Abstract
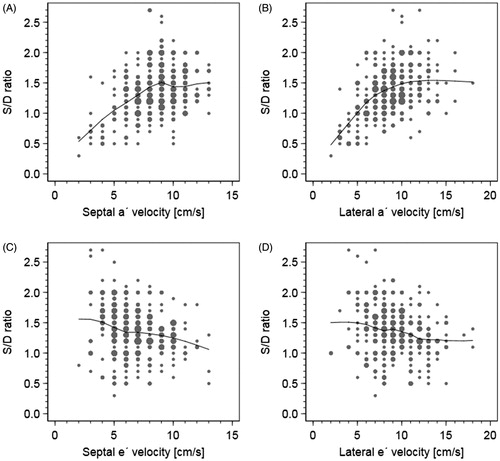
Objectives. To compare the ability of the a´ velocity and the e´ velocity in predicting a dominant diastolic pulmonary vein flow (S/D ratio <1) in patients with normal ejection fraction. Design. We retrospectively evaluated the diastolic function according to the ASE/EACVI guidelines, the S/D ratio and the septal, lateral and average a´ velocity in 293 unselected in-hospital patients, aged 39–86 years, in sinus rhythm and with no or mild valve disease, having a normal systolic function (EF >50%). Results. There was a good linear correlation between the S/D ratio and the a´ velocity, but a tendency towards a negative correlation between the S/D ratio and the e´ velocity. S/D ratio <1 was seen in 43 patients. These patients had a significantly lower a´ velocity compared to those with S/D-ratio ≥1, septal (6,1 ± 2,4 v 8,8 ± 2,1 cm/s; p < .001) and lateral (6,0 ± 2,6 v 9,3 ± 2,5 cm/s; p < .001) No significant difference was seen in the septal e´ velocity (6,8 ± 2,4 v 6,8 ± 2,1 cm/s), lateral e´ velocity (9,4 ± 2,6 v 9,1 ± 2,8 cm/s) or in the ejection fraction (58,6 ± 4,4% v 58,7 ± 4,0%). A diastolic dysfunction was present in 62 patients, normal diastolic function in 231 patients. The a´ velocity was significantly lower in patients with S/D ratio <1 in both groups (p < .01). Conclusion. The a´ velocity is superior to the e´ velocity in predicting S/D ratio <1 in patients with normal ejection fraction regardless the ASE/EACVI diastolic classification. A failing left atrium seems to be the explanation.
Introduction
Studies have shown that in patients with heart failure and a preserved systolic function, the presence of a dominant diastolic component in the pulmonary venous flow and a decreased left atrial contractile function could identify patients with an impaired clinical short and long-term outcome [Citation1–5]. Furthermore an isolated diastolic heart failure could be explained by an increased content of collagen and a changed regulation in the titin springs of the myocyte leading to a high end-diastolic left ventricular filling pressure in patients with significant coronary artery disease [Citation6]. These studies suggest that it would be of interest to try to elucidate the correlation between the LA contractile status and the pulmonary vein flow pattern and the hemodynamic correlation between the left atrial function and the S/D ratio especially when S/D ratio <1 is present. The current ASE/EACVI guidelines from 2016 [Citation7,Citation8] do not include the S/D ratio or any direct parameter reflecting the LA contractile status in their criteria of evaluating a diastolic dysfunction in patients with a normal ejection fraction. The a´ velocity in the tissue-Doppler is correlated to the left atrial contractile status [Citation9–11] and might be a reflector of the late LV diastolic phase. However the correlation between the a´ velocity and the S/D ratio has never been clarified in a study in patients with normal ejection fraction. Therefore the aim of the study was to compare the ability of the a´ velocity and the e´ velocity in identifying S/D ratio <1 in patients with a normal ejection fraction and suggest a hemodynamic explanation for this relation.
Method and material
Study group
This retrospective study included acute (90%) and elective patients (10%), totally 441 patients, who during the time period April 2011 to January 2016 underwent a clinically indicated complete echocardiographic examination in the department of physiology at Sundsvall Hospital, performed by one cardiologist (BJ), using the same echocardiographic system, where the major issue was left ventricular systolic or diastolic heart failure. The systolic ejection fraction could be evaluated in all patients but in order to evaluate the different diastolic parameters, the patient had to be in sinus rhythm and suffer from no more than a mild valve disease. Consequently, the exclusion criteria were: atrial fibrillation, atrial flutter and moderate or severe valve disease. A total of 113 patients had a decreased systolic function (EF ≤50%), twenty-three patients had atrial fibrillation and twelve patients had a significant valve disease and were excluded from the study. In 37 patients, suboptimal pulmonary vein flow signal was present and these patients were found in the patient groups with decreased ejection fraction, atrial fibrillation or a significant valve disease and these patients were excluded anyway. The remaining 293 patients (147 men; mean age 64,8 ± 12,4 years) had a normal systolic function (EF >50%), sinus rhythm and no or only mild valve disease and constituted the study group. The study protocol was approved by the ethics committee of Umeå University (Dnr 2016-209-31) and a written informed consent was obtained from all patients.
Echocardiographic system
The ultrasound system used for the echocardiographic examinations of the study group was a commercially available Philips iE33 ultrasound system, Philips Electronics, Netherlands using an S5-1 with 1–5 MHz transducer.
All measurements were performed using the incorporated calculation program in the ultrasound machine. The tissue velocity of the myocardium, the e´ velocity and the a´ velocity was measured (cm/s) just below the AV-plane in the 4-chamber view of the left ventricle in both the septal and lateral wall and the average e´ = (septal e´+ lateral e´)/2 and the average a´ = (septal a´ + lateral a´)/2 were calculated. The maximal velocity of the pulmonary vein inflow into the left atrium during systole (S) and diastole (D) was recorded (cm/s) and the S/D ratio was calculated.
Evaluation of the left ventricular function
The ejection fraction (EF) was used as a measure of the left ventricular systolic function. A normal systolic function was defined as EF >50% and a decreased systolic function was defined as EF ≤50% [Citation12]. The diastolic left ventricular function was defined in accordance with the current ASE/EACVI guideline algorithms from 2016 (6,7). The following criteria were used to characterize a diastolic dysfunction: average E/e´ > 14, septal e´ velocity <7 cm/s or lateral e´ velocity <10, TR velocity >2,8 m/s and LA volume index >34 ml/m2. Consequently, if a majority of these criteria were fulfilled, the patient was considered to have a diastolic dysfunction. S/D ratio <1 was considered decreased.
Reproducibility
High intra-observer and inter-observer correlation coefficients of 0,944–0,982 respective 0,927–0,983 between measurements for septal, lateral a´ velocity and the S/D ratio at two different occasions have been validated in an earlier study by our group [Citation13].
Statistics
Baseline characteristics were described with means, standard deviations, frequencies and relative frequencies. Differences in tissue velocities (lateral and septal a´, and lateral and septal e´ ) between groups based on the S/D ratio were analyzed with independent samples t-test, and the ability of each velocity to detect S/D < 1 were investigated with ROC curves and the area under the curve (AUC) with confidence intervals. Confidence intervals and test of AUC between septal e´ and septal a´, and between lateral e´ and lateral a´, were computed with the method earlier described [Citation14]. To illustrate the dependence between tissue velocities and S/D ratio we used scatter plots and non-parametric running line smoothers, Stata command running with standard bandwidth [Citation15]. All statistical analyses were made with Stata MP/4 15.0, using 95% confidence intervals and two-sided tests with significance level 0.05.
Results
The patients were stratified into two groups depending on S/D ratio ≥1 or <1 as illustrated in ). The baseline characteristics with this stratification are seen in and the assessment of the left ventricular systolic and diastolic variables are presented in . The correlation between the e´ velocity, a´ velocity and the S/D ratio both septal and lateral in all patients are presented in ). shows the ROC curves for the accuracy of a´ velocity and e´ velocity to detect S/D ratio <1, both septal and lateral in all patients with a normal ejection fraction. presents the results of the a´ velocity, e´ velocity both septal and lateral as well as the ejection fraction if patients are divided into two groups depending on the S/D ratio; patients with S/D ratio ≥1 (n = 250) and S/D ratio <1 (n = 43). In the same results are presented if the patients are divided into two groups according to the ASE/EACVI guidelines; patients with a normal diastolic function (n = 231) and a diastolic dysfunction (n = 62).
Figure 2. The ROC curves for the accuracy of a´ velocity and e´ velocity both septal and lateral to detect S/D ratio <1 in all patients with a normal ejection fraction (n = 293).
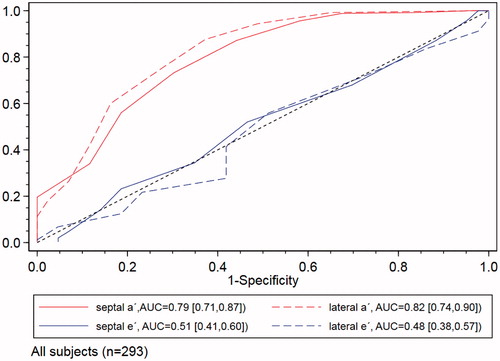
Figure 3. (A–H) Illustrations showing Doppler of mitral inflow, tissue-Doppler of both basal-septal LV and basal-lateral LV and Doppler of pulmonary vein flow for patients stratified for S/D ratio ≥1 (3A–D) and for patients with S/D ratio <1 (3E–H). Traces of mitral inflow, tissue-Doppler both septal and lateral and pulmonary vein flow in a patient with normal diastolic function and normal S/D ratio >1(A–D) and a patient with a grade II–III diastolic dysfunction and a decreased S/D ratio <1(E–H).
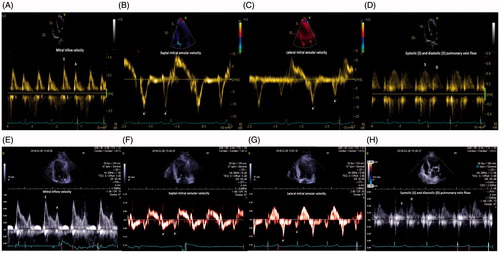
Table 1. Baseline characteristics of patients stratified for S/D ratio ≥1 or <1.
Table 2. Assessement of the left ventricular systolic and diastolic function in patients stratified for S/D ratio ≥1 or <1.
Table 3. The Results of the a´ velocity, e´ velocity and the ejection fraction in patients with S/D ratio ≥1 compared to S/D ratio <1.
Table 4. The Results of the a´ velocity, e´ velocity and the ejection fraction in patients with S/D ratio ≥1 compared to S/D ratio <1 in patients with a normal diastolic function or a diastolic dysfunction according to the ASE/EACVI guidelines.
As seen in , the patients with S/D ratio <1 had a highly significantly lower a´ velocity both septal and lateral compared to patients with S/D-ratio ≥1 but no significant difference was seen in the e´ velocity or in the ejection fraction between the two groups.
shows a highly significantly lower a´ velocity, septal and lateral in patients with S/D ratio <1 compared to those with S/D ratio ≥1, both in patients with an abnormal and a normal diastolic function according to the ASE/EACVI guidelines. The e´ velocity was significantly higher both septal and lateral in patients with S/D ratio <1 and a normal diastolic function. Lateral e´ velocity was also significantly higher in patients with S/D ratio <1 in the group with a diastolic dysfunction. The ejection fraction was not significantly different between patients with S/D ratio <1 compared those with S/D ratio ≥1 regardless if the diastolic function was normal or not.
Discussion
An isolated diastolic heart failure is reported in up to 50% of the patients with heart failure and is associated with a morbidity and mortality similar to systolic heart failure [Citation16–18]. Studies have shown that in patients with a preserved systolic function, the presence of a dominant diastolic component in the pulmonary venous flow (S/D ratio <1) and a decreased left atrial contractile function can identify patients with an impaired clinical short and long-term outcome [Citation1–5]. Furthermore an isolated diastolic heart failure in patients with significant coronary artery disease could be explained by an increased diastolic stiffness due to an increased amount of both collagen 1 and 3 and a changed regulation of the three different titin springs (tandem Ig segment, PEVK and N2B(A) bus) leading to a high left ventricular end-diastolic filling pressure [Citation6]. The current ASE/EACVI guidelines from 2016 [Citation7,Citation8] do not include the S/D ratio or any direct parameter reflecting the LA contractile status in their criteria of evaluating a diastolic dysfunction or an increased LV filling pressure in patients with a normal ejection fraction. The recently published invasive multicenter Euro-Filling study [Citation19] could not establish any significant correlation between the non-invasive echo estimates of LVFP compared to invasive measurements of left ventricular end diastolic pressure (LVEDP). In this study where 75% of the patients had a normal ejection fraction, only a weak correlation was found between the Doppler and the tissue-Doppler parameters and invasive LVEDP.
These results could suggest a need for further effort to elucidate the correlation between the late LV diastolic filling phase, the LA contractile status and the hemodynamic correlation to the S/D ratio in patients with a normal ejection fraction.
The a´ velocity in the tissue-Doppler is correlated to the left atrial contractile status [Citation9–11] and could be a better reflector of the late diastolic phase than the e´ velocity. The aim of this study was to investigate a possible relation between an impaired left atrial function, measured as decreased a´ velocity and S/D ratio <1 and suggest a hemodynamic explanation for this relation.
Our results show that there was a good linear correlation between the a´ velocity and the S/D ratio but a negative correlation between the e´ velocity and the S/D ratio in the entire group of patients with a normal ejection fraction. Furthermore there was a highly significant decrease in the a´ velocity, but not in the e´ velocity both septal and lateral in patients with S/D ratio <1 compared to patients with S/D ratio ≥1. Maybe even more interesting is that these results were found regardless the classification of the diastolic function according to the ASE/EACVI guidelines. How can our results be interpreted?
We suggest that the answer can be found in the development of a diastolic dysfunction. The first stage of a diastolic dysfunction, i.e an impaired relaxation is seen as a decreasing E-wave, an increasing A wave and an E/A ratio <1 in the mitral blood flow and a decreasing e´ velocity, an increasing a´ velocity in the tissue-Doppler [Citation10] and in this stage the LV mean filling pressure is usually still normal [Citation20]. The real problem starts when the left atrial contraction can no longer compensate for the progressively increasing diastolic stiffness in the left ventricle and the left atrial stroke volume can no longer be maintained [Citation21–23]. The left atrial forward failure which can be seen as a decreasing a´ velocity [Citation9,Citation10] leads to an increasing mean LA pressure and this parameter is strongly negatively correlated to the systolic pulmonary vein flow component, seen especially in patients with PCW pressure >15 mmHg [Citation24,Citation25]. Thus, the systolic (S) pulmonary vein flow into the LA will decrease due to a lowered pressure gradient between the pulmonary circulation and the LA but instead, the diastolic pulmonary vein flow (D) will increase as the E-wave velocity is rising due to the increased driving pressure from the LA to the LV during early diastole. The hemodynamic consequence is that the S/D ratio starts to fall and becomes increasingly lower as the diastolic dysfunction progresses and the LV and LA filling pressure increases and S/D ratio <1 will appear.
This scenario is supported by our study as, in contrast to the e´ velocity, there was both a good linear correlation between the a´ velocity and the S/D ratio generally and furthermore there was a highly significantly lower a´ velocity in patients with a S/D ratio <1 compared to S/D ratio ≥1 regardless if a normal or abnormal diastolic function was present according to the ASE/EACVI guidelines. These results suggest that a failing left atrium is strongly correlated to a decrease in the S/D ratio to <1 and furthermore hemodynamically could contribute to explain the occurrence of S/D ratio <1. Similar results was also found in a study by Banthit et al [Citation10] as the a´ velocity was decreased in patients with a severe diastolic dysfunction but the correlation to the S/D ratio was not investigated in that study. Our results suggest that left atrial dysfunction, represented by a falling a´ velocity may be helpful in identifying patients with heart failure and normal EF. A low a´ velocity appears to be a more robust and eligible sign of diastolic dysfunction compared to a low e´ velocity since normally the a´ velocity, in contrast to the e´ velocity, increases with age in patients without heart failure [Citation26].
An objection in the evaluation of a diastolic dysfunction in patients with a normal ejection fraction is that the downwards movement of the AV plane at LV contraction, could create a false high S/D ratio as a good LV suction leads to a higher systolic pulmonary vein flow component [Citation27]. However, the finding of S/D ratio <1 despite a good suction would rather increase the probability of an increased LA pressure. Hatle et others have shown that the main underlying factor for the systolic vein flow component is the LV filling pressure and the mean LA pressure, and only to a much lesser degree can be attributed to the LV systolic function [Citation24,Citation25,Citation27,Citation28]. This could support that S/D ratio <1 in our study really reflects an increased LV filling pressure in absence of invasive data.
Finally, why use the a´ velocity as a measurement of the left atrial function? We think that the a´ velocity is a very simple robust parameter eligible in all patients and in clinical practice more useful then more time consuming estimations of the left atrial function. Left atrial strain by two dimensional speckle tracking has recently been introduced as a promising method to categorize LV dysfunction in patients with preserved EF [Citation29] but this technique was not eligible in our study for comparison with the a´ velocity.
In summery
There is a strong correlation between the a´ velocity and the S/D ratio in patients with a normal ejection fraction regardless the classification of the diastolic function according to the ASE/EACVI guidelines. A failing left atrium may contribute to the development of S/D ratio <1 in patients with heart failure and normal EF.
Limitations of the study
There are several major limitations in this pilot study: This is a retrospective study. No invasive measurement of the LV filling pressure was performed. Furthermore we compared our results with a recommended but not so far validated ASE/EACVI algorithm. The a´ velocity is not an accepted parameter in the guidelines in this patient category and the results in this study must be confirmed in larger and if possible invasive studies.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ren X, Na B, Ristow B, et al. Usefulness of diastolic dominant pulmonary vein flow to predict hospitalization for heart failure and mortality in ambulatory patients with coronary heart disease (from the Heart and Soul Study)). Am J Cardiol. 2009;103:482–485.
- Buffle E, Kramarz J, Elazar E, et al. Added value of pulmonary venous flow Doppler assessment in patients with preserved ejection fraction and its contribution to the diastolic grading paradigm. Eur Heart J Cardiovasc Imaging. 2015;16:1191–1197.
- Kaminski M, Steel K, Jerosch-Herold M, et al. Strong cardiovascular prognostic implication of quantitative left atrial contractile function assessed by cardiac magnetic resonance imaging in patients with chronic hypertension. J Cardiovasc Magn Reson. 2011;13:42.
- Hedberg P, Selmeryd j, Leppert J, et al. Long-term prognostic impact of left atrial volumes and emptying fraction in a community-based cohort. Heart. 2016;103:687–693.
- Santos ABS, Kraigher-Krainer E, Gupta DK, for the PARAMOUNT Investigators, et al. Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014;16:1096–1103.
- Zile MR, Baicu CF, Ikonomidis J, et al. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation. 2015;131:1247–1259.
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. An update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2016;29:277–314.
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–1360.
- Hesse B, Schuele SU, Thamilasaran M, et al. A rapid method to quantify left atrial contractile function: Doppler tissue imaging of the mitral annulus during atrial systole. Eur J Echocardiogr. 2004;5:86–92.
- Khankirawatana B, Khankirawatana S, Peterson B, et al. Peak atrial systolic mitral annular velocity by Doppler tissue reliably predicts left atrial systolic function. Am Soc Echocardiogr. 2004;17:353–360.
- Thomas L, Levett K, Boyd A, et al. Changes in regional left atrial function with aging: evaluation by Doppler tissue imaging. Eur J Echocardiogr. 2003;4:92–100.
- Paulus WJ, Tschöpe C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–2550.
- Johansson B, Lundin F, Tegeback R, et al. /a´ratio a simple detector of left ventricular dysfunction in patients with decreased ejection fraction. Scand Cardiovasc J. 2018;52:20–27.
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845.
- Royston P, Sauerbrei W. Multivariable model-building: a pragmatic approach to regression analysis based on fractional polynomials for modelling continuous variables. New York: John Wiley & Sons Ltd; 2009.
- Khouri SJ, Maly GT, Suh DD, et al. A practical approach to the echocardiographic evaluation of diastolic function. J Am Soc Echocardiogr. 2004;17:290–297.
- Di Tullio MR. Diastolic dysfunction: does ethnicity matter? J Am Coll Cardiol. 2008;52:1015–1021.
- Little WC. Diastolic dysfunction heart failure. J Card Fail. 2008;14:132.
- Lancellotti P, Galderisi M, Edvardsen T, et al. Echo-Doppler estimation of left ventricular filling pressure: results of the multicentre EACVI Euro-Filling study. Eur Heart J Cardiovasc Imaging. 2017;18;961–968.
- Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527–1533.
- Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol. 1988;12:426–440.
- Thomas L, Levett K, Boyd A, et al. Compensatory changes in atrial volumes with normal aging: is atrial enlargement inevitable? J Am Coll Cardiol. 2002;40:1630–1635.
- Prioli A, Marino P, Lanzoni L, et al. Increasing degrees of left ventricular filling impairment modulate left atrial function in humans. Am J Cardiol. 1998;82:756–761.
- Kuecherer HF, Kusumot F, Muhiudeen JA, et al. Pulmonary venous flow patterns by transesophageal pulsed Doppler echocardiography: relation to parameters of left ventricular systolic and diastolic function. Am Heart J. 1991;122:1683–1693.
- Basnight MA, Gonzalez MS, Kershenovich SC, et al. Pulmonary venous flow velocity: relation to hemodynamics, mitral flow velocity and left atrial volume, and ejection fraction. J Am Soc Echocardiogr. 1991;4:547–558.
- Thomas L, Levett K, Boyd A, et al. Changes in regional left atrial function with aging: evaluation by Doppler tissue imaging. Eur J Echocardiography. 2003;4:92–100.
- Rossvoll O, Hutle LK. Pulmonary venous flow velocities by transthoracic doppler ultrasound: Relation to left ventricular diastolic pressures. J Am Coll Cardiol. 1993;21:1687–1696.
- Kuecherer HF, Muhiudeen IA, Kusumoto FM, et al. Estimation of mean left atrial pressure from transesophageal pulsed Doppler echocardiography of pulmonary venous flow. Circulation. 1990;82:1127–1139.
- Singh A, Addetia K, Maffesanti F, et al. LA strain for categorization of LV diastolic dysfunction. JACC Cardiovas Imaging. 2017;10:735–743.