Abstract
Objectives: Growing number of patients with terminal heart failure and a shortage of heart donors have increased use of short- and long-term mechanical circulatory support (MCS). Few studies have analyzed survival rates and healthcare costs for heart transplantation (HTx), with or without extracorporeal membrane oxygenation (ECMO) and left ventricular assist device (LVAD).
Design: In a retrospective, single-center study, data were analyzed from patients listed for HTx who died on the waiting list (DWL, n = 12), underwent HTx (n = 206), had ECMO as bridge to HTx (ECHTx, n = 15), or received LVAD treatment, either isolated (LVAD, n = 19) or bridging to HTx (LVADHTx, n = 26) during 2005–2012. Survival and hospital costs were assessed.
Results: One- and five-year survival rates were 96% and 83% for the LVADHTx group, 92% and 81% for HTx, 70% and 70% for ECHTx, 48% and 36% for LVAD and 0% for the DWL group (overall survival, p < 0.001). Total hospital cost at one year was $102,101 ± 202,604 for DWL, $151,685 ± 86,892 for HTx, $292,078 ± 101,915 for ECHTx, $427,337 ± 365,154 for LVAD, and $600,897 ± 198,109 for LVADHTx.
Conclusion: The LVADHTx and HTx groups showed excellent one- and five-year survival. The combined group of DWL and HTx patients had similar survival to the combined groups of MCS, but use of LVAD pre-transplant quadrupled the cost.
Introduction
Heart failure (HF) remains a major health problem worldwide. Indeed, the incidence of HF and associated mortality has increased over the last three decades. One-year survival following end-stage HF, even with modern medical and electrical device therapy, is only in the range 10–25%.[Citation1] Heart transplantation (HTx) is an established treatment for a selected group of patients, but its use is restricted by the shortage of suitable donors.[Citation2] Extracorporeal membrane oxygenation (ECMO) and implantable long-term left ventricular assist device (LVAD) therapy offer short- or long-term treatment options in the management of end-stage HF.[Citation3,Citation4]
Survival and cost analyses have compared HTx versus LVADs as a bridge to transplant (BTT). LVAD is less cost-effective than HTx mainly due to the high acquisition costs and short duration of use.[Citation5–8] However, few published reports have compared HTx, ECMO or LVAD treatment (either ongoing or followed by HTx) in the context of refractory, life-threatening HF.[Citation9] The main objective of the current analysis was to assess short- and long-term survival, hospital length of stay and costs associated with different strategies for cardiac replacement therapy at a single center.
Materials and methods
Patients
Following approval from the institutional review board at Oslo University Hospital, data were obtained from medical records in the center’s HTx, ECMO and LVAD database. All patients accepted by a multidisciplinary heart team as HTx candidates from January 2005 (the start of the continuous flow LVAD program) to December 2012 were included. Since the only indication for LVAD was BTT, all LVAD recipients were on the HTx waiting list. Patients were divided into five groups: (1) patients who died on the HTx waiting list (DWL) either at home or in hospital (including ECMO patients); (2) patients who had HTx surgery after optimal medical management, including intra-aortic balloon pump (IABP) support (HTx); (3) patients in cardiogenic shock who received successful ECMO as a bridge to urgent HTx (ECHTx); (4) patients with ongoing LVAD awaiting HTx; (5) LVAD patients with a successful BTT (LVADHTx).
From 2005 to 2009, the Ventracor® (Sydney, Australia) device was used in 20 patients. Subsequently, the HeartWare LVAD® (Fremingham, MA) device was used in 25 patients. After LVAD implantation, a three-month recovery period was required before re-listing for HTx. Patients in need of IABP as circulatory support were not analyzed separately since the use and costs of IABP were integrated into the DWL, HTx, ECHTx, LVAD and LVADHTx groups.
Hospitalization costs
The costs were calculated only for our hospital patients and divided into the following periods: (1) On waitlist for HTx or the pre-implant period for LVAD, including ECMO therapy and hospitalization after acceptance to HTx. This pre-surgical period included all costs for our hospital for the last three months before intervention. (2) The surgical stay from date of HTx or LVAD implantation until discharge or in-hospital death. Costs in this period included organ procurement, transportation and staff costs, the device purchase cost, and costs related to the outpatient management facility or intensive care costs for patients who died on the waiting list. (3) The follow-up or post-surgical period. This was defined as the date of discharge to either death or the end of 2013, the censoring point for survivors which allowed a minimum of one year’s follow-up for all the patients. For patients on LVAD who underwent HTx, costs associated with the period pre-HTx were also calculated, as well as a second follow-up period.
For each defined time period, costs were summarized as the total cost per patient. Patient-level costs were based on clinical pathways identified through the hospital patient administrative systems. Costs were calculated by a two-step procedure. First, unit costs for healthcare personnel (i.e. a nursing hour), procedures and items were calculated along each clinical pathway. Unit costs included overhead costs. Second, the unit cost was multiplied by the patient’s length of hospital stay at different stages of the clinical pathway or by the number of items used, then summed up to obtain the total patient cost. For a detailed description of methods, see Mishra et al.[Citation10] Resources used for IABP treatment were included in the costs for each patient group. ECMO resources used in DWL and LVAD group patients were included in the two groups.
The cost evaluation was undertaken from the center’s perspective, such that costs from outside the hospital (other hospitals, primary care, etc.) were not included. For the first year after surgery, post-procedural costs included all readmission and outpatient visits. In the absence of cost data for subsequent years, a standard resource package based on our institute medical practice was calculated in order to determine the costs of resources used per patient to last follow-up. The HTx patient group resource package included the cost of outpatient visits, heart biopsies, invasive studies and immunosuppressive drugs. The postoperative course for all LVAD and HTx patients included a stay in an outpatient facility close to the hospital, until they were physically and mentally capable of self-care at home. The length of stay in this facility was included in the total hospital stay. A 24/7 VAD coordinator or VAD/transplant physician responded to all contact from patients or local healthcare providers.
Cost and survival analyses were performed for patients surviving to one, three, five and seven years.
All costs were inflated to 2012 prices by the consumer price index, and converted to $using an exchange rate of $1 to 5.8 Norwegian kroner. demonstrates unit costs as well as device costs.
Table 1. Unit cost.
Statistical analysis
Survival analyses are presented as Kaplan–Meier plots and as absolute rates. Survival was defined as freedom from death from the date of intervention until study end.
SPSS for Windows (release 21.0 SPSS inc. Chicago, IL) was used for statistical analysis. Data are presented as mean ± SD unless stated otherwise.
Results
Patient population
In total, 278 patients were included in the study. Patient demographics and baseline characteristics are shown in . The majority of patients were male, and dilated cardiomyopathy was the most frequent diagnosis for the cause of end-stage HF. Patients in the DWL, ECHTx and LVADHTx groups were younger compared to the HTx and LVAD groups. In the DWL group, 67% had undergone previous cardiac surgery (including three patients listed for re-HTx and two on ECMO treatment), compared to 28%, 26%, 11% and 12% in the HTx, ECHTx, LVAD and LVADHTx groups, respectively. The patients were all followed for a minimum of one year, and a maximum of seven years.
Table 2. Demographics and baseline characteristics according to the patient group.
The mean number of days on ECMO support was 9.1 ± 8.5 in the ECHTx group compared to 6.7 ± 4.2 days in the LVADHTx group and 23 days in the only patient on ECMO in the LVAD group. Of the 45 LVAD patients, 11 were on ECMO, one assisted by Impella (12 patients INTERMACS I) and 26 on IABP (26 patients INTERMACS II) with an additional five patients INTERMACS III and three patients INTERMACS IV consistent with a critically ill group before implantation. The mean duration of LVAD support was 384 ± 615 days for the LVAD group and 219 ± 157 days for the LVADHTx group.
Length of hospital stay and time to HTx
Patients on LVAD had double the length of total hospital stay and time in the intensive care unit compared to HTx recipients (). The DWL group spent a mean of 46 days in hospital, including 25 days in the intensive care unit, indicating substantial use of resources before death.
Table 3. Length of hospital stay and mortality according to patient group.
The time interval from day of waitlisting to HTx was 87 ± 104 days for the HTx group and 39 ± 85 for the ECHTx group including 8 ± 7 days on ECMO. For the LVADHTx group, the waiting time from LVAD to HTx was 219 ± 157 days (including 90 days recovery before re-listing).
Survival and cause of death
One-year survival was highest in the LVADHTx and HTx groups, 96% and 92% respectively, including excellent long-term survival (, ). At seven years, survival in the ECHTx group approached that of these two groups (LVADHTx 83%, HTx 77%, ECHTx 70%). Nine of the 45 LVAD patients died during follow-up, three patients were converted from BTT to destination therapy and seven remained on LVAD as BTT at the end of follow-up. Patients who remained on LVAD without HTx had inferior short-term survival, while overall successful BTT or ongoing LVAD for all 45 LVAD patients was 80% at the end of the study period. shows the survival for those patients transplanted from LVAD and for those ongoing, either as waiting for HTx or converted to destination due to LVAD complications. For all the patients on MCS five-year survival rate was 70%. Pooled data from the DWL and HTx groups with optimal medical management versus pooled data for all the patients who received MCS with or without HTx (i.e. the ECHTx, LVADHTx and LVAD groups) showed no significant survival difference (p = 0.80) (). summarizes the cause of death in each group in the first 30 days, or more than 30 days, after listing or procedures. In the DWL group, 75% of the patients died of sudden cardiac death, mostly caused by arrhythmia and irreversible cardiogenic shock, even though nine of the 12 patients had an implanted defibrillator, with a further two patients on ECMO and one on IABP. In the HTx group, the most frequent causes of death within the first 30 days post-transplant were primary graft failure and multi-organ failure, which were often interrelated. The reasons for late mortality post-HTx were graft dysfunction, presenting either as verified coronary allograft vasculopathy or sudden death of unknown etiology. For the LVAD group, both short- and long-term multi-organ failure was the most frequent cause of death.
Figure 1. Actuarial survival according to the patient group. DWL: died on waiting list; ECHTx: ECMO as a bridge to urgent HTx; HTx: heart transplantation; LVAD: left ventricular assist device; LVADHTx: left ventricular assist device as bridge to HTx.
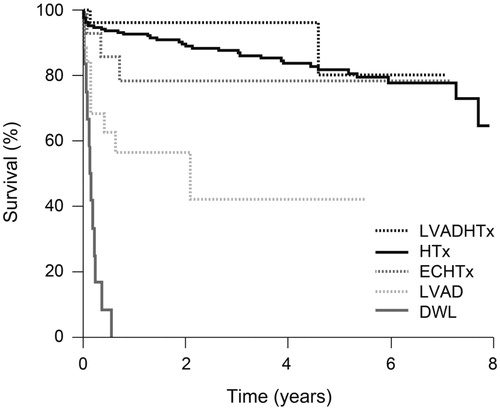
Figure 2. Pooled actuarial survival for death on the HTx waiting list and heart transplantation versus mechanical circulatory support. DWL: died on waiting list; ECHTx: ECMO as a bridge to urgent HTx; HTx: heart transplantation; LVAD: left ventricular assist device; LVADHTx: left ventricular assist device as bridge to HTx.
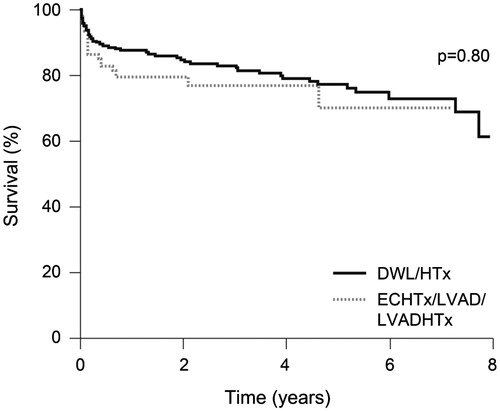
Table 4. Cause of death data according to patient group <30 days or >30 days after listing or procedure, n.
Hospital costs
The total hospital cost per patient within the first year after listing, including pre-listing studies and examinations, was $102,101 ± 202,604 for the DWL group, $151,685 ± 86,892 for the HTx group, $292,078 ± 101,915 for the ECHTx group, $427,337 ± 365,154 for the LVAD group and $600,897 ± 198,109 for the LVADHTx group. For both the HTx and ECHTx groups, costs increased over time (). For the long-term LVAD survivors, either as ongoing or LVADHTx patients, a high LVAD acquisition cost was spread over time ().
Table 5. Costs to one, three, five and seven years according to patient group.
The contribution of different time periods to the total one-year cost is presented in . Within the DWL group, costs pre- and post-listing contributed to 14% and 86% of the total cost, respectively. In the HTx group, the pre-transplant costs, transplant procedure and post-transplant follow-up accounted for 5%, 87% and 8%, respectively, of total costs. For the ECHTx group, the pre-transplant treatment, HTx and follow-up contributed to 53%, 38% and 9%, respectively, of total costs. For LVAD patients, the pre-implant period, LVAD implant and follow-up contributed to 23%, 75%, 2% respectively, of total costs. The pre-implant phase high costs were associated with use of IABP/ECMO, with ECMO costs calculated at $15,000/day (). IABP treatment costs in the intensive care unit/coronary care unit are less than 10% of the ECMO costs and we have therefore included IABP in the intensive care unit costs.
Figure 3. Mean total cost per patient during year 1 according to the patient group. DWL: died on waiting list; ECHTx: ECMO as bridge to urgent HTx; HTx: heart transplantation; LVAD: left ventricular assist device; LVADHTx: left ventricular assist device as bridge to HTx; pts: patients; VAD: ventricular assist device.
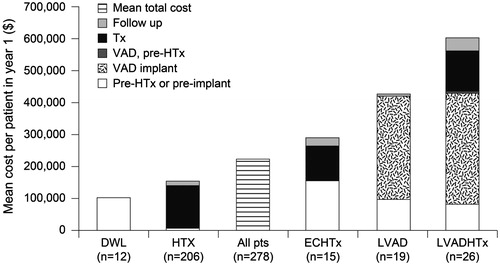
For LVADHTx, the total cost made up 13%, 57%, 1%, 22% and 7% of costs associated with the pre-LVAD period, the LVAD implantation period, post-LVAD follow-up, the HTx procedure and follow-up post-HTx, respectively. The device cost contributed to 54% of the total cost in the LVAD implantation period. For the combined total of 218 patients in the DWL (n = 12) and HTx (n = 206) groups, the mean total cost per patient at one year was $165 099 ± 107,478 compared to $557,700 ± 212,262 for the groups receiving MCS as BTT. Overall, the mean one-year cost per patient for all the patients in the program was $222,496 + 157,211 ().
Discussion
Successful management of end-stage HF centers depends on careful patient selection and timing of possible interventions using the available resources. At our center, the majority of patients are hemodynamically stable and receiving optimal medical management or IABP treatment while waiting approximately three months for HTx. With a successful IABP program, patients are bridged to HTx if hemodynamically stable and only patients deteriorating on IABP have a LVAD implanted. The aim of HTx and LVAD is to extend survival and regain quality of life. HTx is still the preferred treatment due to superior long-term results, although the side effects of immunosuppression are well known.[Citation11–15] The organ donation rate in Norway is satisfactory (21 per 1000), and during the study period the annual HTx rate was seven per million of the population. This HTx rate and the relatively short waiting time favor deferring MCS if possible. It is challenging, however, to identify patients who are likely to deteriorate or develop multi-organ failure with or without the use of IABP and thus become poor candidates for HTx or LVAD.
In this analysis, both HTx and LVADHTx were associated with excellent short- and long-term survival rates. However, need for LVAD before successful HTx increased costs four-fold compared to HTx without previous LVAD. A low proportion of patients died while on the waiting list for HTx: the DWL comprised only 4.3% of patients, including the death of two DWL patients on ECMO. In the DWL group, sudden cardiac death was the primary reason for mortality even though 75% of the patients had an implantable cardioverter-defibrillator. In severe HF, rhythm conversion is often inadequate and leads to hemodynamic collapse that is difficult to prevent. During the study period, LVAD treatment included a long pre-implant phase with high costs that included IABP/Impella treatment or ECMO in 38 out of 45 patients, classified as INTERMACS I or II, compared to the 75% of the patients who were treated with HTx as the primary intervention. Kirklin et al. report one-year LVAD survival of 80% in a mixed population of patients, including high-risk INTERMACS I patients similar to our LVAD cohort.[Citation16] In our study, a high proportion of the patients going directly to HTx indicates LVAD for those deteriorating to a lower INTERMACS class and affecting survival, a strategy that depends on an acceptable waiting time for HTx. Theoretical models have estimated survival rates for end-stage HF.[Citation17,Citation18] Similar to our findings, these models confirm that optimal medical management is insufficient for patients with the most severe HF. They also demonstrate that BTT survival depends on the waiting time, as observed in our HTx group. Droogne et al. postulated that hypothetical models often underestimate survival since life-saving LVAD is frequently introduced.[Citation17] Most of these studies were carried out in centers where the waiting time for HTx is unacceptably long. The benefits of ECMO and short-term MCS for severe respiratory and cardiac failure has been reported over the last decade as a bridge to HTx or LVAD implantation.[Citation3,Citation4] Although some patients can be weaned from MCS as a bridge to recovery, mortality remains high for ECMO. However, if HTx can be undertaken quickly, the five-year survival of 70% observed in our series is reasonable and justifies the use of ECMO in critically ill patients who can be stabilized before HTx.[Citation16] It should be noted, however, that our analysis did not include an unknown number of ECMO patients who were never listed for HTx due to unsuccessful ECMO treatment, complications, or ineligibility for HTx.
Cost analyses have demonstrated that LVAD treatment is not cost effective due to high device costs and the need for short-term support while on LVAD, [Citation5,Citation6] consistent with the current analysis. Importantly, Clarke et al. state that LVAD cost begins to approach the cost for recommended end-of-life care, estimated to exceed $150,000/year.[Citation7] The mean cost of LVAD devices at our center was $186,000 – including mean device cost of $154,000 – and an accessories cost of $32,000 (). Our center device costs are 45% higher than reported by Clarke, but whether the data includes costs for accessories, the type of device or higher profit margins in Norway is not known. Comparable centers report similar device costs, but they are not comparable to high volume European and American centers.[Citation19–21] However, increasing experience in our LVAD program has lowered the total costs per procedure by 12% over time.[Citation10]
A study by Giorgi et al. [Citation22] reported that the overall cost for LVAD treatment exceeded that of HTx over a 123-day period (LVAD $197,957, HTx $151,646), largely due to differences in the initial hospital stay and greater severity of illness in the LVAD patients. First-year LVAD costs of approximately $200,000 have also been reported by Mulloy et al.[Citation23] In our series 16% of the HTx group received LVAD pre-transplant, which increased total costs. Improved long-term results in the LVADHTx group would distribute costs over an extended survival period post-HTx, narrowing the cost gap versus HTx alone.
In contrast to our ECMO costs of $15,000/day, Maxwell et al. report charges for ECMO treatment of $40,000/day. In their analysis, the duration of ECMO was twice as long as in our cohort,[Citation24] although this difference may be biased by including only patients eligible for HTx or LVAD in our group of ECMO patients.
Previous studies have considered the costs for HTx and LVAD.[Citation8,Citation9] Our study aimed to address these issues in addition to length of stay and survival in the era of increasingly limited organ availability and hospital resources for the growing number of patients with end-stage HF. The number of LVAD patients in our series cohort is limited compared to larger European and American centers but our strategy of performing HTx within a reasonable time, using LVAD or ECMO as BTT for patients deteriorating on optimal medical management, has led to improved patient survival in our patient population.
A transplant/VAD center must take into account the total cost of the program, not only the costs and outcomes associated with each separate treatment modality. This overall cost inevitably exceeds that of successful transplantation in stable patients who do not need advanced MCS (). In our center we have a long and successful tradition of using IABP as a bridge to HTx, a strategy that shows good results and significantly lower costs compared to those who deteriorate and thus need a LVAD.[Citation25,Citation26] Accordingly, our strategy is – and will continue to be – to bridge as many patients as possible with IABP, and use LVAD for those who are hemodynamically unstable, have antibodies, or large body mass etc., or who are in the category “bridge to decision”. The implication of this strategy is that a larger proportion of patients are transplanted from IABP and a smaller proportion of patients transplanted from LVAD. Both categories have a long pre-transplant period with or without LVAD. The costs to our LVAD program are therefore increased because of a long and expensive pre-implant phase including ECMO, but the total program costs are reduced by bridging a large proportion of patients to HTx using a low-cost IABP treatment. For some LVAD patients who deteriorate on IABP, the implant should ideally be performed earlier and the post-LVAD period prolonged due to lower INTERMACS class.
Limitations of this study include the cost estimation from the hospital perspective, retrospective, single-center design with limited patient numbers, and the fact that initial diagnostic work-up and follow-up were carried out at local hospitals. Notably, we have only included costs acquired at our hospital. For all LVAD patients all costs were registered prospectively, but for the other groups costs were estimated retrospectively. Although the analysis included a detailed calculation of costs incurred by the transplant center, the management strategy for end-stage HF at our center is influenced by satisfactory donor availability, but waiting list and donation policies can vary from one country to another and thus the conclusions may not be valid in other countries where the waiting time for HTx is longer. We have focused on the survival and total costs of the treatment, and not considered the obvious improvement of quality of life which by itself might support use of significant resources irrespective of thr treatment group in our study.
Conclusions
In this analysis of outcomes and costs associated with all the treatment modalities for the end-stage HF, LVADHTx and HTx both resulted in excellent one-year survival rates but use of LVAD pre-transplant quadrupled the cost. Patients managed with ECHTx experienced lower early survival than LVADHTx or HTx, at twice the cost of HTx, but late survival approached that of the other two groups. LVAD implantation in critically ill patients had a success rate of 80%. In the population as a whole, survival in patients with MCS did not differ significantly to that of patients on optimal medical management awaiting HTx.
Funding information
The study received no external funding.
Disclosure statement
None of the authors has any conflict of interest to declare. Arnt Fiane, Einar Gude and Gro Sørensen provide LVAD courses, which are partly financed by HeartWare International, Inc., but the content of the course reflects the independent view of the lecturers.
References
- Rathi S, Deedwania PC. The epidemiology and pathophysiology of heart failure. Med Clin North Am. 2012;96:881–890.
- Stehlik J, Edwards LB, Kucheryavaya AY, et al. The registry of the international society for heart and lung transplantation: twenty-seventh official adult heart transplant report. J Heart Lung Transplant. 2010;29:1089–1103.
- Sauer CM, Yuh DD, Bonde P. Extracorporeal membrane oxygenation use has increased by 433% in adults in the United States from 2006 to 2011. Asaio J. 2015;61:31–36.
- Stretch R, Sauer CM, Yuh DD, et al. National trends in the utilization of short-term mechanical circulatory support: incidence, outcomes, and cost analysis. J Am Coll Cardiol. 2014;64:1407–1415.
- Moskowitz AJ, Rose EA, Gelijns AC. The cost of long-term LVAD implantation. Ann Thorac Surg. 2001;71:S195–S198.
- Beyersdorf F. Economics of ventricular assist devices: European view. Ann Thorac Surg. 2001;71:S192–S194.
- Clarke A, Pulikottil-Jacob R, Connock M, et al. Cost-effectiveness of left ventricular assist devices (LVADs) for patients with advanced heart failure: analysis of the British NHS bridge to transplant (BTT) program. Int J Cardiol. 2014;171:338–345.
- Stehlik J, Stevenson LW, Edwards LB, et al. Organ allocation around the world: insights from the ISHLT international registry for heart and lung transplantation. J Heart Lung Transplant. 2014;33:975–984.
- Owens AT, Jessup M. Should left ventricular assist device be standard of care for patients with refractory heart failure who are not transplantation candidates?: left ventricular assist devices should not be standard of care for transplantation-ineligible patients. Circulation. 2012;126:3088–3094.
- Mishra V, Geiran O, Fiane AE, et al. Costs and reimbursement gaps after implementation of third-generation left ventricular assist devices. J Heart Lung Transplant. 2010;29:72–78.
- Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361:2241–2251.
- Petrucci RJ, Wright S, Naka Y, et al. Neurocognitive assessments in advanced heart failure patients receiving continuous-flow left ventricular assist devices. J Heart Lung Transplant. 2009;28:542–549.
- Kamouh A, John R, Eckman P. Successful treatment of early thrombosis of HeartWare left ventricular assist device with intraventricular thrombolytics. Ann Thorac Surg. 2012;94:281–283.
- Topkara VK, Kondareddy S, Malik F, et al. Infectious complications in patients with left ventricular assist device: etiology and outcomes in the continuous-flow era. Ann Thorac Surg. 2010;90:1270–1277.
- Frazier OH, Rose EA, Oz MC, et al. Multicenter clinical evaluation of the heartmate; vented electric left ventricular assist system in patients awaiting heart transplantation. J Heart Lung Transplant. 2001;20:201–202.
- Kirklin JK, Naftel DC, Pagani FD, et al. Long-term mechanical circulatory support (destination therapy): on track to compete with heart transplantation? J Thorac Cardiovasc Surg. 2012;144:584–603.
- Droogne W, Jacobs S, Van den Bossche K, et al. Cost of 1-year left ventricular assist device destination therapy in chronic heart failure: a comparison with heart transplantation. Acta Clin Belg. 2014;69:165–170.
- Kirklin JK, Mehra MR. The dawn of the ISHLT mechanical assisted circulatory support (IMACS) registry: fulfilling our mission. J Heart Lung Transplant. 2012;31:115–116.
- Vanden Eynden F, Antoine M, El Oumeiri B, et al. How to cope with a temporarily aborted transplant program: solutions for a prolonged waiting period. Ann Transl Med. 2015;3:306.
- Pulikottil-Jacob R, Suri G, Connock M, et al. Comparative cost-effectiveness of the HeartWare versus HeartMate II left ventricular assist devices used in the United Kingdom National health service bridge-to-transplant program for patients with heart failure. J Heart Lung Transplant. 2014;33:350–358.
- Karason K, Dellgren G, Redfors B, et al. Left Ventricular Assist Device as permanent support in patients with terminal heart failure. Göteborg: Västra Götalandsregionen, Sahlgrenska Universitetssjukhuset, HTA-centrum; 2014. Regional activity-based HTA 2014:66
- Digiorgi PL, Reel MS, Thornton B, et al. Heart transplant and left ventricular assist device costs. J Heart Lung Transplant. 2005;24:200–204.
- Mulloy DP, Bhamidipati CM, Stone ML, et al. Orthotopic heart transplant versus left ventricular assist device: a national comparison of cost and survival. J Thoracic Cardiovasc Surg. 2013;145:566–573.
- Maxwell BG, Powers AJ, Sheikh AY, et al. Resource use trends in extracorporeal membrane oxygenation in adults: an analysis of the Nationwide inpatient sample 1998-2009. J Thorac Cardiovasc Surg. 2014;148:416–421.
- Gjesdal O, Gude E, Arora S, et al. Intra-aortic balloon counterpulsation as a bridge to heart transplantation does not impair long-term survival. Eur J Heart Fail. 2009;11:709–714.
- Lahpor J, Khaghani A, Hetzer R, et al. European results with a continuous-flow ventricular assist device for advanced heart-failure patients. Eur J Cardiothorac Surg. 2010;37:357–361.
