Abstract
Background
General practitioners (GPs) are increasingly confronted with people with both mild intellectual disability (MID) and mental health (MH) problems. Little is known about the type of MH problems for which people with MID visit their GP and the care provided.
Objectives
To identify the type and prevalence of MH disorders and MH-related complaints in people with MID in primary care and care provided, compared to people without ID.
Methods
By linking the Netherlands Institute for Health Services Research’s primary care databases, comprising electronic health records, with Statistic Netherlands’ social services and chronic care databases, we identified 11,887 people with MID. In this four-year retrospective study, MH-related International Classification of Primary Care (ICPC) codes and care characteristics were compared between people with MID and without ID.
Results
Of the people with MID, 48.8% had MH problems recorded vs. 30.4% of the people without ID, with significant differences in substance abuse, suicide attempts, and psychosis. Of the MID group, 80.3% were not registered by their GP with the ICPC code mental retardation. GPs provided more care to people with MID and MH problems than people without ID but with MH-problems regarding consultations (median 6.4 vs. 4.0 per year) and variety of prescribed medications (median 2.7 vs. 2.0 per year).
Conclusion
In primary care, the prevalence of MH problems and care provided is high in people with MID. To improve primary mental healthcare for this group, it is essential to increase GPs’ awareness and knowledge on the combination of MID and MH.
KEY MESSAGES
Nearly half of patients with mild intellectual disability (MID) experience mental health (MH) problems.
Patients with both MID and MH problems are provided with more consultations and medication prescriptions than patients without intellectual disability (ID) or with MID alone.
In more than 80% of the patients with MID, the ID was not properly registered and potentially unrecognised by the GP.
Introduction
People with mild intellectual disability (MID), characterised by a significant deficit in intellectual and adaptive functioning [Citation1], suffer from more mental health (MH) disorders compared to people without intellectual disability (ID) but often do not receive appropriate mental healthcare [Citation2–8]. General practitioners (GPs) are often the first point of contact for people with MH problems and are gatekeepers to specialised mental healthcare services [Citation9]. Prevalence studies in primary care with a specific focus on mental health in people with MID are scarce and focus on established MH disorders only, implicating a lack of knowledge on MH-related complaints (problems presented, no established diagnoses) in primary care.
There are several reasons for concern. First, the identification of both MH disorders and MID are problematic [Citation2,Citation9,Citation10]. Second, people with ID experience general health disparities, including mental health, because of barriers to providing timely, appropriate, and effective primary healthcare [Citation6]. Long-term conditions, like psychosis and depression, are poorly managed in primary care and psychotropic prescriptions exceed the number of reported MH disorders, suggesting inappropriate prescriptions [Citation2,Citation5,Citation9]. Finally, GPs themselves indicate a lack of knowledge and feel insecure about providing the care needed [Citation9,Citation11].
Nevertheless, little is known about the type of MH problems for which people with MID visit their GP and the care they receive. This primary care database study aims to provide an overview of the prevalence of both MH disorders and MH complaints in people with MID and the care provided in terms of consultations and medication prescriptions compared to people without ID. In addition, we study how often the GP adequately codes a person with MID.
Method
Study design
For this retrospective database study, we used databases from the Netherlands Institute for Health Services Research Primary Care Database (NIVEL-PCD) and Statistic Netherlands (SN) [Citation12,Citation13]. NIVEL collects healthcare data from routine electronic health register systems from over 400 representative Dutch general practices, covering approximately 10% of the Dutch population [Citation12]. The NIVEL-PCD files provided data regarding personal characteristics, type of health problems, consultations, and medication prescriptions from 1 January 2015 to 31 December 2018. MH problems were identified by ICPC-P codes (International Classification of Primary Care, Psychological category) [Citation14]. Medication prescriptions were coded according to the Anatomical Therapeutic Chemical (ATC) classification system up to level 3, the pharmacological subgroup [Citation15]. We included persons 18 years or older in 2015 who remained in the NIVEL-PCD for > 1 year.
Selection of study objectives
To identify people with MID in the NIVEL-PCD, that database was linked with an SN-MID database. In this database, persons are identified who, in 2015, used services under the Dutch Chronic Care Act, the Disability Benefit Act, or the Sheltered Employment Act with a MID registration ().
Figure 1. Composition of groups.
NIVEL-PCD: Netherlands Institute for Health Services Research Primary Care Database; SN: Statistics Netherlands; MID: Group with mild intellectual disability; No-ID: Group with no-intellectual disability; MH: people who had one or more MH problems coded with an ICPC-P other than P85; Match: Match control group; MID-MH: Group with mild intellectual disability and a mental health problem; Match-MH: Match control group with MH problem.
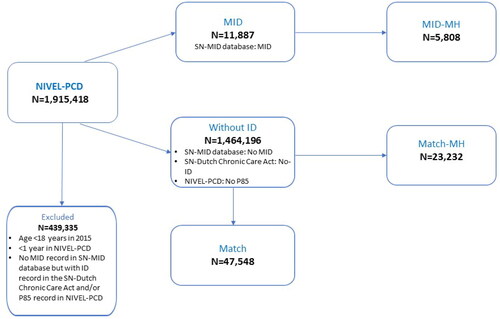
The comparison group without ID was not shown with a MID in the SN-MID database, had no ICPC code P85 (mental retardation) in the NIVEL-PCD, and was not eligible for ID-specific care according to the SN-Dutch Chronic Care Act database. We matched each individual from the MID group by age, sex and number of years in the dataset to four random individuals in the group without ID, to allow a robust comparison without overpowering.
We compiled a MID-MH group containing people who had one or more MH problems coded with an ICPC-P other than P85. An additional matched control group was asembled from the group without ID.
This study was reviewed and approved by the Medical Ethical Committee of Radboud University Medical Centre (2017-3921) and conducted according to the NIVEL and SN governance code. Results are reported per the RECORD statement.
Outcomes
The MID was considered ‘registered’ by the GP if the person had a P85 code in the NIVEL-PCD. To calculate the period prevalence of MH problems, MH illness episodes were constructed according to Nielen et al.’s algorithm [Citation16]. MH problems were divided into MH complaints with an ICPC code P1 to P29 and MH disorders with a code P70 to P99. We calculated the prevalence of unique MH problems and the median number of unique MH problems per patient during the research period. Additionally, ICPC codes relating to psychosis and substance abuse were combined and calculated per patient.
We described the number and type of consultations with a GP and mental health nurse practitioner (MHNP) and unique kinds of medication prescription categories. For comparison, we also described these for the MID group as a whole and their match group without ID, including people with and without MH problems. Each person’s medication prescription categories were recorded and divided into three selected categories: 1) Total medication use; 2) Psychotropics, including antipsychotics (N05A), anxiolytics (N05B), hypnotics and sedatives (N05C), antidepressants (N06A), psychostimulants (N06B), anti-dementia drugs (N06D), and drugs used in addictive disorders (N07B); and 3) Anti-epileptic medication (N03A), which may be prescribed for specific MH problems. It was impossible to link separate consultations and prescriptions to specific ICPC codes.
Statistical analysis
Groups were stratified by age groups and sex. Student’s t-tests, Chi-squared tests, or Mann-Whitney U-tests were used to test statistical significance. Logistic regression was used to examine the association with the presence of MID on outcomes, calculating odds ratios (OR) with 95% confidence intervals (95% CI) adjusted for age, sex, and years registered in the database. A p-value < .05 was considered statistically significant. Only variables with a number of ≥ 30 people were included to ensure clinical relevance. All analyses were conducted using SPSS version 25.0.
Results
Demographics
In the NIVEL-PCD, 11,887 persons with MID were identified, with a mean age of 37.8 years, of whom 61.7% male, compared to, respectively, 48.4 years and 48.8% male in the group without ID (n = 1,464,196). Of the people with a MID, 80.3% had no ICPC code P85 registration ().
Table 1. Demographics.
Period prevalence of MH problems
Of the people with MID, 48.9% had an MH problem over the four years period, either an MH complaint or an MH disorder, compared to 30.4% in the group without ID. They were significantly younger (37.1 vs. 50.6 years) and had a higher number of unique MH problems (median 2.0 vs. 1.0). In both groups, the prevalence of MH problems was higher in women. presents the ICPC codes with the highest OR for both MH complaints and MH disorders (a full overview can be found in Supplementary Table A).
Table 2. Prevalence of mental health problems in persons with and without intellectual disability.
More people with MID experienced an MH complaint than those without ID (36.2 vs. 21.4%; p < .001). The largest differences were seen in the codes ‘limited function and disability’ (P28; OR 38.18, 95% CI 33.34–43.72), ‘specific learning problems’ (P24; OR 6.23, 95% CI 5.14–7.55). In addition, 13.0% of the people with MID had an ICPC code associated with substance abuse (P15–P19), compared to 5.2% in the group without ID.
The prevalence of MH disorders was also higher in people with MID than those without ID (25.3 vs. 15.0%; p < .001). Large differences were seen in the codes ‘suicide/suicide attempt’ (P77; OR 3.80, 95% CI 3.14–4.60) and ‘psychological disorders, others’ (P99; OR 3.83, 95% CI 3.51–4.18). In addition, 4.2% of the people with MID had an ICPC code associated with psychosis (P71–73 and/or P98), compared to 1.4% in the group without ID.
Care provided
The GP had a median of 6.4 consultations per person per year in the MID group with an MH problem, compared to 4.0 consultations in the matched group without ID (). In the MID group as a whole, this was 4.3 consultations versus 2.3 in the group without ID (Supplementary Table B). In all groups, women had more consultations. Slightly fewer people in the MID group with MH problems had an MHNP consultation (24.8 vs. 26.7%; p <.001), and both the GP and the MHNP provided more short than lengthy consultations and more home visits to people with both MID and MH problems, compared to the matched group without ID ().
Table 3. Consultations with general practitioners and mental health nurse practitioners.
The GP provided a median of 2.7 unique types of medication prescription categories per person per year in the MID group with an MH problem, compared to 2.0 prescriptions in the matched group without ID (). In the whole MID group, this was 2.0 prescriptions vs. 1.0 in the group without ID (Supplementary Table B). Of the MID group with an MH problem, 55.4% received at least one psychotropic prescription (OR 1.39, 95% CI 1.31–1.47), 19.9% an antipsychotic (N05A; OR 3.15, 95% CI 2.90–3.41), and 24.9% an anxiolytic (N05B; OR 1.41, 95%CI 1.32–1.51). In addition, 8.7% received an anti-epileptic prescription (N03A; OR 2.05, 95%CI 1.83–2.29).
Table 4. Medication prescriptions.
Discussion
Main findings
In this primary care database study, we found that almost half of the people with MID experienced MH problems versus one-third of those without ID, with large differences in substance abuse, suicide attempts, and psychosis. GPs provided more consultations and types of medication prescriptions to people with a combination of MID and an MH problem compared to matched people without ID or with MID alone. More than 80% of the persons with MID were not registered by the GP as such.
Strengths and limitations
This study’s unique focus on people with mild intellectual disabilities is an important strength. We identified people with MID in primary care by linking a primary care database with a social services information database. This fills a blind spot about people with MID who would have been overlooked without data linkage. Another important strength is that this study does not focus only on MH disorders but gives a broader view by including MH complaints.
There are some limitations regarding databases containing routinely collected (health) data. In the NIVEL-PCD, details of diagnoses and treatments were limited and the care provided could not be linked to specific ICPC-P codes. The SN-MID database is composed mainly of users of work-related social services, resulting in an under-representation of older people. Finally, the database contains no exact information on intellectual and adaptive functioning on an individual level, so it cannot be ruled out that some people with more severe ID or borderline intelligence were included in our MID group. However, the SN-MID database is currently the most complete method available in the Netherlands to identify people with MID.
Comparison with existing literature
In our study, 25.3% of the people with MID had an MH disorder. This is comparable to Sheehan et al.’s primary care cohort study [Citation2], which found a point prevalence of 21% in people with any form of ID. Our incorporation of MH complaints has not been studied before in primary care.
The high prevalence of psychosis in MID (4.2%) we found was also observed in other primary care studies [Citation5,Citation17]. We found a higher prevalence of substance abuse in people with MID than those without ID. A systematic review that did not include primary care settings concluded that people with MID are at high risk of developing substance use disorder [Citation18]. The striking relatively high prevalence of ‘suicide/suicide attempt’ (P77) and unspecified ICPC-P codes (P29, P99) has not been previously reported in primary care studies. However, Dodd et al.’s systematic review of suicidality in people with ID revealed that having an MH disorder is an important risk factor for suicide in these patients [Citation19]. More importantly, it shows a lack of well-designed studies on suicide in people with ID, and there are limited ID-specific assessments or therapeutic interventions for suicidality.
The absence of a P85 code for most people with MID is in line with previous research [Citation10]. The relatively high prevalence of the ICPC codes ‘limited function/disability’ (P28) and ‘specific learning problems’ (P24) in people with MID in this study could indicate that these codes are used as a substitute for P85.
The higher number of GP consultations, home visits, and telephone consultations for people with MID and MH problems is in line with earlier research on people with ID in general in primary care [Citation17,Citation20,Citation21]. The relatively high number of medication prescriptions, especially psychotropics, for people with MID is consistent with earlier primary care research concerning people with ID [Citation2,Citation20,Citation22]. From earlier research it is known that people with ID have greater healthcare needs with higher morbidity and premature mortality levels than patients without ID, a situation to which insufficient quality of healthcare is a substantial contributor [Citation23]. Therefore, the differences that we found in the prevalence of MH problems and provided care between patients with MID and without ID indicate different healthcare needs in this specific patient group. However, our recent review on primary MH care to people with ID revealed that current primary MH care to this patient group is of an insufficient standard in terms of underdiagnosis of MH disorders, overmedication, and lack of effective patient follow-up, as well as limited GP experience in managing these patients [Citation9]. A possible reflection of the reported difficulties in providing adequate MH care to these patients may contribute to the differences observed.
Implications for research and practice
Timely recognition and treatment of not only MH disorders but also MH complaints are essential for the physical and emotional well-being and thus for the quality of life, of people with MID and therefore needs to be prioritised [Citation24]. This requires GPs to be aware of the high prevalence of MH problems in people with MID and to be aware and knowledgeable about the effect of MID on symptom presentation, communication, and treatment. This study’s results give rise to several opportunities to improve the quality of primary MH care for people with MID. First, the relatively high use of unspecified ICPC-P codes (P29, P99) and the relatively high number of people with MID who received psychotropic prescriptions could be signs that GPs experience difficulties in classifying and treating MH problems in people with MID. Communication difficulties, an atypical presentation of MH symptoms, and diagnostic masking or overshadowing, where symptoms are obscured by the ID or mislabelled, can contribute to these difficulties [Citation25]. Therefore, research on applicable primary MH guidelines for this patient group is important. Second, it is highly recommended to invest in recurring specific (postgraduate) training programmes for GPs. The relatively high prevalence of substance abuse and suicide in our study suggests that a proactive and preventive approach, aimed at identifying risk factors for MH problems and providing health education, should be part of this education. Third, GPs should be aware of the importance of identifying and registering MID for good care provision and for research purposes. ID screening tools can help identify MID and have been developed for GP practice but further implementation is needed [Citation26,Citation27]. GPs should reach clear agreement about when and how MID is recorded.
Fourth, it is important that primary care is accessible for people with MID and that their (mental) health needs are met. Future research should address the nature of the identified high-care utilisation in more detail. Our findings may be seen as a sign of additional healthcare needs and more intensive GP care provided to this patient group, putting a relatively high demand on primary care practices. As previous research indicated, GPs do not feel confident about providing care to people with ID [Citation28], particularly those with additional MH problems [Citation9,Citation11]. Support for GPs may help them better address these complex health needs and improve the care that they provide. According to patients with ID, adaptations in how care is provided could be helpful, such as enhancing GPs’ communication skills, extra consultation time, continuity of care from the same GP, and involvement of family or carers in consultations and information provision [Citation29,Citation30]. Periodic health assessments, supported by an instrument, are another way to identify (mental) health needs [Citation31]. Finally, although our database contained no information on referrals and consultations, GPs need to look to care professionals in their direct network for collaboration and support. Effective collaboration, specifically, is regarded as beneficial for the outcome of mental healthcare in primary care [Citation32]. Therefore it is important to learn from best practices [Citation32–34] and invest in (local) integrative and collaborative primary MH care models.
It remains of utmost importance to actively engage GPs and patients with MID in developing the suggested improvement strategies to ensure that they meet their needs and are applicable and feasible in daily practice.
Conclusion
We found that MID is most often not registered by GPs and most likely partially unrecognised. Almost half of the people with MID visited the GP with an MH problem and were provided with more care in consultations and types of prescribed medication categories than those without ID or with MID alone. This may indicate that people with both MID and MH problems have even higher healthcare needs than people with MID alone, with a corresponding higher demand for primary care. In addition, our results suggest that GPs struggle to register the MID as such, to establish the correct MH diagnosis and, consequently, to provide appropriate treatment. These findings illustrate the relevance of improving the quality of primary MH care for people with MID. This may be achieved by creating more GP awareness and knowledge of MH problems in people with MID, the importance of MID recognition, additional (care) needs, and the need for collaboration with relevant local care professionals.
Supplemental Tables
Download MS Word (45.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Aggregated data from the databases used in this study are publicly available on a dedicated website of Statistics Netherlands (http://statline.cbs.nl), and Netherlands Institute for Health Services Research (https://www.nivel.nl/en/nivel-zorgregistraties-eerste-lijn/nivel-primary-care-database). The non-public microdata used to link databases is, under certain conditions, accessible for statistical and scientific research (fees apply). Procedures can be found at www.cbs.nl and www.nivel.nl. For further information: [email protected] and [email protected]
Additional information
Funding
References
- American Assosiation on Intellectual and Developmental Disabilities. Intellectual disability: definition, classification, and systems of supports. 11th ed. Washington (DC): American Association on Intellectual and Developmental Disabilities; 2010.
- Sheehan R, Hassiotis A, Walters K, et al. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ. 2015;351:h4326.
- Cooper SA, Smiley E, Morrison J, et al. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190:27–35.
- van Duijvenbode N, VanDerNagel JE, Didden R, et al. Substance use disorders in individuals with mild to borderline intellectual disability: current status and future directions. Res Dev Disabil. 2015;38:319–328.
- Cooper SA, Hughes-McCormack L, Greenlaw N, et al. Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: a population-based cohort study. J Appl Res Intellect Disabil. 2018;31:68–81.
- Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev. 2006;12(1):70–82.
- Wieland J, Ten Doesschate M. Awareness and accessibility of the Dutch mental health care system for people with borderline intellectual functioning or mild intellectual disabilities. AMHID. 2018;12(3/4):114–120.
- Mason J, Scior K. ‘Diagnostic overshadowing’ amongst clinicians working with people with intellectual disabilities in the UK. J Appl Res Int Dis. 2004;17(2):85–90.
- Pouls KP, Koks-Leensen MC, Mastebroek M, et al. Adults with intellectual disabilities and mental health disorders in primary care: a scoping review. Br J Gen Pract. 2022;72(716):e168–e178.
- Russell AM, Bryant L, House A. Identifying people with a learning disability: an advanced search for general practice. Br J Gen Pract. 2017;67(665):e842–e850.
- Fredheim T, Haavet OR, Danbolt LJ, et al. Intellectual disability and mental health problems: a qualitative study of general practitioners’ views. BMJ Open. 2013;3(3):e002283.
- Netherlands Institute for Health Services Research (NIVEL). NIVEL primary care database. [cited 2022 Oct 26]. Available from: https://nivel.nl/en/nivel-primary-care-database
- Statistic Netherlands Organisation (CBS). About Statistic Netherlands. [cited 2022 Oct 26]. Available from: https://www.cbs.nl/en-gb/about-us/organisation
- Lamberts H, Wood M. International classification of primary care (ICPC). Oxford: Oxford University Press; 1987.
- World Health Organisation. Guidelines for ATC classification and DDD assignement 2020. [cited 2022 October 26]. Available from: https://www.whocc.no/atc_ddd_index_and_guidelines/guidelines/
- Nielen MMJ, Spronk I, Davids R, et al. Estimating morbidity rates based on routine electronic health records in primary care: observational study. JMIR Med Inform. 2019;7(3):e11929.
- Carey IM, Shah SM, Hosking FJ, et al. Health characteristics and consultation patterns of people with intellectual disability: a cross-sectional database study in English general practice. Br J Gen Pract. 2016;66(645):e264–e270.
- van Duijvenbode N, VanDerNagel JEL. A systematic review of substance use (disorder) in individuals with mild to borderline intellectual disability. Eur Addict Res. 2019;25(6):263–282.
- Dodd P, Doherty A, Guerin S. A systematic review of suicidality in people with intellectual disabilities. Harv Rev Psychiatry. 2016;24(3):202–213.
- Cassidy G, Martin DM, Martin GHB, et al. Health checks for people with learning disabilities: community learning disability teams working with general practitioners and primary health care teams. J Learn Disabil. 2002;6(2):123–136.
- Straetmans J, van Schrojenstein Lantman-de Valk H, Schellevis F, et al. Health problems of people with intellectual disabilities: the impact for general practice. Br J Gen Pract. 2007;57(534):64–66.
- Doan TN, Lennox NG, Taylor-Gomez M, et al. Medication use among Australian adults with intellectual disability in primary healthcare settings: a cross-sectional study. J Intellect Dev Disabil. 2013;38(2):177–181.
- Heslop P, Blair PS, Fleming P, et al. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet. 2014;383(9920):889–895.
- Schalock RL, Verdugo MA. Handbook on quality of life for human service practitioners. Washington (DC): American Association on Mental Retardation; 2002.
- Manohar H, Subramanian K, Kandasamy P, et al. Diagnostic masking and overshadowing in intellectual disability-how structured evaluation helps. J Child Adolesc Psychiatr Nurs. 2016;29(4):171–176.
- Hayes SC. Hayes Ability Screening Index (HASI), manual. Sydney: Department of Behavioural Sciences in Medicine, University of Sydney; 2000.
- Nijman H, Kaal H, van Scheppingen L, et al. Development and testing of a screener for intelligence and learning disabilities (SCIL). J Appl Res Intellect Disabil. 2018;31(1):e59–e67.
- Wilkinson J, Dreyfus D, Cerreto M, et al. “Sometimes I feel overwhelmed”: educational needs of family physicians caring for people with intellectual disability. Intellect Dev Disabil. 2012;50(3):243–250.
- Mastebroek M, Naaldenberg J, van den Driessen Mareeuw FA, et al. Experiences of patients with intellectual disabilities and carers in GP health information exchanges: a qualitative study. Fam Pract. 2016;33(5):543–550.
- Perry J, Felce D, Kerr M, et al. Contact with primary care: the experience of people with intellectual disabilities. J Appl Res Intellect Disabil. 2014;27(3):200–211.
- Bakker-van Gijssel EJ, Olde Hartman TC, Lucassen PL, et al. GPs’ opinions of health assessment instruments for people with intellectual disabilities: a qualitative study. Br J Gen Pract. 2017;67(654):e41–e48.
- Ervin DA, Williams A, Merrick J. Primary care: mental and behavioral health and persons with intellectual and developmental disabilities. Front Public Health. 2014;2:76.
- Health NKC. Community learning disability Team [Information webside]. 2020 Aug [cited 2022 Oct 27]. Available from: https://www.kentcht.nhs.uk/service/community-learning-disability-team/
- National Association of Intellectual Disability Physicians (NVAVG), National Association of General Practitiones (LHV). Handreiking samenwerking huisarts en AVG. 2017. [cited 2022 October 27]. Available from: https://www.lhv.nl/product/handreiking-samenwerking-huisarts-en-avg/
