Abstract
Objective: There have been attempts to modify the Montreal Cognitive Assessment (MoCA), a brief cognitive screening tool, for use across several Asian countries, but evidence to support the utility of these translations has been limited, particularly for the Vietnamese translation of the MoCA (MoCA-V). This two-part study aimed to evaluate the MoCA-V in a Vietnamese sample. Methods: In the first stage, we examined the relationships between the MoCA-V subscales and common neuropsychological tests among healthy Vietnamese adults (n = 129) and individuals with moderate-to-severe traumatic brain injury (n = 80). In the second stage, we explored the relationship of TBI status (TBI vs non-TBI) and demographic variables to MoCA-V performance and investigated the optimal cut-off score of the MoCA-V using the two samples combined. Results: The MoCA-V Attention, Language, and Executive Function subscales were correlated with the Digit Span Test, Verbal Fluency Test, and Trail Making Test, respectively, across healthy participants and participants with TBI. Global performance on the MoCA-V was predicted by TBI status, education, and age. Our ROC analysis revealed that a cut-off score of 22 offered the best sensitivity (76.3%) and specificity (71.3%) trade-off for identifying cognitive impairment as measured by the MoCA-V. Conclusions: In addition to identifying a cut-off score for cognitive screening, the findings provide support for the validity of the examined MoCA-V subscales and for the MoCA-V’s ability to distinguish TBI survivors vs controls. These results may pave the way for larger-scale investigations of the MoCA-V and for the development of more neuropsychological batteries in Vietnamese.
Despite the overall growth of clinical neuropsychology worldwide within the last quarter-century, there are still many disparities in the availability of neuropsychological resources, particularly within developing or economically disadvantaged countries. For example, there were no practicing clinical neuropsychologists in many Southeast Asian countries in 2017, including Vietnam (Ponsford, Citation2017). In addition, because most cognitive assessments have been developed and validated for Western, English-speaking individuals, there is a lack of culturally relevant tests for those who do not hold those identities. The simple translation of English-language tests into different languages is insufficient for addressing the barrier of limited test availability because direct translations may not consider unique cultural differences that may affect test interpretation. Further, simple translation does not account for whether a test measures a cognitive construct it intends to measure (Siedlecki et al., Citation2010). Thus, it is important to consider language and other cultural factors (e.g. history, within-culture diversity) when attempting to develop and validate tests for non-Western populations.
The Montreal Cognitive Assessment (MoCA) (Nasreddine et al., Citation2005) is a brief test designed to screen for mild cognitive impairment (MCI) or dementia. The 30-point measure consists of items that measure orientation, attention, language, short-term memory, visuospatial abilities, and aspects of executive functioning (i.e. working memory, abstract thinking, and verbal fluency), many items of which are adapted from other embedded or standalone assessments (e.g. Wechsler Adult Intelligence Test of Intelligence—Digit Span subtest, Verbal Fluency Test, and Trail Making Test). The original MoCA normative sample (mean age of 70) included English and French participants, with 90 cognitively intact controls, 94 older adults with MCI, and 93 individuals with Alzheimer’s (AD). The recommended cut-off score for indicating impairment is <26, with a one-point adjustment for level of education (Nasreddine et al., Citation2005). Although the MoCA was initially developed to screen for dementia-related conditions, many professionals currently use the MoCA as a brief cognitive screener across clinical settings and presentations, such as stroke (Chan et al., Citation2014) and traumatic brain injury (De Guise et al., Citation2014).
Since the MoCA was originally established and normed with Western samples, there have been many attempts to adapt and evaluate the screener in non-English languages while keeping in mind cultural and linguistic differences. Examples of Asian adaptations of the MoCA include those created for Chinese (Hu et al., Citation2013), Korean (Lee et al., Citation2008), Indonesian (Husein et al., Citation2010), and Singaporean (Ng et al., Citation2013) samples. Findings from these studies indicated the promising utility of adapted versions of the MoCA and revised cut-off scores that vary across groups. For instance, Lee et al. (Citation2008) proposed that a cut-off score of 22/23 on the Korean version of the MoCA (i.e. MoCA-K) had excellent sensitivity (89%) and good specificity (84%) for screening MCI. Li and Yu (Citation2012) examined the utility of the recommended cut-off score of 26 on a Chinese version of the MoCA (MoCA-CV) and found that while the score had excellent sensitivity (90.4%) for detecting MCI from controls, the specificity was relatively poor (32.0%); they proposed that using a lower cut-off score of 22 was optimal for balancing a sensitivity of 68.7% and specificity of 65.2%. However, while the MoCA has been assessed in different Asian cultures, examinations of MoCA adaptations in Vietnam have been scant (Quang et al., Citation2022).
A study of the Vietnamese MoCA (MoCA-V) by Do et al. (Citation2022) in a sample of 48 Vietnamese American older adults found evidence in support of the validity of the measure. Specifically, they found moderate to large correlations between the MoCA-V subdomains and total score (r’s = .48 to .79) and good internal consistency (.80) for the measure. Additionally, although they did not specifically diagnose participants with MCI, their findings noted that the traditional cut-off score of 26 would likely not be appropriate for this sample as it resulted in an unreasonably large proportion of the sample (∼90%) screening positive for MCI. In Nguyen et al.’s (Citation2022) study examining cognitive functioning in Vietnamese American women with and without exposure to neurotoxins, the authors found associations between MoCA scores with education and exposure index but not with age or English proficiency. These findings highlight the importance of considering demographic factors when implementing and interpreting the MoCA-V. Additional work needs to be done to examine the use of the MoCA-V in assessing cognitive functioning among other Vietnamese clinical populations.
Vietnam currently stands as the 15th largest country in the world, with a population of more than 97 million people, most of whom (over 85%) belong to the Kinh ethnic group and speak Vietnamese. This language has three major dialects that correspond to the three main geographic regions of Vietnam: Northern Vietnam, Central Vietnam, and Southern Vietnam. Due to its geographic location and long history of war, occupation, and colonization by other countries such as China and France, Vietnam’s values, customs, and educational systems contain influences from both Eastern and Western sources (Tran et al., Citation2022). Following the end of the civil war between the Communist North and anti-Communist South in 1975, Vietnam experienced significant economic growth that subsequently led to an increase in motorization, with motorcycles and bicycles constituting the majority of traffic in this country (Ngo et al., Citation2012; Tran et al., Citation2022).
A common outcome of traffic accidents in Vietnam is traumatic brain injury (TBI), which has been associated with various physical, emotional, and cognitive symptoms (Carr et al., Citation2018; Vu et al., Citation2019) with the level of resulting dysfunction correlating with the severity of the injury (Hawryluk & Manley, Citation2015). Accurate detection of, and timely intervention for, cognitive impairment is important to improve patients’ functioning and quality of life (Gorgoraptis et al., Citation2019). Standard neuropsychological testing can require a significant amount of time and resources. As an alternative, brief cognitive screeners are often used in outpatient settings to detect signs of cognitive impairment and signal a need for a more comprehensive evaluation or to monitor changes in global cognition over time (Beinhoff et al., Citation2005).
The use of cognitive screeners may be especially beneficial in settings such as Vietnam, where resources and extensive follow-up on patients may be limited, as individuals with moderate-to-severe TBI are most often treated through conservative treatment methods and family-based care (Vu, Citation2021). That said, simple translation and application of existing screeners are not enough. Recent studies examining the assessment of common TBI-related symptoms, like apathy, suggest the need to adapt measures in ways that account for the sociocultural factors that affect symptom presentation among Vietnamese individuals (Quang et al., Citation2022; Quang et al., Citation2022).
Currently, cognitive screening measures with Vietnamese language versions include the MoCA, Mini-Mental State Examination, and Vietnamese Clinical Dementia Rating scale (Le & Tran, Citation2017; Leggett et al., Citation2013; Nguyen & Tran, Citation2017). Although these measures are utilized for assessing cognitive functioning in Vietnam, when Western-derived cut-off scores are used to identify cognitive impairment, there is often misclassification or misdiagnosis (Leggett et al., Citation2013). In a validation study of the MoCA-V conducted by Nguyen and Tran (Citation2017), the authors identified cut-offs for differentiating between those with major (cut-off of 16/17) or mild (cut-off of 21/22) neurocognitive disorders from normal controls. However, they did not describe the specific etiologies of their participants with major/mild neurocognitive disorders and did not examine the construct validity of the MoCA-V. Given that the original proposed cut-off score of 26 may not be adequate for identifying cognitive impairment in diverse samples, there is a need for additional research to determine more accurate cut-off scores and to examine how the MoCA-V may be used among different clinical populations, including those with moderate-to-severe TBI.
Purpose of study
This two-part study aimed to evaluate the psychometric properties of the Vietnamese translation of the MoCA (MoCA-V) in Vietnam. In the first stage, we examined the relationships between the MoCA-V Attention, Language, and Executive Function subscales and common neuropsychological tests, such as the Digit Span Test, Verbal Fluency Test, and Trail Making Test, among healthy Vietnamese adults and patients with moderate-to-severe TBI. In the second stage, we explored the effects of TBI and demographic variables (age, gender, and education) on general performance on the MoCA-V. We identified the optimal cut-off score of the MoCA-V to assess for persisting cognitive symptoms at least nine months post-injury.
Methods
Participants
This study was conducted in Ho Chi Minh City and its adjacent metropolises in Vietnam in 2020. Healthy participants were recruited through advertisements on social media. Potential participants with interest in the study were contacted and pre-screened. Inclusion criteria were: (a) being 18 to 65 years of age, (b) having normal-to-corrected vision and hearing, and (c) being able to provide informed consent. Participants were excluded if they reported any significant history, or current presence, of a neurological or psychiatric disorder diagnosis. They were also administrated a comprehensive neuropsychological battery whereby any abnormal cognitive ability was noted and reviewed by a team of neurologists and neuropsychologists. Participants received either course credit (if they were students) or VND200,000 (∼USD10) as compensation for their participation.
Patients with moderate-to-severe TBI were recruited in stage 2 based on a patient dataset at Cho Ray Hospital (the largest hospital specializing in brain injuries in Southern Vietnam) using the keyword “frontal contusion,” with the hospital admission time frame set from 2016 to 2019. Inclusion criteria were: (a) being 18 to 65 years of age at the time of injury, (b) having a Glasgow Coma Scale score of < 13 within 24 hours of injury indicating moderate to severe injuries, and (c) having neuroimaging evidence of brain damage. Patients were excluded if they (1) had a history of any diagnosed neurological/psychiatric disorder and/or had prior moderate to severe brain injuries, (2) had vision or hearing problems that could not be corrected, (3) were unable to show some level of movement (e.g. sitting), (4) had substance misuse, or (5) had limited Vietnamese proficiency. At the time of assessment, all patients had been discharged from the hospital and had been living in the community for at least nine months. The first screening was conducted based on patients’ medical records and yielded 1106 patients satisfying eligibility criteria. These patients were contacted via telephone and re-screened for criteria that could not be obtained via medical records. Of those, 80 patients with TBI were eligible, contactable, agreed to participate in the research, and had data available for the MoCA-V. All patients with TBI were evaluated by a neurologist at the time of the research. Patients with TBI were reimbursed with medical costs (∼USD30) for their time participating in the study. The study was approved by the University of New South Wales’ Human Ethics Committee and the Cho Ray Hospital’s Ethics Committee for Biomedical Research. All participants and their informants/caregivers gave written informed consent before participation.
Measures
Details for the adaptation processes of the MoCA-V, Trail Making Test Parts A & B, Verbal Fluency Test, and Digit Span Test are outlined below. We selected the Trail Making Test Parts A & B, Verbal Fluency Test, and Digit Span Test because they are commonly used to assess neurocognitive performance after TBI and do not require extensive cultural adaptations. Test instructions and materials were translated by a bilingual neuropsychological researcher (HQ). Two independent examiners conducted a pilot administration on 16 participants (data not included in the final analyses), followed by a thorough revision of test instructions and materials.
Vietnamese Montreal cognitive assessment (MoCA-V)
All participants in this study were administered the MoCA-V version 7.1 retrieved from the MoCA’s official webpage (https://www.mocatest.org/) for a general evaluation of cognitive functioning (Nasreddine et al., Citation2005). This version was translated by a Vietnamese neurologist and approved by the MoCA’s original author. Like the English version, the maximum total score for the MoCA-V is 30 points, with higher scores indicating better cognitive performance. One point is added if the examinee has 12 years of education or fewer. No robust cut-off scores for cognitive impairment for the MoCA-V have been identified prior to this study, and there have been no prior comparisons of the MoCA-V to more comprehensive cognitive measures to establish construct validity. The MoCA-V is a translation of the English MoCA with adaptations and modifications to account for cultural and linguistic factors relevant to the Vietnamese population. Namely, English letters and words were replaced with Vietnamese ones, while sentences and pictures were changed to ensure local familiarity.
Index scores for the MoCA sub-domains are calculated as officially instructed (Julayanont et al., Citation2014). In particular, the MoCA-Memory was calculated by adding the number of words remembered in free delayed recall, category-cued recall, and multiple choice–cued recall multiplied by 3, 2, and 1, respectively, with a score ranging from 0 to 15. The MoCA-Executive functions were obtained by adding raw scores for the modified Trail-Making Test Part B, clock drawing, digit span forward and backward, letter A tapping, serial-7 subtraction, letter fluency, and abstraction items, with a score ranging from 0 to 13. The Attention Index Score is the sum of points from digit span forward and backward, letter A tapping, serial-7 subtraction, sentence repetition, and the words recalled in both immediate recall trials, with a score ranging from 0 to 18. The MoCA-Language was determined by adding the raw scores for naming, sentence repetition, and letter fluency, with a score ranging from 0 to 6. The MoCA-Visuospatial ability was obtained by adding the raw scores of the cube copy, clock drawing, and naming items, with a score ranging from 0 to 7. Lastly, the MoCA-Orientation was the sum of scores for the orientation section items, with a score ranging from 0 to 6.
Trail making test parts A and B
The Trail Making Test (TMT; Reitan & Wolfson, Citation1995) is a two-part measure that examines visual attention and set-shifting (i.e. task-switching) abilities. These timed visual-motor tasks require examinees to first connect a series of numbers (TMT-A) and to then alternate between connecting numbers and letters in order (TMT-B) as quickly as possible. We used the original TMT-A for this study, given that numbers are universal across the English and Vietnamese language. For the TMT-B, all English letters were replaced with letters according to the Vietnamese alphabet.
Verbal fluency tests
Verbal fluency tests are commonly used in research and clinical practice to evaluate verbal generation ability based on language. There are two components of verbal fluency: (1) letter fluency, in which participants are required to produce as many words as possible beginning with a given letter (e.g. “F”), and (2) semantic fluency, in which participants are provided with a category (e.g. animal) and asked to generate words that fit in the category. The time limit for generating each letter or semantic trial is 60 seconds.
As the letters F, A, and S, which are most used in the English verbal fluency test, are not appropriate for the Vietnamese language, we developed a Vietnamese Verbal Fluency Test (VVFT) following a previously published procedure (Kosmidis et al., Citation2004). We selected two of the most authoritative and comprehensive Vietnamese dictionaries and ranked all 29 Vietnamese letters based on the ratio of words starting with these letters relative to the total number of words in the dictionary. We then reviewed how frequently each letter was used at the beginning of Vietnamese words. For the English verbal fluency tests, the letters S was consistently reported among the most frequent initial letters in English (ranked between the first to fourth), A was ranked the second or third, and F was between the fifth to eleventh. Based on this, the Vietnamese letters selected for the VVFT were H, N, and T. We continued to utilize animals as the category for measuring semantic fluency.
Digit span test
The Digit Span test (Wechsler, Citation2008) is a commonly used measure of auditory attentional capacity and working memory. This test requires examinees to repeat a string of numbers in forward and backward order. Like the TMT-A, the original Digit Span test (with original items translated into Vietnamese) was used in this study.
Data analysis
Descriptive statistics (i.e. means, standard deviations, and ranges) were generated for demographic and test variables. Parametric assumptions were tested using Shapiro-Wilk tests. Spearman’s correlations were performed to investigate the relationships between MoCA-V scores and variables from the Digit Span Test, Verbal Fluency Test, and Trail Making Tests within healthy individuals and people with TBI. To assess the effect of TBI on MoCA-V performance, a multiple regression model was conducted across healthy participants and individuals with TBI, with group status (TBI vs. non-TBI) and demographic variables (age, sex, and education) as predictors. Collinearity assumptions were checked and met (all Tolerance values > .58 and all VIF values < 1.70). A receiving-operator curve (ROC) analysis was employed with all participants (80 individuals with TBI and 129 healthy participants) to identify an optimal cut-off score for identifying general cognitive impairment after TBI. P values were set as ≤.05 for significant results. SPSS Statistics, Version 26, was used for all statistical analyses.
Results
Performance on the MoCA-V in healthy people
The healthy sample was composed of 129 participants, with a mean age of 31.6 years (standard deviation [SD] = 13.25) and a mean educational attainment of 11.96 years (SD = 4.55). 49% of the sample was female. The majority of participants were blue-collar workers (32.6%), white-collar workers (29.5%), and students (29.5%), whereas 6.3% of people were freelancers, 1.6% were homemakers, and 0.8% were retired. The demographic characteristics and cognitive variables are presented in .
Table 1. Demographic and cognitive characteristics of healthy participants and participants with TBI.
Correlations between individual MoCA domain scores, digit span, verbal fluency, and TMT
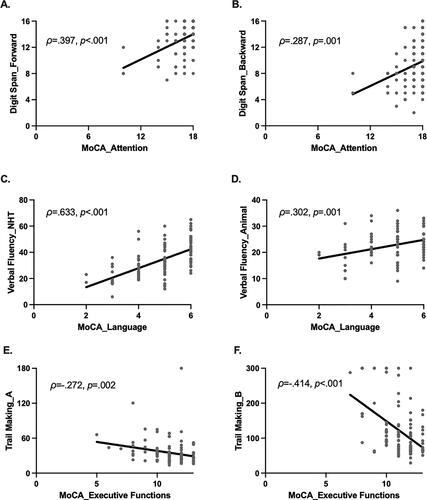
Spearman’s correlations revealed that higher scores on the MoCA-attention domain were significantly correlated with higher scores on Digit Span Forward [ρ(110) = .397, p < .001; ] and Digit Span Backward [ρ(110) = .287, p = .001; ]. Higher scores on the MoCA-Language index were also significantly correlated with more correct items generated for both letter [ρ(107) = .633, p < .001; ] and semantic fluency [ρ(107) = .302, p = .001, ]. Finally, greater performance on the MoCA-Executive Function index was significantly associated with faster completion times on the TMT-A [ρ(108) = −.272, p = .002; ] and TMT-B [ρ(108) = −.414, p <. 001; ].
Performance of the MoCA-V in individuals with moderate-to-severe TBI
Demographic and clinical features of the participants with moderate-to-severe TBI can be seen in . The TBI sample included 80 participants, with a mean age of 34.13 years (SD = 11.54) and a mean educational attainment of 9.07 years (SD = 3.96). 11.25% of the sample was female. The participants with moderate-to-severe TBI had a mean age at injury of 31.88 years (SD = 11.40), a mean time since injury of 26.54 months (SD = 11.46, range = 9–51), and a mean score on the Glasgow Coma Scale obtained within the first 24 hours of injury of 8.7 (SD = 2.52). Time since injury was not significantly correlated with TBI severity as measured with the Glasgow Coma Scale (ρ(78) = −.189, p = .093).
Correlations between individual MoCA domain scores, digit span, verbal fluency, and TMT after TBI
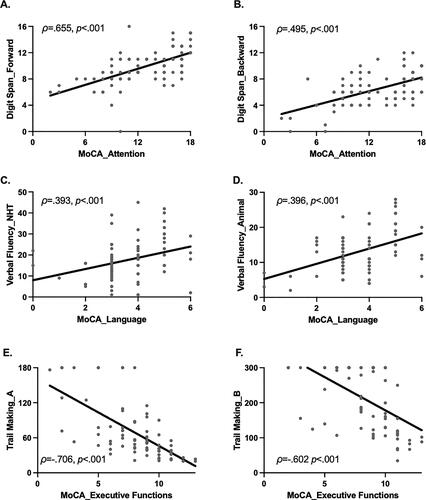
Spearman’s correlations revealed that higher scores on the MoCA-Attention domain were significantly correlated with higher scores on Digit Span Forward [ρ(78) = .655, p < .001; ] and Digit Span Backward [ρ(78) = .495, p < .001; ]. Higher scores on the MoCA Language domain were also significantly correlated with more correct items generated for both letter [ρ(71) = .393, p < .001; ] and semantic fluency [ρ(75) = .396, p < .001, ]. Finally, greater performance on the MoCA-Executive Function domain was significantly associated with faster completion times on the TMT-A [ρ(77) = −.706, p < .001; ] and TMT-B [ρ(71) = −.602, p <. 001; ].
Effects of TBI and demographic variables on MoCA-V performance and cut-off score identification
The regression model for TBI status (TBI vs non-TBI) and demographic predictors of the MoCA-V was significant (F(4, 204) = 79.225, p <.001; ). TBI, age, and education were significant predictors, accounting for 10.37%, 2.07%, and 13.91% of the variance in MoCA-V scores, respectively. By contrast, sex did not significantly predict cognitive performance measured by the MoCA-V (p = .550).
Table 2. Regression models for the demographic and clinical predictors of MoCA total scores (N = 209).
The ROC results revealed that a score of 22.5 offered the best sensitivity (76.3%) and specificity (71.3%) trade-off (). The area under the curve was 0.811 (95% CI = .75 − .87, p < .001), suggesting that the diagnostic accuracy of the test is good (). Therefore, a cut-off of 22 or lower is recommended for the identification of cognitive impairment on the MoCA-V. Based on this cut-off of ≤22, 76.3% of the people in the TBI group had cognitive impairment.
Table 3. Sensitivity and specificity according to different cut-offs (N = 209).
Discussion
Without an empirically validated cognitive screening tool, implementing clinical assessment for Vietnamese patients with impairments in cognition has been challenging. There have been efforts to translate common neuropsychological measures into the Vietnamese language. However, most of these tests were not developed with consideration of the Vietnamese culture and have lacked empirical support. The purpose of this study was to evaluate the psychometric properties of the Vietnamese translation of the MoCA by comparing it to performances on other common neuropsychological tests such as the Digit Span Test, Verbal Fluency Test, and Trail Making Test. Furthermore, we explored optimal cut-off scores for the MoCA-V among healthy participants and patients with TBI with cognitive impairment.
Our findings suggest good construct validity of the MoCA-V Attention, Language, and Executive Function subscales when these subscales were compared to neuropsychological tests adapted for this study. The translation and adaptation of the verbal fluency measure utilized in this study strictly followed the guidelines established in identifying common letters in the Vietnamese alphabet (Kosmidis et al., Citation2004) and the TMT-B was adapted with English letters being substituted with letters from the Vietnamese alphabet. We found that several individual MoCA-V domain scores significantly correlated with common neuropsychological measures intended to measure similar cognitive constructs. Specifically, MoCA-V Attention, Language, and Executive Function domain scores were significantly correlated with the Digit Span test, Verbal Fluency test, and TMT-B, respectively. These findings demonstrate convergent validity for the components of the MoCA-V that we examined and are consistent with other studies that have compared the MoCA to more comprehensive cognitive measures in different languages, including English (Vogel et al., Citation2015), French (Moafmashhadi & Koski, Citation2013), and Italian (Siciliano et al., Citation2019).
In addition to finding an effect of TBI status (TBI vs non-TBI) in predicting cognitive dysfunction, this study reports the roles of age, gender, and education on MoCA-V performances. Our study supports previous empirical findings that increased age is associated with lower general cognitive performance on the MoCA (Gluhm et al., Citation2013). We also found that education was a significant predictor of MoCA-V scores, and these results are consistent with findings reported from different ethnic populations (Aiello et al., Citation2022; Borland et al., Citation2017). This finding is consistent with the cognitive reserve theory in TBI, which suggests that higher pre-morbid education is significantly predictive of better outcomes post-injury (Kesler et al., Citation2003; Spitz et al., Citation2012).
Our ROC analysis suggests that a MoCA-V cut-off score of 22 significantly differentiates between individuals with a history of TBI and cognitive impairment from individuals with a history of TBI and without cognitive impairment (AUC = .82; 76% sensitivity, 71% specificity). In addition, the lower cut-off is similar to many other international studies on the validation of the MoCA. Delgado et al. (Citation2019) reported a cut-off of <21 and <20 for differentiating between amnestic mild cognitive impairment and mild dementia; Lu et al. (Citation2011) identified the optimal cut-off points as 13/14 for illiterate individuals, 19/20 for individuals with 1 to 6 years of education, and 24/25 for individuals with 7 or more years of education; and Chu et al. (Citation2015) identified the optimal cut-off score for detection of Alzheimer’s as 19/20 in a Chinese population. Of note, our study’s cut-off is similar to Nguyen and Tran’s (Citation2017) cut-off of 21/22 for distinguishing between those with a mild neurocognitive disorder and healthy controls in a Vietnamese sample.
The present study has noteworthy strengths and limitations that may inform future research in cross-cultural assessments of the Vietnamese population. First, we conducted the first cultural adaptation and validation of several common neuropsychological measures in Vietnamese. Future studies may examine the utility of the MoCA-V for determining the need for more extensive neuropsychological evaluation across populations, particularly given the well-known limitations of the MoCA’s ability to detect abnormalities in specific cognitive domains. Another limitation of our study was that we only examined the Attention, Language, and Executive Function subscales from the MoCA-V. Findings from this study are also limited to the sample of patients with TBI from frontal contusions, which were examined cross-sectionally. Thus, our results may not generalize to individuals with other types of brain injuries. Furthermore, because participants with TBI were examined at least nine months post-injury rather than at the time of their injury, we cannot draw conclusions about the utility of the MoCA-V in predicting prognosis. While recognizing this, it should also be noted that detecting cognitive deficits in the sub-acute and chronic phases of TBI is of particular importance in the context of Vietnam where cognitive functioning does not represent a priority in first-line assessment or interventions provided in the acute stage of TBI. Patients and families often seek cognitive assessments many years following TBI, after they notice the significant impact TBI symptoms on daily functioning. Finally, since the MoCA was developed to detect MCI and dementia, which relies upon the test’s episodic memory and orientation items, the absence of measures for these constructs is a limitation. Additional studies are needed to examine the properties of the Memory and Visuospatial subscales of the MoCA-V, increase the generalizability of these findings among other clinical populations, and evaluate test-retest reliability on the MoCA-V for clinical practice. As age and education have been consistently reported to be significant predictors of the MoCA scores, even after the scores were corrected for education, a next important step would be collecting normative data based on a larger Vietnamese sample, stratified by age and education, to provide specific cut-offs for different demographic groups.
In summary, our findings have important implications for clinical practice and future research. This study is among the first to provide empirical support for the validity of the MoCA-V Language, Attention, Executive Function subscales and their related neuropsychological measures. The MoCA-V with a cut-off score of 22 is also demonstrated to be suitable for screening for cognitive impairment post-TBI and may be helpful for guiding clinical decision-making on whether a full neuropsychological evaluation is needed. This study offers evidence for using an important cognitive assessment tool to examine neurological conditions in research and clinical practice among an underserved population. This may pave the way for larger-scale investigations of the MoCA-V and for the development of more comprehensive neuropsychological test batteries in Vietnamese.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aiello, E. N., Gramegna, C., Esposito, A., Gazzaniga, V., Zago, S., Difonzo, T., Maddaluno, O., Appollonio, I., & Bolognini, N. (2022). The Montreal Cognitive Assessment (MoCA): Updated norms and psychometric insights into adaptive testing from healthy individuals in Northern Italy. Aging clinical and Experimental Research, 34(2), 375–382. https://doi.org/10.1007/s40520-021-01943-7
- Beinhoff, U., Hilbert, V., Bittner, D., Grön, G., & Riepe, M. W. (2005). Screening for cognitive impairment: A triage for outpatient care. Dementia and Geriatric Cognitive Disorders, 20(5), 278–285. https://doi.org/10.1159/000088249
- Borland, E., Nägga, K., Nilsson, P. M., Minthon, L., Nilsson, E. D., & Palmqvist, S. (2017). The Montreal Cognitive Assessment: Normative data from a large Swedish population-based cohort. Journal of Alzheimer’s Disease, 59(3), 893–901.
- Carr, C., Kahn, L., Mathkour, M., Biro, E., Bui, C. J., & Dumont, A. S. (2018). The shifting burden of neurosurgical disease: Vietnam and the middle-income nations. Neurosurgical Focus, 45(4), E12. https://doi.org/10.3171/2018.7.FOCUS18297
- Chan, E., Khan, S., Oliver, R., Gill, S. K., Werring, D. J., & Cipolotti, L. (2014). Underestimation of cognitive impairments by the Montreal Cognitive Assessment (MoCA) in an acute stroke unit population. Journal of the Neurological Sciences, 343(1–2), 176–179.
- Chu, L. W., Ng, K. H., Law, A. C., Lee, A. M., & Kwan, F. (2015). Validity of the Cantonese Chinese Montreal cognitive assessment in Southern Chinese. Geriatrics & Gerontology International, 15(1), 96–103. https://doi.org/10.1111/ggi.12237
- De Guise, E., Alturki, A. Y., LeBlanc, J., Champoux, M.-C., Couturier, C., Lamoureux, J., Desjardins, M., Marcoux, J., Maleki, M., & Feyz, M. (2014). The Montreal cognitive assessment in persons with traumatic brain injury. Applied neuropsychology: Adult, 21(2), 128–135. https://doi.org/10.1080/09084282.2013.778260
- Delgado, C., Araneda, A., & Behrens, M. (2019). Validation of the Spanish-language version of the Montreal Cognitive Assessment test in adults older than 60 years. Neurología (English Edition), 34(6), 376–385. https://doi.org/10.1016/j.nrleng.2018.12.008
- Do, M., Bui, B. K. H., Pham, N. K., Anglewicz, P., Nguyen, L., Nguyen, T., Tran, C. T., & van Landingham, M. (2022). Validation of MoCA test in Vietnamese language for cognitive impairment screening. Journal of Global Health Neurology and Psychiatry, e2022008. https://doi.org/10.52872/001c.35656
- Gluhm, S., Goldstein, J., Loc, K., Colt, A., Van Liew, C., & Corey-Bloom, J. (2013). Cognitive performance on the mini-mental state examination and the Montreal Cognitive Assessment across the healthy adult lifespan. Cognitive and Behavioral Neurology: Official Journal of the Society for Behavioral and Cognitive Neurology, 26(1), 1–5. https://doi.org/10.1097/WNN.0b013e31828b7d26
- Gorgoraptis, N., Zaw-Linn, J., Feeney, C., Tenorio-Jimenez, C., Niemi, M., Malik, A., Ham, T., Goldstone, A. P., & Sharp, D. J. (2019). Cognitive impairment and health-related quality of life following traumatic brain injury. NeuroRehabilitation, 44(3), 321–331. 10.3233/NRE-182618 31177238
- Hawryluk, G. W., & Manley, G. T. (2015). Classification of traumatic brain injury: Past, present, and future. Handbook of Clinical Neurology, 127, 15–21. https://doi.org/10.1016/B978-0-444-52892-6.00002-7
- Hu, J-b., Zhou, W-h., Hu, S-h., Huang, M-l., Wei, N., Qi, H-l., Huang, J-w., & Xu, Y. (2013). Cross-cultural difference and validation of the Chinese version of Montreal Cognitive Assessment in older adults residing in Eastern China: Preliminary findings. Archives of Gerontology and Geriatrics, 56(1), 38–43. https://doi.org/10.1016/j.archger.2012.05.008
- Husein, N., Lumempouw, S. F., & Ramli, Y. (2010). Montreal Cognitive Assessment Versi Indonesia (Moca-Ina) Untuk Skrining Gangguan Fungsi Kognitif. Neurona.
- Julayanont, P., Brousseau, M., Chertkow, H., Phillips, N., & Nasreddine, Z. S. (2014). Montreal Cognitive Assessment Memory Index Score (MoCA‐MIS) as a predictor of conversion from mild cognitive impairment to Alzheimer’s disease. Journal of the American Geriatrics Society, 62(4), 679–684.
- Kesler, S. R., Adams, H. F., Blasey, C. M., & Bigler, E. D. (2003). Premorbid intellectual functioning, education, and brain size in traumatic brain injury: An investigation of the cognitive reserve hypothesis. Applied Neuropsychology, 10(3), 153–162. https://doi.org/10.1207/S15324826AN1003_04
- Kosmidis, M. H., Vlahou, C. H., Panagiotaki, P., & Kiosseoglou, G. (2004). The verbal fluency task in the Greek population: Normative data, and clustering and switching strategies. Journal of the International Neuropsychological Society, 10(2), 164–172. https://doi.org/10.1017/s1355617704102014
- Le, T. Y. P., & Tran, C. T. (2017). Suy giảm nhận thức sau chấn thương sọ não. Nghiên Cứu Y Học, 21(2), 217–222.
- Lee, J.-Y., Cho, S.-J., Na, D. L., Kim, S.-K., Youn, J.-H., Kwon, M., Lee, J.-H., Dong, W. L, Hong, J. J., You, R. L., & Maeng, J. C. (2008). Brief screening for mild cognitive impairment in elderly outpatient clinic: Validation of the Korean version of the Montreal Cognitive Assessment. Journal of Geriatric Psychiatry and Neurology, 21(2), 104–110., https://doi.org/10.1177/0891988708316855
- Leggett, A., Zarit, S. H., Hoang, C. N., & Nguyen, H. T. (2013). Correlates of cognitive impairment in older Vietnamese. Aging & Mental Health, 17(8), 915–923. https://doi.org/10.1080/13607863.2013.799116
- Li, J., & Yu, J. (2012). P-1023-A Chinese version of Montreal cognitive assessment as a brief screening tool for mild cognitive impairment: A population-based study. European Psychiatry, 27, 1. https://doi.org/10.1016/S0924-9338(12)75190-8
- Lu, J., Li, D., Li, F., Zhou, A., Wang, F., Zuo, X., Jia, X.-F., Song, H., & Jia, J. (2011). Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: A population-based study. Journal of Geriatric Psychiatry and Neurology, 24(4), 184–190. https://doi.org/10.1177/0891988711422528
- Moafmashhadi, P., & Koski, L. (2013). Limitations for interpreting failure on individual subtests of the Montreal Cognitive Assessment. Journal of Geriatric Psychiatry and Neurology, 26(1), 19–28.
- Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., Cummings, J. L., & Chertkow, H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699.
- Ng, A., Chew, I., Narasimhalu, K., & Kandiah, N. (2013). Effectiveness of Montreal Cognitive Assessment for the diagnosis of mild cognitive impairment and mild Alzheimer’s disease in Singapore. Singapore Medical Journal, 54(11), 616–619. https://doi.org/10.11622/smedj.2013220.
- Ngo, A. D., Rao, C., Phuong Hoa, N., Hoy, D. G., Thi Quynh Trang, K., & Hill, P. S. (2012). Road traffic related mortality in Vietnam: Evidence for policy from a national sample mortality surveillance system. BMC public Health, 12(1), 561–569. https://doi.org/10.1186/1471-2458-12-561
- Nguyen, T.-N., Chen, S., Chan, K., Nguyen, M. T., & Hinton, L. (2022). Cognitive functioning and nail salon occupational exposure among Vietnamese immigrant women in Northern California. International Journal of Environmental Research and Public Health, 19(8), 4634. https://doi.org/10.3390/ijerph19084634
- Nguyen, T. X. L., & Tran, C. T. (2017). Đánh giá thang MoCA trong tầm soát suy giảm nhận thức ở người Việt Nam. Nghiên Cứu Y Học, 21(2), 210–215.
- Ponsford, J. (2017). International growth of neuropsychology. Neuropsychology, 31(8), 921–933. https://doi.org/10.1037/neu0000415
- Quang, H., Kumfor, F., Balleine, B., Nguyen, T. V., Nguyen, T. Q., Nguyen, M. N., & McDonald, S. (2022). Contributions of intrinsic and extrinsic reward sensitivity to apathy: Evidence from traumatic brain injury. Neuropsychology, 36(8), 791–802. https://doi.org/10.1037/neu0000858
- Quang, H., McDonald, S., Huynh-Le, P., Nguyen, T.-V., Le, N.-A., Lam-Nguyen, N.-T., & Kumfor, F. (2022). Apathy in a high prevalence population of moderate to severe traumatic brain injury. An investigation in Vietnam: Neuropsychology, 36(1), 94. https://doi.org/10.1037/neu0000781
- Quang, H., Sin, K., Kumfor, F., & McDonald, S. (2022). Adaptation, validation and preliminary standardisation of the frontal systems behaviour scale–apathy subscale and the dimensional apathy scale in Vietnamese healthy samples. Journal of the International Neuropsychological Society: JINS, 28(3), 300–310. https://doi.org/10.1017/S135561772100031X
- Reitan, R. M., & Wolfson, D. (1995). Category test and trail making test as measures of frontal lobe functions. The Clinical Neuropsychologist, 9(1), 50–56. https://doi.org/10.1080/13854049508402057
- Siciliano, M., Chiorri, C., Battini, V., Sant’Elia, V., Altieri, M., Trojano, L., & Santangelo, G. (2019). Regression-based normative data and equivalent scores for Trail Making Test (TMT): An updated Italian normative study. Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology, 40(3), 469–477. https://doi.org/10.1007/s10072-018-3673-y
- Siedlecki, K. L., Manly, J. J., Brickman, A. M., Schupf, N., Tang, M.-X., & Stern, Y. (2010). Do neuropsychological tests have the same meaning in Spanish speakers as they do in English speakers? Neuropsychology, 24(3), 402–411. https://doi.org/10.1037/a0017515
- Spitz, G., Ponsford, J. L., Rudzki, D., & Maller, J. J. (2012). Association between cognitive performance and functional outcome following traumatic brain injury: A longitudinal multilevel examination. Neuropsychology, 26(5), 604–612. https://doi.org/10.1037/a0029239
- Tran, B., Nguyen, A. T., Ba, C., & Nguyễn, C. M. (2022). Neuropsychological assessment of Vietnamese Americans. In Cultural Diversity in Neuropsychological Assessment (pp. 298–311). Routledge.
- Vogel, S. J., Banks, S. J., Cummings, J. L., & Miller, J. B. (2015). Concordance of the Montreal cognitive assessment with standard neuropsychological measures. Alzheimer’s & Dementia (Amsterdam, Netherlands), 1(3), 289–294. https://doi.org/10.1016/j.dadm.2015.05.002
- Vu, H. M., Dang, A. K., Tran, T. T., Vu, G. T., Truong, N. T., Nguyen, C. T., Doan, A. V., Pham, K. T. H., Tran, T. H., & Tran, B. X. (2019). Health-related quality of life profiles among patients with different road traffic injuries in an urban setting of Vietnam. International Journal of Environmental Research and Public Health, 16(8), 1462. https://doi.org/10.3390/ijerph16081462
- Vu, H. M. D. (2021). Kết quả điều trị chấn thương sọ não nhẹ tại bệnh viện đa khoa tỉnh thái bình. Tạp chí Y học Việt Nam, 503(2), 36–39.
- Wechsler, D. (2008). WAIS-IV: Administration and scoring manual. The Psychological Corporation.