Abstract
Background
Emergency department (ED) staff are often the first point of contact for individuals in suicidal crisis. Despite this, there is no published research systematically examining the factors influencing decision-making for this patient group.
Methods
MedLine, CINAHL, PsycINFO, Web of Science and Cochrane Library databases were searched for three key concepts: (1) suicide, (2) accident and emergency department and (3) decision-making. Three reviewers screened titles, abstracts and full papers independently against the eligibility criteria. Data synthesis was achieved by extracting and analyzing study characteristics and findings. The Mixed Methods Appraisal Tool (MMAT) was used to assess the quality of included studies.
Results
Seventeen studies met the eligibility criteria and were included in this systematic review. Studies were published from 2004 to 2020 and were of good methodological quality. A number of patient (method of self-harm, age, gender), contextual (availability of services and staff) and staff-related factors (attitudes, training, knowledge) were reported to influence decision-making for patients in suicidal crisis presenting to EDs.
Conclusion
Decision-making in the ED is complex and is influenced by patient, contextual and staff-related factors. These decisions can have an impact on the future care and clinical pathways of patients in suicidal crisis. Additional training is needed for ED staff specifically related to suicide prevention.
INTRODUCTION
Suicide is a major public health issue (World Health Organisation, Citation2019). A total of 5,224 deaths by suicide were registered in England and Wales in 2020 (Office of National Statistics, Citation2021). Suicidal thoughts and self-harm are associated with greater distress and are strong risk factors for death by suicide; indeed, individuals in crisis often need rapid care to minimize potential harm (Kienhorst, Citation1995). The prevalence of self-harm has been shown to have increased from 2.4% in 2000 to 6.4% in 2014 (McManus et al., Citation2019). This increasing prevalence of suicide-related thoughts and behaviors are a significant burden on the National Health Service (NHS) (Naghavi, Citation2019; Vigo, Kestel, Pendakur, Thornicroft, & Atun, Citation2019).
The rates of suicidal presentations to EDs are rising and there has been a general increase in self-harm presentations between 2009 and 2018 (Stapelberg, Sveticic, Hughes, & Turner, Citation2020). An estimated 150,000 people experiencing self-harm present to EDs annually, accounting for 220,000 presentations (Hawton et al., Citation2007), with this figure expected to be much higher due to inconsistencies in coding (McCarthy, Saini, Nathan, & McIntyre, Citation2021). EDs are therefore a key setting for suicide prevention (Miller et al., Citation2017; Siry et al., Citation2021).
ED staff are often the first point of contact for individuals experiencing suicide-related distress (Ceniti, Heinecke, & McInerney, Citation2020; Perera et al., Citation2018). Despite this, staff receive minimal psychiatric training and few opportunities for additional education on the care of patients presenting for suicidal emergencies (Knorr et al., Citation2020; Zun, Citation2012). The National Institute for Health and Care Excellence (NICE) guidelines highlight the important role EDs have in the treatment, support and management of patients who self-harm (Carr et al., Citation2016; Morgan et al., Citation2018). However, there are no recommendations for the management of suicidal ideation within EDs (National Institute for Health and Care Excellence (NICE), Citation2004).
Previous research suggests that several factors impact the decision-making and treatment for patients presenting in suicidal crisis. Most notable are factors related to a person’s suicidal presentation (i.e., intent) and history (i.e., prior suicide attempt) (Miret et al., Citation2011; So et al., Citation2021; Unick et al., Citation2011). Staff-related factors have also been reported frequently in the literature. Specifically, a clinician’s attitude toward self-harm, training and knowledge have been shown to influence patient experience and subsequent care (Owens, Hansford, Sharkey, & Ford, Citation2016; Saunders, Hawton, Fortune, & Farrell, Citation2012). The majority of research, however, is based in psychiatric hospital units which often reflect more severe and complex cases. There are a large cohort of patients who experience suicide-related thoughts and behaviors who are therefore not captured in this research.
Although research emphasizes the importance of appropriate treatment plans and care pathways for patients in suicidal crisis, both internal and external factors may hinder the care of such patients. There is no synthesized evidence regarding the factors that affect decision-making of ED staff involved in the management of this group. The aim of this systematic review is to examine patient, contextual and staff factors influencing ED decision-making and how these specific factors can affect clinical pathways for patients presenting in suicidal crisis, with self-injury and/or following a suicide attempt.
METHOD
Protocol
The protocol was registered with PROSPERO (CRD42022303429). Available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=303429
Search Strategy
A comprehensive search for relevant studies was conducted on five electronic databases (MedLine, CINAHL, PsycINFO, Web of Science and Cochrane Library) for three key concepts: (1) suicide, (2) accident and emergency department and (3) decision-making. Search terms were revised after the initial searches revealed new terms. MeSH terms were run in combination with free-text searches of titles and abstracts. A supplementary search was conducted to include the term “disposition” following review of the included papers.
Eligibility Criteria
Studies were included if they reported factors affecting the decision-making of ED staff, including medical (e.g., triage nurses, ED doctors) and mental health staff (e.g., mental health nurses, consultant liaison psychiatrists). Studies were included if theory or past research hypothesized the factor would be related to decision-making. Studies were included regardless of whether they found significant effects related to clinical pathways or decision-making. Outcome variables were identified using relevant literature and included medical admission, self-discharge, psychiatric admission and psychosocial assessment. The study eligibility criteria are outlined in .
TABLE 1. Inclusion and exclusion criteria.
Study Screening and Selection
Three authors independently reviewed titles, abstracts and full texts against the eligibility criteria. Discrepancies were resolved though discussion. There was high agreement between authors (85%).
Data Extraction and Quality Assessment
Eligible full texts were subjected to data extraction and quality assessment by the primary author. Data were extracted on the study aims, design, location, sample size and demographic information. Detailed data relating to the factors influencing decision-making were also extracted.
The Mixed Methods Appraisal Tool (MMAT) was used to assess methodological quality of included studies (Pace et al., Citation2012; Pluye, Gagnon, Griffiths, & Johnson-Lafleur, Citation2009). All studies found in the review were included in data synthesis, regardless of risk of bias/quality assessment.
Data Synthesis
Narrative synthesis using the framework developed by Popay et al. (Citation2006) was conducted. Using synthesis tables, the sample characteristics and factors(s) influencing decision-making were reported. The relationship within and across studies were explored by examining the similarities and differences between them (see supplementary Table 1 for further information).
RESULTS
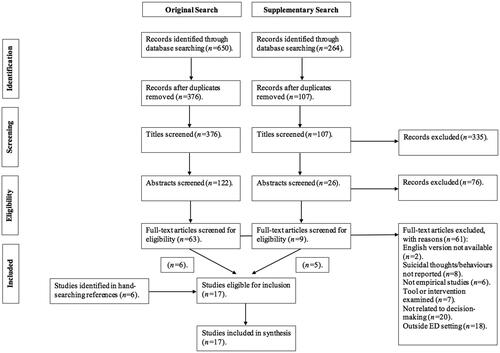
The search yielded 650 records from which 376 citations were screened. Sixty-one full texts were reviewed for eligibility. A supplementary search revealed an additional nine full texts to review. Seventeen studies were included in the final synthesis. outlines the flow of studies within the review.
FIGURE 1. PRISMA flow diagram indicating the steps taken to retrieve relevant articles for systematic review.
Study Characteristics
Included studies involved a range of ED staff (ED doctors, nurses, psychiatrists/psychiatry residents, medical record coders, ED managers) from Europe (n = 8), USA (n = 6), Australia (n = 2) and Asia (n = 1). The mean age of included participants was 34.84, with the majority of studies (n = 14) including more female than male participants. The majority of studies (n = 11) utilized hospital data sets as a means for data collection. Study characteristics and details are reported in .
TABLE 2. Studies included in this review.
Quality Assessment
The MMAT was used in this review. MMAT includes two screening questions followed by a series of additional questions dependent on the study design. These criteria are scored on a nominal scale (Yes/No/Can’t tell) and allow for the assessment of five main type of studies. Studies were rated as low (0–40%), medium (40–60%) or high quality (60%+). The majority of included studies (n = 12) scored high. Reasons for lower quality ratings were low response rate (n = 3), incomplete individual dataset (n = 1) and limited statistical analysis (n = 1). See supplementary Table 2 for further information on MMAT scores and the reasons for the assigned score.
Factors Influencing Decision-Making
The following section reports the primary outcomes of the systematic review: patient, contextual and staff factors that influence ED decision-making for individuals in suicidal crisis.
Patient
Patient-related factors were reported most frequently (n = 13). Method of self-harm was cited most commonly insofar as patients using more lethal means were more likely to be hospitalized (Arensman et al., Citation2018; Baca-García et al., Citation2004; Griffin, Gunnell, & Corcoran, Citation2020; Hepp, Moergeli, Trier, Milos, & Schnyder, Citation2004; Jimenez-Trevino et al. Citation2015; Phillips, Gerdtz, Elsom, Weiland, & Castle, Citation2015). One study reported ED visits for self-harm with suicidal ideation were most likely to result in hospitalization (94.7%), compared to suicidal ideation (84.0%) or self-harm alone (73.1%) (Schmutte, Olfson, Xie, & Marcus, Citation2019b). Similar findings were reported by Schmutte, Olfson, Xie, and Marcus (Citation2020), presentations for suicide attempts or suicidal ideation were less likely to be discharged than self-harm.
Age was shown as a key factor across included studies (Arensman et al., Citation2018; Griffin et al., Citation2020; Hepp et al., Citation2004; Jimenez-Trevino et al. Citation2015). Older patients were most commonly hospitalized, whereas younger patients were more likely to self-discharge (Griffin et al., Citation2020). One study, however, reported age to not be associated with hospitalization (Faris et al., Citation2019). Variation was reported in relation to gender; for example, Griffin et al. (Citation2020) found that males were more likely to self-discharge and be admitted into a psychiatric facility, whereas Faris et al. (Citation2019) reported increased hospital admission for females. Ethnicity was noted in one study which reported patients of an African American ethnicity were less likely to be hospitalized (Schmutte, Olfson, Xie, & Marcus, Citation2019a). Other patient factors, i.e., previous hospitalizations and axis I diagnosis (“mood disorder”) were also found to influence decision-making (Hepp et al., Citation2004; Jimenez-Trevino et al. Citation2015; Schmutte et al., Citation2019a, Citation2019b). Social support was noted in one study; Kroll et al. (Citation2018) reported 25% of patients who had been hospitalized could have been discharged had social support become available. Living alone and employment status was not associated with hospitalization (Faris et al., Citation2019). One study, however, reported that clinical pathways were not influenced by patient demographics, socioeconomic status and type of self-harm (Polling, Bakolis, Hotopf, & Hatch, Citation2019).
Contextual
Three studies noted contextual factors that affect ED decision-making. The availability of services and staff were reported across two studies (Griffin et al., Citation2020; Pope, Burn, Ismail, Harris, & McCoy, Citation2017). Hospital location affected future care of patients presenting with self-harm (Arensman et al., Citation2018). For example, there was a reduced risk of self-discharge if presentations were made outside of Dublin city, Ireland (Griffin et al., Citation2020). Hospital facilities (e.g., onsite psychiatric in-patient facilities) also increased the likelihood of patients being admitted to a psychiatric ward compared to hospitals where the facilities were located offsite (Griffin et al., Citation2020). Other contextual factors reported were busyness, time of the day and the 4-hour wait target in EDs. Specifically, ED doctors, inpatient doctors and nurses were more likely to admit a patient rather than discharge if these factors were present (Pope et al., Citation2017). Hospital-related factors (location, availability of services and/or staff) explained the variation in care pathways for patients attending EDs in suicidal crisis (Arensman et al., Citation2018; Griffin et al., Citation2020). Arensman et al. (Citation2018) reported regional variation in recommended next care; for example, general admission ranged from 11.2% in Dublin North East Hospital compared to 61.0% in the South Eastern Hospital Group. Admission to a psychiatric ward was also lowest in North Eastern Hospital Group (3.7%) and highest in the South Hospital Group (19.3%).
Staff
Some ED staff held negative attitudes toward patients in suicidal crisis. One study reported 63.2% of staff had “somewhat negative” feelings toward self-harm (Egan, Sarma & O'Neill, Citation2012). Another study, however, indicated overall positive attitudes as evidenced by high levels of disagreement with several negatively worded questionnaire items, i.e., “individuals who attempted suicide in prominent places were primarily interested in seeking attention” (McCann, Clark, McConnachie, & Harvey, Citation2007). The culture of the ED was acknowledged in one study (Pope et al., Citation2017). Many participants felt that departmental culture (staff attitudes, motivation and relationships) had significant influences on admission practices for individuals in suicidal crisis.
Further, confidence and knowledge were reported to impact decision-making (Egan et al., Citation2012; Betz et al., Citation2013). One study stated staff felt more confidence screening suicide than creating safety plans (Betz et al., Citation2013). Egan et al. (Citation2012) reported 82% of staff had a good knowledge of self-harm and 74% expressed that they felt “somewhat confident” managing self-harm. One study, however, reported most nurses had no educational preparation or training to support patients with self-harm and over 20% of EDs had either no practice guidelines or staff did not know of their existence (McCann et al., Citation2007).
Clinical Pathways
Variation in clinical pathways were reported within and between EDs. The most commonly noted pathway was psychiatric inpatient unit admission, which was reported in 11 studies (Arensman et al., Citation2018; Baca-García et al., Citation2004; Drew, Jones, Meldon, & Varley, Citation2006; Griffin et al., Citation2020; Jimenez-Trevino et al. Citation2015; Faris et al., Citation2019; Hepp et al. Citation2004; Kroll et al., Citation2018; Schmutte et al., Citation2019a, Citation2019b; Schmutte et al., Citation2020). The majority of ED presentations in Schmutte et al. (Citation2019b) study resulted in hospital admission (81.9%), with most being admitted to an inpatient psychiatric unit (62.8%). Large variation was also reported by Griffin et al. (Citation2020). Their findings showed self-harm presentations resulting in self-discharge ranged from 4.7 to 17.8%; medical admission 8.2–53.0% and psychiatric admission 0.3 and 28.3%. Follow-up care was reported in Schmutte et al. (Citation2019a) who reported 39.0% of community discharged patient received 30-day follow-up outpatient mental health care. Similarly, those who attended EDs following suicide attempts or suicidal ideation were more likely to receive follow-up mental health support compared to those attending for self-harm (Schmutte et al., Citation2020).
DISCUSSION
The aim of this review was to examine factors that influence ED decision-making for patients presenting in suicidal crisis, following self-harm and/or a suicide attempt. Three groups of factors were identified: patient, contextual and staff.
Patient factors were most commonly reported to affect care pathways (Arensman et al., Citation2018; Faris et al., Citation2019; Griffin et al., Citation2020; Hepp et al., Citation2004; Kroll et al., Citation2018; Schmutte et al., Citation2019a, Citation2019b, Citation2020). Notably, older age was associated with hospitalization, whereas younger age groups were more likely to self-discharge (Griffin et al., Citation2020). Self-harm methods associated with greater lethality (e.g., attempted hanging or drowning) were associated with hospitalization (Baca-García et al., Citation2004; Griffin et al., Citation2020; Schmutte et al., Citation2019b). Inconsistent findings were reported in relation to gender (e.g., Faris et al., Citation2019; Griffin et al., Citation2020). Staff attitudes, knowledge and confidence were also shown to influence decision-making within EDs (Egan et al., Citation2012; McCann et al., Citation2007; Pope et al., Citation2017). Staff felt more confident at earlier stages of the clinical pathway, i.e., screening risk compared to creating safety plans (Betz et al., Citation2013). Contextual factors, including service and staff availability, were examined much less, yet were still reported to affect decision-making (i.e., Griffin et al., Citation2020; Pope et al., Citation2017). Hospital facilities (i.e., onsite psychiatric in-patient facilities) increased the likelihood of patients being admitted to psychiatric wards compared to hospitals where these facilities were located offsite (Griffin et al., Citation2020).
Prominent across the existing literature is the finding that patient-related factors (e.g., severity of psychiatric symptoms, suicide risk) significantly affects care pathways (So et al., Citation2021; Unick et al., Citation2011). This systematic review reported similar findings. Importantly, age, gender and self-harm method were reported in many of the included studies. Contextual factors (i.e., service and staff availability), however, have been reported less frequently in the literature. Despite the low number of studies, contextual factors were still shown to influence decision-making for patients presenting with self-harm. In contrast, George, Durbin, Sheldon, and Goering (Citation2002) reported site and bed availability were not associated with decision-making. Their study, however, was conducted across two emergency psychiatric services; thus, it is possible that the differences in presentations to EDs and psychiatric services explain the divergent effects.
A study conducted by Zun (Citation2012) reported that EDs may not be the most effective setting to support individuals in suicidal crisis. Rutto, Chepchirchir, and Odero (Citation2012) reported one third of nurses felt uncomfortable and nervous when attending to patients who had attempted suicide and more than half expressed frustration. This is consistent with the present review as confidence and attitudes toward self-harm were identified to influence care pathways. Contradictory findings, however, were reported; McCann et al. (Citation2007) indicated positive attitudes across ED nurses, whereas Egan et al. (Citation2012) noted negative feelings toward self-harm across ED nurses and doctors. Inconsistent findings could be a result of the difficulty in examining and measuring attitudes toward self-harm, particularly among medical staff (Egan et al., Citation2012; Patterson, Whittington, & Bogg, Citation2007).
Strengths and Limitations
This is the first systematic review to examine ED decision-making for patients in suicidal crisis. The review methodology was consistent with established standards (PRISMA guidelines) for study selection, data extraction and quality assessment.
The primary limitation of this systematic review relates to the small number of included studies; although, this is reflective of the lack of research into this patient group within an ED setting. It is notable that few studies have investigated contextual (service/staff availability) and staff-related factors in EDs. Studies were also only included if they were published in the English language, or where an English translation was available. This may explain the paucity of non-Western countries explored. Cultural variation in clinician attitudes toward self-harm may also be relevant (e.g., Ramon & Breyter, Citation1978). Furthermore, study data was extracted by the primary author, thus, limiting the validity and reliability of findings. The validity and reliability of reported findings would have been increased if more than one person extracted data from the included studies (Xu et al., Citation2022). Finally, the majority of included studies utilized hospital data sets as the primary means of data collection. This may limit current findings due to the underestimation of suicidal presentations to EDs. Research has reported self-harm presentations may be underrepresented by as much as 60% (Clements et al., Citation2016). Lack of coding for suicidal ideation may result in some presentations being missed, limiting the ability to draw accurate conclusions. Better coding practices and reporting of suicidal crisis among EDs would enable more accurate exploration into clinical pathways.
Implications for Clinical Practice
This review highlights the lack of research into the factors that influence ED decision-making. Particularly evident was the lack of studies examining contextual factors. The COVID-19 pandemic has exacerbated staffing pressures, with an increase in ED wait time and staff burnout due to the pandemic (Gemine et al., Citation2021; Mahase, Citation2022). Poor service availability can have detrimental effects on patient distress and delays in treatment can increase the number of patients needing emergency care. Future research is needed to further explore the impact of contextual factors on ED decision-making for patients in suicidal crisis.
This review also identifies an urgent need for mandatory and ongoing training for ED staff to improve knowledge and confidence in managing suicide-related presentations. Clinicians being cautious in their decision-making may be due to staff feeling unsupported and fearful of future adverse outcomes; the attribution of fault and personal consequences can lead staff to be risk adverse (Nathan et al., Citation2021). Related to this is the possibility that staff do not have a framework by which to understand suicidal thoughts. Empirical studies can help staff better understand suicidal thoughts that in turn can lead to better approaches toward such patients. Evidence suggests that there is no gold standard for assessing and managing suicidal crisis (Harmer et al. Citation2021; Bernert, Hom, & Roberts, Citation2014). Future research would therefore benefit from developing, testing and implementing a measurement to examine ED training and confidence specifically for people attending in suicidal crisis. Integrating research and practice will be beneficial to support patients in suicidal crisis.
A patient’s experience and journey through the ED can be affected by staff attitudes. Negative attitudes can be conveyed through the way clinicians interact with patients, i.e., invalidating comments, which may be subtle or overt. The assessment approach can also impact patient outcomes (e.g., reduce feelings of hopelessness and in turn suicidal thoughts/behaviors) (Kapur et al., Citation2013). Equally, some clinicians adopt counter-therapeutic stances which may increase the likelihood of suicidal thoughts (Dunster-Page, Haddock, Wainwright, & Berry, Citation2017). Staff attitudes are therefore crucial to future help-seeking behavior. Patients attending EDs in suicidal crisis also encounter a wide range of staff including receptionists, triage nurses and liaison psychiatrists. Prior research, however, mainly recruits nurses to explore attitudes toward self-harm. There is a need for a specific tool to measure a wide range of ED staff attitudes for treating and managing patients in suicidal crisis.
This review highlights substantial variation in the decision-making and subsequent care pathways for patients attending EDs in suicidal crisis. For EDs to assess, treat and support patients in suicidal crisis more effectively a better understanding of why there are differences between and within EDs is needed. This review is an initial step in exploring variation; however, there are still gaps in the current evidence base to be explored further. More research is needed on staff-based factors (i.e., clinicians’ conceptualizations of self-harm and uncertainty management) and contextual factors (e.g., the pressure to both manage limited resources whilst not “missing” someone who goes on to seriously harm themselves). Finally, it will be important to explore the impact of different decision-influencing factors identified in this review on patient outcomes.
Supplemental Material
Download MS Word (13.4 KB)Additional information
Notes on contributors
Molly McCarthy
Molly McCarthy and Jason McIntyre, Liverpool John Moores University, Liverpool, United Kingdom of Great Britain and Northern Ireland.
Jason McIntyre
Molly McCarthy and Jason McIntyre, Liverpool John Moores University, Liverpool, United Kingdom of Great Britain and Northern Ireland.
Rajan Nathan
Rajan Nathan, Cheshire and Wirral Partnership NHS Foundation Trust, Chester, United Kingdom of Great Britain and Northern Ireland.
Pooja Saini
Pooja Saini, Liverpool John Moores University, Liverpool, United Kingdom of Great Britain and Northern Ireland.
REFERENCES
- Arensman, E., Griffin, E., Daly, C., Corcoran, P., Cassidy, E., & Perry, I. J. (2018). Recommended next care following hospital-treated self-harm: Patterns and trends over time. PLOS one, 13(3), e0193587.
- Baca-García, E., Diaz-Sastre, C., Resa, E. G., Blasco, H., Conesa, D. B., Saiz-Ruiz, J., & De Leon, J. (2004). Variables associated with hospitalization decisions by emergency psychiatrists after a patient’s suicide attempt. Psychiatric services, 55(7), 792–797.
- Bernert, R. A., Hom, M. A., & Roberts, L. W. (2014). A review of multidisciplinary clinical practice guidelines in suicide prevention: Toward an emerging standard in suicide risk assessment and management, training and practice. Academic Psychiatry, 38(5), 585–592. doi:10.1007/s40596-014-0180-1
- Betz, M. E., Sullivan, A. F., Manton, A. P., Espinola, J. A., Miller, I., Camargo, C. A., … Jr, ED-SAFE Investigators. (2013). Knowledge, attitudes, and practices of emergency department providers in the care of suicidal patients. Depression and Anxiety, 30(10), 1005–1012.
- Carr, M. J., Ashcroft, D. M., Kontopantelis, E., Awenat, Y., Cooper, J., Chew-Graham, C., … Webb, R. T. (2016). The epidemiology of self-harm in a UK-wide primary care patient cohort, 2001–2013. BMC psychiatry, 16(1), 1–10.
- Ceniti, A. K., Heinecke, N., & McInerney, S. J. (2020). Examining suicide-related presentations to the emergency department. General hospital Psychiatry, 63, 152–157.
- Clements, C., Turnbull, P., Hawton, K., Geulayov, G., Waters, K., Ness, J., … Kapur, N. (2016). Rates of self-harm presenting to general hospitals: A comparison of data from the multicentre study of self-harm in England and hospital episode statistics. BMJ open, 6(2), e009749. doi:10.1136/bmjopen-2015-009749
- Drew, B. L., Jones, S. L., Meldon, S. W., & Varley, J. D. (2006). Emergency department visits for suicidality in three hospitals. Archives of Psychiatric Nursing, 20(3), 117–125. doi:10.1016/j.apnu.2005.11.001
- Dunster-Page, C., Haddock, G., Wainwright, L., & Berry, K. (2017). The relationship between therapeutic alliance and patient’s suicidal thoughts, self-harming behaviours and suicide attempts: A systematic review. Journal of Affective Disorders, 223, 165–174.
- Egan, R., Sarma, K. M., & O'Neill, M. (2012). Factors influencing perceived effectiveness in dealing with self-harming patients in a sample of emergency department staff. The journal of Emergency Medicine, 43(6), 1084–1090.
- Faris, N., Baroud, E., Al Hariri, M., Bachir, R., El-Khoury, J., & Batley, N. J. (2019). Characteristics and dispositional determinants of psychiatric emergencies in a University Hospital in Beirut. Asian journal of Psychiatry, 42, 42–47.
- Gemine, R., Davies, G. R., Tarrant, S., Davies, R. M., James, M., & Lewis, K. (2021). Factors associated with work-related burnout in NHS staff during COVID-19: A cross-sectional mixed methods study. BMJ open, 11(1), e042591.
- George, L., Durbin, J., Sheldon, T., & Goering, P. (2002). Patient and contextual factors related to the decision to hospitalize patients from emergency psychiatric services. Psychiatric Services, 53(12), 1586–1591.
- Griffin, E., Gunnell, D., & Corcoran, P. (2020). Factors explaining variation in recommended care pathways following hospital-presenting self-harm: A multilevel national registry study. BJPsych open, 6(6), 1–8.
- Harmer, B., Lee, S., Duong, T., & Saadabadi, A. (2021). Suicidal ideation. Treasure Island, FL: StatPearls Publishing.
- Hawton, K., Bergen, H., Casey, D., Simkin, S., Palmer, B., Cooper, J., … Owens, D. (2007). Self-harm in England: A tale of three cities. Social psychiatry and Psychiatric Epidemiology, 42(7), 513–521.
- Hepp, U., Moergeli, H., Trier, S. N., Milos, G., & Schnyder, U. (2004). Attempted suicide: Factors leading to hospitalization. The Canadian Journal of Psychiatry, 49(11), 736–742.
- Jimenez-Trevino, L., Saiz, P. A., Corcoran, P., Burón, P., García-Portilla, M. P., Chinea, E. R., … Bobes, J. (2015). Factors associated with hospitalization after suicide spectrum behaviors: Results from a multicenter study in Spain. Archives of Suicide Research, 19(1), 17–34.
- Kapur, N., Steeg, S., Webb, R., Haigh, M., Bergen, H., Hawton, K., … Cooper, J. (2013). Does clinical management improve outcomes following self-harm? Results from the multicentre study of self-harm in England. PLOS one, 8(8), e70434. doi:10.1371/journal.pone.0070434
- Kienhorst, I. C. (1995). Crisis intervention and a suicidal crisis in adolescents. Crisis, 16(4), 154–156.
- Knorr, A. C., Ammerman, B. A., LaFleur, S. A., Misra, D., Dhruv, M. A., Karunakaran, B., & Strony, R. J. (2020). An investigation of clinical decisionmaking: Identifying important factors in treatment planning for suicidal patients in the emergency department. Journal of the American College of Emergency Physicians Open, 1(4), 383–391. doi:10.1002/emp2.12087
- Kroll, D. S., Karno, J., Mullen, B., Shah, S. B., Pallin, D. J., & Gitlin, D. F. (2018). Clinical severity alone does not determine disposition decisions for patients in the emergency department with suicide risk. Psychosomatics, 59(4), 388–393.
- Mahase, E. (2022). Covid-19: Shorten isolation periods to relieve NHS pressures, say leaders. BMJ, 376, o38. doi:10.1136/bmj.o38
- McCann, T. V., Clark, E., McConnachie, S., & Harvey, I. (2007). Deliberate self‐harm: Emergency department nurses’ attitudes, triage and care intentions. Journal of Clinical Nursing, 16(9), 1704–1711. doi:10.1111/j.1365-2702.2006.01555.x
- McCarthy, M., Saini, P., Nathan, R., & McIntyre, J. (2021). Improve coding practices for patients in suicidal crisis. BMJ : British Medical Journal (Online), 375. doi:10.1136/bmj.n2480
- McManus, S., Gunnell, D., Cooper, C., Bebbington, P. E., Howard, L. M., Brugha, T., … Appleby, L. (2019). Prevalence of non-suicidal self-harm and service contact in England, 2000–14: Repeated cross-sectional surveys of the general population. The Lancet-Psychiatry, 6(7), 573–581.
- Miller, I. W., Camargo, C. A., Arias, S. A., Sullivan, A. F., Allen, M. H., Goldstein, A. B., … Ed, S. I. (2017). Suicide prevention in an emergency department population: The ED-SAFE study. JAMA psychiatry, 74(6), 563–570.
- Miret, M., Nuevo, R., Morant, C., Sainz-Cortón, E., Jiménez-Arriero, M. Á., López-Ibor, J. J., … Ayuso-Mateos, J. L. (2011). The role of suicide risk in the decision for psychiatric hospitalization after a suicide attempt. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 32(2), 65–73.
- Morgan, C., Webb, R. T., Carr, M. J., Kontopantelis, E., Chew-Graham, C. A., Kapur, N., & Ashcroft, D. M. (2018). Self-harm in a primary care cohort of older people: Incidence, clinical management, and risk of suicide and other causes of death. The Lancet Psychiatry, 5(11), 905–912.
- Naghavi, M. (2019). Global, regional, and national burden of suicide mortality 1990 to 2016: Systematic analysis for the Global Burden of Disease Study 2016. British Medical Journal, 364. doi:10.1136/bmj.l94
- Nathan, R., Gabbay, M., Boyle, S., Elliott, P., Giebel, C., O'loughlin, C., … Saini, P. (2021). Use of acute psychiatric hospitalisation: A study of the factors influencing decisions to arrange acute admission to inpatient mental health facilities. Frontiers in Psychiatry, 12, 891.
- National Institute for Health and Care Excellence (NICE). (2004). Self-harm in over 8s: Short-term management and prevention of recurrence. Retrieved from https://www.nice.org.uk/guidance/cg16/resources/selfharm-in-over-8s-shortterm-management-and-prevention-of-. recurrence-pdf-975268985029.
- Office of National Statistics. (2021). Suicides in England and Wales: 2020 registrations. Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/suicidesintheunitedkingdom/2020registrations.
- Owens, C., Hansford, L., Sharkey, S., & Ford, T. (2016). Needs and fears of young people presenting at accident and emergency department following an act of self-harm: Secondary analysis of qualitative data. The British Journal of Psychiatry, 208(3), 286–291. doi:10.1192/bjp.bp.113.141242
- Pace, R., Pluye, P., Bartlett, G., Macaulay, A. C., Salsberg, J., Jagosh, J., & Seller, R. (2012). Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. International journal of Nursing Studies, 49(1), 47–53.
- Patterson, P., Whittington, R., & Bogg, J. (2007). Measuring nurse attitudes towards deliberate self‐harm: The Self‐Harm Antipathy Scale (SHAS). Journal of Psychiatric and Mental Health Nursing, 14(5), 438–445.
- Perera, J., Wand, T., Bein, K. J., Chalkley, D., Ivers, R., Steinbeck, K. S., … Dinh, M. M. (2018). Presentations to NSW emergency departments with self‐harm, suicidal ideation, or intentional poisoning, 2010–2014. The Medical Journal of Australia, 208(8), 348–353. doi:10.5694/mja17.00589
- Phillips, G., Gerdtz, M. F., Elsom, S. J., Weiland, T. J., & Castle, D. (2015). Mental health nurses’ dispositional decision‐making for people presenting to the emergency department with deliberate self‐harm: An exploratory study. Perspectives in Psychiatric Care, 51(2), 148–153.
- Pluye, P., Gagnon, M. P., Griffiths, F., & Johnson-Lafleur, J. (2009). A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. International journal of Nursing Studies, 46(4), 529–546. doi:10.1016/j.ijnurstu.2009.01.009
- Polling, C., Bakolis, I., Hotopf, M., & Hatch, S. L. (2019). Differences in hospital admissions practices following self-harm and their influence on population-level comparisons of self-harm rates in South London: An observational study. BMJ open, 9(10), e032906.
- Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., … Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. Prod ESRC Methods Programme Version. 2006;1:b92.
- Pope, I., Burn, H., Ismail, S. A., Harris, T., & McCoy, D. (2017). A qualitative study exploring the factors influencing admission to hospital from the emergency department. BMJ open, 7(8), e011543. doi:10.1136/bmjopen-2016-011543
- Ramon, S., & Breyter, C. E. (1978). Attitudes towards self-poisoning among British and Israeli doctors and nurses in a psychiatric hospital. Israel Annals of Psychiatry & Related Disciplines, 16(3), 206–218.
- Rutto, J., Chepchirchir, A., & Odero, T. (2012). Nurse’s knowledge, attitude and practice on the initial management of acute poisoning among adult casualties: Study at Kenyatta National Hospital, Kenya. [Masters Dissertation, The University of Nairobi]. eRepository. http://erepository.uonbi.ac.ke/handle/11295/10654
- Saunders, K. E., Hawton, K., Fortune, S., & Farrell, S. (2012). Attitudes and knowledge of clinical staff regarding people who self-harm: A systematic review. Journal of Affective Disorders, 139(3), 205–216. doi:10.1016/j.jad.2011.08.024
- Schmutte, T., Olfson, M., Xie, M., & Marcus, S. C. (2019a). Deliberate self‐harm in older adults: A national analysis of US emergency department visits and follow‐up care. International journal of Geriatric Psychiatry, 34(7), 1058–1069.
- Schmutte, T., Olfson, M., Xie, M., & Marcus, S. C. (2019b). National study of emergency department disposition for high suicide risk geriatric patients. General hospital Psychiatry, 58, 67–70.
- Schmutte, T., Olfson, M., Xie, M., & Marcus, S. C. (2020). Self-harm, suicidal ideation, and attempted suicide in older adults: A national study of emergency department visits and follow-up care. The American Journal of Geriatric Psychiatry, 28(6), 646–658. doi:10.1016/j.jagp.2019.12.003
- Siry, B. J., Polzer, E., Omeragic, F., Knoepke, C. E., Matlock, D. D., & Betz, M. E. (2021). Lethal means counseling for suicide prevention: Views of emergency department clinicians. General hospital Psychiatry, 71, 95–101. doi:10.1016/j.genhosppsych.2021.04.011
- So, P., Wierdsma, A. I., Kasius, M. C., Cornelis, J., Lommerse, M., Vermeiren, R. R., & Mulder, C. L. (2021). Predictors of voluntary and compulsory admissions after psychiatric emergency consultation in youth. European child & Adolescent Psychiatry, 30(5), 747–756. doi:10.1007/s00787-020-01558-9
- Stapelberg, N. J., Sveticic, J., Hughes, I., & Turner, K. (2020). Suicidal presentations to emergency departments in a large Australian public health service over 10 years. International journal of Environmental Research and Public Health, 17(16), 5920.
- Unick, G. J., Kessell, E., Woodard, E. K., Leary, M., Dilley, J. W., & Shumway, M. (2011). Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. General hospital Psychiatry, 33(6), 618–625. doi:10.1016/j.genhosppsych.2011.06.004
- Vigo, D. V., Kestel, D., Pendakur, K., Thornicroft, G., & Atun, R. (2019). Disease burden and government spending on mental, neurological, and substance use disorders, and self-harm: Cross-sectional, ecological study of health system response in the Americas. The Lancet-Public Health, 4(2), e89–e96. doi:10.1016/S2468-2667(18)30203-2
- World Health Organisation [WHO]. (2019). Suicide in the world: Global health estimates. World Health Organisation. Retrieved from https://apps.who.int/iris/handle/10665/326948.
- Xu, C., Yu, T., Furuya-Kanamori, L., Lin, L., Zorzela, L., Zhou, X., … Vohra, S. (2022). Validity of data extraction in evidence synthesis practice of adverse events: Reproducibility study. BMJ , 377, e069155. doi:10.1136/bmj-2021-069155
- Zun, L. S. (2012). Pitfalls in the care of the psychiatric patient in the emergency department. The Journal of Emergency Medicine, 43(5), 829–835. doi:10.1016/j.jemermed.2012.01.064
