Abstract
Objective: Although the prognostic efficacy of C-reactive protein (mg/L) and albumin levels (g/L) has been previously associated with poor prognosis in ST elevation myocardial infarction (STEMI), to the best of our knowledge, the prognostic efficacy of C-reactive protein/Albumin ratio (CAR) (mg/g) has not been investigated yet. Thus, this study aimed to investigate the potential efficacy of the CAR in predicting prognosis in STEMI patients.
Method: We conducted a detailed investigation of 2437 patients with first STEMI treated with a primary percutaneous coronary intervention. After evaluation regarding to exclusion criteria, 2243 patients were found to be eligible for analysis. The mean follow-up of the study was 34 ± 15 months.
Results: The median CAR value of the study population was 2.70 (range: 1.44–4.76), and the patients were divided into three tertiles according to their CAR values. Kaplan-Meier survival analysis showed significantly lower in-hospital and long-term survival rates for the patients in a high CAR tertile. In addition, the CAR was found to be an independent predictor of all-cause mortality (Hazards ratio: 1.033, 95% Confidence Interval: 1.007–1.061, p = .033), and the prognostic performance of the CAR was superior to that of C-reactive protein, albumin, and neutrophil to lymphocyte ratio in the receiver operating characteristic curve comparison.
Conclusion: The CAR, a newly introduced inflammation-based risk index, was found to be a potentially useful prognostic tool for predicting a poor prognosis in STEMI patients. However, this finding needs to be validated in the future prospective studies.
Introduction
Although there has been a reduction in the incidence and mortality of ST elevation myocardial infarction (STEMI) in recent years according to the European Society of Cardiology guidelines, 14% of women and 16% of men die due to acute myocardial infarction [Citation1]. The decreasing trend in STEMI mortality is mainly attributed to the widespread use of reperfusion therapies, especially primary percutaneous coronary intervention (pPCI) [Citation2]. However, the survival rates are still not in the desired range. Thus, early risk classification remains important in STEMI patients, and it is useful in the selection of treatment regimens as well as in planning hospital discharge and the long-term treatment.
The effect of inflammation on atherosclerosis development and destabilization has been more clearly understood in recent years; hence, the inflammatory biomarkers are now increasingly being used in coronary artery disease screening and prognosis [Citation3]. C-reactive protein (CRP), one of the most commonly used biomarkers for this purpose, has been associated with endothelial dysfunction, prothrombotic state, atherosclerotic plaque remodeling, and destabilization [Citation4,Citation5]. Furthermore, the increased value of CRP is found to be related to the atherosclerotic burden and major adverse cardiovascular events in patients with coronary artery disease [Citation6,Citation7]. On the other hand, the inflammation causes hypoalbuminemia due to the reduced synthesis and increased catabolism of albumin. Serum albumin is the most important serum protein in the human body. In addition to its vital functions, it has several anti-atherogenic properties, including anti-oxidant activities, inhibition of platelet activation and aggregation through the modulation of arachidonic acid metabolism [Citation8]. Several previous studies reported that hypoalbuminemia is associated with the development of new myocardial infarction and the increased mortality in patients with acute coronary syndrome [Citation9–11]. When compared to CRP or albumin alone, CRP/Albumin ratio (CAR), a newly introduced inflammation-based risk index, is demonstrated to better reflect the inflammatory status, and thus the prognosis in patients with acute medical illness and malignancy [Citation12,Citation13]. However, to the best of our knowledge, no study has investigated the possible association between the CAR and in-hospital and long-term prognosis in STEMI patients. Therefore, in the present study, we aimed to investigate whether the CAR, calculated from the admission blood samples, has a prognostic value in STEMI patients who underwent pPCI.
Methods
Study population
In total, 2437 patients with first STEMI who underwent pPCI from January 2010 to January 2015 were retrospectively enrolled in the study. Patients with a prior history of active malignancy, acute infection, connective tissue disorders, proteinuria, coronary artery disease, those treated with emergency coronary artery bypass graft surgery owing to pPCI failure, and patients with incomplete data in the hospital records were excluded from the study. Finally, the study population comprised of 2243 patients. Patients’ demographic characteristics and related clinical information were obtained from the hospital’s electronic database. Thrombolysis in myocardial infarction (TIMI) risk score was also calculated for each patient. All patients were treated with the standard therapy according to the current guidelines [Citation1]. Our local ethics committee approved the study protocol in accordance with the principle of the Declaration of Helsinki.
Coronary angiography
Coronary angiography and pPCI were performed according to Judkins percutaneous trans-femoral technique. All patients received anticoagulation therapy with unfractionated heparin (70–100 units/kg (maximal dose 10.000 U) and dual antiplatelet therapy with an acetyl salic acid (300 mg) and a loading dose of clopidogrel (300–600 mg) before the procedure. Coronary blood flow patterns before and after the pPCI were subjected to a thorough evaluation for the TIMI flow grade using grades 0, 1, 2, and 3 [Citation14]. Myocardial blush grade (MBG) was assessed according to the technique defined by Van’t Hof et al. [Citation15]. If the TIMI flow was <3 or the patient had TIMI flow of 3 with MBG <2, it was defined as angiographic no-reflow. Thrombus burden was assessed according to the TIMI thrombus grading scale that ranged from grade 0 (no thrombus) to grade 5 (very large thrombus causing vessel occlusion). Patients with a grade 5 thrombus were re-classified into grade 0, 1, 2, 3, or 4 after recanalization with a guide-wire or a small balloon [Citation16].
Laboratory measurements
Routine complete blood cell count and blood chemistry measurements, including albumin (g/L) and CRP (mg/L), were performed on a blood sample obtained on admission. Cardiac troponin I (ng/L) and creatine kinase-myocardial band (U/L) measurements were repeated at 6 h until the peak values were achieved. The albumin and CRP levels were measured using Roche Diagonistics Cobas 8000 c502 analyzer. The CAR (mg/g) was calculated as the ratio of CRP to albumin level and the neutrophil to lymphocyte ratio (NLR) was calculated as the ratio of the number of neutrophil to lymphocytes, both of which obtained from the same blood samples. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation. The left ventricular ejection fraction was measured using the modified Simpson method.
In-hospital outcomes and long-term follow-up
The primary outcome of the present study was the in-hospital and long-term all-cause mortality. Secondary outcomes consisted of reinfarction, revascularization, and heart failure. In-hospital all events were determined by a trained study coordinator who evaluated the hospital files and computer records. For the evaluation of secondary outcomes, follow-up interviews (directly or by telephone) and/or visiting outpatient clinics and/or hospital electronic database were used.
Definitions
STEMI was defined based on the following criteria: I-) ongoing ischemic symptoms (within 12 h), II-) typical rise or fall in the cardiac biomarkers, and III-) a new ST elevation in ≥2 contiguous leads with leads V1, V2, and V3 measuring ≥0.2 mV or ≥0.1 mV in the remaining leads or new developed left bundle-branch block pattern [Citation1]. Myocardial reinfarction was defined as the recurrence of typical clinical symptoms and new electrocardiography changes with a new elevation of the creatine kinase myocardial band levels > twice the upper normal limit or any rise by at least >50% of the previously elevated level within 28 days of incident myocardial infarction. If myocardial infarction occurred after 28 days following an incident myocardial infarction; it was termed recurrent myocardial infarction [Citation17]. Revascularization was defined as repeated PCI or bypass grafting of not only the infarct-related artery, but also the non- infarct-related artery, driven by ischemic symptoms. New-onset heart failure was defined as the presence of heart failure with symptoms compatible with New York Heart Association class III–IV that occurred <24 h after the index event.
Statistical analyses
Statistical analyses were performed using the MedCalc trial version 16.8.4 (MedCalc Software bvba, Ostend, Belgium) and SPSS version 22.0 (IBM, Chicago, Illinois). Normality of the data was analyzed using the Kolmogorov-Smirnov test. Continuous variables with normal distribution are expressed as mean ± standard deviation and were compared using the analysis of variance test. Non-normal data are expressed as median (0.25–0.75 percentiles) values and compared using the Kruskal-Wallis H-test. The categorical variables are expressed as numbers (percentages) and were compared using Fisher’s exact test or χ2-test. Event-free survival curves of the CAR tertiles were demonstrated using Kaplan-Meier survival curve analysis and compared using the log-rank test. The risk factors for all-cause mortality were analyzed using a multivariate Cox proportional hazard analyses with variables that showed statistically significant associations with mortality in the univariate analyses. The additive predictive value of CAR for predicting all-cause mortality was assessed using reclassification tables, net reclassification improvement, and integrated discriminative improvement methods, as described by Pencina et al. [Citation18]. The receiver operating characteristic (ROC) curve was utilized to derive the best cut-off values of the CAR for predicting all-cause mortality. The method proposed by DeLong et al. was then used to compare the ROC curves of the CAR, CRP, albumin, and the NLR for predicting all-cause mortality. A p value < .05 was considered statistically significant.
Results
The study population comprised 2243 STEMI patients who underwent a pPCI. The median CAR value of the study population was 2.70 (range: 1.44–4.76). The subjects were divided into three groups according to their CAR tertiles; patients with CAR <1.82 were allocated to a low tertile group (n: 748), those with 1.82 < CAR <3.94 were in an intermediate tertile group (n: 748), and those with CAR >3.94 formed a high tertile group (n: 747).
Comparison of baseline characteristics, laboratory, and angiographic findings
The demographic, clinical, laboratory and angiographic characteristics of all patients are listed in . The frequencies of diabetes mellitus, history of hypertension, family history of coronary artery disease, and a previous statin use were more frequent in patients with a high CAR tertile. Patients in a high CAR tertile had a significantly longer time from pain onset as well as an elevated heart rate, Killip class >1, and cardiac arrest on admission than those in an intermediate and low CAR tertiles. As the CAR tertiles increased, hemoglobin and eGFR levels decreased, while the white blood cell count, blood glucose on admission, peak troponin I, peak creatine kinase myocardial band, brain natriuretic peptide levels, and NLR increased. An evaluation of the angiographic characteristics of the study population showed that patients with a high CAR had a significantly elevated frequency of the left anterior descending as the infarct-related artery, proximal/ostial lesion for infarct-related artery, baseline TIMI flow <3, high thrombus grade, angiographic no-reflow, the left main coronary artery disease, and chronic total occlusion of non-infarct related vessels than those with a low CAR. The patients within a high CAR tertile had also higher TIMI risk score compared to those with an intermediate and low CAR tertiles.
Table 1. Demographic, clinical, laboratory and angiographic characteristics of all patients.
In-hospital and long-term outcomes
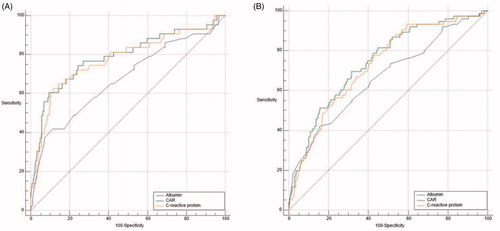
In-hospital and long-term events for all patients are listed in . A total of 86 (3.8%) patients died during in-hospital course. The all-cause mortality rate of patients in a high CAR tertile was significantly higher than that of the patients in an intermediate and low tertiles (1.3% vs. 1.3% vs. 8.8%, respectively; p < .001). We noted that adverse secondary outcomes were more frequent in a high CAR tertile than in the intermediate and lower tertiles during hospital stay. The mean long-term follow-up of the study was 34 ± 15 months. A total of 145 (6.5%) patients died during long-term follow-up. All-cause mortality, myocardial reinfarction, and advanced heart failure rate were more frequent in a high CAR tertile than in the intermediate and lower tertiles. Kaplan-Meier survival analysis showed significantly lower in-hospital (log rank = 45.7, p < .001, ) and long-term survival rates (log rank = 95.1, p < .001, ) for the patients in a high CAR tertile.
Figure 1. Kaplan Meier survival analysis of in-hospital (A) and long-term all-cause mortality (B) in patients located in a low, intermediate, and high C-reactive protein/Albumin ratio (CAR) tertiles.
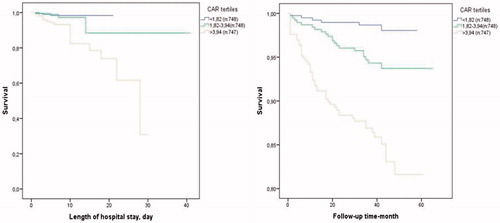
Table 2. In-Hospital and long-term events of all patients and C-reactive protein/albumin ratio (CAR) tertiles with p value.
Independent predictors of all-cause mortality
To identify the independent predictors of all-cause mortality, a multivariate Cox regression analyses with a stepwise backward model were performed using the variables that showed marginal association with all-cause mortality in the univariate analyses. These variables are shown in . Age, cardiac arrest on admission, the NLR, eGFR, the CAR, peak troponin I, left ventricular ejection fraction, the TIMI risk score, and chronic total occlusion were found to be independent predictors of all-cause mortality in multivariate analysis.
Table 3. Independent predictors of all-cause mortality.
ROC analysis and comparison
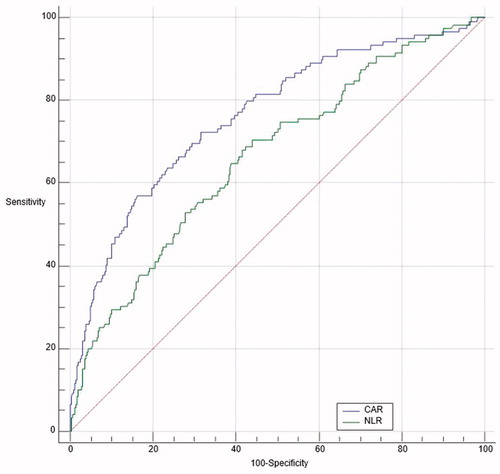
The optimal cut-off value of CAR for predicting in-hospital and long-term all-cause mortality was >7.38 with a sensitivity of 60.5% and a specificity of 90.5% (area under the curve [AUC]: 0.787; 95%CI: 0.769–0.804). To assess whether CAR had an additional prognostic value over CRP and albumin levels; their ROC curves were compared. The AUC value of CAR was found to be significantly higher than that of CRP (AUC: 0.774; %95 CI: 0.756–0.791; p = .0018) and albumin level (AUC: 0.712, %95 CI: 0.692–0.730; p = .0478) in predicting in-hospital mortality (). Moreover, CAR surpassed CRP (AUC: 0.721, %95 CI: 0.701–0.739; p < .001) and albumin levels (AUC: 0.663, %95 CI: 0.643–0.683; p = .005) in the prediction of long-term all-cause mortality (). On comparison of the ROC curve of CAR with that of NLR, the AUC value of CAR (AUC: 0.758, %95 CI: 0.724–0.793, p < .001) was superior to that of NLR (AUC: 0.662, %95 CI: 0.624–0.700; p < .001) in the prediction of all-cause mortality (p < .001) ().
Net reclassification and integrated discrimination improvement
The reclassification improvement of the CAR plus TIMI risk score vs. TIMI risk score was assessed by monitoring movement between low (defined as <5%), moderate (defined as 5%–15%), and high (defined as >15%) risk categories (). When CAR plus TIMI risk score compared to TIMI risk score alone, it produced a net reclassification improvement of 0.041 with p = .042, that is an 4.1% improved classification. The integrated discrimination improvement was 1.436 (p < .001).
Table 4. The changes in risk prediction for all-cause mortality using CAR plus TIMI risk score vs. TIMI risk score.
Discussion
Recent studies have shown that the inflammation is one of the leading factors in all the stages of atherogenesis, from fatty streaks to plaque rupture. In two studies that included apparently healthy men and women, the increased body inflammation that demonstrated by using CRP measurements was associated with increased development of myocardial infarction and stroke [Citation19,Citation20]. CRP has also been studied in patients with stable coronary artery disease and acute coronary syndrome, and has been related to the severity of coronary artery disease, recurrent coronary events, and mortality [Citation6,Citation7,Citation21,Citation22]. Although there is an ongoing debate about whether CRP is a bystander or an active participant in atherogenesis, recent studies have shown that CRP itself has several pro-atherogenic effects [Citation3–5,Citation23]. Besides that, the inflammation may lead to low levels of negative acute phase reactants such as albumin in the body. The inflammatory response of the body decreases the synthesis of serum albumin and increases its degradation. Serum albumin has also several properties other than its vital function that is claimed to have a protective effect against atherosclerosis. These functions include the inhibition of low density lipoprotein cholesterol oxidation [Citation24], enhanced vasodilatation, inhibition of platelet activation and aggregation through the reduced synthesis of thromboxane A2, and the increased bioavailability of prostacyclin [Citation8,Citation25,Citation26]. In clinical practice, decreased serum albumin levels have been shown to be associated with poor prognosis in patients with acute coronary syndrome [Citation10,Citation11].
The CAR, which is a novel inflammation-based risk index, was first reported in patients with acute illness [Citation12,Citation27]. In addition, CAR has been previously studied in patients with malignancy [Citation13], and it was observed that an elevated CAR was closely related to poor prognosis among these patients. This inverse relationship between CRP and albumin in the determination of the poor prognosis in patients with acute illness and malignancy led us to investigate whether the combination of these biomarkers in a single parameter might have an additional value for predicting the mortality in STEMI patients. According to the ROC curve, the AUC value of the CAR was found to be higher than CRP and albumin alone or NLR for predicting in-hospital and long-term all-cause mortality in STEMI patients. Additionally, we found that an increased CAR was significantly associated with myocardial reinfarction and advanced heart failure during in-hospital stay and in the long-term follow-up. Also, we were able to show that when CAR plus TIMI risk score compared to TIMI risk score alone, it results in a net improvement of 4.1% over the original score. Consequently, our findings demonstrated a significant relationship between the CAR and overall survival, which might suggest that a combination of these two parameters was even more useful predictor of short and long-term clinical outcomes in STEMI patients who underwent a pPCI. Thus, we do believe that our results point to a promising simple risk stratification tool for these STEMI patients.
The inflammatory markers is closely related to the magnitude of myocardial damage [Citation28]. In addition, the timing of the measurements of CAR is closely related to magnitude of myocardial damage. In the study, we observed that patients with a high CAR tertile had also a longer time form pain onset, hence these patient had larger magnitude of myocardial damage. This finding therefore may imply as a proxy of the delay from symptom onset to treatment, and it may be related to poor outcome among these patients. Also, elevated CAR values on admission may be a marker of underlying atherosclerotic risk because the frequency of the left anterior descending as the infarct-related artery and proximal/ostial lesion for the infarct-related artery were significantly higher in patients with a high CAR tertile compared to those with an intermediate and low CAR tertiles. However, multi-vessel disease was not different between the groups. In our study, we also noted that patients in a high CAR tertile had a significantly higher prevalence of anterior myocardial infarction, Killip class >1 on admission, high thrombus grade, and angiographic no-reflow than patients in an intermediate and lower CAR tertiles, these findings suggested that patients with a high CAR had a large infarction, thereby demonstrating a poor prognosis.
Of note, our results demonstrated that the CAR may have an additive prognostic value in the development of an individual-risk approach and surveillance of STEMI patients who underwent a pPCI. Particularly, the patients with an elevated CAR may require more frequent follow-up and intense therapy. Moreover, as an easily accessible parameter, the CAR is simple to calculate, and it can be standardized without additional cost, thus offering increased convenience for prognostication of these patients.
Limitations of the study
Certain limitations of the present study need to be acknowledged while interpreting the results of this study. First, the present study had a retrospective design; therefore, the results could be biased. Second, the patients with a previous history of coronary artery diseases were excluded; thus, these results cannot be generalized to all STEMI patients. Third, despite the fact that patients with a known prior history of active malignancy, acute infection, connective tissue disorders, proteinuria were screened, subclinical condition that could cause an increased CRP and decreased albumin might not have excluded. Finally, the prognostic value of CAR needs to be validated in further prospective studies.
Conclusion
The present study provided evidence that an elevated CAR, which is a novel inflammation-based risk index, is an independent predictor of in-hospital and long-term all-cause mortality in STEMI patients who were treated with a pPCI. The results suggest that the CAR is a more efficacious prognostic tool than CRP and albumin alone or NLR in this context. However, our findings warrant confirmation by large, well-designed prospective and randomized trials.
Acknowledgements
The authors thank www.metastata.com for their contributions to statistical analysis and trial design. We also thank İnanç Artaç, Doğan İliş, Eray Atalay, and Mesut Öterkuş for their assistance in data acquisition and cleaning.
Disclosure statement
All authors declare that they do not have a potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J. 2012;33:2569–2619.
- Sidney S, Rosamond WD, Howard VJ, et al. The “heart disease and stroke statistics-2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127:21–23.
- Bisoendial RJ, Boekholdt SM, Vergeer M, et al. C-reactive protein is a mediator of cardiovascular disease. Eur Heart J. 2010;31:2087–2091.
- Bisoendial RJ, Kastelein JJP, Peters SLM, et al. Effects of CRP infusion on endothelial function and coagulation in normocholesterolemic and hypercholesterolemic subjects. J Lipid Res. 2007;48:952–960.
- Devaraj S, Kumaresan PR, Jialal I. Effect of C-reactive protein on chemokine expression in human aortic endothelial cells. J Mol Cell Cardiol. 2004;36:405–410.
- Taniguchi H, Momiyama Y, Ohmori R, et al. Associations of plasma C-reactive protein levels with the presence and extent of coronary stenosis in patients with stable coronary artery disease. Atherosclerosis. 2005;178:173–177.
- Haverkate F, Thompson SG, Pyke SD, et al. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997;349:462–466.
- Purdon AD, Rao AK. Interaction of albumin, arachidonic acid and prostanoids in platelets. Prostaglandins, Leukot Essent Fat Acids. 1989;35:213–218.
- Nelson JJ, Liao D, Sharrett AR, et al. Serum albumin level as a predictor of incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2000;151:468–477.
- Oduncu V, Erkol A, Karabay CY, et al. The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron Artery Dis. 2013;24:88–94.
- Kurtul A, Murat SN, Yarlioglues M, et al. Usefulness of serum albumin concentration to predict high coronary SYNTAX score and in-hospital mortality in patients with acute coronary syndrome. Angiology. 2016;67:34–40.
- Fairclough E, Cairns E, Hamilton J, et al. Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clin Med (Lond). 2009;9:30–33.
- Kinoshita A, Onoda H, Imai N, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22:803–810.
- Gibson CM, Cannon CP, Murphy SA, et al. Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation. 2002;105:1909–1913.
- van’t Hof AW, Liem A, Suryapranata H, et al. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Circulation. 1998;97:2302–2306.
- Gibson CM, de Lemos JA, Murphy SA, et al. Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation. 2001;103:2550–2554.
- Mendis S, Thygesen K, Kuulasmaa K, et al. World Health Organization definition of myocardial infarction: 2008-09 revision. Int J Epidemiol. 2011;40:139–146.
- Pencina MJ, D’Agostino RB, D’Agostino RB, Jr, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Statist Med. 2008;27:157–172.
- Ridker PM, Buring JE, Shih J, et al. Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733.
- Ridker PM, Cushman M, Stampfer MJ, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–979.
- Karadeniz M, Duran M, Akyel A, et al. High sensitive CRP level is associated with intermediate and high syntax score in patients with acute coronary syndrome. Int Heart J. 2015;56:377–380.
- Makrygiannis SS, Ampartzidou OS, Zairis MN, et al. Prognostic usefulness of serial c-reactive protein measurements in ST-elevation acute myocardial infarction. Am J Cardiol. 2013;111:26–30.
- Zwaka TP, Hombach V, Torzewski J. C-reactive protein-mediated low density lipoprotein uptake by macrophages: implications for atherosclerosis. Circulation. 2001;103:1194–1197.
- McDowell IFW, McEneny J, Trimble ER. A rapid method for measurement of the susceptibility to oxidation of low-density lipoprotein. Ann Clin Biochem an Int J Biochem Lab Med. 1995;32:167–174.
- Mikhailidis DP, Ganotakis ES. Plasma albumin and platelet function: relevance to atherogenesis and thrombosis. Platelets. 1996;7:125–137.
- Mikhailidis DP, Mikhailidis AM, Dandona P. Effect of human plasma proteins on stabilisation of platelet anti-aggregatory activity of prostacyclin. Ann Clin Biochem. 1982;19:241–244.
- Ranzani OT, Zampieri FG, Forte DN, et al. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013;8:e59321.
- Chan D, Ng LL. Biomarkers in acute myocardial infarction. BMC Med. 2010; 8:34