing.
- Rothman, K. J., Greenland, S., & Lash, T. L. (2008). Modern epidemiology. Lippincott Williams & Wilkins.
- SIDIAP. (n.d). SIDIAP: Information system for research in primary care. Retrieved August 4, 2019, from https://www.sidiap.org/index.php/en/database/general-details.
- Stark, C. R., Vaughan, S., Huc, S., & O’Neill, N. (2012). Service contacts prior to death in people dying by suicide in the Scottish Highlands. Rural and Remote Health, 12, 1876. http://www.ncbi.nlm.nih.gov/pubmed/22856505.
- Stene-Larsen, K., & Reneflot, A. (2019). Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017. Scandinavian Journal of Public Health, 47(1), 9–17. doi:10.1177/1403494817746274
- Turecki, G., & Brent, D. A. (2016). Suicide and suicidal behaviour. The Lancet, 387(10024), 1227–1239. doi:10.1016/S0140-6736(15)00234-2
- Vasiliadis, H.-M., Ngamini-Ngui, A., & Lesage, A. (2015). Factors associated with suicide in the month following contact with different types of health services in Quebec. Psychiatric Services, 66(2), 121–126. doi:10.1176/appi.ps.201400133
- Wang, Y., Hunt, K., Nazareth, I., Freemantle, N., & Petersen, I. (2013). Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open, 3(8), e003320. doi:10.1136/bmjopen-2013-003320
- World Health Organization. (2013). Mental health action plan 2013–2020. Retrieved from https://www.who.int/publications/i/item/9789241506021.
- World Health Organization. (2014). Preventing suicide. A global imperative. Retrieved from http://www.who.int/iris/handle/10665/131056.
- World Health Organization. (2018). Mental health atlas 2017. Retrieved from https://www.who.int/mental_health/evidence/atlas/mental_health_atlas_2017/en/.