Abstract
Background: In patients with an acute lower respiratory tract infection (LRTI), general practitioners (GPs) often find it challenging to decide to prescribe antibiotics or not. C-reactive protein (CRP) point of care test (POCT), and chest X-ray are diagnostic tests that can optimize the treatment decision. However, their usefulness in clinical practice is unknown.
Objectives: To determine the proportion of Dutch GPs using CRP and chest X-ray in patients with an acute LRTI. To determine whether clinical factors and C-reactive protein point of care test affect the behaviour in requesting chest X-rays.
Methods: In 2014, a questionnaire was sent to a random sample of 900 Dutch GPs. Outcome parameters are the use of CRP and chest X-ray, the percentage of GPs who guide their decision in requesting chest X-rays by CRP testing and the GP’s expectation regarding presence or absence of pneumonia. In addition, considerations for requesting chest X-rays were assessed.
Results: Two hundred and fifty-five completed questionnaires (29%) were returned. In 2014, 54% of the responding GPs used the CRP test. These GPs tend to use fewer chest X-rays (p = 0.07). GPs overestimate the chance that pneumonia will be present on the radiograph. Seventy percent consider the possibility of abnormalities other than pneumonia as the main reason for requesting a chest X-ray.
Conclusion: In patients with an acute lower respiratory tract infection, GPs report that CRP results affect their behaviour regarding the request of a chest X-ray in patients with lower respiratory tract infection and therefore research is needed to substantiate the use of these diagnostic tools for this purpose.
Introduction
KEY MESSAGES
A vast majority of GPs use the CRP test and most of them requested a chest X-ray on CRP result.
GPs that use CRP test reported to request fewer chest X-rays in patients with an acute lower respiratory tract infection.
GPs overestimate the chance of finding pneumonia on chest X-rays.
Two types of additional (diagnostic) tests for acute LRTI can be used in general practice: the C-reactive protein point of care test (CRP POCT) and the chest X-ray. A low CRP (<20 mg/l) can exclude pneumonia with reasonable certainty, irrespective of clinical findings while an elevated CRP (>100 mg/l) greatly increases the chance of pneumonia warranting antibiotic treatment [Citation8,Citation10]. A recent meta-analysis ascertained that even when clinical variables are taken into account, the CRP test can help to confirm or exclude pneumonia [Citation11]. Different guidelines (e.g. the British and the Dutch guidelines) therefore, indicated the use of the CRP test in moderately ill patients [Citation1,Citation12]. Studies that evaluated whether the CRP POCT reduced the number of antibiotic prescriptions showed variable results [Citation13,Citation14].
A chest X-ray can be used to detect pneumonia but the use of this examination in all individuals in whom pneumonia is suspected is not recommended. The chest X-ray is currently only recommended in the Dutch guideline to investigate, the cause of lack of recovery, uncertainty about the diagnosis or treatment, or when a condition other than pneumonia is suspected as an explanation for the symptoms [Citation1]. The British guideline does not mention the chest X-ray as a diagnostic tool in patients with suspected pneumonia or exacerbations of asthma and COPD. Every year, GPs request about 31 chest radiographs per 1000 person-years [Citation15]. Research into the effectiveness of requesting chest X-rays by the GP for certain subgroups of patients with an acute LRTI is lacking. The objective of this study was to assess the use of chest X-ray and the CRP POCT in patients with an acute respiratory tract infection in Dutch primary care. We asked the GPs about their estimates and experiences with this complex situation where evidence for a specific strategy is lacking.
Methods
Study design and setting
Between May and September 2014, a questionnaire-based cross-sectional study was performed in the Netherlands. The registry from the Netherlands Institute for Healthcare Research (NIVEL) contains address information of all GPs in the Netherlands. A random sample of 900 addresses was drawn. The questionnaire (Supplementary Appendix) was sent in May 2014 per mail to these family practice addresses.
Construction of the questionnaire
The two principal investigators (GHG and RJP) held an exploratory focus group discussion with various GPs in the Leiden region, the Netherlands. In this discussion, open questions were asked about the way in which the GPs use additional diagnostic tests in patients with acute LRTI and in what way the results of the tests affect their treatment policy [Citation16]. An acute LRTI was defined as complaints for less than three weeks.
Based on the results, a list with open and closed questions was generated and distributed among 15 GPs in the Leiden region via the newsletter of the Leiden Primary Care Research Network. The answers and feedback received via this route contributed to the final quantitative questionnaire.
Quantitative questionnaire
First, the questionnaire asks about the number of years of work experience, the number of hours a week that the GP works at the general practice, and an estimate of the number of chest X-rays requested in a year for patients with acute LRTI.
Main outcomes are the use of CRP POCT, the percentage of GPs who guide their decision in requesting chest X-rays by CRP testing and the expectation regarding presence of pneumonia on chest X-rays. In addition, indications for the use of CRP POCT, clinical parameters and distribution of reasons for requesting chest X-rays (in GPs with and without CRP test available), which other pathology the GP wants to exclude and diagnostic and therapeutic consequences when pneumonia is present or absent were assessed.
Various characteristics and consequences could be scored on five-point Likert scales, with answers varying from ‘(almost) never’/‘very unimportant’ to ‘(almost) always’/‘very important.’ The complete questionnaire is available in the Supplementary Appendix.
Analysis
The returned questionnaires were anonymized. Descriptive analyses and comparison of proportion with chi-squared test were performed with SPSS (IBM SPSS Statistics for Windows, Version 23.0., Armonk, NY).
Results
Study population
Twenty-three questionnaires were returned due to outdated address details. In total, after one reminder letter, 255 of the 877 (29%) questionnaires were returned completed in September 2014. The respondents reported a median work experience of 14 years, (interquartile range, IQR, 9–22 years) and a median workweek of 36 h (IQR: 30–41.5 h) at the general practice.
Chest X-ray
Median reported the number of chest X-rays per year for patients with an acute LRTI was 10 (IQR: 4–12). The 24 respondents (9%) that never requested a chest X-ray for this indication could not answer the remaining questions. Median work experience and work week in the respondents who never request a chest X-ray did not differ from respondents who did request chest X-rays.
and provide an overview of the reports of GPs regarding considerations and objectives to request a chest X-ray. Most GPs (70%) consider the detection or exclusion of abnormalities other than pneumonia as one of the main reasons for requesting a chest X-ray. The exclusion of malignancy, heart failure, sarcoidosis, and tuberculosis are mentioned repeatedly. If the chest X-ray has been required to exclude other pathology, the GP will state this in 90% of the cases on the X-ray application form. Factors that play an essential role in the decision to request a chest X-ray are mainly age, smoking, and the duration of the complaints.
Table 1. Questionnaire response from general practitioners: Clinical factors in the consideration to request a chest X-ray in patients with an acute lower respiratory tract infection (n = 226Table Footnotea).
Table 2. Questionnaire response from general practitioners: Reasons to request a chest X-ray in patients with an acute lower respiratory tract infection (n = 228Table Footnotea).
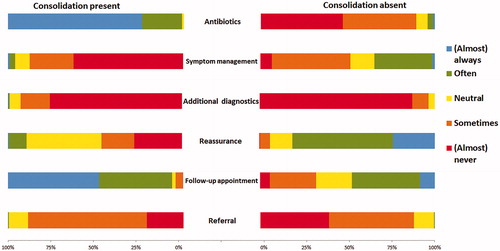
The assumption of 217 GPs (14 GPs did not answer this question and 24 never requested a chest X-ray) to detect a lung infiltrate on the chest X-ray was less than 10% in 13% of GPs, between 10 and 20% in 19% of GPs, and more than 50% in 68% of GPs. If an infiltrate suspect for pneumonia is present, 227 of the 230 GPs (99%; 1 GP did not answer this question and 24 GPs never request a chest X-ray) often, to almost always, prescribe an antibiotic. In the absence of pneumonia, 4% of GPs often, to nearly always, prescribe an antibiotic ().
Figure 1. Questionnaire response from general practitioners: Policy following the chest X-ray in patients with an acute lower respiratory tract infection (n = 230a). Bi-directional bar chart. On the left the policy followed in case a pneumonia was detected on the chest X-ray, on the right the policy followed in case no pneumonia was detected on the chest X-ray. In the middle, description of the policy. a24 respondents never request a chest X-ray and one did not answer this question.
CRP point of care test
The CRP POCT is used by the vast majority of GPs (54%). Most GPs also use the test to evaluate suspected infections other than pneumonia (), e.g. diverticulitis, urinary tract infection, or an unknown ‘other’ infection. GPs (80%) reported that they foresee that CRP POCT can replace chest X-ray as a diagnostic test partially or completely. GPs with CRP test available are more confident than those that do not have this test available (86% vs 71%, p <0.01).
Table 3. Questionnaire response from general practitioners: Use and indications for use of the CRP point of care test (n = 246Table Footnotea).
Difference between GPs with and without CRP test
GPs with CRP POCT available reported requesting fewer chest X-rays than their colleagues without CRP POCT available (median 6, IQR: 3–10 vs median 10, IQR: 5–14, respectively; p = 0.07).
Expectation regarding the presence of pneumonia did not differ between GPs with or without CRP POCT available (p = 0.67).
Presence and colour of sputum were reported to be more critical when considering chest X-ray by GPs without, than those with, CRP POCT available (Figure S1).
Guidance whether or not to prescribe antibiotics is reported as a reason for requesting chest X-ray less frequently in GPs with CRP than in GPs without CRP. Other reasons were not different (Figure S2).
GPs who do not use CRP POCT reported more frequently than those who do use CRP POCT starting symptom management in case pneumonia is confirmed (neutral to almost always 15% vs 9%; p = 0.05) or ruled out with chest X-ray (neutral to almost always 57% vs 41%; p <0.01). The remaining policy items did not differ significantly between GP groups.
Discussion
Main findings
This study shows that in 255 Dutch GPs, the use of additional diagnostic tools for the suspicion of acute LRTI was diverse. GPs reported estimating the probability of having pneumonia as high among patients for whom they request a chest X-ray. Nearly 70% of GPs request the photo mainly to exclude other pathology. The vast majority of GPs had the CRP POCT available in 2014 and most GPs used this test to determine whether or not to request a chest X-ray. GPs using CRP POCTs reported requesting fewer chest X-rays than GPs who did not use this test. These latter GPs reported using chest X-ray more often to guide the decision to prescribe antibiotics. Many GPs also used the CRP POCT for other purposes.
Strengths and limitations
The strengths of this study are the random sample of GPs in the Netherlands and the considerable number of 255 completed surveys that were available for analysis. The inventory based on focus group interview and pilot questionnaires during the pilot study means that the diversity of ideas, experiences, and behaviours in the target group were well explored. The fact that both GPs with and without a CRP POCT, as well as GPs that vary from never to frequently requesting chest X-rays have responded, means that the sample has included all extremes of diagnostic policy.
A limitation of the study is the potential occurrence of sampling bias. The ‘selection’ of respondents could be different from that of the GPs who did not respond. Although the absolute number of questionnaires analysed is considerable, the response rate of 29% is not high. A review by Creavin et al. showed a mean response rate of 61% [Citation17]. However, the response rate in recent surveys among Dutch GPs is substantially lower [Citation17–19]. Respondents could be more interested in this topic than non-responders and thereby more aware of guidelines and evidence, resulting in more prudent use of diagnostic tools. The years of work experience and the number of working hours of the respondents correspond to the national average, 14.9 years and 31.2 h per week, respectively [Citation20]. Moreover, McFarlane et al. demonstrated that higher response rates in a survey of physicians are not associated with lower selection bias [Citation21].
Nonetheless, the potential difference in characteristics between GPs who filled in the questionnaire and the ones that did not respond might still be present. However, the study provides a useful insight into the considerations of the Dutch GP about additional diagnostic tools for acute LRTIs.
Not every possible consideration has been asked in this short questionnaire. For example, it is not clear in what type of patient the CRP POCT is used, if CRP kinetics are taken into consideration, and how GPs interpret the results. A previous study showed that most GPs use the CRP POCT in patients who are moderately ill when it is not immediately obvious whether or not the patient needs an antibiotic. In the same study, it was found that the CRP POCT is sometimes used too frequently, even in situations where this test should have no consequences for the policy [Citation22].
This is a survey-based study about opinions and perceptions, which do not necessarily reflect the real management and prescription habits. The survey was completed in 2014. It is possible that with an increase in use, the interpretation of the results will also change slightly.
Interpretation
GPs’ expectation about the likelihood of detecting a lung infiltrate on the X-ray is high. Two-thirds expect an infiltrate in more than 20% of the patients. This estimate does not match the findings in several primary care studies, where pneumonia on the chest X-ray was detected in only 5–13% [Citation8,Citation11,Citation23].
The chest X-ray is the gold standard for the detection or exclusion of pneumonia, while clinical features, including a low CRP value, can safely exclude pneumonia [Citation11,Citation12]. The benefit of chest X-rays in the detection or exclusion of pneumonia is, therefore, primarily present in the group of patients with a high probability of the presence of an infiltrate. This mainly concerns patients with clinical characteristics fitting with pneumonia that have an elevated CRP value. We hypothesize that GPs may request too many chest X-rays because they overestimate the likelihood of pneumonia. With better pretest (pre-chest X-ray) assessment, for example by using CRP, pneumonia could be ruled out more often without chest X-ray. Differently, GPs incorrectly withhold some patients from chest X-rays because they do not adequately determine the group of patients with a high pretest (pre-chest X-ray) probability, partially because only 54% in our study used the CRP test. Additionally, given the discrepancy between the pretest assessment and the actual percentage of pneumonia present on lung images, pneumonia can often be excluded with a chest X-ray. In the latter case, antibiotics are prescribed less frequently.
The lack of evidence is the reason that the chest X-ray is currently not clearly defined in the standard of the Dutch Society of GPs or the British guidelines for the detection or exclusion of pneumonia [Citation1,Citation12]. However, this study shows that GPs already use the results of the CRP test in their decision to request a chest X-ray and/or they foresee that the CRP test can replace the chest X-ray as a diagnostic tool.
Often the detection or exclusion of a condition other than pneumonia is indicated as the main reason to request a chest X-ray. In a European cohort of nearly 3000 patients with an acute cough who underwent a chest X-ray, a clinically relevant abnormality—other than pneumonia—was found in 3% [Citation24]. Therefore, the chance that a GP will find such aberrations is small. Malignancy can be missed on the chest X-ray, especially if at that time an infiltrate is present in the same area. It is then preferable to repeat the chest X-ray after pneumonia has been treated [Citation25].
Accurate information about the availability and use of CRP POCT in European countries is not known. Oppong et al. reported that CRP POCT was available in 12 of 14 primary care networks in 13 European countries [Citation26]. There were marked differences in the availability of CRP tests between Spain and Denmark and between CRP use in Belgium (3%) [Citation27], the UK (15%), and the Netherlands (48%) in 2012–2013 [Citation28]. The use of CRP has increased in Scandinavian countries between 2004 and 2013 [Citation29].
When comparing Danish primary care versus Spanish primary care, chest X-rays are used more frequently to confirm pneumonia in Spain [Citation27].
Implications
With the frequent use of the CRP POCT to aid in the decision to request a chest radiograph, there appears to be a need for research into a diagnostic algorithm, that would incorporate clinical characteristics and a CRP result, to determine in which patient a chest X-ray has added value.
This study also shows that GPs using the CRP POCT frequently use it for infections other than pneumonia. The use of the CRP test is only recommended for patients with acute LRTIs or diverticulitis. For both disorders, the use of the CRP test has many limitations [Citation1,Citation30]. Restraint in its use is therefore required until new research proves that either the CRP POCT has added value for other indications, or that the CRP test can replace a chest radiograph.
Conclusion
GPs widely use the CRP POCT and often base their decision to request a chest X-ray on the outcome. They overestimate the chance of finding pneumonia in these patients. Clinical variables in combination with the CRP POCT could help the GP to request chest radiographs more selectively for patients with acute LRTI. Research, however, is first needed to substantiate the use of these diagnostic tools for this purpose.
Original questionnaire
Download PDF (181.2 KB)Figure S2. Bidirectional bar chart questionnaire response from general practitioners about reasons to request a chest X ray in patients with an acute RTI
Download JPEG Image (106.8 KB)Figure S1. Considerations to request a chest X ray with or without CRP
Download PNG Image (23.6 KB)Acknowledgements
The authors thank the GPs from the Leiden region who contributed to the realization of the survey, GPs who provided feedback in the pilot study, and all GPs who completed and returned the final questionnaire.
Disclosure statement
The authors report no conflicts of interests. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Verheij TJM, Hopstaken RM, Prins JM, et al. NHG standard acute cough (First review). Huisarts Wet. 2011;54:68–92.
- Rosh AJ, Newman DH. Evidence-based emergency medicine/rational clinical examination abstract. Diagnosing pneumonia by medical history and physical examination. Ann Emerg Med. 2005;46:465–467.
- Adriaenssens N, Coenen S, Versporten A, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient antibiotic use in Europe (1997–2009). J Antimicrob Chemother. 2011;66: Suppl 6:vi3–12.
- Volksgezondheidenzorg.info. Users antibiotics per municipality [Internet]. Bilthoven: RIVM; 2013 [cited 2019 Mar 21]. Available from: https://www.volksgezondheidenzorg.info/onderwerp/genees-en-hulpmiddelen-en-lichaamsmaterialen/regionaal-internationaal/geneesmiddelen#node-gebruikers-antibiotica-gemeente.
- Little P, Stuart B, Moore M, et al. Amoxicillin for acute lower-respiratory-tract infection in primary care when pneumonia is not suspected: a 12-country, randomised, placebo-controlled trial. Lancet Infect Dis. 2013;13:123–129.
- Teepe J, Little P, Elshof N, et al. Amoxicillin for clinically unsuspected pneumonia in primary care: subgroup analysis. Eur Respir J. 2016;47:327–330.
- Zaat Jom SW, Assendelft WJJ. Knock, knock, who is there? A systematic literature review of the value of anamnesis and physical examination for suspected pneumonia. Huisarts Wet. 1998;41:461–469.
- Hopstaken RM, Muris JW, Knottnerus JA, et al. Contributions of symptoms, signs, erythrocyte sedimentation rate, and C-reactive protein to a diagnosis of pneumonia in acute lower respiratory tract infection. Br J Gen Pract. 2003;53:358–364.
- Graffelman AW, Le Cessie S, Knuistingh Neven A, et al. Can history and exam alone reliably predict pneumonia? J Fam Pract. 2007;56:465–470.
- van Vugt SF, Broekhuizen BD, Lammens C, et al. Use of serum C reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: diagnostic study. Br Med J. 2013;346:f2450.
- Minnaard MC, de Groot JA, Hopstaken RM, et al. The added value of C-reactive protein measurement in diagnosing pneumonia in primary care: a meta-analysis of individual patient data. CMAJ. 2017;189:E56–E63.
- National Institute for Health and Excellence (NICE). Pneumonia in adults: diagnosis and management; 2014 [cited 2019 May 22]. Available from: https://www.nice.org.uk/guidance/cg191/chapter/1-Recommendations
- Minnaard MC, van de Pol AC, Hopstaken RM, et al. C-reactive protein point-of-care testing and associated antibiotic prescribing. FAMPRJ. 2016;33:408–413.
- Huang Y, Chen R, Wu T, et al. Association between point-of-care CRP testing and antibiotic prescribing in respiratory tract infections: a systematic review and meta-analysis of primary care studies. Br J Gen Pract. 2013;63:e787–794.
- Speets AM, Kalmijn S, Hoes AW, et al. Frequency of chest radiography and abdominal ultrasound in the Netherlands: 1999–2003. Eur J Epidemiol. 2005;20:1031–1036.
- Moser A, Korstjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24:9–18.
- Creavin ST, Creavin AL, Mallen CD. Do GPs respond to postal questionnaire surveys? A comprehensive review of primary care literature. Fam Pract. 2011;28:461–467.
- Wammes JJ, Jeurissen PP, Verhoef LM, et al. Is the role as gatekeeper still feasible? A survey among Dutch general practitioners. Fam Pract. 2014;31:538–544.
- Sinnema H, Franx G, Spijker J, et al. Delivering stepped care for depression in general practice: results of a survey amongst general practitioners in the Netherlands. Eur J Gen Pract. 2013;19:221–229.
- Cijfers uit de registratie van huisartsen [Internet]. Utrecht: Stichting NIVEL; 2015 [cited 2019 Mar 21] Available from: https://www.nivel.nl/nl/publicatie/cijfers-uit-de-registratie-van-huisartsen-peiling-2015
- McFarlane E, Olmsted MG, Murphy J, et al. Nonresponse bias in a mail survey of physicians. Eval Health Prof. 2007;30:170–185.
- Cals JW, Chappin FH, Hopstaken RM, et al. C-reactive protein point-of-care testing for lower respiratory tract infections: a qualitative evaluation of experiences by GPs. Fam Pract. 2010;27:212–218.
- Speets AM, Hoes AW, van der Graaf Y, et al. Chest radiography and pneumonia in primary care: diagnostic yield and consequences for patient management. Eur Respir J. 2006;28:933–938.
- van Vugt S, Broekhuizen L, Zuithoff N, et al. Incidental chest radiographic findings in adult patients with acute cough. Ann Fam Med. 2012;10:510–515.
- Tang KL, Eurich DT, Minhas-Sandhu JK, et al. Incidence, correlates, and chest radiographic yield of new lung cancer diagnosis in 3398 patients with pneumonia. Arch Intern Med. 2011;171:1193–1198.
- Oppong R, Coast J, Hood K, et al. Resource use and costs of treating acute cough/lower respiratory tract infections in 13 European countries: results and challenges. Eur J Health Econ. 2011;12:319–329.
- Christensen SF, Jorgensen LC, Cordoba G, et al. Marked differences in GPs’ diagnosis of pneumonia between Denmark and Spain: a cross-sectional study. Prim Care Respir J. 2013;22:454–458.
- Howick J, Cals JW, Jones C, et al. Current and future use of point-of-care tests in primary care: an international survey in Australia, Belgium, The Netherlands, the UK and the USA. BMJ open. 2014;4:e005611
- Haldrup S, Thomsen RW, Bro F, et al. Microbiological point of care testing before antibiotic prescribing in primary care: considerable variations between practices. BMC Fam Pract. 2017;18:9.
- Berger MY, De Wit NJ, Vogelenzang R, et al. NHG-standaard diverticulitis [NHG standard diverticulitis]. Huisarts Wet. 2011;54:492–499.
