Abstract
Objectives. Due to age-related differences in aortic valve structure, it is likely that the pathophysiology of aortic stenosis (AS) and associated risk factors differ between age groups. Here we prospectively studied the influence of traditional cardiovascular risk factors on AS development requiring surgery among patients without concomitant coronary artery disease (CAD) and stratified for age. Design. This study included 322 patients, who had prior to surgery for AS participated in population-based surveys, and 131 of them had no visible CAD upon preoperative coronary angiogram. For each case, we selected four referents matched for age, gender, and geographic area. To identify predictors for surgery, we used multivariable conditional logistic regression with a model including arterial hypertension (or measured blood pressure and antihypertensive medication), cholesterol levels, diabetes, body mass index (BMI), and smoking. Results. In patients without CAD, future surgery for AS was associated with arterial hypertension and elevated levels of diastolic blood pressure in patients younger than 60 years at surgery (odds ratio [95% confidence interval]), (3.40 [1.45–7.93] and 1.60 [1.09–2.37], respectively), and with only impaired fasting glucose tolerance in patients 60 years or older at surgery (3.22 [1.19–8.76]). Conclusion. Arterial hypertension and elevated diastolic blood pressure are associated with a risk for AS requiring surgery in subjects below 60 years of age. Strict blood pressure control in this group is strongly advocated to avoid other cardiovascular diseases correlated to hypertension. If hypertension and elevated diastolic blood pressure are risk factors for developing AS requiring surgery need further investigations. Notably, elevated fasting glucose levels were related to AS requiring surgery in older adults without concomitant CAD.
Background
In western countries, aortic valve replacement is the second most common cardiothoracic procedure, following coronary artery by-pass surgery [Citation1]. Among patients with aortic stenosis over 60 years old, tricuspid valves are most prevalent, comorbidity with coronary atherosclerosis is common [Citation2], and traditional cardiovascular risk factors play an important role [Citation3]. However, in patients under 60 years old, bicuspid aortic valve (BAV) is the most common underlying valve pathology, and little information is available regarding the influence of traditional cardiovascular risk factors on aortic stenosis development in this population. Studies of clinical factors related to aortic stenosis development are usually retrospective or cross-sectional, and commonly utilize data obtained near the time of surgery, i.e in patients with severely affected valves. Several possible risk factors, such as hypercholesterolemia, have emerged in this context. However, treatment targeting these risk factors has not been shown to modify the course of disease progression [Citation4–6].
The prevalence of BAV varies with age in aortic valve disease, and can occur with or without concomitant coronary artery disease (CAD); thus, we hypothesised that the influence of traditional cardiovascular risk factors would vary among these groups. In our present study, we prospectively studied the presence of traditional cardiovascular risk factors prior to surgery for aortic stenosis among patients without CAD and stratified for age (<60 years and ≥60 years old).
Methods
Study population
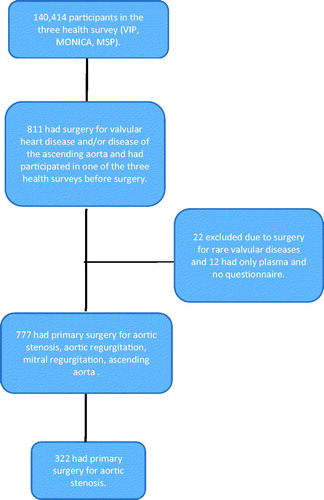
A total of 6691 patients underwent surgery for valvular heart disease and/or disease of the ascending aorta at the Department of Cardiothoracic Surgery, Umeå University Hospital, Umeå, Sweden, between March 1988 and December 2014. Prior to their first surgery, 799 of these patients had participated in one of three population-based health studies in Northern Sweden: 619 patients in the Västerbotten Intervention Program (VIP), 101 patients in the Northern Sweden MONItoring Of trends and Determinants in CArdivascular Disease (MONICA) survey, and 79 patients in the Mammary Screening Program (MSP). Among these study participants, 322 had undergone surgery for the primary indication of aortic stenosis.
The VIP is an ongoing community intervention program targeting cardiovascular disease and diabetes prevention. At the ages of 30, 40, 50, and 60 years, subjects are asked to participate in a health survey at their primary health centre. MONICA enrolment involves inviting randomly selected individuals to participate in a health survey. Participants are 25–74 years of age, and from the counties of Västerbotten and Norrbotten [Citation7]. The MSP cohort comprises women who attended a routine mammography screening. Altogether, these three surveys included 140,414 participants up to December 2014, with participation rates of 65–75%. The study base and the selection of cases are further illustrated in .
For each case, we randomly selected four referents who were matched for sex, age (±2 years), type of survey (MONICA, VIP, or MSP), date of health survey (±4 months), and geographical area. We did not exclude participants with a history of cancer or myocardial infarction. Altogether, 2.8% of cases and 5.6% of referents had cancer within 5 years prior to surgery (or the corresponding date for referents). Similarly, 4.3% of cases and 2.0% of referents reported prior myocardial infarction.
The study protocol was approved by the Regional Ethical Review Board in Umeå (07–174M) and complies with the Declaration of Helsinki. All participants gave written informed consent for future use of the data.
Perioperative characteristics
From hospital files, we obtained data from preoperative assessments, including medical history, current medication, anthropometry, blood pressure, electrocardiogram, coronary angiogram, and echocardiography when available. According to established practise, all cases underwent coronary angiogram, and the findings were used to categorize CAD. Any sign of arteriosclerosis or atheromatosis was considered to indicate CAD (found in 59.3% of all cases).
Baseline clinical examinations and biochemical analysis
At the initial health survey, VIP and MONICA participants were asked to complete a health questionnaire regarding their living conditions and cardiovascular risk factors, and anthropometry and blood pressure measurements were taken. Participant weight was measured in light indoor clothing without shoes, and recorded to the nearest 0.2 kg. Height was measured without shoes to the nearest centimetre. Body mass index (BMI) was calculated as weight divided by height squared. Subjects were categorized as daily smokers, ex-smokers, or never-smokers.
An oral glucose tolerance test, including measurements of fasting and post-load glucose levels, was routinely performed in the VIP, was performed in 60% of MONICA participants, and was not performed in the MSP. Diabetes presence was determined based on self-reported usage of anti-diabetic medication, fasting plasma glucose levels ≥ 7.0 mmol/L, and/or post-load plasma glucose levels ≥ 11.1 mmol/L (≥12.2 mmol/L based on capillary plasma in the VIP). Impaired fasting glucose was defined as a fasting glucose level of ≥6.1 and <7.0 mmol/L. Impaired glucose tolerance was defined as a post-load glucose level of ≥7.8 and <11.1 (≥8.9 and <12.2 in the VIP) combined with a non-diabetic fasting glucose level.
In all surveys, blood pressure was measured after 5 minutes of rest, using a mercury sphygmomanometer prior to 2004, and using semi-automatic devices since 2004 (Omron M7, Omron Corp., Kyoto, Japan). Patients were seated for blood pressure measurement throughout the MONICA and MSP surveys, whereas in the VIP survey, blood pressure was measured with participants in the recumbent position until September 2009 and thereafter in the sitting position. Measurements obtained with participants in the recumbent position were adjusted using a sex- and age-specific formula [Citation8]. Hypertension was defined as systolic blood pressure of ≥140 mmHg, diastolic blood pressure of ≥90 mmHg, and/or use of anti-hypertensive medication. The usage of antihypertensive medication was self-reported.
Total serum cholesterol was measured at the time of the health survey using a bench-top analyser (ReflotronR, Boehringer Mannheim GmbH Diagnostica, Mannheim, Germany) in the VIP until September 2009, or at a central laboratory using an enzymatic method (Boehringer Mannheim GmbH Diagnostica, Mannheim, Germany) in MONICA and the VIP after September 2009. Cholesterol values obtained using the bench-top method were adjusted to the results measured at the central laboratory.
Statistical analysis
Missing values for categorical variables were treated as a separate category and are not included in the tables. Data are presented as mean and 95% confidence interval (CI). Student’s t-tests were used to analyse differences in the means between cases and referents. Continuous variables were categorized into quartiles based on the distribution of the referent values, separately for men and women. In addition, systolic and diastolic blood pressure were analysed as z-scores based on the distribution among referents, and were calculated separately for men and women. As a conservative approach, missing values were replaced with the median value obtained among the referents. Since cases and referents had the same follow-up time within strata in this nested and matched case-referent study, logistic regression analysis (rather than Cox regression) using the conditional maximum likelihood routine designed for matched analysis was used to estimate odds ratios (ORs) and 95% CIs, and the influence of studied variables on surgery for aortic stenosis was tested in univariate and multivariable models. The analyses were stratified for age at surgery (less than 60 years or 60 years and more), presence of any visible CAD on the preoperative angiogram, and time-interval between health survey and valvular surgery (more than 5 years or less). For multivariable analyses, we used a model including established cardiovascular risk factors, i.e arterial hypertension, total cholesterol, BMI, glucose tolerance, and smoking. All calculations were performed using the statistical program SPSS version 24 (IBM, Armonk, NY, USA).
Results
Of the 322 patients operated for the primary indication of aortic stenosis, 70 underwent surgery before 60 years of age and 252 after 60 years of age. presents the characteristics of the study population at the baseline health survey, stratified for age at surgery and presence of CAD. All patients underwent open-chest surgery for aortic valvular replacement and no one had a transcatheter aortic valve implantation (TAVI) procedure. Two patients reported previous surgery for coarctation and had surgery for AS at the age of 55 and 57 years, respectively.
Table 1. Characteristics of the study population at the time of survey.
The presence of arterial hypertension predicted independently of other risk markers future aortic valve surgery in patients <60 years of age at surgery, irrespective of coexisting CAD (). After exclusion of those with valvular surgery within 5 years after survey, the point estimates for increased risk remained although not significant for those with CAD (odds ratio [95% confidence interval]) (6.70 [2.06–21.76] and 6.64 [0.96–45.92] for those without CAD and with CAD respectively). In contrast, a high systolic blood pressure did not independently predict valvular surgery irrespective of coexisting CAD (data not shown). However, a high diastolic blood pressure (z-score) independently predicted valvular surgery in those without CAD (1.60 [1.09–2.37]), but not in those with CAD (1.22 [0.64–2.31]). These associations were attenuated after further adjustment for self-reported antihypertensive medication (1.47 [0.97–2.23] and (1.09 [0.54–2.21], respectively).
Table 2. Predictors of aortic stenosis requiring surgery at the age less than 60 years.
After exclusion of those with valvular surgery within 5 years after survey, diastolic blood pressure (z-score) remained independently associated with surgery in those without CAD (1.98 [1.22–3.21], and 1.73 [1.03–2.91] after further adjustment for antihypertensive medication).
Among patients who underwent surgery at ≥60 years of age and who had concomitant CAD, the risk of future aortic valve surgery was increased by arterial hypertension, diabetes, high cholesterol levels, and active smoking (). In this group of elderly patients with CAD, a high systolic and diastolic blood pressure (z-scores) also predicted valvular surgery tested in separate models, (1.43 [1.17–1.74] and 1.25 [1.01–1.54], respectively), and remained associated with surgery after exclusion of those with surgery within 5 years, (1.42 [1.13–1.78] and 1.28 [1.02–1.62], respectively). The association between systolic blood pressure (z-score) and surgery remained after further adjustment for antihypertensive medication (1.39 [1.14–1.70]).
Table 3. Predictors of aortic stenosis requiring surgery at the age of 60 years or higher.
However, among patients in the older group who did not have CAD, future valvular surgery was predicted only by increased fasting glucose levels expressed as impaired fasting glucose, and this association remained only in those with valvular surgery more than 5 years after the health survey (4.34 [1.36–13.83]). Arterial hypertension, systolic or diastolic blood pressure did not predict surgery in this elderly group without CAD (data not shown).
Multivariable analyses using quartiles of systolic or diastolic blood pressure did not add any extra information (data not shown).
Discussion
Our present results demonstrated that arterial hypertension was associated with future surgery for aortic stenosis among younger patients (<60 years old) who are expected to show a high frequency of bicuspid valves. On the other hand, numerous classical cardiovascular risk factors predicted surgery among older adults (≥60 years old) with CAD. Notably, impaired fasting glucose was strongly associated with aortic stenosis requiring surgery among older adults without CAD.
Earlier cross-sectional studies have reported that aortic stenosis is associated with hypertension and elevated cholesterol [Citation3,Citation9]. Several randomized clinical trials have examined whether cholesterol level reduction can slow the stenosis progression rate [Citation6,Citation10,Citation11]. However, none of these interventional trials have been effective, likely due to late treatment initiation during an already ongoing and advanced process.
Bicuspid valves occur in about 2% of the population, and a substantial proportion of these patients will require replacement surgery [Citation12]. In our present study, arterial hypertension was more common among the younger patients, which also may increase the life-time risk for other cardiovascular diseases [Citation13]. We suggest that hypertension may be part of the vascular syndrome that includes bicuspid aortic valve, coarctation of the aorta, and ascending aorta dilatation. Correspondingly, arterial hypertension is common in patients with coarctation of the aorta, even after reconstructive surgery [Citation14,Citation15].
Elevated systolic blood pressure, but not hypertension, is reportedly related to faster aortic valve calcification—notably, with a differential effect on aortic valvular calcium vs. coronary artery calcium [Citation16]. This may be caused by increased mechanical strain that induces mineralization in the aortic valvular interstitial cells [Citation17]. In relation to anti-hypertensive treatment, it is also possible that drugs affecting the renin-angiotensin system could modulate aortic stenosis progression [Citation18].
To our knowledge, a high diastolic blood pressure has not been associated with the development of aortic stenosis requiring surgery. In this study, elevated diastolic blood pressure, but not elevated systolic blood pressure, predicted valvular surgery in younger patients without visible CAD. Diastolic hypertension is a risk factor for cardiovascular disease in younger individuals, and is associated with increased peripheral vascular resistance [Citation19]. In our younger patients with assumingly high frequency of bicuspid valves, alteration in the vascular system as a part of the bicuspid valve vascular syndrome might explain the increase of elevated diastolic pressure.
We used a composite definition of arterial hypertension based on antihypertensive medication or measured high levels of systolic or diastolic blood pressure. This definition has been frequently used in previous trials and case-referent studies and should better mirror lifelong exposure for elevated blood pressure than measured levels at the health survey [Citation13,Citation20,Citation21]. Furthermore, the antihypertensive treatment and the blood pressure effect of the progressing aortic stenosis could also explain why a high systolic blood pressure did not predict valvular surgery in our study. However, the effect of arterial hypertension and elevated diastolic blood pressure on future risk for valvular surgery remained after exclusion of those with surgery within five years from the survey. This indicates that the progressive valvular disease did not explain the results, and that the negative effect of high blood pressure on the aortic valve takes years to develop.
In the older group with concomitant CAD, the high systolic and diastolic blood pressure is probably one of several risk factors involved in the arteriosclerotic process comprising both the coronary arteries and the aortic valve. In fact, the diastolic blood pressure acts on the closed aortic valve and may hypothetically be more important than the systolic pressure that opens the valve.
Reduced glucose tolerance is reportedly associated with CAD, and impaired fasting glucose has been identified as an independent predictor of all-cause mortality and cardiovascular mortality [Citation22–25]. In our present study, we revealed an association between impaired fasting glucose and aortic stenosis requiring surgery in older adults without CAD. These findings have not previously been described and is in line with the theory that impaired fasting glucose is a risk factor for cardiovascular disease.
Limitations
The inclusion criteria for the VIP survey may have affected the age distribution of the patient population, i.e. persons were included only if they had a health survey performed at 30, 40, 50, or 60 years of age. This may have led to underrepresentation of younger patients with bicuspid valves in our study. In this study, we do not have complete data on the underlying valve morphology. However, in patients younger than 60 years of age bicuspid valves are by far the most common valve morphology. Finally, the present study included only patients requiring surgery and, thus, the results cannot necessarily be generalised to patients with less severe disease.
Conclusions
Our results indicate that a diagnosis of arterial hypertension and elevated diastolic blood pressure are more common among patients who require surgery for aortic stenosis before the age of 60 years, regardless of concomitant CAD. On the other hand, a diagnosis of hypertension was not a risk marker for patients who need surgery for aortic stenosis after the age of 60 years and who do not have CAD. Within this patient group, impaired fasting glucose was a risk marker for development of aortic stenosis requiring surgery.
Authors' contributions
SS, BJ and JL designed the study, acquired and analysed data. JL, BJ and SS have drafted the manuscript and all authors have revised the manuscript critically for important intellectual content. All authors approved the final version and are accountable for all aspects of the manuscript.
Acknowledgements
We deeply appreciate the assistance from Jan Henschel, Elin Albersson, Paul Holmer, Veronica Hellström, Åsa Ågren, Göran Hallmans, Camilla Ring, Mattias Söderberg, and Catrin Johansson, all of whom have been instrumental for the completion of this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability
The datasets generated and/or analysed during the current study are not publicly available as the data set contains identifiable patient data but are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Vahanian A, Alfieri O. Guidelines on valvular heart disease in clinical practice. EuroIntervention 2013;9:S11–S13.
- Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 2005;111:920–925.
- Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–634.
- Carabello BA. The SEAS Trial. Curr Cardiol Rep. 2010;12:122–124.
- Rajamannan NM, Greve AM, Moura LM, et al. SALTIRE-RAAVE: targeting calcific aortic valve disease LDL-density-radius theory. Expert Rev Cardiovasc Ther. 2015;13:355–367.
- Chan KL, Teo K, Dumesnil JG, et al. Effect of Lipid lowering with rosuvastatin on progression of aortic stenosis: results of the aortic stenosis progression observation: measuring effects of rosuvastatin (ASTRONOMER) trial. Circulation 2010;121:306–314.
- Eriksson M, Holmgren L, Janlert U, et al. Large improvements in major cardiovascular risk factors in the population of northern Sweden: the MONICA study 1986–2009. J Intern Med. 2011;269:219–231.
- Weinehall L, Hallgren CG, Westman G, et al. Reduction of selection bias in primary prevention of cardiovascular disease through involvement of primary health care. Scand J Prim Health Care. 1998;16:171–176.
- Wang C, Jiang L, Feng S, et al. Risk factor analysis of calcification in aortic and mitral valves in maintenance peritoneal dialysis patients. Kidney Blood Press Res. 2013;37:488–495.
- Rossebo AB, Pedersen TR. Hyperlipidaemia and aortic valve disease. Curr Opin Lipidol. 2004;15:447–451.
- Cowell SJ, Newby DE, Prescott RJ, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. 2005;352:2389–2397.
- Otto CM, Prendergast B. Aortic-valve stenosis-from patients at risk to severe valve obstruction. N Engl J Med. 2014;371:744–756.
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219.
- Teo LL, Cannell T, Babu-Narayan SV, et al. Prevalence of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol. 2011;32:1120–1127.
- Toro-Salazar OH, Steinberger J, Thomas W, et al. Long-term follow-up of patients after coarctation of the aorta repair. Am J Cardiol. 2002;89:541–547.
- Tastet L, Capoulade R, Clavel MA, et al. Systolic hypertension and progression of aortic valve calcification in patients with aortic stenosis: results from the PROGRESSA study. Eur Heart J Cardiovasc Imaging. 2017;18:70–78.
- Bouchareb R, Boulanger MC, Fournier D, et al. Mechanical strain induces the production of spheroid mineralized microparticles in the aortic valve through a RhoA/ROCK-dependent mechanism. J Mol Cell Cardiol. 2014;67:49–59.
- Bull S, Loudon M, Francis JM, et al. A prospective, double-blind, randomized controlled trial of the angiotensin-converting enzyme inhibitor Ramipril In Aortic Stenosis (RIAS trial). Eur Heart J Cardiovasc Imaging. 2015;16:834–841.
- Lewington S, Clarke R, Qizilbash N, Prospective Studies C, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–1913.
- Rossebo AB, Pedersen TR, Boman K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med. 2008;359:1343–1356.
- Söderberg S, Stegmayr B, Stenlund H, et al. Leptin, but not adiponectin, predicts stroke in males. J Intern Med. 2004;256:128–136.
- Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet. 2002;359:2140–2144.
- Qiao Q, Jousilahti P, Eriksson J, et al. Predictive properties of impaired glucose tolerance for cardiovascular risk are not explained by the development of overt diabetes during follow-up. Diabetes Care. 2003;26:2910–2914.
- Di Pino A, Urbano F, Piro S, et al. Update on pre-diabetes: focus on diagnostic criteria and cardiovascular risk. World J Diabetes. 2016;7:423–432.
- Barr EL, Zimmet PZ, Welborn TA, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Circulation 2007;116:151–157.